You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
SPECIALITY CL FORUM BY ALEX PETTY*<br />
ORTHO-KERATOLOGY FOR THE POST-LASIK CORNEA<br />
Before we delve into our next case I should<br />
make it known that shortly after my<br />
last column was published in May I was<br />
summoned to an urgent meeting with the<br />
NZ Optics editorial team. Disturbing reports<br />
had emerged of the readership falling asleep<br />
when perusing the contents of Speciality<br />
Contact Lens Forum. Admittedly, I was shocked<br />
that there were optometrists out there not<br />
captivated by weird rigid lenses like me. I was<br />
issued an ultimatum: inject some personality<br />
into my case reports or be shipped back to the<br />
penal colony across the Tasman as penance for<br />
the crime of dull writing. Jokes aside it is great<br />
to see the energy Lesley and Jai are putting into<br />
the magazine and I’m excited and grateful to<br />
help out in a small way as NZ Optics evolves.<br />
Naturally I apologise in advance for the glut of<br />
‘dad’ jokes and inappropriate puns that I now<br />
have free-reign to include in future missives.<br />
On to the optometry.<br />
We all know that the results of laser refractive<br />
eye surgery are becoming increasingly<br />
impressive. However, the reality is that despite<br />
the success of the initial surgery, zero refractive<br />
error is not a guarantee as the years continue.<br />
One report suggests that in a 2-13 year followup<br />
of LASIK patients only 64.8% of low myopes<br />
and 37.3% of high myopes remained within<br />
±0.50D of their attempted correction 1 . Not<br />
only can a cornea change shape over time but<br />
the onset of presbyopia can humble/anger<br />
the patient that expects the rest of their life<br />
to be devoid of optical aids. Unsurprisingly the<br />
typical post-LASIK patient is highly reluctant to<br />
return to their bespectacled former selves. This<br />
is where contact lenses come in.<br />
Traditionally I have found that even<br />
experienced optometrists are wary to meddle<br />
with a patient’s cornea that has already been<br />
permanently reshaped by our colleagues in<br />
ophthalmology. You wouldn’t re-glaze a cake<br />
created by a top chef would you? There are<br />
concerns about flap dehiscence, the structural<br />
weaknesses of a thinner cornea and perhaps a<br />
reluctance to incur the wrath of the patient’s<br />
eye surgeon should something go wrong,<br />
(“You put WHAT on my perfectly designed<br />
cornea?!”). Perhaps we should proceed with<br />
caution. Research shows that the central<br />
flap interface following LASIK has only 2.4%<br />
of the strength of normal stroma, while the<br />
peripheral margin is 10x stronger at 28% 2 .<br />
However, the general consensus is that the<br />
use of contact lenses in conjunction with<br />
lasered corneae is quite safe, as despite the<br />
histologically weakened interface LASIK flaps<br />
are quite robust. A fantastically designed<br />
study performed LASIK on the eyes of 18<br />
rabbits then ejected them from a fighter jet<br />
cockpit to see what happened. They concluded<br />
that ‘healed LASIK flaps...are stable when<br />
subjected to a rapid vertical ejection at nine<br />
times the force of gravity 3 . I would hazard a<br />
guess that this is more than most eyes endure<br />
with the use of a contact lens.<br />
Fitting standard contact lenses to a<br />
remodelled cornea is not always straight<br />
forward however. Frequently, following<br />
laser eye surgery, the corneal curvature falls<br />
outside the normal limits that off-the-shelf<br />
You wouldn’t reglaze a cake like this! My birthday treat in 2012<br />
soft contact lenses are designed for. By way of<br />
example I should divulge that I had a highly<br />
successful iLASIK surgery to both of my highly<br />
myopic eyes three years ago courtesy of Dr<br />
Trevor Gray and the team at Eye Institute.<br />
My refractive error was eliminated (but not<br />
my long axial lengths sadly, more on this in a<br />
future article) and I see a superb 6/4.8 unaided<br />
now with just a hint of astigmatism in my<br />
right eye. Needless to say I am one of the<br />
optometrists in the pro-LASIK camp. Prior to<br />
my surgery I was the best contact lens wearer<br />
I had ever met, with complaints of discomfort<br />
few and far between. At the launch of one of<br />
the fantastic new daily-disposables recently<br />
I popped a few -0.50D lenses in to test them<br />
out. Within five minutes they were in the bin.<br />
With every blink the vision would blur over, I<br />
had a noticeable foreign body sensation and<br />
the lens quickly dried out rendering it useless.<br />
Turns out my new 35D corneae did not take to<br />
kindly to a one-size-fits-all policy.<br />
Post-LASIK dryness can also be a factor when<br />
