ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
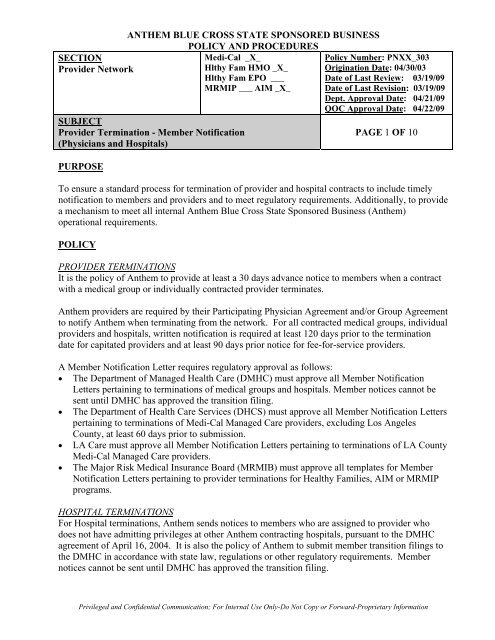
<strong>ANTHEM</strong> <strong>BLUE</strong> <strong>CROSS</strong> <strong>STATE</strong> <strong>SPONSORED</strong> <strong>BUSINESS</strong><br />
<strong>POLICY</strong> AND PROCEDURES<br />
SECTION<br />
Medi-Cal _X_<br />
Policy Number: PNXX_303<br />
Provider Network<br />
Hlthy Fam HMO _X_ Origination Date: 04/30/03<br />
Hlthy Fam EPO ___ Date of Last Review: 03/19/09<br />
SUBJECT<br />
MRMIP ___ AIM _X_ Date of Last Revision: 03/19/09<br />
Dept. Approval Date: 04/21/09<br />
QOC Approval Date: 04/22/09<br />
Provider Termination - Member Notification<br />
(Physicians and Hospitals)<br />
PAGE 1 OF 10<br />
PURPOSE<br />
To ensure a standard process for termination of provider and hospital contracts to include timely<br />
notification to members and providers and to meet regulatory requirements. Additionally, to provide<br />
a mechanism to meet all internal Anthem Blue Cross State Sponsored Business (Anthem)<br />
operational requirements.<br />
<strong>POLICY</strong><br />
PROVIDER TERMINATIONS<br />
It is the policy of Anthem to provide at least a 30 days advance notice to members when a contract<br />
with a medical group or individually contracted provider terminates.<br />
Anthem providers are required by their Participating Physician Agreement and/or Group Agreement<br />
to notify Anthem when terminating from the network. For all contracted medical groups, individual<br />
providers and hospitals, written notification is required at least 120 days prior to the termination<br />
date for capitated providers and at least 90 days prior notice for fee-for-service providers.<br />
A Member Notification Letter requires regulatory approval as follows:<br />
• The Department of Managed Health Care (DMHC) must approve all Member Notification<br />
Letters pertaining to terminations of medical groups and hospitals. Member notices cannot be<br />
sent until DMHC has approved the transition filing.<br />
• The Department of Health Care Services (DHCS) must approve all Member Notification Letters<br />
pertaining to terminations of Medi-Cal Managed Care providers, excluding Los Angeles<br />
County, at least 60 days prior to submission.<br />
• LA Care must approve all Member Notification Letters pertaining to terminations of LA County<br />
Medi-Cal Managed Care providers.<br />
• The Major Risk Medical Insurance Board (MRMIB) must approve all templates for Member<br />
Notification Letters pertaining to provider terminations for Healthy Families, AIM or MRMIP<br />
programs.<br />
HOSPITAL TERMINATIONS<br />
For Hospital terminations, Anthem sends notices to members who are assigned to provider who<br />
does not have admitting privileges at other Anthem contracting hospitals, pursuant to the DMHC<br />
agreement of April 16, 2004. It is also the policy of Anthem to submit member transition filings to<br />
the DMHC in accordance with state law, regulations or other regulatory requirements. Member<br />
notices cannot be sent until DMHC has approved the transition filing.<br />
Privileged and Confidential Communication; For Internal Use Only-Do Not Copy or Forward-Proprietary Information
SECTION<br />
Medi-Cal _X_<br />
Provider Network<br />
Hlthy Fam HMO _X_<br />
Hlthy Fam EPO ___<br />
MRMIP ___ AIM _X_<br />
SUBJECT<br />
Provider Termination - Member Notification<br />
(Physicians and Hospitals)<br />
DEFINITIONS<br />
Policy Number: PNXX_303<br />
QOC Approval Date: 04/22/09<br />
PAGE 2 OF 10<br />
“Affected Member(s)” means a member(s) assigned to a terminating medical group or Primary Care<br />
Provider (PCP); members treated by a Specialty Care Practitioner (SCP) within the last 6 months; or<br />
members who reside within a 15-mile radius of a terminating hospital.<br />
“Continued Access to Care/Continuity of Care” means the process of authorizing continuation of<br />
services with a terminating physician, medical group or hospital under specified conditions and for<br />
