VCP 2010 Application of TEG/TEM to veterinary - UC Davis School ...
VCP 2010 Application of TEG/TEM to veterinary - UC Davis School ...
VCP 2010 Application of TEG/TEM to veterinary - UC Davis School ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
INVITED REVIEW<br />
<strong>Application</strong> <strong>of</strong> thrombelas<strong>to</strong>graphy/thromboelas<strong>to</strong>metry <strong>to</strong><br />
<strong>veterinary</strong> medicine<br />
Amir Kol 1 , Dori L. Borjesson 2<br />
1 Veterinary Medical Teaching Hospital and 2 Department <strong>of</strong> Pathology, Microbiology and Immunology, <strong>School</strong> <strong>of</strong> Veterinary Medicine,<br />
University <strong>of</strong> California–<strong>Davis</strong>, <strong>Davis</strong>, CA, USA<br />
Key Words<br />
Coagulation, hemostasis, hypercoagulability,<br />
hypocoagulability, <strong>TEG</strong><br />
Correspondence<br />
Dr. Amir Kol, Veterinary Medical Teaching<br />
Hospital, <strong>School</strong> <strong>of</strong> Veterinary Medicine,<br />
University <strong>of</strong> California–<strong>Davis</strong>, One Shields<br />
Avenue, <strong>Davis</strong>, CA 95616, USA<br />
E-mail: akol@ucdavis.edu<br />
DOI:10.1111/j.1939-165X.<strong>2010</strong>.00263.x<br />
I. Introduction<br />
II. Blood Samples and Instrumentation<br />
III. Terminology<br />
IV. <strong>TEG</strong> Variables and Correlation with Routine Coagulation Assays<br />
V. Validation Studies and Preanalytical Fac<strong>to</strong>rs<br />
VI. Clinical <strong>Application</strong>s in Veterinary Medicine<br />
A. Hypercoagulable states<br />
B. Hypocoagulable states<br />
C. Moni<strong>to</strong>ring anticoagulant therapy<br />
D. Platelet function<br />
VII. Summary<br />
Introduction<br />
Hemostasis is a complex physiologic process in which<br />
blood vessels, blood cells, and soluble fac<strong>to</strong>rs in plasma<br />
interact in order <strong>to</strong> prevent hemorrhage and thrombosis.<br />
In 1856, the physician Rudolf Virchow suggested<br />
that altered blood flow, endothelial injury, and hypercoagulability<br />
contribute <strong>to</strong> the development <strong>of</strong><br />
venous thrombosis (VT). These fac<strong>to</strong>rs are known as<br />
Virchow’s triad and are still considered the basic<br />
Veterinary Clinical Pathology ISSN 0275-6382<br />
Abstract: Thrombelas<strong>to</strong>graph analyzers are point-<strong>of</strong>-care hemostatic<br />
analyzers that provide global assessment <strong>of</strong> the hemostatic process. Thrombelas<strong>to</strong>graphy<br />
(<strong>TEG</strong>) detects and provides a continuous recording <strong>of</strong> the<br />
changes in the viscoelastic properties <strong>of</strong> whole blood from initial clot<br />
formation through fibinolysis. <strong>TEG</strong> has been validated for use in dogs, horses,<br />
and cats. Hemostasis research using <strong>TEG</strong> has focused on test validation, alterations<br />
<strong>of</strong> <strong>TEG</strong> tracings in animals with naturally occurring diseases, and the<br />
use <strong>of</strong> <strong>TEG</strong> for moni<strong>to</strong>ring various therapeutic modalities. This article reviews<br />
<strong>TEG</strong> methodology and terminology, including potential sources <strong>of</strong> preanalytical<br />
and analytical errors, the correlation between <strong>TEG</strong> and other routine<br />
hemostatic assays, and current clinical applications <strong>of</strong> <strong>TEG</strong>, with emphasis on<br />
<strong>veterinary</strong> medical practice. Data suggest that <strong>TEG</strong> may be a sensitive and<br />
useful adjunctive <strong>to</strong>ol for evaluating an animal with an underlying coagulopathy,<br />
including hypercoagulability and hypocoagulability. Additional<br />
prospective studies are needed <strong>to</strong> (1) correlate <strong>TEG</strong> tracing patterns with a<br />
clinical predisposition for bleeding or thrombosis in various disease states and<br />
(2) determine whether moni<strong>to</strong>ring and treating hemostatic disorders based<br />
on <strong>TEG</strong> tracings improve clinical outcome.<br />
underlying mechanisms <strong>of</strong> thrombosis <strong>to</strong>day.<br />
Thrombelas<strong>to</strong>graphy (<strong>TEG</strong>) is an in vitro diagnostic<br />
technique initially introduced in Germany in the late<br />
1940s by Hartert. 1,2 <strong>TEG</strong> integrates the cellular and<br />
soluble components <strong>of</strong> the hemostatic process <strong>to</strong> yield<br />
a global assessment <strong>of</strong> hemostasis. The technique is<br />
based on a continuous detection and recording <strong>of</strong><br />
changes in the viscoelastic properties <strong>of</strong> whole blood<br />
while it clots. <strong>TEG</strong> tracings may better reflect the cellbased<br />
model <strong>of</strong> hemostasis 3 and thus better predict the<br />
kinetics <strong>of</strong> coagulation compared with routine plasmabased<br />
assays. Routine coagulation assays are limited in<br />
their capacity <strong>to</strong> predict hemorrhage or thrombosis,<br />
especially in patients who undergo invasive diagnostic<br />
and therapeutic procedures. The increased use and interest<br />
in <strong>TEG</strong> in <strong>veterinary</strong> medicine is based on the<br />
potential for <strong>TEG</strong> results <strong>to</strong> better predict thrombotic as<br />
well as hemorrhagic events in the clinical setting. 4,5<br />
The terms thrombelas<strong>to</strong>graphy, thrombelas<strong>to</strong>graph,<br />
and <strong>TEG</strong> were used generically in the scientific<br />
literature until 1996. At that time, Haemoscope Corporation<br />
(Niles, IL, USA) named its thrombelas<strong>to</strong>graph<br />
Vet Clin Pathol 39/4 (<strong>2010</strong>) 405–416 c <strong>2010</strong> American Society for Veterinary Clinical Pathology 405
<strong>Application</strong> <strong>of</strong> <strong>TEG</strong> <strong>to</strong> <strong>veterinary</strong> medicine<br />
analyzer ‘‘<strong>TEG</strong>,’’ which became a registered trademark<br />
<strong>of</strong> the company. Later, a second analyzer, rotational<br />
thromboelas<strong>to</strong>metry (RO<strong>TEM</strong>), became available (Pentapharm<br />
GmbH, Munich, Germany). The RO<strong>TEM</strong> analyzer<br />
is currently used primarily in Europe and has<br />
recently been approved by the US Food and Drug Administration<br />
for clinical use in the United States. 6 Comparison<br />
<strong>of</strong> <strong>TEG</strong> and RO<strong>TEM</strong> analyzers is beyond the<br />
scope <strong>of</strong> this review and for a more in-depth comparison<br />
the reader is referred elsewhere. 7,8 For the purpose<br />
<strong>of</strong> this article, ‘‘<strong>TEG</strong>’’ will be used generically, and the<br />
terms ‘‘Haemoscope <strong>TEG</strong>’’ or ‘‘RO<strong>TEM</strong>’’ will be used<br />
when referring <strong>to</strong> specific analyzers.<br />
<strong>TEG</strong> was originally designed <strong>to</strong> be a bed-side point<strong>of</strong>-care<br />
analyzer that utilized whole nonanticoagulated<br />
blood. However, recent advances, including the use <strong>of</strong><br />
anticoagulated blood and a variety <strong>of</strong> coagulation activa<strong>to</strong>rs<br />
and specific inhibi<strong>to</strong>rs, have allowed <strong>TEG</strong> instrumentation<br />
<strong>to</strong> be utilized by diagnostic labora<strong>to</strong>ries as<br />
well. 8 Since the 1980s, <strong>TEG</strong> has been widely used in clinical<br />
settings in human medicine, especially during liver<br />
transplantation and cardiac surgery. <strong>TEG</strong> results guide<br />
administration <strong>of</strong> blood products and anticoagulants and<br />
predict hemorrhage during surgery and pos<strong>to</strong>peratively.<br />
9,10 In <strong>veterinary</strong> medicine, <strong>TEG</strong> and RO<strong>TEM</strong> have<br />
been validated for use in dogs, horses, and cats. 11–17<br />
The objectives <strong>of</strong> this review are <strong>to</strong> introduce <strong>TEG</strong><br />
technique, including its strengths and limitations,<br />
highlight important preanalytical fac<strong>to</strong>rs and quality<br />
control checkpoints that affect <strong>TEG</strong> results, review<br />
published data regarding clinical applications <strong>of</strong> <strong>TEG</strong><br />
in human and <strong>veterinary</strong> medicine, and discuss potential<br />
future applications <strong>of</strong> this technique.<br />
Blood Samples and Instrumentation<br />
Blood should be collected atraumatically in<strong>to</strong> sodium citrate<br />
(3.2% or 3.8%) anticoagulant. <strong>TEG</strong> pro<strong>to</strong>cols using<br />
anticoagulated citrated blood <strong>to</strong> which various activa<strong>to</strong>rs<br />
are added have been validated for animals. The use <strong>of</strong><br />
whole nonanticoagulated blood or anticoagulated blood<br />
without activation (recalcified method) is impractical in<br />
the <strong>veterinary</strong> setting and likely leads <strong>to</strong> an unacceptably<br />
high degree <strong>of</strong> intraassay variation. 12,13,17 Various<br />
activa<strong>to</strong>rs and specific inhibi<strong>to</strong>rs are currently in use for<br />
<strong>TEG</strong> analysis. Standard reagents and products manufactured<br />
