ESC Guidelines on the diagnosis and treatment of peripheral artery ...
ESC Guidelines on the diagnosis and treatment of peripheral artery ...
ESC Guidelines on the diagnosis and treatment of peripheral artery ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Page 40 <strong>of</strong> 56<br />
identified four independent risk factors for carotid stenosis in c<strong>and</strong>idates<br />
for CABG: age .70 years, neck bruit, history <strong>of</strong> cerebrovascular<br />
disease, <strong>and</strong> presence <strong>of</strong> clinical or subclinical LEAD. In a<br />
prospective assessment, <strong>the</strong>y found that performing DUS scanning<br />
<strong>on</strong>ly in patients with at least <strong>on</strong>e <strong>of</strong> <strong>the</strong>se risk factors detected<br />
100% <strong>of</strong> those with a carotid stenosis .70%, <strong>and</strong> decreased <strong>the</strong><br />
number <strong>of</strong> useless scans by 40%. This approach does, however,<br />
need validati<strong>on</strong> in a multicentre study.<br />
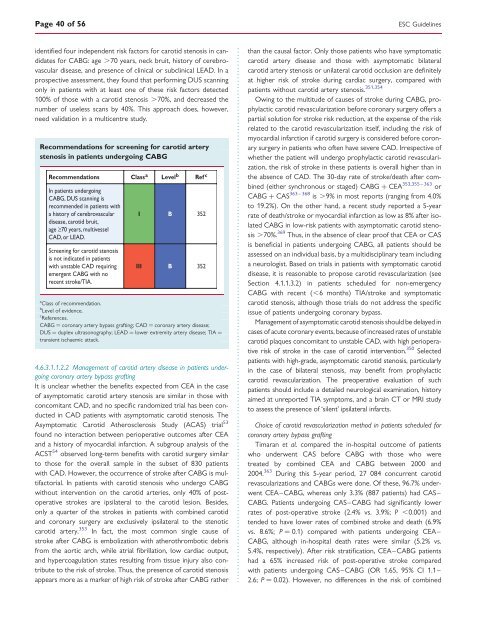
Recommendati<strong>on</strong>s for screening for carotid <strong>artery</strong><br />
stenosis in patients undergoing CABG<br />
Recommendati<strong>on</strong>s Class a Level b Ref c<br />
In patients undergoing<br />
CABG, DUS scanning is<br />
recommended in patients with<br />
a history <strong>of</strong> cerebrovascular<br />
disease, carotid bruit,<br />
age ≥70 years, multivessel<br />
CAD, or LEAD.<br />
Screening for carotid stenosis<br />
is not indicated in patients<br />
with unstable CAD requiring<br />
emergent CABG with no<br />
recent stroke/TIA.<br />
I B 352<br />
III B 352<br />
a<br />
Class <strong>of</strong> recommendati<strong>on</strong>.<br />
b<br />
Level <strong>of</strong> evidence.<br />
c<br />
References.<br />
CABG ¼ cor<strong>on</strong>ary <strong>artery</strong> bypass grafting; CAD ¼ cor<strong>on</strong>ary <strong>artery</strong> disease;<br />
DUS ¼ duplex ultras<strong>on</strong>ography; LEAD ¼ lower extremity <strong>artery</strong> disease; TIA ¼<br />
transient ischaemic attack.<br />
4.6.3.1.1.2.2 Management <strong>of</strong> carotid <strong>artery</strong> disease in patients undergoing<br />
cor<strong>on</strong>ary <strong>artery</strong> bypass grafting<br />
It is unclear whe<strong>the</strong>r <strong>the</strong> benefits expected from CEA in <strong>the</strong> case<br />
<strong>of</strong> asymptomatic carotid <strong>artery</strong> stenosis are similar in those with<br />
c<strong>on</strong>comitant CAD, <strong>and</strong> no specific r<strong>and</strong>omized trial has been c<strong>on</strong>ducted<br />
in CAD patients with asymptomatic carotid stenosis. The<br />
Asymptomatic Carotid A<strong>the</strong>rosclerosis Study (ACAS) trial 53<br />
found no interacti<strong>on</strong> between perioperative outcomes after CEA<br />
<strong>and</strong> a history <strong>of</strong> myocardial infarcti<strong>on</strong>. A subgroup analysis <strong>of</strong> <strong>the</strong><br />
ACST 54 observed l<strong>on</strong>g-term benefits with carotid surgery similar<br />
to those for <strong>the</strong> overall sample in <strong>the</strong> subset <strong>of</strong> 830 patients<br />
with CAD. However, <strong>the</strong> occurrence <strong>of</strong> stroke after CABG is multifactorial.<br />
