changing the course of stroke - New Jersey Medical School ...
changing the course of stroke - New Jersey Medical School ...
changing the course of stroke - New Jersey Medical School ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Treating Complex<br />
Head and Neck Malignancies<br />
H<br />
ead and neck malignancies,<br />
including those found in <strong>the</strong><br />
voice box, throat, mouth, salivary<br />
glands and sinuses, account for<br />
about 5 percent <strong>of</strong> all cancers. However,<br />
at University Hospital (UH), head and<br />
neck malignancies total about 15 to 17<br />
percent <strong>of</strong> all cancers treated.<br />
What brings <strong>the</strong>se patients to <strong>New</strong>ark<br />
is a multidisciplinary program led by<br />
Soly Baredes, MD, chief <strong>of</strong> <strong>the</strong> division<br />
<strong>of</strong> otolaryngology-head and neck surgery<br />
and associate pr<strong>of</strong>essor <strong>of</strong> surgery at<br />
<strong>New</strong> <strong>Jersey</strong> <strong>Medical</strong> <strong>School</strong>. “Head and<br />
neck tumors can be difficult to manage<br />
in a community setting because <strong>of</strong> <strong>the</strong><br />
complexity <strong>of</strong> treatment,” says Baredes.<br />
For example, tumors at <strong>the</strong> base <strong>of</strong> <strong>the</strong><br />
skull require <strong>the</strong> skills <strong>of</strong> a neurosurgeon,<br />
ophthalmologist and plastic surgeon<br />
as well as an otolaryngologist.<br />
O<strong>the</strong>r head and neck malignancies may<br />
need treatment by oral and maxill<strong>of</strong>acial<br />
surgeons as well.<br />
Baredes says <strong>the</strong> collaboration among<br />
surgeons makes UH’s program unique<br />
in <strong>New</strong> <strong>Jersey</strong>. “For example, our skull<br />
base team includes a neurosurgeon,<br />
ophthalmologist and otolaryngologist,”<br />
he explains. “We collaborate on complex<br />
tumors that cross <strong>the</strong> barriers between<br />
<strong>the</strong> nasal cavities, sinuses, and <strong>the</strong><br />
brain.” UH is <strong>the</strong> only facility in <strong>the</strong><br />
state, and one <strong>of</strong> a few in <strong>the</strong> U.S., with<br />
intraoperative MRI technology, pioneered<br />
here by neurosurgeon Michael<br />
Schulder, MD. It allows surgeons to<br />
pinpoint <strong>the</strong> tumor location and remove<br />
it with minimal damage to surrounding<br />
tissue. Ano<strong>the</strong>r special feature <strong>of</strong> <strong>the</strong><br />
program is interventional radiology.<br />
Preoperative embolization <strong>of</strong> tumors<br />
decreases blood loss during surgery to<br />
remove lesions.<br />
A cornerstone <strong>of</strong> <strong>the</strong> program are <strong>the</strong><br />
weekly head and neck tumor confer-<br />
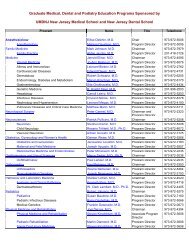
Left and above: The CT scan pictured<br />
is that <strong>of</strong> a parotid tumor.<br />
Below: Soly Baredes, MD, examining<br />
a patient<br />
ences, which are attended by representatives<br />
<strong>of</strong> <strong>the</strong> many specialties on <strong>the</strong><br />
interdisciplinary team. (In addition to<br />
those listed above, <strong>the</strong>se also include<br />
medical and radiation oncologists,<br />
pathologists, head and neck radiologists,<br />
and specialized nursing staff.)<br />
The Head and Neck Cancer Resource<br />
Center at UH, funded by a grant from<br />
<strong>the</strong> HealthCare Foundation <strong>of</strong> <strong>New</strong><br />
<strong>Jersey</strong>, provides patients and <strong>the</strong>ir families<br />
with a variety <strong>of</strong> rehabilitative services.<br />
“This type <strong>of</strong> surgery affects basic<br />
survival skills, such as <strong>the</strong> ability to eat,<br />
brea<strong>the</strong> and communicate,” says<br />
advanced practice nurse Ray Scarpa,<br />
MA, CNS, AOCN. “Some 40 to 60<br />
percent <strong>of</strong> patients may have tracheostomies,<br />
and many also have laryngectomies.”<br />
The Center staff, which<br />
includes four advance practice nurses,<br />
helps with <strong>the</strong> physical management <strong>of</strong><br />
supplemental devices, from feeding<br />
tubes to breathing aids. ●<br />
PETER BYRON NEW JERSEY MEDICAL SCHOOL 5