by Haemoscope Corporation for use with this<br />
company’s instrument are kaolin reagent, heparinasecoated<br />
cups for moni<strong>to</strong>ring heparin therapy, and a rapid<br />
<strong>TEG</strong> (r-<strong>TEG</strong>) reagent that includes a mixture <strong>of</strong> kaolin<br />
and tissue fac<strong>to</strong>r (TF). Additional nonstandardized activa<strong>to</strong>rs,<br />
including celite and recombinant human TF<br />
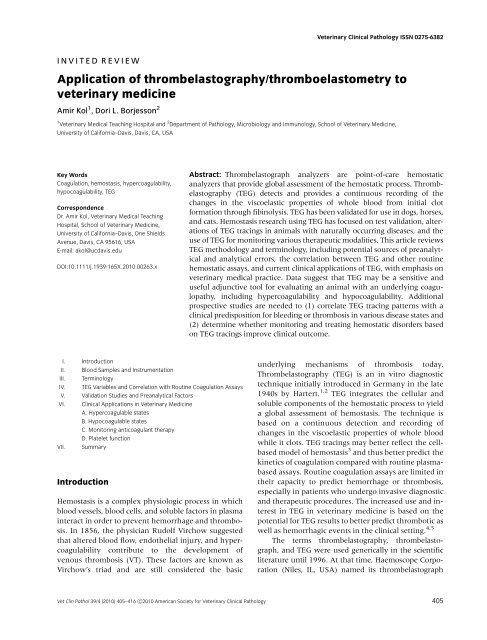
Figure 1. Haemoscope <strong>TEG</strong> analyzer with illustration <strong>of</strong> the composition<br />
<strong>of</strong> the cup, pin, and <strong>to</strong>rsion wire and their oscillation pattern. Blood in a<br />
volume <strong>of</strong> 360 mL is placed in a cup preheated <strong>to</strong> 371C. The activa<strong>to</strong>r and<br />
calcium are added; then the pin is immediately introduced in<strong>to</strong> the blood<br />
and oscillation begins. As a clot forms, the pin is engaged, represented<br />
by the ‘‘split point.’’ From this point on, 2 symmetrical branches are plotted<br />
(see Figure 2). Additional increases <strong>to</strong> the strength <strong>of</strong> the clot are indicated<br />
by increases in the tracing amplitude (graphic <strong>of</strong> the Haemoscope<br />
<strong>TEG</strong> thrombelas<strong>to</strong>graph components [cup, pin, and wire] is reprinted with<br />
permission <strong>of</strong> Haemonetics Corporation, Braintree, MA, USA).<br />
(rhTF), are also in use. 17–20 Reagents for the RO<strong>TEM</strong> include<br />
a TF activa<strong>to</strong>r, a contact activa<strong>to</strong>r, a reagent that<br />
includes TF and a platelet inhibi<strong>to</strong>r for qualitative assessment<br />
<strong>of</strong> fibrinogen, a TF and apro<strong>to</strong>nin mixture for<br />
detection <strong>of</strong> increased fibrinolysis, and a contact activa<strong>to</strong>r<br />
with heparinase for moni<strong>to</strong>ring heparin therapy. 21<br />
Recalcification serves as the set point from which coagulation<br />
is initiated and the tracing begins.<br />
The <strong>TEG</strong> instruments consist <strong>of</strong> a pin attached <strong>to</strong> a<br />
<strong>to</strong>rsion wire that is introduced in<strong>to</strong> a cup, preheated <strong>to</strong><br />
371C, containing a 360 mL aliquot <strong>of</strong> the blood sample<br />
(Figure 1). Movement is initiated by the cup (Haemoscope<br />
<strong>TEG</strong>) or the pin (RO<strong>TEM</strong>). As the blood<br />
clots, tension exerted on the wire is translated <strong>to</strong> an<br />
electrical signal that yields a graphic display, or tracing,<br />
in which the amplitude <strong>of</strong> the wire oscillation in millimeters<br />
is on the y-axis and the time in seconds is on<br />
the x-axis (Figure 2A). Amplitude is directly converted<br />
<strong>to</strong> physical units that represent the strength <strong>of</strong> the<br />
formed clot.<br />
Terminology<br />
Kol and Borjesson<br />
The <strong>TEG</strong> and RO<strong>TEM</strong> measure the same variables but<br />
utilize different terminology (Table 1). R or CT (clotting<br />
time) is the time in minutes from clot initiation until<br />
the first fibrin polymers are produced and the amplitude<br />
reaches 2 mm. K or CFT (clot formation time) is<br />
the time in minutes from the end <strong>of</strong> R until an amplitude<br />
<strong>of</strong> 20 mm is reached and represents the speed <strong>of</strong><br />
clot formation. Alpha (a) is the angle in degrees tangent<br />
<strong>to</strong> the curve as K is reached and represents the<br />
406 Vet Clin Pathol 39/4 (<strong>2010</strong>) 405–416 c <strong>2010</strong> American Society for Veterinary Clinical Pathology
Kol and Borjesson <strong>Application</strong> <strong>of</strong> <strong>TEG</strong> <strong>to</strong> <strong>veterinary</strong> medicine<br />
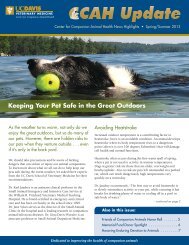
Figure 2. Haemoscope <strong>TEG</strong> tracings using canine kaolin-activated blood.<br />
(A) Normal tracing. The x-axis represents time in minutes (min) and the yaxis<br />
the amplitude <strong>of</strong> pin rotation in millimeters. The tracing is completely<br />
symmetrical relative <strong>to</strong> the horizontal midline. R and K are the times that<br />
it takes for the tracing <strong>to</strong> reach the amplitudes <strong>of</strong> 2 and 20 mm, respectively.<br />
Alpha (a) is the angle <strong>of</strong> the slope in degrees (deg), representing<br />
acceleration <strong>of</strong> clot formation, and MA is the maximal amplitude <strong>of</strong> the<br />
tracing, representing the maximal strength <strong>of</strong> the clot. MA may be modified<br />
<strong>to</strong> physical units (G; dyne-s/cm 2 ) as follows: G dyn=cm 2 = (5000 MA)/<br />
(100 MA). LY30, expressed as a percentage <strong>of</strong> MA, is the reduction in<br />
amplitude after 30 minutes and represents the percent <strong>of</strong> clot lysis. The<br />
result for each variable is found in row 3, and the reference intervals are<br />
in row 4. (B) Tracings indicating normocoagulable (green), hypocoagulable<br />
(blue), hypercoagulable (red), and secondary fibrinolytic (black)<br />
states. The result for each variable is found in rows 4–7, and the reference<br />
intervals are in row 3.<br />
acceleration/kinetics <strong>of</strong> fibrin formation and crosslinking.<br />
MA or MCF (maximal clot strength) is<br />
the maximum amplitude in millimeter and reflects<br />
maximal clot strength. G is the modification <strong>of</strong> MA<br />
<strong>to</strong> physical units. LY30/60 or CLI30/60 are the percent<br />
<strong>of</strong> clot lysis detected at 30 and 60 minutes, respectively,<br />
after MA is reached. A normal canine <strong>TEG</strong> tracing<br />
(Figure 2A) illustrates each variable, and examples<br />
<strong>of</strong> tracings that depict hypocoagulable, hypercoagulable,<br />
and secondary fibrinolytic states (Figure 2B) are<br />
provided.<br />
<strong>TEG</strong> Variables and Correlation with Routine<br />
Coagulation Assays<br />
Multiple studies have examined how the results <strong>of</strong><br />
<strong>TEG</strong> analysis correlate with standard coagulation assays.<br />
20,22–25 Traditionally, the R time (Figure 2A) has<br />
been associated with soluble clotting fac<strong>to</strong>r activity. 20<br />
K time and a angle (Figure 2A) are nonspecific and<br />
have been associated with platelet concentration and<br />
function, fibrinogen concentration and function, and<br />
clotting fac<strong>to</strong>rs activity. 20 The MA and G, a value calculated<br />
from MA and discussed <strong>to</strong>gether with MA,<br />
have been associated with platelet concentration and<br />
function and, <strong>to</strong> a lesser degree, with fibrinogen concentration.<br />
20 As <strong>TEG</strong> usage has increased, these previously<br />
ascribed correlations between <strong>TEG</strong> results and<br />
other hemostatic assay results (such as clotting fac<strong>to</strong>r<br />
activity and platelet concentration) have been modified.<br />
Although some studies have demonstrated a significant<br />
positive correlation between R time and<br />
prothrombin time (PT) or activated partial thromboplastin<br />
time (aPTT), these results could not be reproduced<br />
in other studies. 9,13,20,24–26 PT correlated with R<br />
time using rhTF-Haemoscope <strong>TEG</strong> in dogs admitted <strong>to</strong><br />
an intensive care unit (ICU) and in healthy horses 13,26 ;<br />
however, there was no correlation between R time and<br />
PT or aPTT in healthy people or in people with<br />
Table 1. Nomenclature <strong>of</strong> selected thrombelas<strong>to</strong>graphy (<strong>TEG</strong>) variables measured by the Haemoscope <strong>TEG</strong> and rotational thromboelas<strong>to</strong>metry<br />
(RO<strong>TEM</strong>) analyzers.<br />
Variable Units Haemoscope <strong>TEG</strong> RO<strong>TEM</strong><br />
Initiation time (time 0–2 mm amplitude) Minutes R CT (clot time)<br />
Clot kinetics (time 2–20 mm amplitude) Minutes K CFT (clot formation time)<br />
Clot kinetics (the slope between 2 and<br />
20 mm amplitude)<br />
Degrees a angle a angle<br />
Maximal clot strength and stability Millimeters MA (maximum amplitude) MCF (maximal clot strength)<br />
Maximal clot strength and stability Dynes/cm 2<br />
G —<br />
Clot lysis Percent LY30, LY60 CLI30, CLI60<br />
Vet Clin Pathol 39/4 (<strong>2010</strong>) 405–416 c <strong>2010</strong> American Society for Veterinary Clinical Pathology 407
<strong>Application</strong> <strong>of</strong> <strong>TEG</strong> <strong>to</strong> <strong>veterinary</strong> medicine<br />
malignancies when using native or celite-activated<br />
Haemoscope <strong>TEG</strong>. 20<br />
Fibrinogen concentration has been shown <strong>to</strong> be<br />
highly correlated with G/MA and K time. This has been<br />
demonstrated utilizing various activa<strong>to</strong>rs and methodologies,<br />
both in people and in various animals. 13,20,26–29<br />
In a group <strong>of</strong> human patients with solid tumors, hyperfibrinogenemia<br />
had a sensitivity and specificity <strong>of</strong><br />
86.5% and 83.3%, respectively, for a RO<strong>TEM</strong> tracing<br />
indicating hypercoagulability. 27 Hyperfibrinogenemia is<br />