In patients with carotid stenosis who undergo CABG<br />
without interventi<strong>on</strong> <strong>on</strong> <strong>the</strong> carotid arteries, <strong>on</strong>ly 40% <strong>of</strong> postoperative<br />
strokes are ipsilateral to <strong>the</strong> carotid lesi<strong>on</strong>. Besides,<br />
<strong>on</strong>ly a quarter <strong>of</strong> <strong>the</strong> strokes in patients with combined carotid<br />
<strong>and</strong> cor<strong>on</strong>ary surgery are exclusively ipsilateral to <strong>the</strong> stenotic<br />
carotid <strong>artery</strong>. 353 In fact, <strong>the</strong> most comm<strong>on</strong> single cause <strong>of</strong><br />
stroke after CABG is embolizati<strong>on</strong> with a<strong>the</strong>rothrombotic debris<br />
from <strong>the</strong> aortic arch, while atrial fibrillati<strong>on</strong>, low cardiac output,<br />
<strong>and</strong> hypercoagulati<strong>on</strong> states resulting from tissue injury also c<strong>on</strong>tribute<br />
to <strong>the</strong> risk <strong>of</strong> stroke. Thus, <strong>the</strong> presence <strong>of</strong> carotid stenosis<br />
appears more as a marker <strong>of</strong> high risk <strong>of</strong> stroke after CABG ra<strong>the</strong>r<br />
<str<strong>on</strong>g>ESC</str<strong>on</strong>g> <str<strong>on</strong>g>Guidelines</str<strong>on</strong>g><br />
than <strong>the</strong> causal factor. Only those patients who have symptomatic<br />
carotid <strong>artery</strong> disease <strong>and</strong> those with asymptomatic bilateral<br />
carotid <strong>artery</strong> stenosis or unilateral carotid occlusi<strong>on</strong> are definitely<br />
at higher risk <strong>of</strong> stroke during cardiac surgery, compared with<br />
patients without carotid <strong>artery</strong> stenosis. 351,354<br />
Owing to <strong>the</strong> multitude <strong>of</strong> causes <strong>of</strong> stroke during CABG, prophylactic<br />
carotid revascularizati<strong>on</strong> before cor<strong>on</strong>ary surgery <strong>of</strong>fers a<br />
partial soluti<strong>on</strong> for stroke risk reducti<strong>on</strong>, at <strong>the</strong> expense <strong>of</strong> <strong>the</strong> risk<br />
related to <strong>the</strong> carotid revascularizati<strong>on</strong> itself, including <strong>the</strong> risk <strong>of</strong><br />
myocardial infarcti<strong>on</strong> if carotid surgery is c<strong>on</strong>sidered before cor<strong>on</strong>ary<br />
surgery in patients who <strong>of</strong>ten have severe CAD. Irrespective <strong>of</strong><br />
whe<strong>the</strong>r <strong>the</strong> patient will undergo prophylactic carotid revascularizati<strong>on</strong>,<br />
<strong>the</strong> risk <strong>of</strong> stroke in <strong>the</strong>se patients is overall higher than in<br />
<strong>the</strong> absence <strong>of</strong> CAD. The 30-day rate <strong>of</strong> stroke/death after combined<br />
(ei<strong>the</strong>r synchr<strong>on</strong>ous or staged) CABG + CEA 353,355 – 363 or<br />
CABG + CAS 363 – 368 is .9% in most reports (ranging from 4.0%<br />
to 19.2%). On <strong>the</strong> o<strong>the</strong>r h<strong>and</strong>, a recent study reported a 5-year<br />
rate <strong>of</strong> death/stroke or myocardial infarcti<strong>on</strong> as low as 8% after isolated<br />
