changing the course of stroke - New Jersey Medical School ...
changing the course of stroke - New Jersey Medical School ...
changing the course of stroke - New Jersey Medical School ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
nothing short <strong>of</strong> a miracle. One <strong>of</strong> Chu’s patients—an engineer<br />
whose entire body was burned in a chemical accident—had visited<br />
many ophthalmologists over a period <strong>of</strong> years, but was told<br />
nothing could be done to restore his sight. His left eye was completely<br />
scarred, and <strong>the</strong> only thing he could see was if <strong>the</strong> light<br />
was on or <strong>of</strong>f. With a limbal cell transplant (cells were donated<br />
by his daughter, who is in her 20s) combined with <strong>the</strong> amniotic<br />
membrane transplant, <strong>the</strong> patient’s vision in <strong>the</strong> left eye was<br />
restored to 20/50, and he is now undergoing plastic surgery.<br />
Chu, also a member <strong>of</strong> <strong>the</strong> department’s Section <strong>of</strong> Corneal<br />
Wound Healing and Ocular Immunology, has been trained in<br />
<strong>the</strong> use <strong>of</strong> chemo<strong>the</strong>rapy for suppression <strong>of</strong> <strong>the</strong> immune system<br />
and frequently treats manifestations <strong>of</strong> autoimmune diseases—<br />
such as lupus, Crohn’s disease, pemphagoid, and rheumatoid<br />
arthritis—on <strong>the</strong> cornea and o<strong>the</strong>r visible portions <strong>of</strong> <strong>the</strong> eye.<br />
Administering chemo<strong>the</strong>rapy, such as cytoxan and methotrexate,<br />
for <strong>the</strong>se conditions is not mainstream ophthalmology, he<br />
says, but can save sight.<br />
Inventors at Work<br />
Glaucoma can generally be remedied with drugs that<br />
ei<strong>the</strong>r decrease <strong>the</strong> amount <strong>of</strong> fluid in <strong>the</strong> eye or<br />
increase <strong>the</strong> amount <strong>of</strong> fluid flowing out <strong>of</strong> <strong>the</strong> eye. In<br />
both cases, <strong>the</strong> aim is to reduce fluid pressure build-up, which<br />
can damage <strong>the</strong> optic nerve. When drug <strong>the</strong>rapy doesn’t do <strong>the</strong><br />
Eye diagram (right).<br />
20<br />
PULSE SPRING 2003<br />
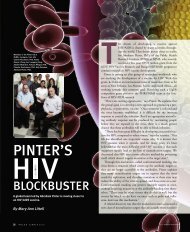
Proliferative retinopathy, an<br />
advanced form <strong>of</strong> diabetic retinopathy,<br />
occurs when abnormal new blood<br />
vessels and scar tissue form on <strong>the</strong><br />
surface <strong>of</strong> <strong>the</strong> retina (left).<br />
trick, lasers are <strong>of</strong>ten used to improve drainage and lower<br />
pressure.<br />
What happens when <strong>the</strong> usual methods don’t work?<br />
According to glaucoma specialist Robert D. Fechtner, MD, 50<br />
percent <strong>of</strong> glaucoma surgeries fail within five years. That has<br />
been his incentive to explore a better way.<br />
Just this past fall, he pulled <strong>of</strong>f a first in this part <strong>of</strong> <strong>the</strong> world.<br />
A young deaf woman was losing her sight to glaucoma and was<br />
not responsive to <strong>the</strong> standard <strong>the</strong>rapies. Using a 2 ml metal<br />
tube fashioned by an Israeli company that manufactures cardiac<br />
stents, he implanted <strong>the</strong> “drain” into her eye employing a needle.<br />
The tube passes from <strong>the</strong> front <strong>of</strong> <strong>the</strong> eye (<strong>the</strong> anterior<br />
chamber) into <strong>the</strong> space between <strong>the</strong> eyeball and <strong>the</strong> skin-like<br />
covering <strong>of</strong> <strong>the</strong> eye (<strong>the</strong> subconjunctival space). The excess fluid<br />
in <strong>the</strong> eye flows out through <strong>the</strong> miniature tube, lessening pressure.<br />
The young woman’s vision has been restored and <strong>the</strong> outlook<br />
is very promising.<br />
Fechtner enjoys wrestling with <strong>the</strong> unusual problems. He is<br />
part <strong>of</strong> an inventors’ alliance, which includes optical technology<br />
specialists Richard Greene, MD, PhD, and Gordon A.<br />
Thomas, PhD, both at NJIT. Their immediate aim is to devise<br />
a means for diabetics to test blood sugar without piercing <strong>the</strong>ir<br />
skin. The team’s concept involves a small device—to be integrated<br />
into an eyeglass lens—that uses a type <strong>of</strong> laser light that<br />
will change color when it hits glucose molecules in <strong>the</strong> aqueous<br />
portion <strong>of</strong> <strong>the</strong> eye. The device will function as an artificial pancreas,<br />
taking constant readings <strong>of</strong> <strong>the</strong> patient’s glucose levels in<br />
<strong>the</strong> aqueous humour, and triggering insulin release from a<br />
pump as needed. The work is underwritten by a grant from <strong>the</strong><br />
Pfeiffer Research Foundation.<br />
The team also has a $296,362 grant from <strong>the</strong> National<br />
<strong>Medical</strong> Technology Test Bed to develop two devices to improve<br />
glaucoma monitoring. The “self-tonometer” uses a technology<br />
called piezo-spectroscopy to allow glaucoma patients to measure<br />
<strong>the</strong>ir own intra-ocular pressure (IOP) by touching <strong>the</strong> device to<br />
<strong>the</strong>ir eyelids. Currently glaucoma patients have <strong>the</strong>ir pressure<br />
measured three to four times yearly by an ophthalmologist.<br />
More frequent readings will mean less damage to <strong>the</strong> optic<br />
nerve should <strong>the</strong>re be a rise in intra-ocular pressure. Patients<br />
will be instructed to call <strong>the</strong>ir physician if <strong>the</strong>ir IOP rises.<br />
The second device looks and functions like a miniaturized<br />
movie camera. For use by physicians, it records “moving pictures”<br />
<strong>of</strong> <strong>the</strong> inside <strong>of</strong> <strong>the</strong> eye, zooming in on areas <strong>of</strong> <strong>the</strong> retina<br />
damaged by obstructed blood flow. The “retinal mapper”<br />
also records changes in <strong>the</strong> color <strong>of</strong> <strong>the</strong> retina, an early indication<br />
<strong>of</strong> glaucoma and o<strong>the</strong>r eye diseases. In addition, it will cor-<br />
NATIONAL EYE INSTITUTE, NIH