likely an independent risk fac<strong>to</strong>r for both venous and<br />
arterial thrombosis. 30,31<br />
Platelet concentration also correlates with G/MA<br />
and K time in dogs and in people. 20,22,26,29 The correlation<br />
between platelet count and G/MA was stronger<br />
after application <strong>of</strong> a logarithmic transformation <strong>to</strong> the<br />
platelet concentration. 22,24 We and others have noted<br />
that platelet concentration correlates with G and MA<br />
when platelet concentration is within the reference<br />
interval or decreased; however, thrombocy<strong>to</strong>sis<br />
(4 400,000 platelets/mL) does not correlate with an<br />
increase in G and MA, 29 an observation consistent<br />
with the concept that whereas thrombocy<strong>to</strong>penia<br />
may contribute <strong>to</strong> a hemorrhagic phenotype, reactive<br />
thrombocy<strong>to</strong>sis is not associated with hypercoagulability.<br />
32,33<br />
In human medicine, there is an association between<br />
increased D-dimer concentration, fibrinogen/<br />
fibrin degradation products (FDPs), and increased<br />
<strong>TEG</strong> fibrinolytic variables (LY30 or CLI30; Table 1 and<br />
Figure 2B). 9,25,34 The <strong>TEG</strong> markers <strong>of</strong> hyperfibrinolysis<br />
may be superior <strong>to</strong> other labora<strong>to</strong>ry measurements<br />
in human trauma and liver transplantation settings.<br />
9,25,34,35 To date, establishing similar correlations<br />
in <strong>veterinary</strong> medicine has had little success. 29 In<br />
dogs with experimentally induced thrombus formation,<br />
there was good agreement between <strong>TEG</strong> fibrinolysis<br />
variables, FDPs, thrombus size, and local blood<br />
flow at the site <strong>of</strong> the thrombus after fibrinolytic<br />
therapy. 36 However, in a recent case series <strong>of</strong> dogs<br />
with disseminated intravascular coagulation (DIC)<br />
and subsequent secondary fibrinolysis, there was no<br />
association between D-dimer concentration and<br />
increased rhTF-Haemoscope <strong>TEG</strong> fibrinolytic variables.<br />
29 Similar results were reported in a study in<br />
which human patients with severe sepsis, with or<br />
without overt DIC, had increased D-dimer concentration<br />
with no concurrent increase in RO<strong>TEM</strong> fibrinolytic<br />
markers using TF activation. 37 The latter<br />
findings are compatible with our experience, in which<br />
D-dimer concentration correlated poorly with kaolinactivated<br />
Haemoscope <strong>TEG</strong> variable, LY30 (unpublished<br />
data).<br />
Kol and Borjesson<br />
Validation Studies and Preanalytical Fac<strong>to</strong>rs<br />
In <strong>veterinary</strong> and human medicine, validation studies<br />
have been conducted <strong>to</strong> better characterize and define<br />
preanalytical and analytic fac<strong>to</strong>rs that affect <strong>TEG</strong> variables.<br />
12–14,17,38–41 As with most hemostatic assays, preanalytical<br />
fac<strong>to</strong>rs, including the delay between blood<br />
collection and analysis and the sample temperature,<br />
are important in <strong>TEG</strong> analysis. Blood for <strong>TEG</strong> analysis<br />
should be collected using a standardized pro<strong>to</strong>col <strong>to</strong><br />
minimize preanalytical variation. In several studies, a<br />
clinically acceptable intraassay coefficient <strong>of</strong> variation<br />
(CV) for the various Haemoscope <strong>TEG</strong> variables in dogs<br />
has been reported and varies from 3% <strong>to</strong> 18% depending<br />
on the variable. 12,17 S<strong>to</strong>rage <strong>of</strong> blood for 120 minutes<br />
may result in a mild but significant trend <strong>to</strong>ward<br />
a tracing that indicates hypercoagulability. 17,41 In<br />
horses, acceptable intraassay CVs <strong>of</strong> 1–12%, depending<br />
on the variable, were found when using both<br />
the Haemoscope <strong>TEG</strong> and RO<strong>TEM</strong> analyzers, 13,14,16<br />
although effects on results were noted as soon as 60<br />
minutes after blood collection in one study. 14 Blood<br />
samples refrigerated at 41C had decreased a angle and<br />
prolonged CT but also increased MCF, changes that are<br />
consistent both with hypocoagulability and hypercoagulability,<br />
respectively. 16 These findings are consistent<br />
with those noted in human medicine. In human<br />
medical practice, 120 minutes is an acceptable period<br />
<strong>of</strong> time between blood collection and <strong>TEG</strong> analysis<br />
with all variables having clinically acceptable CVs using<br />
various activa<strong>to</strong>rs. 38–40 Variability in <strong>TEG</strong> results<br />
has also been attributed <strong>to</strong> differences between analyzers<br />
and opera<strong>to</strong>rs. 13,38 These data indicate that <strong>TEG</strong><br />
is valid for clinical use in dogs, horses, and cats although<br />
special attention should be given <strong>to</strong> minimize<br />
preanalytical fac<strong>to</strong>rs, such as traumatic venipuncture,<br />
increased s<strong>to</strong>rage time, aberrant temperature, and in<br />
vitro hemolysis, as possible sources <strong>of</strong> error.<br />
In addition <strong>to</strong> preanalytical fac<strong>to</strong>rs, red cell mass<br />
correlates with various <strong>TEG</strong> variables. Evidence suggests<br />
there is an inverse linear correlation between<br />
hema<strong>to</strong>crit and G/MA and a angle in people and various<br />
animal species. 16,20,42–46 Whether decreased red cell<br />
mass truly reflects in vivo hypercoagulability is subject<br />
<strong>to</strong> debate. 43,44,46,47 In people and dogs, decreased and<br />
increased hema<strong>to</strong>crit has been associated with hypercoagulability<br />
and hypocoagulability, respectively, in<br />
vivo. 16,20,42–46 Isolated reduction <strong>of</strong> hema<strong>to</strong>crit, in<br />
people, with no change in platelet concentration, coagulation<br />
fac<strong>to</strong>r concentration, or anticoagulant concentration<br />
accelerated blood coagulation, as demonstrated<br />
with celite-activated samples using the Haemoscope<br />
<strong>TEG</strong> and RO<strong>TEM</strong>. 44,46 Moreover, people with iron<br />
408 Vet Clin Pathol 39/4 (<strong>2010</strong>) 405–416 c <strong>2010</strong> American Society for Veterinary Clinical Pathology
Kol and Borjesson <strong>Application</strong> <strong>of</strong> <strong>TEG</strong> <strong>to</strong> <strong>veterinary</strong> medicine<br />
deficiency anemia and splenec<strong>to</strong>mized thalassemic individuals<br />
had RO<strong>TEM</strong> tracings that were consistent<br />
with hypercoagulability. 43,44 However, a separate<br />
measure <strong>of</strong> hypercoagulability, the endogenous<br />
thrombin potential test, failed <strong>to</strong> provide supporting<br />
results. 43,44 Some authors have interpreted these data<br />
<strong>to</strong> suggest that decreased red cell density will result in<br />
an artifact in tracings that suggests hypercoagulability.<br />
However, others have argued that given the increased<br />
risk for thrombosis in thalassemic patients and the lack<br />
<strong>of</strong> increased potential for thrombin generation,<br />
the RO<strong>TEM</strong> may be superior <strong>to</strong> the plasma-based<br />
endogenous thrombin potential assay in detecting<br />
hypercoagulability that precedes thrombosis. In animals,<br />
increased hema<strong>to</strong>crit was associated with <strong>TEG</strong><br />
variables indicative <strong>of</strong> hypocoagulability in Greyhound<br />
dogs and in transgenic mice with marked<br />
erythrocy<strong>to</strong>sis. 42,45 In both studies, <strong>TEG</strong> tracings that<br />
indicated hypocoagulability were associated with<br />
hypocoagulable phenotypes, ie, an increased bleeding<br />
tendency. However, when the murine blood was diluted<br />
in vitro with maintenance <strong>of</strong> the platelet count,<br />
the <strong>TEG</strong> tracing normalized. 45 Induction <strong>of</strong> moderate<strong>to</strong>-severe<br />
in vitro hemolysis in canine and equine citrated<br />
blood samples resulted in significantly decreased<br />
G and MA values, consistent with hypocoagulability.<br />
16,48 This was attributed <strong>to</strong> in vitro platelet activation<br />
with resultant hyporeactive platelets contributing<br />
<strong>to</strong> decreased clot strength. 48<br />
Clinical <strong>Application</strong>s in Veterinary Medicine<br />
<strong>TEG</strong> has been studied in various clinical settings,<br />
mostly in dogs. Although recently validated for use in<br />
horses and cats, clinical studies have yet <strong>to</strong> be published<br />
outlining the clinical utility <strong>of</strong> <strong>TEG</strong> in these species.<br />
However, published abstracts suggest that the<br />
clinical use <strong>of</strong> <strong>TEG</strong> is being focused on critically ill foals<br />
and horses with colic. 49–51 There are sporadic reports <strong>of</strong><br />
evaluation <strong>of</strong> coagulation in cattle, pigs, sheep, guinea<br />
pigs, rats, and various species <strong>of</strong> fish using <strong>TEG</strong>, 52–59<br />
but, <strong>to</strong> date there are no widely accepted guidelines <strong>to</strong><br />