using a contact lens, even with a customised<br />
daily RGP (which can be an excellent option<br />
to mask corneal irregularities and fit the<br />
unusual bespoke cornea). Fortunately, we<br />
live in a realm of new technologies and their<br />
applications: It may surprise you that many<br />
post-laser refractive surgery patients with<br />
troublesome residual refractive error do very<br />
well when fitted with ortho-Keratology lenses.<br />
Cue the deafening sounds of aghastment.<br />
Fitting an already heathen device to a<br />
previously altered cornea? You must be mad!<br />
Indeed, in the main orthokeratology ‘bible’;<br />
John Mountford’s Orthokeratology: Principles<br />
and Practice published back in 2004, there is<br />
no mention of fitting ortho-K to the post-<br />
LASIK cornea (although John is working on<br />
a new edition which may address this). A<br />
pubmed search shows no articles about<br />
ortho-K on a post-LASIK cornea. Despite this<br />
many experienced ortho-Keratologists around<br />
the world practice ortho-K on the post-LASIK<br />
cornea with excellent results. I personally<br />
believe there is no more harm in fitting ortho-<br />
Keratology lenses to a lasered cornea than to a<br />
virgin example. It is the understanding of most<br />
orthokeratologists that the refractive effect of<br />
ortho-K comes about due to modification of<br />
the epithelial cells of the cornea, although the<br />
jury is still out in some circles. This OCT (Fig 1.)<br />
of a patient of mine using ortho-K lenses for<br />
high myopia illustrates this by showing the<br />
thinned epithelium centrally and thickened<br />
layer para-centrally. The stroma remains<br />
relatively uniform. In contrast all forms of laser<br />
refractive corneal surgery involve permanent<br />
modification to the stroma of the cornea.<br />
The mechanism of refractive change in<br />
these two modalities are mutually exclusive.<br />
In post-LASIK ortho-K the main challenge<br />
comes with designing the back surface of an<br />
orthokeratology lens to firstly fit the paracentral<br />
cornea safely and comfortably, and<br />
secondly remodel the central epithelium in a<br />
way to correct the refractive error. Let’s look at<br />
an example:<br />
A 67-year-old lady saw me due to the sudden<br />
appearance of flashes and floaters the previous<br />
weekend. Dilated exam revealed a benign<br />
posterior vitreous detachment. The woman<br />
had hyperopic LASIK carried out to both eyes six<br />
years before but she was having more trouble<br />
with her distance vision lately. She was also<br />
sick of using reading glasses. Unaided distance<br />
vision was only R 6/10 and L 6/12 and refraction<br />
revealed residual hyperopia of R +0.75/-0.25<br />
x 175 (6/5), L +1.50/-0.50 x 85 (6/5). Her<br />
topography confirmed her hyperopic LASIK with<br />
tangential maps showing a flatter para-central<br />
ring encircling a steeper central cornea (Fig 2.).<br />
Her left cornea was slightly steeper which was<br />
surprising given the higher hyperopic error.<br />
Given the foundations were essentially already<br />
in place hyperopic post-LASIK orthokeratology<br />
was offered to this patient. We chose to further<br />
steepen her cornea in a monovision set up, with<br />
her dominant right eye for distance<br />
and her left for near tasks.<br />
In these complex cases using<br />
topography-based lens design is a nobrainer<br />
for me. To marry the correct<br />
peripheral fit with the appropriate<br />
sagittal height and base curve for the<br />
desired refractive change with a trial<br />
lens would be time-consuming and<br />
inaccurate, even if such a post-LASIK<br />
hyperopic design set existed. Instead<br />
I plugged the patients topography<br />
into rigid lens simulation software<br />
EyeSpace (Innovatus Technology,<br />
Fig 3.) and designed a custom hyperopic<br />
ortho-K lens for each eye. Because the cornea<br />
is reasonably regular we can use a rotationally<br />
symmetrical lens to get a great fit. Of course<br />
with all hyperopic ortho-K the lens base curve<br />
is steeper than the existing corneal curvature to<br />
create additional plus power.<br />
One month later the patient was thrilled<br />
with her vision as she was no longer using<br />
reading glasses and seeing well at distance.<br />
Her right eye was seeing 6/6 N8 with a<br />
modest central steepening. Her left eye was<br />
6/15 N4 with an impressive 4.7D steepening<br />
in a well centred location (Fig 4.). Importantly<br />
she experienced no discomfort and her cornea<br />
was pristine with no trace of corneal insult.<br />
Unfortunately, not all post-LASIK refractive<br />
error is regular. Post-LASIK ectasia can be<br />
highly debilitating and severely limit the<br />
corrective options available. In some cases,<br />