a limited period of time with a plan of care to transition the member to a network provider.<br />
“Provider Contracting and Database Administration (PCDA)” is the department responsible for<br />
system updates and changes.<br />
“Hospital” means a general acute care hospital.<br />
“Medical Group” means a medical group, independent practice association or any other similar<br />
organization, reimbursed at a fee-for-service (FFS) or capitated per member per month (capitated)<br />
basis.<br />
“Member Notification Letter” means an appropriately approved letter being sent to members<br />
regarding a provider termination.<br />
“Physicians” means Primary Care Providers (PCP) or Specialty Care Providers (SCP) contracted<br />
either individually or through a Medical Group.<br />
“Provider” means an individual physician, medical group or hospital contracted with Anthem to<br />
provide services to Anthem members.<br />
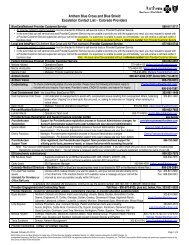
PROCESS<br />
PCDA is responsible for receiving and processing termination notices from providers and tracking<br />
provider terminations internally.<br />
PCDA coordinates efforts with:<br />
• PCDA Reporting conducting impact analysis reports;<br />
• Compliance (regulatory approvals)<br />
• Health Care Management (Hospitals and Capitated Medical Groups)<br />
• Credentialing (terminations for cause)<br />
• Case Management (Continued Access to Care)<br />
• QI/Compliance Analyst (coordination of transition plan and member notification for groups and<br />
hospitals, coordinating the required notification to regulatory agencies, members and other<br />
interested parties)<br />
• PCDA Reporting (member mailing information)<br />
• Network Management and Field Operations (Professional Contracts)
SECTION<br />
Medi-Cal _X_<br />
Provider Network<br />
Hlthy Fam HMO _X_<br />
Hlthy Fam EPO ___<br />
MRMIP ___ AIM _X_<br />
SUBJECT<br />
Provider Termination - Member Notification<br />
(Physicians and Hospitals)<br />
Policy Number: PNXX_303<br />
QOC Approval Date: 04/22/09<br />
PAGE 3 OF 10<br />
The following information details the procedure and process specific to medical group terminations,<br />
hospital terminations and individual physician terminations.<br />
PROCEDURE<br />
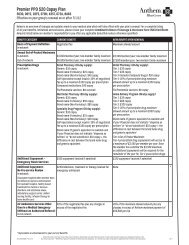
Capitated Medical Group/IPA and Hospital Terminations<br />
Anthem provider agreements 1 require medical groups/IPAs and hospitals to provide Anthem with<br />
written notification of the intent to terminate their agreement at least 120 days prior to the<br />
termination date.<br />
Notification of the intent to terminate either a provider or hospital contract is received by Anthem<br />
Contracting, PCDA and/ or Health Care Management. Notification of the intent to terminate by<br />
Anthem is outline in policy PNXX_008.<br />
• Within 24 hours of receipt of a notice of intent to terminate,<br />
o PCDA notifies Anthem’s Compliance, Reporting, Medical Management, as well as<br />
the QI/Compliance Analyst for FFS medical group (PCP and SCP) terminations.<br />
o Health Care Management notifies the QI/Compliance Analyst, Compliance, Network<br />
Reporting and PCDA of the impending capitated medical group or hospital<br />
termination.<br />
o If the medical group has 2,000 members or more PCDA Reporting will be required<br />
to complete an impact analysis and forward the analysis to the Q/I Compliance<br />
Analyst<br />
o The Q/I Compliance Analyst will prepare a Provider Group Block Transfer Filing<br />
which includes the impact analysis and member notification letter template. The<br />
Filing will be submitted to the Legal department for review.<br />
o Once approval has been obtained from Legal, the Q/I Compliance Analyst will<br />
submit the filing to the DMHC 75 days in advance of the termination date.<br />
o The Q/I Compliance Analyst will also forward the filing to the Compliance<br />
department.<br />
o The Compliance Department will submit the filing to the DHCS.<br />