direct appropriate clinical use or interpretation <strong>of</strong> <strong>TEG</strong><br />
tracings in these species.<br />
Hypercoagulable states<br />
VT is a serious and life-threatening complication <strong>of</strong><br />
many underlying disease processes, including neoplasia,<br />
immune-mediated hemolytic anemia (IMHA), sepsis,<br />
heartworm disease, hyperadrenocorticism, and others;<br />
associated risk fac<strong>to</strong>rs for the development <strong>of</strong> VT in animals<br />
are well described. 60–62 Routine hemostatic assays<br />
have poor sensitivity for the detection <strong>of</strong> hypercoagulability,<br />
5,26,29,63,64 and <strong>TEG</strong> has been evaluated for its<br />
capacity <strong>to</strong> provide early, sensitive detection <strong>of</strong> hypercoagulability.<br />
26,29,50,51,63–68 Discrepancies among studies,<br />
including variability <strong>of</strong> <strong>TEG</strong> methodology and the<br />
occasional absence <strong>of</strong> concurrent hema<strong>to</strong>logic data,<br />
including platelet count, fibrinogen concentration, and<br />
hema<strong>to</strong>crit, limit our ability <strong>to</strong> fully interpret and compare<br />
<strong>TEG</strong> results among studies. Interpretation is further<br />
hindered by the absence <strong>of</strong> long-term prospective studies<br />
that confirm a positive correlation between <strong>TEG</strong> tracings<br />
that indicate hypercoagulability and true risk <strong>of</strong><br />
thrombosis in the animal. To date, hypercoagulability, as<br />
evidenced by alterations in the <strong>TEG</strong> components G and<br />
MA, has been demonstrated in dogs with parvoviral enteritis,<br />
neoplasia, DIC, and IMHA and in dogs admitted<br />
<strong>to</strong> ICU. 26,29,63–65<br />
In an early case–controlled study, 9 puppies with<br />
naturally occurring parvoviral enteritis were compared<br />
with 9 age-matched control dogs. 63 Hypercoagulability<br />
was detected in all <strong>of</strong> the puppies with parvoviral<br />
entiritis, as evidenced by an increased MA using<br />
recalcified citrated blood. These puppies also had<br />
significantly increased fibrinogen concentrations<br />
compared with control puppies. Four <strong>of</strong> the dogs with<br />
parvoviral enteritis developed clinical evidence <strong>of</strong><br />
catheter-associated VT or phlebitis. 63<br />
Underlying malignancy is considered a risk fac<strong>to</strong>r<br />
for thrombosis in animals and people. 60–62,69–73 The<br />
proposed mechanisms <strong>of</strong> thrombus formation are not<br />
fully characterized but may include altered plasmaor<br />
cell-based procoagulant or fibrinolytic activity,<br />
increased production <strong>of</strong> cy<strong>to</strong>kines, including tumor<br />
necrosis fac<strong>to</strong>r, interleukin-1b, and vascular endothelial<br />
growth fac<strong>to</strong>r, by tumor cells, 72 aberrant TF expression,<br />
procoagulant fac<strong>to</strong>r production by neoplastic cells, and<br />
antiphospholipid antibody production. 72,74 In one study<br />
using rhTF-Haemoscope <strong>TEG</strong>, 67% <strong>of</strong> dogs with malignant<br />
neoplasia had hemostatic dysfunction, defined as<br />
an altered G value. Of these dogs, 75% were hypercoagulable<br />
and 25% were hypocoagulable. 64 Dogs with<br />
malignant neoplasia were significantly more likely <strong>to</strong> be<br />
hypercoagulable compared with dogs that had benign<br />
neoplasms, although 31% <strong>of</strong> the dogs with benign neoplasms<br />
were also hypercoagulable. 64 Hypercoagulability<br />
was not attributable <strong>to</strong> fibrinogen concentration as<br />
there was no significant difference in the fibrinogen<br />
concentrations <strong>of</strong> dogs with malignant compared with<br />
those with benign neoplasia. No information was provided<br />
on the overall correlation between fibrinogen<br />
concentration and G/MA or the number <strong>of</strong> dogs with<br />
<strong>TEG</strong> tracings indicative <strong>of</strong> hypercoagulability that developed<br />
VT. These findings are consistent with a similar<br />
Vet Clin Pathol 39/4 (<strong>2010</strong>) 405–416 c <strong>2010</strong> American Society for Veterinary Clinical Pathology 409
<strong>Application</strong> <strong>of</strong> <strong>TEG</strong> <strong>to</strong> <strong>veterinary</strong> medicine<br />
study in which people with malignant neoplasms had<br />
increased G/MA values. 27<br />
<strong>TEG</strong> tracings that indicated hypercoagulable,<br />
normocoagulable, and hypocoagulable states were also<br />
found in dogs with DIC. In 50 dogs diagnosed with DIC<br />
based on a wide battery <strong>of</strong> hemostatic assays, tracings<br />
obtained using rhTF-<strong>TEG</strong> indicated that 22% were<br />
hypocoagulable, 34% were normocoagulable, and<br />
44% were hypercoagulable. 29 Interestingly, hypocoagulable<br />
dogs had a 2.4 times greater relative risk <strong>of</strong><br />
death within 28 days than hypercoagulable dogs. The<br />
G value was concluded <strong>to</strong> best reflect the hemostatic<br />
status <strong>of</strong> dogs with DIC, and a <strong>TEG</strong> tracing indicating<br />
hypercoagulability was considered a favorable prognostic<br />
indica<strong>to</strong>r. 29 In a similar study in human patients<br />
with severe sepsis with or without overt DIC, the<br />
RO<strong>TEM</strong> MCF value (equivalent <strong>to</strong> the MA value) in<br />
patients with severe sepsis did not differ significantly<br />
from the value in the healthy control group; however,<br />
patients with overt DIC had significantly decreased<br />
MCF, indicative <strong>of</strong> hypocoagulability. 37<br />
Hypercoagulability was also a common hemostatic<br />
abnormality in dogs admitted <strong>to</strong> an ICU with a variety <strong>of</strong><br />
underlying disorders and in dogs with IMHA. 26,65 Eleven<br />
<strong>of</strong> 27 dogs in the ICU were classified as hypercoagulable<br />
by rhTF-<strong>TEG</strong> with supportive evidence that<br />
included decreased antithrombin activity and increased<br />
D-dimer concentration. 26 The majority <strong>of</strong> dogs with<br />
IMHA had <strong>TEG</strong> tracings, obtained using recalcified citrated<br />
blood, indicating hypercoagulability with only 6 <strong>of</strong><br />
39 dogs classified as normocoagulable. 65 One potential<br />
confounding fac<strong>to</strong>r in the dogs with IMHA was that all<br />
dogs in the study were pretreated with corticosteroids,<br />
which are suspected <strong>to</strong> induce a hypercoagulable state 75<br />
and alter <strong>TEG</strong> variables. 68 The investiga<strong>to</strong>rs claimed that,<br />
in this specific clinical setting, a <strong>TEG</strong> tracing indicating<br />
normocoagulability was a poor prognostic marker. 65<br />
Evidence in human clinical settings supports the<br />
hypothesis that a hypercoagulable state indicated by a<br />
<strong>TEG</strong> tracing is predictive <strong>of</strong> thromboembolic events, especially<br />
pos<strong>to</strong>peratively. 18,76–78 Nonetheless, the data<br />
are not consistent. In a recent review paper, the predictive<br />
accuracy <strong>of</strong> <strong>TEG</strong> results for pos<strong>to</strong>perative thromboembolic<br />
events was judged <strong>to</strong> be ‘‘highly variable,’’<br />
and the authors recommended further prospective studies.<br />
76 Certainly in <strong>veterinary</strong> medicine, prospective studies<br />
are warranted <strong>to</strong> better characterize the effects <strong>of</strong><br />
fibrinogen concentration, platelet concentration, and<br />
red cell mass on <strong>TEG</strong> tracings and <strong>to</strong> determine the sensitivity,<br />
specificity, positive predictive value, negative<br />
predictive value, and accuracy <strong>of</strong> <strong>TEG</strong> tracings that indicate<br />
hypercoagulability in predicting thromboembolic<br />
events in various clinical settings.<br />
Hypocoagulable states<br />
Kol and Borjesson<br />
Accurate detection <strong>of</strong> hypocoagulability with resultant<br />
increased risk <strong>of</strong> hemorrhage could guide transfusion<br />
and hemostatic therapy during and after surgery or<br />
other invasive procedures, such as liver biopsy. Coagulation<br />
assays such as PT and aPTT, fibrinogen concentration,<br />
and platelet concentration are commonly used<br />
in both <strong>veterinary</strong> and human medicine <strong>to</strong> assess the<br />
risk <strong>of</strong> bleeding as a result <strong>of</strong> a diagnostic or surgical<br />
procedure. However, a poor correlation was found in<br />
people between prolonged PT and hemorrhage after<br />
invasive procedures, 4 leading <strong>to</strong> the conclusion that<br />
there was insufficient evidence <strong>to</strong> support the use <strong>of</strong><br />
transfusion before procedures based on results <strong>of</strong><br />
plasma-based hemostatic tests. 4 Similarly, in <strong>veterinary</strong><br />
medicine, 2 retrospective studies have demonstrated<br />
variable correlation between coagulation test<br />
results and bleeding after fine-needle aspiration and<br />
tissue-core biopsy. 79,80 Given the poor capacity <strong>of</strong><br />