CABG in low-risk patients with asymptomatic carotid stenosis<br />
.70%. 369 Thus, in <strong>the</strong> absence <strong>of</strong> clear pro<strong>of</strong> that CEA or CAS<br />
is beneficial in patients undergoing CABG, all patients should be<br />
assessed <strong>on</strong> an individual basis, by a multidisciplinary team including<br />
a neurologist. Based <strong>on</strong> trials in patients with symptomatic carotid<br />
disease, it is reas<strong>on</strong>able to propose carotid revascularizati<strong>on</strong> (see<br />
Secti<strong>on</strong> 4.1.1.3.2) in patients scheduled for n<strong>on</strong>-emergency<br />
CABG with recent (,6 m<strong>on</strong>ths) TIA/stroke <strong>and</strong> symptomatic<br />
carotid stenosis, although those trials do not address <strong>the</strong> specific<br />
issue <strong>of</strong> patients undergoing cor<strong>on</strong>ary bypass.<br />
Management <strong>of</strong> asymptomatic carotid stenosis should be delayed in<br />
cases <strong>of</strong> acute cor<strong>on</strong>ary events, because <strong>of</strong> increased rates <strong>of</strong> unstable<br />
carotid plaques c<strong>on</strong>comitant to unstable CAD, with high perioperative<br />
risk <strong>of</strong> stroke in <strong>the</strong> case <strong>of</strong> carotid interventi<strong>on</strong>. 350 Selected<br />
patients with high-grade, asymptomatic carotid stenosis, particularly<br />
in <strong>the</strong> case <strong>of</strong> bilateral stenosis, may benefit from prophylactic<br />
carotid revascularizati<strong>on</strong>. The preoperative evaluati<strong>on</strong> <strong>of</strong> such<br />
patients should include a detailed neurological examinati<strong>on</strong>, history<br />
aimed at unreported TIA symptoms, <strong>and</strong> a brain CT or MRI study<br />
to assess <strong>the</strong> presence <strong>of</strong> ‘silent’ ipsilateral infarcts.<br />
Choice <strong>of</strong> carotid revascularizati<strong>on</strong> method in patients scheduled for<br />
cor<strong>on</strong>ary <strong>artery</strong> bypass grafting<br />
Timaran et al. compared <strong>the</strong> in-hospital outcome <strong>of</strong> patients<br />
who underwent CAS before CABG with those who were<br />
treated by combined CEA <strong>and</strong> CABG between 2000 <strong>and</strong><br />
2004. 363 During this 5-year period, 27 084 c<strong>on</strong>current carotid<br />
revascularizati<strong>on</strong>s <strong>and</strong> CABGs were d<strong>on</strong>e. Of <strong>the</strong>se, 96.7% underwent<br />
CEA–CABG, whereas <strong>on</strong>ly 3.3% (887 patients) had CAS–<br />
CABG. Patients undergoing CAS–CABG had significantly lower<br />
rates <strong>of</strong> post-operative stroke (2.4% vs. 3.9%; P ,0.001) <strong>and</strong><br />
tended to have lower rates <strong>of</strong> combined stroke <strong>and</strong> death (6.9%<br />
vs. 8.6%; P ¼ 0.1) compared with patients undergoing CEA–<br />
CABG, although in-hospital death rates were similar (5.2% vs.<br />
5.4%, respectively). After risk stratificati<strong>on</strong>, CEA–CABG patients<br />
had a 65% increased risk <strong>of</strong> post-operative stroke compared<br />
with patients undergoing CAS–CABG (OR 1.65, 95% CI 1.1–<br />
2.6; P ¼ 0.02). However, no differences in <strong>the</strong> risk <strong>of</strong> combined