o If the medical group has less than 2,000 members, the Compliance Department will<br />
send the impact analysis along with the member notification letter template to the<br />
DHCS or LA Care sixty (60) days prior to the termination date for approval.<br />
• PCDA: PCDA identifies the PCPs within a terminating medical group that will be<br />
terminating and submits a request to PDO to close any open PCP panels so that no new<br />
members are assigned to the terminating providers.<br />
• PCDA Reporting: PCDA Reporting conducts an impact analysis of the terminating<br />
provider(s) to assess the availability of alternate providers in Anthem’s network that are<br />
located within the DMHC’s geographic access standards. This impact analysis is used to<br />
complete a group or hospital termination worksheet, which may, in turn, be used to<br />
1 Fee-for-Service Group Agreements, Capitated Medical Group Agreements and Hospital Agreements
SECTION<br />
Medi-Cal _X_<br />
Provider Network<br />
Hlthy Fam HMO _X_<br />
Hlthy Fam EPO ___<br />
MRMIP ___ AIM _X_<br />
SUBJECT<br />
Provider Termination - Member Notification<br />
(Physicians and Hospitals)<br />
Policy Number: PNXX_303<br />
QOC Approval Date: 04/22/09<br />
PAGE 4 OF 10<br />
prepare an enrollee transfer filing for the DMHC (for medical group terminations). It is<br />
also used to notify regulatory agencies, as necessary or required, of any changes to the<br />
composition of the Anthem network that could materially reduce member’s access to<br />
care.<br />
For hospital terminations, the impact analysis includes an assessment of the availability<br />
of alternate contracting hospitals in the same geographic area, with the same range of<br />
services as the terminating facility. It also includes, among other things, the number of<br />
providers with exclusive admitting privileges at the terminating hospital; the number of<br />
members assigned to providers with exclusive admitting privileges at the terminating<br />
hospital; the number of specialists affiliated with the terminating hospital; the number of<br />
alternate hospitals located in the county; and the percentage of members with and<br />
without access to a hospital within 15 miles. Anthem will verify that the alternate<br />
hospitals comply with the DMHC’s geographic access standards for members. Anthem<br />
will also verify that its contracting physicians/medical groups can admit members to an<br />
alternate hospital that is geographically accessible and has the same range of services as<br />
the terminating hospital.<br />
When a hospital terminates, members are not “block transferred” to another hospital<br />
because Anthem members are not assigned to a particular hospital. Members may<br />
obtain services from any Anthem contracting hospital to which their physician or<br />
medical group maintains admitting privileges. Anthem’s network physicians and<br />
medical groups/IPAs are contractually obligated to admit Anthem members to<br />
contracting hospitals (physicians/medical groups/IPAs are not obligated to admit<br />
members to a particular or designated facility).<br />
In summary, Anthem shall:<br />
A. Provide written notification to the appropriate regulatory agency in compliance with<br />
termination guidelines<br />
B. Submit a full impact analysis to the regulatory agency as to how Anthem will fulfill<br />
the agency’s member access requirements.<br />
C. Notify in writing, all affected members at least and providers of the impending<br />
termination.<br />
D. Ensure that provider and member letters are approved by proper regulatory agency<br />
(DHCS/DMHC/LA CARE) at least 60 days prior to use.<br />
For medical group/IPA terminations, if members will be reassigned to another<br />
contracted medical group (rather than an individually contracting fee for service<br />
physician); Anthem will verify the receiving group’s financial and administrative<br />
capacity to accept the additional membership.
