Dental Asia July/August 2021
For more than two decades, Dental Asia is the premium journal in linking dental innovators and manufacturers to its rightful audience. We devote ourselves in showcasing the latest dental technology and share evidence-based clinical philosophies to serve as an educational platform to dental professionals. Our combined portfolio of print and digital media also allows us to reach a wider market and secure our position as the leading dental media in the Asia Pacific region while facilitating global interactions among our readers.
For more than two decades, Dental Asia is the premium journal in linking dental innovators and manufacturers to its rightful audience. We devote ourselves in showcasing the latest dental technology and share evidence-based clinical philosophies to serve as an educational platform to dental professionals. Our combined portfolio of print and digital media also allows us to reach a wider market and secure our position as the leading dental media in the Asia Pacific region while facilitating global interactions among our readers.
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
User Report<br />
Although mechanical and chemical<br />
indicators do not prove sterilisation has<br />
been achieved, they allow the detection<br />
of certain equipment malfunctions and<br />
identify procedural errors.<br />
Thus, it is recommended that sterilisers are<br />
monitored with spore tests at least weekly,<br />
and any load with an implantable device.<br />
She placed the spore test in the<br />
centre of an empty chamber per the<br />
manufacturer’s instructions and mailed<br />
it for processing.<br />
On Thursday, she received “immediate<br />
notification” from the sterilisation<br />
monitoring service that her spore test<br />
failed.<br />
Unfortunately, incidents such as this still<br />
exist but some measures can be taken to<br />
prevent such situations.<br />
This article will address quality assurance<br />
measures to ensure instrument sterility<br />
and instil a sense of calm and confidence<br />
as well as a culture of safety to dental<br />
personnel who reprocess instruments.<br />
While the combination of monitoring<br />
methods is intended to provide<br />
safeguards and ultimately ensure<br />
sterility, gaps in quality assurance do<br />
exist as demonstrated in the following<br />
case scenario.<br />
CASE SCENARIO<br />
Kim, an experienced dental assistant<br />
was a relatively new employee at a<br />
dental facility. She performed a spore<br />
test early Monday morning on an<br />
autoclave – a different brand from which<br />
she was trained.<br />
Recognising the implications, slight<br />
panic and a series of questions raced<br />
through her mind: “Why did it fail? What<br />
happened to the instruments that have<br />
been processed since the test, and have<br />
they been used for patient care? Could<br />
I identify unused packages, retrieve and<br />
reprocess them? Should the patients<br />
who may be impacted be notified? And,<br />
what should I do next?”<br />
Kim immediately reported this situation<br />
to her infection control coordinator and<br />
the owner/dentist.<br />
“IMMEDIATE NOTIFICATION” MAY<br />
NOT BE SOON ENOUGH<br />
In the scenario above, over three days<br />
of patient care had been performed<br />
utilising numerous instrument packages.<br />
There is a possibility that the autoclave<br />
had been malfunctioning for the entire<br />
three days (or more), or that this was an<br />
isolated cycle-failure incident.<br />
Potentially, one or more patients over the<br />
course of the three days, may have been<br />
treated with instrumentation that failed<br />
a spore test.<br />
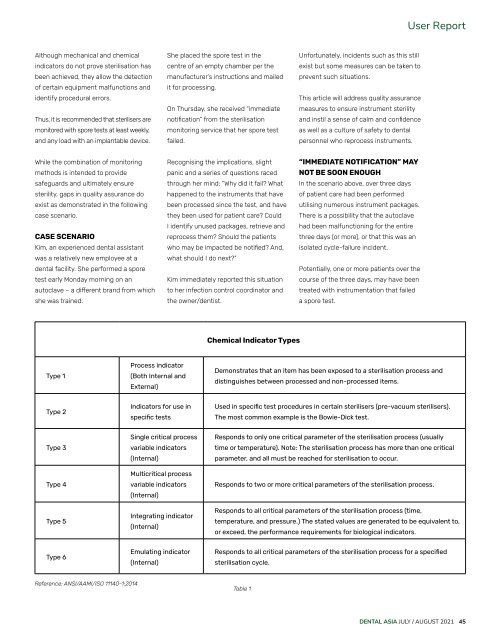
Chemical Indicator Types<br />
Type 1<br />
Process indicator<br />
(Both Internal and<br />
External)<br />
Demonstrates that an item has been exposed to a sterilisation process and<br />
distinguishes between processed and non-processed items.<br />
Type 2<br />
Indicators for use in<br />
specific tests<br />
Used in specific test procedures in certain sterilisers (pre-vacuum sterilisers).<br />
The most common example is the Bowie-Dick test.<br />
Type 3<br />
Type 4<br />
Type 5<br />
Single critical process<br />
variable indicators<br />
(Internal)<br />
Multicritical process<br />
variable indicators<br />
(Internal)<br />
Integrating indicator<br />
(Internal)<br />
Responds to only one critical parameter of the sterilisation process (usually<br />
time or temperature). Note: The sterilisation process has more than one critical<br />
parameter, and all must be reached for sterilisation to occur.<br />
Responds to two or more critical parameters of the sterilisation process.<br />
Responds to all critical parameters of the sterilisation process (time,<br />
temperature, and pressure.) The stated values are generated to be equivalent to,<br />
or exceed, the performance requirements for biological indicators.<br />
Type 6<br />
Emulating indicator<br />
(Internal)<br />
Responds to all critical parameters of the sterilisation process for a specified<br />
sterilisation cycle.<br />
Reference: ANSI/AAMI/ISO 11140-1:2014<br />
Table 1<br />
DENTAL ASIA JULY / AUGUST <strong>2021</strong> 45