these assays <strong>to</strong> predict bleeding, the use <strong>of</strong> <strong>TEG</strong> <strong>to</strong> accurately<br />
detect hypocoagulability and predict bleeding<br />
events has been evaluated.<br />
<strong>TEG</strong> may be superior <strong>to</strong> plasma-based assays in its<br />
capacity <strong>to</strong> correctly predict hemorrhagic episodes in<br />
dogs. 23,81,82 In a prospective study that compared the<br />
hemostatic phenotype in 27 dogs in hypocoagulable<br />
states, 27 in normocoagulable states, and 27 in hypercoagulable<br />
states based on results from rhTF-<strong>TEG</strong>, it was<br />
found that G value alone had a positive and a negative<br />
predictive value for bleeding <strong>of</strong> 89% and 98%, respectively.<br />
Moreover, G value more accurately predicted<br />
bleeding than the combination <strong>of</strong> platelet concentration,<br />
PT and aPTT results, D-dimer concentration, and<br />
fibrinogen concentration. 23 <strong>TEG</strong> results may also predict<br />
bleeding in dogs with severe fac<strong>to</strong>r VIII deficiency<br />
(hemophilia A). 81 In one study, bleeding was induced in<br />
anesthetized dogs with severe fac<strong>to</strong>r VIII deficiency and<br />
bleeding time was documented. The Haemoscope <strong>TEG</strong><br />
component G, obtained using recalcified citrated blood,<br />
was superior <strong>to</strong> aPTT in predicting bleeding in vivo. 81<br />
<strong>TEG</strong> tracings showed incremental improvement associated<br />
with a dose-dependent response <strong>to</strong> therapy,<br />
whereas standard plasma-based assays failed <strong>to</strong> do so. 81<br />
<strong>TEG</strong> tracings may also be useful in moni<strong>to</strong>ring hemostatic<br />
patterns and developing exercise regimens in dogs<br />
with severe hemophilia A; however, in this study,<br />
correlation <strong>of</strong> <strong>TEG</strong> results with hemostatic phenotype<br />
or bleeding tendency was not attempted. 82 Finally, a<br />
tracing indicating hypocoagulability, obtained by rhTF-<br />
<strong>TEG</strong>, was associated with a poorer prognosis and<br />
increased mortality risk in dogs admitted <strong>to</strong> ICU with a<br />
clinical suspicion <strong>of</strong> DIC. 29 These findings are supported<br />
410 Vet Clin Pathol 39/4 (<strong>2010</strong>) 405–416 c <strong>2010</strong> American Society for Veterinary Clinical Pathology
Kol and Borjesson <strong>Application</strong> <strong>of</strong> <strong>TEG</strong> <strong>to</strong> <strong>veterinary</strong> medicine<br />
by a new study in which a hypocoagulable state, based<br />
on kaolin-activated Haemoscope <strong>TEG</strong> tracings, in people<br />
admitted <strong>to</strong> ICU was an independent risk fac<strong>to</strong>r for<br />
death within 30 days. 83<br />
Moni<strong>to</strong>ring anticoagulant therapy<br />
Low-molecular-weight heparin (LMWH) is increasingly<br />
being used in <strong>veterinary</strong> medicine for treatment <strong>of</strong><br />
thromboembolic diseases and as thrombophylaxis in animal<br />
patients at increased risk for thrombosis. 84–88 Antifac<strong>to</strong>r<br />
Xa activity is considered <strong>to</strong> be the ‘‘gold standard’’<br />
for moni<strong>to</strong>ring the effect <strong>of</strong> heparin on coagulability;<br />
however, this assay is expensive and not readily available.<br />
<strong>TEG</strong> has been assessed for its efficacy in moni<strong>to</strong>ring<br />
heparin therapy in animal and human patients. 85,87–89<br />
In recent prospective studies, healthy dogs 21 and cats 19<br />
were given therapeutic doses <strong>of</strong> different heparins, including<br />
LMWH, subcutaneously. Only treatment with<br />
unfractionated heparin reached therapeutic levels as evidenced<br />
by anti-Xa activity and marked prolongation <strong>of</strong><br />
Haemoscope <strong>TEG</strong> R time (recalcified method) with no<br />
clot formation up <strong>to</strong> 12 hours after a single subcutaneous<br />
administration. The in vitro effects <strong>of</strong> LMWH have<br />
also been tested on citrated canine blood. 87 <strong>TEG</strong> tracings<br />
showed dose-dependent prolongation <strong>of</strong> R and K times<br />
and decreased clot strength using rhTF-<strong>TEG</strong> and<br />
heparinase-coated cups, whereas <strong>TEG</strong> tracings using<br />
kaolin-activated <strong>TEG</strong> and heparinase-coated cups were<br />
unremarkable, except for a prolonged R time. 87 Similar<br />
results have been found in a recent study that explored<br />
the use <strong>of</strong> native Haemoscope <strong>TEG</strong> and heparinasecoated<br />
cups for moni<strong>to</strong>ring LMWH for thrombophylaxis<br />
therapy in people with increased risk for deep vein<br />
thrombosis (DVT). 89 The authors suggested that concurrent<br />
measurement <strong>of</strong> Haemoscope <strong>TEG</strong> using plain and<br />
heparinase-coated cups may detect anticoagulated patients<br />
at increased risk <strong>of</strong> developing DVT; however,<br />
sensitivity, specificity, positive predictive value, and<br />
negative predictive value were not calculated. 89 To date,<br />
it appears that <strong>TEG</strong> may have some clinical utility for the<br />
moni<strong>to</strong>ring heparin therapy in animals; however, expected<br />
<strong>TEG</strong> results will depend on the choice <strong>of</strong> activa<strong>to</strong>r,<br />
the choice <strong>of</strong> plain or heparinase-coated cups, and<br />
the dose and type <strong>of</strong> heparin used.<br />
Platelet function<br />
Congenital and acquired disorders <strong>of</strong> platelet dysfunction<br />
are well characterized and relatively common in<br />
animals and have been reviewed. 90–92 Acquired platelet<br />
dysfunction can occur secondary <strong>to</strong> uremia, infection<br />
with various agents, such as Ehrlichia canis and<br />
FeLV, snake envenomation, neoplasia, liver disease,<br />
and drug administration, especially nonsteroidal antiinflamma<strong>to</strong>ry<br />
drugs (NSAID). 92–98 The use <strong>of</strong> specific<br />
platelet inhibi<strong>to</strong>r drugs, such as clopidogrel (platelet<br />
ADP chemorecep<strong>to</strong>r [P2Y 12] inhibi<strong>to</strong>r), and glycoprotein<br />
(GP) IIb/IIIa inhibi<strong>to</strong>rs may predispose animals <strong>to</strong><br />
bleeding. As such, there is interest in platelet function<br />
assays that are readily accessible, reliable, and costeffective<br />
for moni<strong>to</strong>ring antiplatelet therapy or diagnosing<br />
congenital or acquired platelet disorders. 99,100<br />
Platelets have multiple physiologic activa<strong>to</strong>rs and<br />
are a major contribu<strong>to</strong>r <strong>to</strong> the <strong>TEG</strong> G/MA value.<br />
Thrombin is a major and powerful platelet activa<strong>to</strong>r,<br />
and its presence masks the detection <strong>of</strong> platelet dysfunction<br />
that results from alteration <strong>of</strong> pathways <strong>of</strong><br />
weaker activa<strong>to</strong>rs, such as ADP or collagen. 101 Sporadic<br />
studies have shown that <strong>TEG</strong> tracings did not differ between<br />
normal dogs and dogs with either a specific platelet<br />
dysfunction, such as Scott syndrome, or dogs that<br />
were treated with NSAID. 102,103 Haemoscope <strong>TEG</strong><br />
PlateletMapping is a modified <strong>TEG</strong> assay specifically designed<br />
<strong>to</strong> asses platelet function. 101 The concept behind<br />
PlateletMapping is <strong>to</strong> eliminate the potent effect <strong>of</strong><br />
thrombin on blood platelets during clot formation.<br />
Blood is drawn in<strong>to</strong> heparin and further activated with<br />
reptilase and fac<strong>to</strong>r XIIIa <strong>to</strong> allow a small, polymerized<br />
fibrin clot <strong>to</strong> form in the absence <strong>of</strong> thrombin. The clot<br />
serves as a scaffold for platelet activation. Two other<br />
<strong>TEG</strong> cups are used and platelet agonists, ADP and<br />
arachadonic acids, are added <strong>to</strong> induce platelet activation.<br />
A fourth heparinase-coated <strong>TEG</strong> cup and kaolin<br />
activation are also used. Equations are derived <strong>to</strong> assess<br />
the percent MA aggregation response <strong>to</strong> an agonist.<br />
Haemoscope <strong>TEG</strong> PlateletMapping showed good correlation<br />
with optic platelet aggregometry in detecting<br />
platelet dysfunction after in vitro inhibition by antagonists<br />
<strong>of</strong> various platelet recep<strong>to</strong>rs, such as GP IIb/IIIa,<br />
P2Y 12, and thromboxane A 2 recep<strong>to</strong>r. 101 Preliminary<br />
data suggest that Haemoscope <strong>TEG</strong> PlateletMapping<br />
may be used <strong>to</strong> assess platelet inhibition in dogs that<br />
are treated with clopidogrel. 104 The primary uses <strong>to</strong> date<br />
for <strong>TEG</strong> PlateletMapping include moni<strong>to</strong>ring platelet<br />
inhibition therapy and diagnosing naturally occurring<br />
thrombocy<strong>to</strong>pathies; however, this novel technique<br />
may also be able <strong>to</strong> identify platelet hyperreactivity. 105<br />
Recently, PlateletMapping was also validated for use in<br />
RO<strong>TEM</strong> analyzers. 106<br />
Summary<br />