SECTION<br />
Medi-Cal _X_<br />
Provider Network<br />
Hlthy Fam HMO _X_<br />
Hlthy Fam EPO ___<br />
MRMIP ___ AIM _X_<br />
SUBJECT<br />
Provider Termination - Member Notification<br />
(Physicians and Hospitals)<br />
Policy Number: PNXX_303<br />
QOC Approval Date: 04/22/09<br />
PAGE 5 OF 10<br />
Once the impact analysis is complete, PCDA Reporting submits the analysis to the<br />
QI/Compliance Analyst, PCDA, and Compliance. Additionally, PCDA Reporting<br />
submits the provider information (i.e., PCP numbers, medical group TIN) to PCDA<br />
Reporting and the QI/Compliance Analyst.<br />
For SCP medical group terminations, PCDA Reporting provides the list of impacted<br />
SCPs. The QI/Compliance Analyst requests a claims report from PCDA Reporting that<br />
identifies all of the Anthem members seen by the terminating SCP within the past 6<br />
months.<br />
• PCDA Reporting: For impending terminations, PCDA Reporting identifies all affected<br />
members based on the request (i.e. members located within the selected zip codes,<br />
members assigned to the PCP or members seen by the terminating SCP) and submits the<br />
member mailing information to the QI/Compliance Analyst.<br />
• QI/Compliance Analyst: Once the QI/Compliance Analyst has all required data<br />
elements (worksheets, proposed Member Notification Letter, impact analysis and<br />
affected member mailing list), s/he submits all required information to Anthem Legal at<br />
least 85 days prior to the impending termination. Once Anthem Legal approves the<br />
filing, the QI/Compliance Analyst submits the filing to the DMHC at least 75 days prior<br />
to the impending termination date. The QI/Compliance Analyst notifies Anthem Legal,<br />
PCDA, Contract Manager, Network Management, Medical Management, Operations<br />
and Compliance of approvals and the member notification mailing is sent.<br />
• Compliance. Compliance submits the required information to the QI/Compliance<br />
Analyst and Anthem Legal for filing.<br />
For medical group/IPA terminations, Anthem Legal reviews the DMHC enrollee transfer filing and<br />
sends the filing along with the proposed Member Notification Letter back to the QI/Compliance<br />
Analyst for submission to the DMHC<br />
For hospital terminations, pursuant to the DMHC’s revised position on member<br />
notification and filings for hospital terminations (communicated to Anthem via e-mail on<br />
April 16, 2004), Anthem will send a copy of the impact analysis report and voluntary<br />
Member Notification Letter to the DMHC approximately 60 days prior to the effective<br />
date of termination.<br />
• QI/Compliance Analyst: Once the transition plan and proposed Member Notification<br />
Letter are approved by the DMHC, the QI/Compliance Analyst coordinates the Member<br />
Notification Letter mailing with Product Services & Promotions. The mailing is a joint<br />
effort between PCDA, Product Services & Promotions and Mail Services.<br />
For PCP medical group terminations, the 60 day advance Member Notification Letter<br />
will instruct the member to contact Anthem if they:<br />
o Have any questions or require assistance in selecting a new PCP<br />
o Are pregnant
SECTION<br />
Medi-Cal _X_<br />
Provider Network<br />
Hlthy Fam HMO _X_<br />
Hlthy Fam EPO ___<br />
MRMIP ___ AIM _X_<br />
SUBJECT<br />
Provider Termination - Member Notification<br />
(Physicians and Hospitals)<br />
Policy Number: PNXX_303<br />
QOC Approval Date: 04/22/09<br />
PAGE 6 OF 10<br />
o Are receiving ongoing treatment from the terminating provider<br />
o Have a child younger than age 3 who is receiving services from the terminating<br />
provider<br />
o Are scheduled for surgery or other procedure<br />
For SCP medical group terminations, the Member Notification Letter instructs the<br />
member to contact his or her PCP as soon as possible in order to receive a referral to a<br />
new specialist. Additionally, the letter instructs the member to contact Anthem if they:<br />
o Have any questions<br />
o Are pregnant<br />
o Are receiving ongoing treatment from the terminating provider<br />
o Have a child younger than age 3 who is receiving services from the terminating<br />
provider<br />
o Are scheduled for surgery or other procedure<br />
In addition, the QI/Compliance Analyst provides PCDA, Operations, Compliance and<br />
Case Management with a copy of the Member Notification Letter and the member<br />
mailing list to identify potential Continued Access to Care/Continuity of Care cases.<br />
• Case Management: Case Management reviews the member mailing list and identifies<br />
any members that may qualify for Continued Access to Care/Continuity of Care. 2<br />
• PCDA: If the member has not selected a new PCP by the termination date, a new PCP<br />
will be assigned to the member. The PCDA is responsible for the actual system<br />
reassignment. The member receives a new membership card identifying their new PCP.<br />
In addition to the new membership card, a notice is provided advising that the<br />
terminating PCP is no longer available. If the member desires a different PCP than the<br />
one assigned, they are instructed to contact the Customer Care Center.<br />
