2005 Proceedings - ASNR
2005 Proceedings - ASNR
2005 Proceedings - ASNR
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Regions of interest (ROIs) were drawn bilaterally on the<br />
ADC maps in the caudate heads, putamina, thalami, cerebellar<br />
white matter (WM), frontal WM, frontal-parietal WM,<br />
parietal WM, and the posterior internal capsules. The average<br />
size of the ROIs was 40 mm 2 . The ADCs of the frontal<br />
WM, the frontal-parietal WM, and the parietal WM were<br />
measured at three levels. Statistical analysis was the student<br />
t-test with Bonferroni correction. A p-value of < 0.00625 was<br />
taken to be significant.<br />
RESULTS<br />
The CNS vasculitis patients’ average ADCs versus the controls<br />
were found to be 7.7 x 10 -4 mm 2 /sec versus 7.4 x 10 -4<br />
mm 2 /sec for the caudate heads, 7.3 x 10 -4 mm 2 /sec versus 7.1<br />
x 10 -4 mm 2 /sec for the putamina, 7.4 x 10 -4 mm 2 /sec versus<br />
7.2 x 10 -4 mm 2 /sec for the thalami, 6.7 x 10 -4 mm 2 /sec versus<br />
6.4 x 10 -4 for the cerebellar WM, 8.1 x 10 -4 mm 2 /sec versus<br />
7.3 x 10 -4 mm 2 /sec for the frontal WM, 7.3 x 10 -4 mm 2 /sec<br />
versus 6.7 x 10 -4 mm 2 /sec for the frontal-parietal WM, 7.7 x<br />
10 -4 mm 2 /sec versus 7.1 x 10 -4 mm 2 /sec for the parietal WM,<br />
and 7.3 x 10 -4 mm 2 /sec versus 6.9 x 10 -4 mm 2 /sec for the posterior<br />
internal capsules. The vasculitis patients’ ADCs of the<br />
frontal WM, frontal-parietal WM, parietal WM, and the posterior<br />
internal capsules all were found to be significantly elevated<br />
(p < 0.00625). The vasculitis patients’ ADCs of the<br />
caudate heads, putamina, thalami, and the cerebellar WM<br />
were not elevated significantly (p > 0.00625).<br />
CONCLUSION<br />
Significantly elevated ADCs that could indicate occult damage<br />
were detected in the supratentorial NLB white matter in<br />
patients with CNS vasculitis. This unique information may<br />
provide additional data that in the future could be incorporated<br />
into facilitating the diagnosis and the treatment plan of<br />
CNS vasculitis patients.<br />
KEY WORDS: Central nervous system vasculitis, nonlesional<br />
brain, ADC<br />
Paper 301 Starting at 3:53 PM, Ending at 3:58 PM<br />
MR Imaging Findings and Radiologic-Pathologic<br />
Correlation in a Case of Postvaccination<br />
Meningoencephalitis in Alzheimer’s Disease<br />
Gomez-Anson, B. M. 1,2 · Sanchez-Guerra, M. 3 · Ferrer, I. 4,5,6 ·<br />
Boada, M. 3<br />
1 Hospital Clinic, Barcelona, SPAIN, 2 Institut<br />
d’Investigacions Biomèdiques August Pi i Sunyer,<br />
Barcelona, SPAIN, 3 Fundació ACE, Barcelona, SPAIN,<br />
4 Hospital Bellvitge, Barcelona, SPAIN, 5 University of<br />
Barcelona, Barcelona, SPAIN, 6 Brain Bank Hospital Clinic,<br />
Barcelona, SPAIN<br />
PURPOSE<br />
To describe the MR findings, and their pathologic correlates,<br />
in a case of asymptomatic Aβ-postvaccination meningoencephalitis<br />
(ME) for Alzheimer’s disease (AD).<br />
MATERIALS & METHODS<br />
A 76-year-old mild/moderate AD patient (GDS = 5) enrolled<br />
in a multicentric, international phase II trial with Aβ-42immunization<br />
including 3 repeated MR imagings. Six<br />
months after the second injection, he experienced progres-<br />
159<br />
sive worsening of speech and gait, initially related to progression<br />
of AD. There was no fever, focal neurologic signs,<br />
or acute symptoms. On routine MR imaging (9 months after<br />
the second injection), a diagnosis of ME was suggested.<br />
After treatment with corticosteroids, and improvement, reactivation<br />
occurred 11 months after the second injection. The<br />
patient then suffered from endocarditis and aspiration pneumonia,<br />
the neurologic status worsened, and died 4 months<br />
after the reactivation episode at a nursing home. The brain<br />
was donated to the Brain Bank.<br />
RESULTS<br />
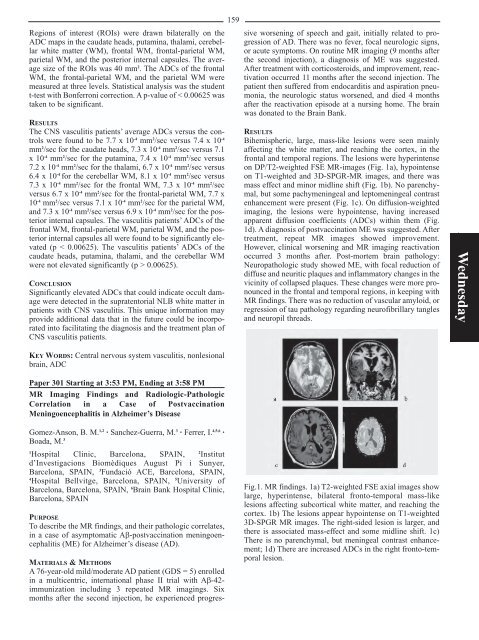
Bihemispheric, large, mass-like lesions were seen mainly<br />
affecting the white matter, and reaching the cortex, in the<br />
frontal and temporal regions. The lesions were hyperintense<br />
on DP/T2-weighted FSE MR-images (Fig. 1a), hypointense<br />
on T1-weighted and 3D-SPGR-MR images, and there was<br />
mass effect and minor midline shift (Fig. 1b). No parenchymal,<br />
but some pachymeningeal and leptomeningeal contrast<br />
enhancement were present (Fig. 1c). On diffusion-weighted<br />
imaging, the lesions were hypointense, having increased<br />
apparent diffusion coefficients (ADCs) within them (Fig.<br />
1d). A diagnosis of postvaccination ME was suggested. After<br />
treatment, repeat MR images showed improvement.<br />
However, clinical worsening and MR imaging reactivation<br />
occurred 3 months after. Post-mortem brain pathology:<br />
Neuropathologic study showed ME, with focal reduction of<br />
diffuse and neuritic plaques and inflammatory changes in the<br />
vicinity of collapsed plaques. These changes were more pronounced<br />
in the frontal and temporal regions, in keeping with<br />
MR findings. There was no reduction of vascular amyloid, or<br />
regression of tau pathology regarding neurofibrillary tangles<br />
and neuropil threads.<br />
Fig.1. MR findings. 1a) T2-weighted FSE axial images show<br />
large, hyperintense, bilateral fronto-temporal mass-like<br />
lesions affecting subcortical white matter, and reaching the<br />
cortex. 1b) The lesions appear hypointense on T1-weighted<br />
3D-SPGR MR images. The right-sided lesion is larger, and<br />
there is associated mass-effect and some midline shift. 1c)<br />
There is no parenchymal, but meningeal contrast enhancement;<br />
1d) There are increased ADCs in the right fronto-temporal<br />
lesion.<br />
Wednesday