<strong>TEG</strong> is an old technique being used in new ways <strong>to</strong> advance<br />
our understanding <strong>of</strong> hemostasis. <strong>TEG</strong> has been<br />
Vet Clin Pathol 39/4 (<strong>2010</strong>) 405–416 c <strong>2010</strong> American Society for Veterinary Clinical Pathology 411
<strong>Application</strong> <strong>of</strong> <strong>TEG</strong> <strong>to</strong> <strong>veterinary</strong> medicine<br />
validated in dogs, horses, and cats. <strong>TEG</strong> analysis should<br />
be performed on citrated blood by experienced personnel<br />
using standard pro<strong>to</strong>cols in which preanalytical<br />
fac<strong>to</strong>rs, including s<strong>to</strong>rage temperature and time<br />
<strong>to</strong> analysis, are controlled. Reference intervals<br />
should be generated locally using specific activa<strong>to</strong>rs.<br />
Hema<strong>to</strong>logic measurements that may confound <strong>TEG</strong><br />
analyses, including fibrinogen concentration, platelet<br />
concentration, and RBC mass, should be considered<br />
when interpreting <strong>TEG</strong> results. We believe that<br />
<strong>TEG</strong> analysis provides complementary information <strong>to</strong><br />
routine coagulation assays. Additional long-term<br />
prospective studies are needed <strong>to</strong> determine whether<br />
<strong>TEG</strong> can be used <strong>to</strong> (1) guide and moni<strong>to</strong>r blood<br />
product transfusion and anticoagulant therapy or (2)<br />
accurately predict severe clinical complications associated<br />
with disruptions in hemostasis, including thrombosis<br />
and hemorrhage.<br />
Disclosure: The authors have indicated they have no affiliations<br />
or financial involvement with any organization or entity<br />
with a financial interest in, or in financial competition<br />
with, the subject matter or materials discussed in this paper.<br />
References<br />
1. Hartert H. Blutgerinnungsstudien mit der<br />
Thrombelas<strong>to</strong>graphie; einem neuen Untersuchungs<br />
verfahren [Coagulation analysis with<br />
thrombelas<strong>to</strong>graphy, a new method]. Klin Wochenschr.<br />
1948;26:577–583.<br />
2. Hartert H. Die thrombelas<strong>to</strong>graphie. Eine methode zur<br />
physikalischen analyse des blutgerinnungsvarganges<br />
[Thrombelas<strong>to</strong>graphy, a method for physical analysis <strong>of</strong><br />
blood coagulation]. Z Gesamte Exp Med.<br />
1951;117:189–203.<br />
3. H<strong>of</strong>fman M, Monroe DM III. A cell-based model <strong>of</strong><br />
hemostasis. Thromb Haemost. 2001;85:958–965.<br />
4. Segal JB, Dzik WH. Paucity <strong>of</strong> studies <strong>to</strong> support that<br />
abnormal coagulation test results predict bleeding in<br />
the setting <strong>of</strong> invasive procedures: an evidence-based<br />
review. Transfusion. 2005;45:1413–1425.<br />
5. Nelson OL, Andreasen C. The utility <strong>of</strong> plasma D-dimer<br />
<strong>to</strong> identify thromboembolic disease in dogs. J Vet Intern<br />
Med. 2003;17:830–834.<br />
6. RO<strong>TEM</strong> Marketing Approval by FDA. Available at:<br />
http://www.accessdata.fda.gov/cdrh_docs/pdf8/<br />
K083842.pdf. Accessed July 27, <strong>2010</strong>.<br />
7. Jackson GN, Ashpole KJ, Yentis SM. The <strong>TEG</strong> vs the<br />
RO<strong>TEM</strong> thromboelas<strong>to</strong>graphy/thromboelas<strong>to</strong>metry<br />
systems. Anaesthesia. 2009;64:212–215.<br />
8. Ludding<strong>to</strong>n RJ. Thrombelas<strong>to</strong>graphy/<br />
thromboelas<strong>to</strong>metry. Clin Lab Haema<strong>to</strong>l.<br />
2005;27:81–90.<br />
9. Kang YG, Martin DJ, Marquez J, et al. Intraoperative<br />
changes in blood coagulation and thrombelas<strong>to</strong>graphic<br />
moni<strong>to</strong>ring in liver transplantation. Anesth Analg.<br />
1985;64:888–896.<br />
10. Spiess BD, Gillies BS, Chandler W, et al. Changes in<br />
transfusion therapy and reexploration rate after<br />
institution <strong>of</strong> a blood management program in cardiac<br />
surgical patients. J Cardiothorac Vasc Anesth.<br />
1995;9:168–173.<br />
11. Kraft W. Das thrombelas<strong>to</strong>gramm der gesunden<br />
hauskatze und die behandlung der<br />
verbrauchskoagulopathie bei panleukopenie<br />
[Thrombelas<strong>to</strong>gram in healthy domestic cats and<br />
therapy <strong>of</strong> disseminated intravascular coagulation<br />
(DIC) in panleukopenia]. Berl Munch Tierarztl<br />
Wochenschr. 1973;86:394–396.<br />
12. Bauer N, Eralp O, Moritz A. Establishment <strong>of</strong> reference<br />
intervals for kaolin-activated thromboelas<strong>to</strong>graphy in<br />
dogs including an assessment <strong>of</strong> the effects <strong>of</strong> sex and<br />
anticoagulant use. J Vet Diagn Invest. 2009;21:641–648.<br />
13. Epstein KL, Brainard BM, Lopes MA, et al.<br />
Thrombelas<strong>to</strong>graphy in 26 healthy horses with and<br />
without activation by recombinant human tissue<br />
fac<strong>to</strong>r. J Vet Emerg Crit Care (San An<strong>to</strong>nio).<br />
2009;19:96–101.<br />
14. Leclere M, Lavoie JP, Dunn M, Bédard C. Evaluation <strong>of</strong><br />
a modified thrombelas<strong>to</strong>graphy assay initiated with<br />
recombinant human tissue fac<strong>to</strong>r in clinically healthy<br />
horses. Vet Clin Pathol. 2009;38:462–466.<br />
15. Marschner CB, Bjornvad CR, Kristensen AT, et al.<br />
Thromboelas<strong>to</strong>graphy results on citrated whole blood<br />
from clinically healthy cats depend on modes <strong>of</strong><br />
activation. Acta Vet Scand. <strong>2010</strong>;52:38–42.<br />
16. Paltrinieri S, Meazza C, Giordano A, Tunesi C.<br />
Validation <strong>of</strong> thromboelas<strong>to</strong>metry in horses. Vet Clin<br />
Pathol. 2008;37:277–285.<br />
17. Wiinberg B, Jensen AL, Rojkjaer R, Johansson P,<br />
Kjelgaard-Hansen M, Kristensen AT. Validation <strong>of</strong><br />
human recombinant tissue fac<strong>to</strong>r-activated<br />
thromboelas<strong>to</strong>graphy on citrated whole blood from<br />
clinically healthy dogs. Vet Clin Pathol.<br />
2005;34:389–393.<br />
18. Kashuk JL, Moore EE, Sabel A, et al. Rapid<br />
thromboelas<strong>to</strong>graphy (r-<strong>TEG</strong>) identifies<br />
hypercoagulability and predicts thromboembolic<br />
events in surgical patients. Surgery. 2009;146:764–772;<br />
discussion 772–764.<br />
19. Alwood AJ, Downend AB, Brooks MB, et al.<br />
Anticoagulant effects <strong>of</strong> low-molecular-weight<br />
Kol and Borjesson<br />
412 Vet Clin Pathol 39/4 (<strong>2010</strong>) 405–416 c <strong>2010</strong> American Society for Veterinary Clinical Pathology
Kol and Borjesson <strong>Application</strong> <strong>of</strong> <strong>TEG</strong> <strong>to</strong> <strong>veterinary</strong> medicine<br />
heparins in healthy cats. J Vet Intern Med.<br />
2007;21:378–387.<br />
20. Zuckerman L, Cohen E, Vagher JP, Woodward E,<br />
Caprini JA. Comparison <strong>of</strong> thrombelas<strong>to</strong>graphy with<br />
common coagulation tests. Thromb Haemost.<br />
1981;46:752–756.<br />
21. Pittman JR, Koenig A, Brainard BM. The effect <strong>of</strong><br />
unfractionated heparin on thrombelas<strong>to</strong>graphic<br />
analysis in healthy dogs. J Vet Emerg Crit Care (San<br />
An<strong>to</strong>nio). <strong>2010</strong>;20:216–223.<br />
22. Bowbrick VA, Mikhailidis DP, Stansby G. Influence <strong>of</strong><br />
platelet count and activity on thromboelas<strong>to</strong>graphy<br />
parameters. Platelets. 2003;14:219–224.<br />
23. Wiinberg B, Jensen AL, Rozanski E, et al. Tissue fac<strong>to</strong>r<br />
activated thromboelas<strong>to</strong>graphy correlates <strong>to</strong> clinical<br />
signs <strong>of</strong> bleeding in dogs. Vet J. 2009;179:121–129.<br />
24. Alexander DC, Butt WW, Best JD, Donath SM,<br />
Monagle PT, Shekerdemian LS. Correlation <strong>of</strong><br />
thromboelas<strong>to</strong>graphy with standard tests <strong>of</strong><br />
anticoagulation in paediatric patients receiving<br />
extracorporeal life support. Thromb Res.<br />
<strong>2010</strong>;125:387–392.<br />
25. Park MS, Martini WZ, Dubick MA, et al.<br />
Thromboelas<strong>to</strong>graphy as a better indica<strong>to</strong>r <strong>of</strong><br />
hypercoagulable state after injury than prothrombin<br />
time or activated partial thromboplastin time.<br />
J Trauma. 2009;67:266–275; discussion 275–266.<br />
26. Wagg CR, Boysen SR, Bedard C. Thrombelas<strong>to</strong>graphy<br />
in dogs admitted <strong>to</strong> an intensive care unit. Vet Clin<br />
Pathol. 2009;38:453–461.<br />
27. Akay OM, Ustuner Z, Canturk Z, Mutlu FS, Gulbas Z.<br />
Labora<strong>to</strong>ry investigation <strong>of</strong> hypercoagulability in<br />
cancer patients using rotation thrombelas<strong>to</strong>graphy.<br />
Med Oncol. 2009;26:358–364.<br />
28. Lang T, Johanning K, Metzler H, et al. The effects <strong>of</strong><br />
fibrinogen levels on thromboelas<strong>to</strong>metric variables in<br />
the presence <strong>of</strong> thrombocy<strong>to</strong>penia. Anesth Analg.<br />
2009;108:751–758.<br />
29. Wiinberg B, Jensen AL, Johansson PI, Rozanski E,<br />
Tranholm M, Kristensen AT. Thromboelas<strong>to</strong>graphic<br />
evaluation <strong>of</strong> hemostatic function in dogs with<br />
disseminated intravascular coagulation. J Vet Intern<br />