highly customised ortho-K lenses can be<br />
used to remodel the irregularity and improve<br />
vision. A patient of mine in his mid-50’s had<br />
myopic LASIK done over a decade before but<br />
had developed severe post-LASIK ectasia in his<br />
right eye and moderate ectasia in his left eye<br />
since then. The better left eye had a variation<br />
of 7D of axial power along the 150 meridian<br />
leading to unaided acuity of 6/12 and a<br />
refraction of -1.00DS (6/6 with aberrations).<br />
This gentleman was very keen to explore his<br />
ortho-K options and we settled on fitting only<br />
the left eye with a custom myopic ortho-K<br />
lens. This had an aspheric back optic zone with<br />
a diameter to match the treatment zone of his<br />
myopic LASIK (Fig 5.).<br />
In these cases, interpreting the axial<br />
difference map can require some thought.<br />
Rather than creating a uniform degree of<br />
refractive change in the form of a ‘bulls-eye’<br />
that we are used to with simple myopic<br />
ortho-K, instead we are trying to create a<br />
post-ortho-K cornea that is more regular.<br />
This will decrease the aberrations in the<br />
optical system. You will see in the axial<br />
difference map (Fig 6.) that the ortho-K lens<br />
has succeeded in steepening the flat section<br />
of the cornea at axis 150 and flattening<br />
the steep section opposite this. The patient<br />
was seeing 6/6 unaided with only a quarter<br />
diopter of residual cylinder when using his<br />
lens. He commented that the halos around<br />
streetlights were much reduced, although<br />
not completely eliminated. His main gripe<br />
was that we couldn’t do the same treatment<br />
on his severely ectatic right cornea due to<br />
its ‘munted’ irregularity! Patients with other<br />
forms of irregular corneae such as forme<br />
fruste keratoconus can also be treated with<br />
ortho-K lens in a similar way (often with an<br />
inferior ‘tuck’ quadrant specific design) as<br />
long as the practitioner is mindful to monitor<br />
the cornea at each aftercare for signs of<br />
progression or insult.<br />
These cases highlight how versatile the<br />
practice of orthokeratology is these days. No<br />
longer is it reserved for simple myopia and<br />
it can be a great problem-solver for those<br />
particular patients that are determined to be<br />
spectacle-free! It is encouraging to know that<br />
when my LASIK goes kaput (as it is bound to,<br />
given my eyes’ record to date) I will have ortho-K<br />
up my sleeve to restore my super-vision.<br />
Tune in next time as I regale you with a story<br />
about the night we invented a revolutionary<br />
contact lens at the pub, and how it did not turn<br />
out to be quite as ingenious as we expected... ▀<br />
1. Dirani M, Couper T, Yau J, Ang EK, Islam FM,<br />
Snibson GR, Vajpayee RB, Baird PN. Long-term<br />
refractive outcomes and stability after excimer laser<br />
surgery for myopia. J Cataract Refract Surg. 2010<br />
Oct;36(10):1709-17.<br />
2. Schmack I, Dawson DG, McCarey BE, Waring GO 3rd,<br />
Grossniklaus HE, Edelhauser HF. Cohesive tensile<br />
strength of human LASIK wounds with histologic,<br />
ultrastructural, and clinical correlations.J Refract<br />
Surg. 2005 Sep-Oct;21(5):433-45.<br />
3. Goodman RL, Johnson DA, Dillon H, Edelhauser HF,<br />
Waller SG. Laser in situ keratomileusis flap stability<br />
during simulated aircraft ejection in a rabbit model.<br />
Cornea. 2003 Mar;22(2):142-5.<br />
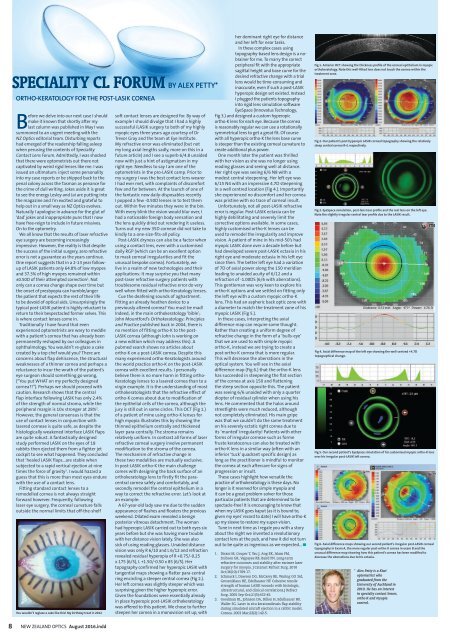
Fig 1. Anterior OCT showing the thickness profile of the corneal epithelium in myopic<br />
orthokeratology. Note this well-fitted lens does not touch the cornea within the<br />
treatment zone.<br />
Fig 2. Our patient’s post hyperopic LASIK corneal topography showing the relatively<br />
steep central cornea R+L respectively.<br />
Fig 3. EyeSpace simulation, post-lens tear profile and the real lens on the left eye.<br />
Note the slightly irregular central tear profile due to the LASIK result.<br />
Fig 4. Axial difference map of the left eye showing the well-centred +4.7D<br />
topographical change.<br />
Fig 5. Our second patient’s EyeSpace simulation of his customised myopic ortho-K lens<br />
over his irregular post-LASIK left cornea.<br />
Fig 6. Axial difference maps showing our second patient’s irregular post-LASIK corneal<br />
topography in Exam A, the more regular post-ortho-K cornea in exam B and the<br />
unusual difference map showing how this patient’s cornea has been modified to<br />
decrease the aberrations due to his ectasia.<br />
* Alex Petty is a Kiwi<br />
optometrist who<br />
graduated from the<br />
University of Auckland in<br />
2010. He has an interest<br />
in specialty contact lenses,<br />
ortho-K and myopia<br />
control.<br />
8 NEW ZEALAND OPTICS <strong>Aug</strong>ust <strong>2016</strong>.indd