Med. 2008;22:357–365.<br />
30. Chan MY, Andreotti F, Becker RC. Hypercoagulable<br />
states in cardiovascular disease. Circulation.<br />
2008;118:2286–2297.<br />
31. Vaya A, Mira Y, Martinez M, et al. Biological risk fac<strong>to</strong>rs<br />
for deep vein thrombosis. Clin Hemorheol Microcirc.<br />
2002;26:41–53.<br />
32. Vannucchi AM, Barbui T. Thrombocy<strong>to</strong>sis and<br />
thrombosis. Hema<strong>to</strong>logy Am Soc Hema<strong>to</strong>l Educ Program.<br />
2007;363–370.<br />
33. Kuo YR, Yang KD, Huang MN, Wei FC, Jeng SF.<br />
Reactive thrombocy<strong>to</strong>sis without endothelial damage<br />
does not affect the microvascular anas<strong>to</strong>motic patency.<br />
Ann Plast Surg. 2003;50:57–63.<br />
34. Levrat A, Gros A, Rugeri L, et al. Evaluation <strong>of</strong> rotation<br />
thrombelas<strong>to</strong>graphy for the diagnosis <strong>of</strong><br />
hyperfibrinolysis in trauma patients. Br J Anaesth.<br />
2008;100:792–797.<br />
35. Schochl H, Frietsch T, Pavelka M, Jambor C.<br />
Hyperfibrinolysis after major trauma: differential<br />
diagnosis <strong>of</strong> lysis patterns and prognostic value <strong>of</strong><br />
thrombelas<strong>to</strong>metry. J Trauma. 2009;67:125–131.<br />
36. Summaria L, Sandesara J, Yang G, Vagher JP, Caprini<br />
JA. In vitro comparison <strong>of</strong> fibrinolytic activity <strong>of</strong><br />
plasminogen activa<strong>to</strong>rs using a thrombelas<strong>to</strong>graphic<br />
method: in vivo evaluation <strong>of</strong> the B-chainstrep<strong>to</strong>kinase<br />
complex in the dog model using pretitered<br />
doses. Thromb Haemost. 1986;56:71–79.<br />
37. Sivula M, Pettila V, Niemi TT, Varpula M, Kuitunen AH.<br />
Thromboelas<strong>to</strong>metry in patients with severe sepsis and<br />
disseminated intravascular coagulation. Blood Coagul<br />
Fibrinolysis. 2009;20:419–426.<br />
38. Theusinger OM, Nurnberg J, Asmis LM, Seifert B,<br />
Spahn DR. Rotation thromboelas<strong>to</strong>metry (RO<strong>TEM</strong>)<br />
stability and reproducibility over time. Eur J<br />
Cardiothorac Surg. <strong>2010</strong>;37:677–683.<br />
39. White H, Zollinger C, Jones M, Bird R. Can<br />
thromboelas<strong>to</strong>graphy performed on kaolin-activated<br />
citrated samples from critically ill patients provide<br />
stable and consistent parameters? Int J Lab Hema<strong>to</strong>l.<br />
<strong>2010</strong>;32:167–173.<br />
40. Johansson PI, Bochsen L, Andersen S, Viuff D.<br />
Investigation <strong>of</strong> the effect <strong>of</strong> kaolin and tissue-fac<strong>to</strong>ractivated<br />
citrated whole blood, on clot-forming<br />
variables, as evaluated by thromboelas<strong>to</strong>graphy.<br />
Transfusion. 2008;48:2377–2383.<br />
41. Wiinberg B, Jensen AL, Kjelgaard-Hansen M, et al.<br />
Study on biological variation <strong>of</strong> haemostatic<br />
parameters in clinically healthy dogs. Vet J.<br />
2007;174:62–68.<br />
42. Vilar P, Cou<strong>to</strong> CG, Westendorf N, Iazbik C, Charske J,<br />
Marin L. Thromboelas<strong>to</strong>graphic tracings in retired<br />
racing greyhounds and in non-greyhound dogs. J Vet<br />
Intern Med. 2008;22:374–379.<br />
43. Tripodi A, Cappellini MD, Chantarangkul V, et al.<br />
Hypercoagulability in splenec<strong>to</strong>mized thalassemic<br />
patients detected by whole-blood thromboelas<strong>to</strong>metry,<br />
but not by thrombin generation in platelet-poor<br />
plasma. Haema<strong>to</strong>logica. 2009;94:1520–1527.<br />
44. Spiezia L, Radu C, Marchioro P, et al. Peculiar whole<br />
blood rotation thromboelas<strong>to</strong>metry (Rotem) pr<strong>of</strong>ile in<br />
40 sideropenic anaemia patients. Thromb Haemost.<br />
2008;100:1106–1110.<br />
Vet Clin Pathol 39/4 (<strong>2010</strong>) 405–416 c <strong>2010</strong> American Society for Veterinary Clinical Pathology 413
<strong>Application</strong> <strong>of</strong> <strong>TEG</strong> <strong>to</strong> <strong>veterinary</strong> medicine<br />
45. Shibata J, Hasegawa J, Siemens HJ, et al. Hemostasis<br />
and coagulation at a hema<strong>to</strong>crit level <strong>of</strong> 0.85:<br />
functional consequences <strong>of</strong> erythrocy<strong>to</strong>sis. Blood.<br />
2003;101:4416–4422.<br />
46. Iselin BM, Willimann PF, Seifert B, et al. Isolated<br />
reduction <strong>of</strong> haema<strong>to</strong>crit does not compromise in vitro<br />
blood coagulation. Br J Anaesth. 2001;87:246–249.<br />
47. Kretschmer V, Daraktchiev A, Karger R. Does<br />
haemodilution produce a hypercoagulable state?<br />
Thromb Haemost. 2004;92:670–671.<br />
48. Bauer NB, Eralp O, Moritz A. Effect <strong>of</strong> hemolysis on<br />
canine kaolin-activated thromboelas<strong>to</strong>graphy values<br />
and ADVIA 2120 platelet activation indices. Vet Clin<br />
Pathol. <strong>2010</strong>;39:180–189.<br />
49. Dallap Schaer BL, Bentz AI, Bos<strong>to</strong>n RC, Palmer JE,<br />
Wilkins PA. Coagulation testing in critically ill neonatal<br />
foals: comparison between viscoelastic analysis and<br />
standard coagulation pr<strong>of</strong>iles [Abstract]. J Vet Emerg Crit<br />
Care (San An<strong>to</strong>nio). 2008;18:421.<br />
50. Mendez J, Vilar P, Mudge M, Cou<strong>to</strong> CG.<br />
Thromboelas<strong>to</strong>graphy (<strong>TEG</strong>) for early detection <strong>of</strong><br />
hemostatic abnormalities in horses with colic<br />
[Abstract]. J Vet Intern Med. 2008;22:816.<br />
51. Mendez JL, Vilar P, Mudge MC, Cou<strong>to</strong> CG.<br />
Thromboelas<strong>to</strong>graphy (<strong>TEG</strong>): an innovative technique<br />
for early detection <strong>of</strong> hemostatic abnormalities in foals<br />
with septicemia [Abstract]. J Vet Intern Med.<br />
2009;23:720.<br />
52. van Vliet KJ, Smit GL, Pieterse JJ, Schoonbee HJ, Van<br />
Vuren JH. Thrombelas<strong>to</strong>graphic diagnosis <strong>of</strong> blood<br />
coagulation in two freshwater fish species. Comp<br />
Biochem Physiol A Comp Physiol. 1985;82:19–21.<br />
53. van Vliet KJ, Smit GL, Pieterse JJ, Schoonbee HJ, Van<br />
Vuren JH. A thrombelas<strong>to</strong>graphic study <strong>of</strong> the effect <strong>of</strong><br />
stress on the blood coagulation in Cyprinus carpio<br />
(Cyprinidae) and Oreochromis mossambicus (Cichlidae).<br />
Comp Biochem Physiol A Comp Physiol. 1985;82:23–27.<br />
54. Raina S, Spillert CR, Greenstein SM, Lazaro EJ. Effect<br />
<strong>of</strong> surgery on tumor-induced accelerated coagulation<br />
in a rat carcinoma. J Surg Res. 1985;38:138–142.<br />
55. Kaspareit J, Messow C, Edel J. Blood coagulation<br />
studies in guinea pigs (Cavia porcellus). Lab Anim.<br />
1988;22:206–211.<br />
56. Moalic P, Gruel Y, Foloppe P, Delahousse B, Leclerc MH,<br />
Leroy J. Hemostasis development in the lamb fetus and<br />
neonate. Am J Vet Res. 1989;50:59–63.<br />
57. Heene D, H<strong>of</strong>fmann-Fezer G, Muller-Berghaus G,<br />
H<strong>of</strong>fmann R, Weiss E, Lasch HG. Gerinnungss<strong>to</strong>rungen<br />
bei akuter scheinepest [Coagulation disorders in acute<br />
hog cholera]. Beitr Pathol. 1971;144:259–271.<br />
58. Hinaidy HK. Thrombelas<strong>to</strong>gramn von mit Fasciola<br />
hepatica infizierten sehafen [The thromboelas<strong>to</strong>gram<br />
Kol and Borjesson<br />
<strong>of</strong> sheep infected with Fasciola hepatica]. Z Parasitenkd.<br />
1968;31:12.<br />
59. Kotschy M. Der einfluss von prothrombin- und<br />
fibrinogen-antisera auf das gerinnungssystem von<br />
rinderblut [Effect <strong>of</strong> prothrombin and fibrinogen<br />
antisera on the clotting system <strong>of</strong> bovine blood]. Folia<br />
Haema<strong>to</strong>l Int Mag Klin Morphol Blutforsch.<br />
1972;98:426–436.<br />
60. Hardie EM, Vaden SL, Spaulding K, Malarkey DE.<br />
Splenic infarction in 16 dogs: a retrospective study. J Vet<br />
Intern Med. 1995;9:141–148.<br />
61. Johnson LR, Lappin MR, Baker DC. Pulmonary<br />
thromboembolism in 29 dogs: 1985–1995. J Vet Intern<br />
Med. 1999;13:338–345.<br />
62. Van Winkle TJ, Bruce E. Thrombosis <strong>of</strong> the portal vein<br />
in eleven dogs. Vet Pathol. 1993;30:28–35.<br />
63. Ot<strong>to</strong> CM, Rieser TM, Brooks MB, Russell MW.<br />
Evidence <strong>of</strong> hypercoagulability in dogs with parvoviral<br />
enteritis. J Am Vet Med Assoc. 2000;217:1500–1504.<br />
64. Kristensen AT, Wiinberg B, Jessen LR, Adreasen E,<br />
Jensen AL. Evaluation <strong>of</strong> human recombinant tissue<br />
fac<strong>to</strong>r-activated thromboelas<strong>to</strong>graphy in 49 dogs with<br />
neoplasia. J Vet Intern Med. 2008;22:140–147.<br />
65. Sinnott VB, Ot<strong>to</strong> CM. Use <strong>of</strong> thromboelas<strong>to</strong>graphy in<br />
dogs with immune-mediated hemolytic anemia: 39<br />
cases (2000–2008). J Vet Emerg Crit Care (San An<strong>to</strong>nio).<br />
2009;19:484–488.<br />
66. Fenty RK, deLaforcade AM, Shaw SP, O’Toole TE.<br />
Identification <strong>of</strong> hypercoagulability in dogs with<br />
primary immune-mediated hemolytic anemia utilizing<br />
thromboelas<strong>to</strong>graphy [Abstract]. J Vet Emerg Crit Care<br />
(San An<strong>to</strong>nio). 2008;18:411.<br />
67. Kol A, Nelson RW, Borjesson DL. Dogs with<br />
hyperadrenocorticism are hypercoagulable and have<br />
prolonged PFA-100 closure times [Abstract]. Vet Clin<br />
Pathol. 2009;38(Suppl):E5.<br />
68. Rose L, Bedrad C, Dunn M. Effect <strong>of</strong> prednisone<br />
administration on thrombelas<strong>to</strong>graphic parameters in<br />
healthy beagles [Abstract]. J Vet Intern Med.<br />
2008;22:738.<br />
69. Khorana AA, Francis CW, Culakova E, Kuderer NM,<br />
Lyman GH. Frequency, risk fac<strong>to</strong>rs, and trends for<br />
venous thromboembolism among hospitalized cancer<br />
patients. Cancer. 2007;110:2339–2346.<br />
70. Mohren M, Markmann I, Jentsch-Ullrich K,<br />
Koenigsmann M, Lutze G, Franke A. Increased risk <strong>of</strong><br />
thromboembolism in patients with malignant<br />
lymphoma: a single-centre analysis. Br J Cancer.<br />
2005;92:1349–1351.<br />
71. Wada H, Sase T, Yamaguchi M. Hypercoagulant states<br />
in malignant lymphoma. Exp Oncol. 2005;27:179–185.<br />
414 Vet Clin Pathol 39/4 (<strong>2010</strong>) 405–416 c <strong>2010</strong> American Society for Veterinary Clinical Pathology
Kol and Borjesson <strong>Application</strong> <strong>of</strong> <strong>TEG</strong> <strong>to</strong> <strong>veterinary</strong> medicine<br />
72. Winter PC. The pathogenesis <strong>of</strong> venous<br />
thromboembolism in cancer: emerging links with<br />
tumour biology. Hema<strong>to</strong>l Oncol. 2006;24:126–133.<br />
73. LaRue MJ, Murtaugh RJ. Pulmonary<br />
thromboembolism in dogs: 47 cases (1986–1987). J Am<br />
Vet Med Assoc. 1990;197:1368–1372.<br />
74. Pusterla S, Previtali S, Marziali S, et al.<br />
Antiphospholipid antibodies in lymphoma: prevalence<br />
and clinical significance. Hema<strong>to</strong>l J. 2004;5:341–346.<br />
75. Van Zaane B, Nur E, Squizza<strong>to</strong> A, et al.<br />
Hypercoagulable state in Cushing’s syndrome: a<br />
systematic review. J Clin Endocrinol Metab.<br />
2009;94:2743–2750.<br />
76. Dai Y, Lee A, Critchley LA, White PF. Does<br />
thromboelas<strong>to</strong>graphy predict pos<strong>to</strong>perative<br />
thromboembolic events? A systematic review <strong>of</strong> the<br />
literature. Anesth Analg. 2009;108:734–742.<br />
77. McCrath DJ, Cerboni E, Frumen<strong>to</strong> RJ, Hirsh AL,<br />
Bennet-Guerrero E. Thromboelas<strong>to</strong>graphy maximum<br />
amplitude predicts pos<strong>to</strong>perative thrombotic<br />
complications including myocardial infarction. Anesth<br />
Analg. 2005;100:1576–1583.<br />
78. Wilson D, Cooke EA, McNally MA, Wilson HK, Yeates<br />
A, Mollan RA. Changes in coagulability as measured by<br />
thrombelas<strong>to</strong>graphy following surgery for proximal<br />
femoral fracture. Injury. 2001;32:765–770.<br />
79. Bigge LA, Brown DJ, Penninck DG. Correlation<br />
between coagulation pr<strong>of</strong>ile findings and bleeding<br />
complications after ultrasound-guided biopsies: 434<br />
cases (1993–1996). J Am Anim Hosp Assoc.<br />
2001;37:228–233.<br />
80. Vaden SL, Levine JF, Lees GE, Groman RP, Graver GF,<br />
Forrester SD. Renal biopsy: a retrospective study <strong>of</strong><br />
methods and complications in 283 dogs and 65 cats. J<br />
Vet Intern Med. 2005;19:794–801.<br />
81. Prasad S, Lillicrap D, Labelle A, et al. Efficacy and safety<br />
<strong>of</strong> a new-class hemostatic drug candidate, AV513, in<br />
dogs with hemophilia A. Blood. 2008;111:672–679.<br />
82. Othman M, Powell S, Chirinian Y, Hegadorn C,<br />
Hopman W, Lillicrap D. Thromboelas<strong>to</strong>graphy reflects<br />
global hemostatic variation among severe haemophilia<br />
A dogs at rest and following acute exercise.<br />
Haemophilia. 2009;15:1126–1134.<br />
83. Johansson PI, Stensballe J, Vindelov N, Perner A,<br />
Espersen K. Hypocoagulability, as evaluated by<br />
thrombelas<strong>to</strong>graphy, at admission <strong>to</strong> the ICU is<br />
associated with increased 30-day mortality. Blood<br />
Coagul Fibrinolysis. <strong>2010</strong>;21:168–174.<br />
84. Feige K, Schwarzwald CC, Bombeli T. Comparison <strong>of</strong><br />
unfractioned and low molecular weight heparin for<br />
prophylaxis <strong>of</strong> coagulopathies in 52 horses with colic: a<br />
randomised double-blind clinical trial. Equine Vet J.<br />
2003;35:506–513.<br />
85. Scott KC, Hansen BD, DeFrancesco TC. Coagulation<br />
effects <strong>of</strong> low molecular weight heparin compared with<br />
heparin in dogs considered <strong>to</strong> be at risk for clinically<br />
significant venous thrombosis. J Vet Emerg Crit Care (San<br />
An<strong>to</strong>nio). 2009;19:74–80.<br />
86. Smith CE, Rozanski EA, Freeman LM, Brown DJ,<br />
Goodman JB, Rush JE. Use <strong>of</strong> low molecular weight<br />
heparin in cats: 57 cases (1999–2003). J Am Vet Med<br />
Assoc. 2004;225:1237–1241.<br />
87. Jessen LR, Wiinberg B, Jensen AL, et al. In vitro<br />
heparinization <strong>of</strong> canine whole blood with low<br />
molecular weight heparin (dalteparin) significantly<br />
and dose-dependently prolongs heparinase-modified<br />
tissue fac<strong>to</strong>r-activated thromboelas<strong>to</strong>graphy<br />
parameters and prothrombinase-induced clotting time.<br />
Vet Clin Pathol. 2008;37:363–372.<br />
88. Vargo CL, Taylor SM, Carr A, Jackson ML. The effect <strong>of</strong><br />
a low molecular weight heparin on coagulation<br />
parameters in healthy cats. Can J Vet Res.<br />
2009;73:132–136.<br />
89. Van PY, Cho SD, Underwood SJ, Morris MS, Watters<br />
JM, Schreiber MA. Thrombelas<strong>to</strong>graphy versus<br />
AntiFac<strong>to</strong>r Xa levels in the assessment <strong>of</strong> prophylacticdose<br />
enoxaparin in critically ill patients. J Trauma.<br />
2009;66:1509–1515; discussion 1515–1507.<br />
90. Brooks MB. von Willebrand disease. In: Feldman BF,<br />
Zinkl JG, Jain NC, eds. Schalm’s Veterinary Hema<strong>to</strong>logy.<br />
5th ed. Ames, IA: Blackwell Publishing; 2000:509–515.<br />
91. Boudreaux MK. Characteristics, diagnosis, and<br />
treatment <strong>of</strong> inherited platelet disorders in mammals.<br />
J Am Vet Med Assoc. 2008;233:1251–1259, 1190.<br />
92. Boudreaux MK. Acquired platelet dysfunction. In:<br />
Feldman BF, Zinkl JG, Jain NC, eds. Schalm’s Veterinary<br />
Hema<strong>to</strong>logy. 5th ed. Ames, IA: Blackwell Publishing;<br />
2000:496–500.<br />
93. Baek SJ, McEntee MF, Legendre AM. Review paper:<br />
cancer chemopreventive compounds and canine<br />
cancer. Vet Pathol. 2009;46:576–588.<br />
94. Papich MG. An update on nonsteroidal antiinflamma<strong>to</strong>ry<br />
drugs (NSAIDs) in small animals. Vet Clin<br />
North Am Small Anim Pract. 2008;38:1243–1266, vi.<br />
95. Mathews KA. Pain management for the pregnant,<br />
lactating, and neonatal <strong>to</strong> pediatric cat and dog. Vet Clin<br />
North Am Small Anim Pract. 2008;38:1291–1308, vi–vii.<br />
96. Goodman L, Coles TB, Budsberg S. Leukotriene<br />
inhibition in small animal medicine. J Vet Pharmacol<br />
Ther. 2008;31:387–398.<br />
97. Lascelles BD, Court MH, Hardie EM, Robertson SA.<br />
Nonsteroidal anti-inflamma<strong>to</strong>ry drugs in cats: a review.<br />
Vet Anaesth Analg. 2007;34:228–250.<br />
Vet Clin Pathol 39/4 (<strong>2010</strong>) 405–416 c <strong>2010</strong> American Society for Veterinary Clinical Pathology 415
<strong>Application</strong> <strong>of</strong> <strong>TEG</strong> <strong>to</strong> <strong>veterinary</strong> medicine<br />
98. Goodrich LR, Nixon AJ. Medical treatment <strong>of</strong><br />
osteoarthritis in the horse—a review. Vet J.<br />
2006;171:51–69.<br />
99. Lindahl TL, Ramstrom S. Methods for evaluation <strong>of</strong><br />
platelet function. Transfus Apher Sci. 2009;41:121–125.<br />
100. Collet JP, Montalescot G. Platelet function testing and<br />
implications for clinical practice. J Cardiovasc<br />
Pharmacol Ther. 2009;14:157–169.<br />
101. Craft RM, Chavez JJ, Bresee SJ, Worthman DC,<br />
Cohen E, Carroll RC. A novel modification <strong>of</strong> the<br />
thrombelas<strong>to</strong>graph assay, isolating platelet function,<br />
correlates with optical platelet aggregation. J Lab Clin<br />
Med. 2004;143:301–309.<br />
102. Brooks MB, Randolph J, Warner K, Center S.<br />
Evaluation <strong>of</strong> platelet function screening tests <strong>to</strong><br />
detect platelet procoagulant deficiency in dogs with<br />
Scott syndrome. Vet Clin Pathol. 2009;38:306–315.<br />
Kol and Borjesson<br />
103. Brainard BM, Meredith CP, Callan MB, et al. Changes<br />
in platelet function, hemostasis, and prostaglandin<br />
expression after treatment with nonsteroidal antiinflamma<strong>to</strong>ry<br />
drugs with various cyclooxygenase<br />
selectivities in dogs. Am J Vet Res. 2007;68:<br />
251–257.<br />
104. Brainard BM, Kleine SM, Budsberg SC. Utility <strong>of</strong><br />
thromelas<strong>to</strong>graph (<strong>TEG</strong>) plateletmapping for<br />
evaluation <strong>of</strong> clopidogrel in dogs [Abstract]. J Vet<br />
Intern Med. 2008;22:739.<br />
105. Bochsen L, Nielsen AB, Steinbruchel DA, Johansson<br />
PI. Higher thrombelas<strong>to</strong>graph platelet reactivity in<br />
cardiac surgery patients than in blood donors. Scand<br />
Cardiovasc J. 2007;41:321–324.<br />
106. Scharbert G, Auer A, Kozek-Langenecker S.<br />
Evaluation <strong>of</strong> the platelet mapping assay on rotational<br />
thromboelas<strong>to</strong>metry RO<strong>TEM</strong>. Platelets.<br />
2009;20:125–130.<br />
416 Vet Clin Pathol 39/4 (<strong>2010</strong>) 405–416 c <strong>2010</strong> American Society for Veterinary Clinical Pathology