• Field Operations Staff: Network Education Representatives (NER) will forward all<br />
provider termination notices received in the local Community Resource Center office<br />
directly to the QI/Compliance Analyst to ensure appropriate tracking and notification.<br />
The NER will participate in all meetings related to large group or hospital terminations<br />
to ensure coordination of issues at a local level.<br />
• Network Management staff (Professional Contracts): Contract Managers will be<br />
responsible to forward provider termination notices received to the QI/Compliance<br />
Analyst.<br />
2<br />
Refer to Anthem Blue Cross SSB and BCC Corporate Policies and Procedures regarding UM/Transition Assistance and Continuity of<br />
Care/Transition Assistance
SECTION<br />
Medi-Cal _X_<br />
Provider Network<br />
Hlthy Fam HMO _X_<br />
Hlthy Fam EPO ___<br />
MRMIP ___ AIM _X_<br />
SUBJECT<br />
Provider Termination - Member Notification<br />
(Physicians and Hospitals)<br />
Policy Number: PNXX_303<br />
QOC Approval Date: 04/22/09<br />
PAGE 7 OF 10<br />
Contract Managers will be participate in all meetings related to large group or hospital<br />
terminations to facilitate contracts with alternative primary care and specialty providers.<br />
It is Anthem ’s practice to cease contract negotiations with a terminating medical<br />
group/IPA once the member notification has been sent. However, in the rare event an<br />
agreement is reached with a terminating medical group/IPA after the member notice has<br />
been sent, but within 30 days after the effective date of termination, Anthem will send a<br />
second notice to members (Attachment B) telling them that a new contract has been<br />
agreed upon and advising that if they would like to return to their prior PCP or medical<br />
group/IPA, then they may contact Blue Cross and request the change. Member notices<br />
advise that members may change PCPs or medical groups/IPAs by contacting Blue<br />
Cross.<br />
By the date of termination, all PCDA databases and mainframe systems reflect that the<br />
provider is no longer a participating provider.<br />
DMHC Waiver<br />
When a provider termination is immediate (due to death or illness of a provider; insolvency of a<br />
provider; or Anthem is provided with inadequate advance notice of the termination), Anthem can<br />
request a waiver of the 60 day notice requirement due to exigent circumstances. All previously<br />
outlined steps apply when a waiver is being requested (i.e., impact analysis and submission to<br />
Anthem Legal). The Q/I Compliance Analyst will submit the waiver to Anthem Legal for approval.<br />
Once Legal has approved the waiver request, the Q/I Compliance Analyst will submit the waiver<br />
request to the DMHC for approval.<br />
Tracking and Communication<br />
The QI/Compliance Analyst is responsible for tracking and maintaining all information regarding<br />
the termination. In addition, the QI/Compliance Analyst coordinates with Associate Development<br />
and Training (AD&T) to ensure that Anthem associates are made aware of information surrounding<br />
the terminations.<br />
AD&T provides communications to Anthem associates and provides any necessary training.<br />
Monthly Meetings<br />
The QI/Analyst conducts monthly meetings with all departments to discuss contract terminations;<br />
operational issues, and other critical information related to the provider/hospital termination<br />
process.<br />
Fee-for-Service (FFS) Physician Terminations<br />
Anthem’s contracts with fee-for-service physicians (PCPs and SCPs) require those physicians to<br />
notify Anthem at least 90 days prior to the termination date. Notification of the intent to terminate<br />
is received by PCDA. PCDA coordinates all aspects of the member notification for individual<br />
physician terminations. PCDA identifies the affected members and sends a Member Notification<br />
letter at least 30 days prior to the termination, indicating the effective date of the termination.
SECTION<br />
Medi-Cal _X_<br />
Provider Network<br />
Hlthy Fam HMO _X_<br />
Hlthy Fam EPO ___<br />
MRMIP ___ AIM _X_<br />
SUBJECT<br />
Provider Termination - Member Notification<br />
(Physicians and Hospitals)<br />
Policy Number: PNXX_303<br />
QOC Approval Date: 04/22/09<br />
PAGE 8 OF 10<br />
If the FFS PCP has membership of 500 or greater, DHCS must be notified sixty (60) days prior to<br />
the termination date. PCDA will notify Reporting to request an impact analysis and prepare the<br />
member notification letters. PCDA will forward the impact analysis and member notification letters<br />
to the Compliance department. Compliance will send the impact analysis and the member<br />
notification letter template to the DHCS for approval.<br />
• Individually Contracting FFS Primary Care Provider Terminations<br />
To assist the member in selecting a new PCP, a Member Notification Letter is sent outlining the<br />
process for selecting a new PCP. Additionally, the letter will instruct the member to contact<br />
Anthem if they:<br />
o Have any questions or require assistance in selecting a new PCP<br />
o Are pregnant<br />
o Are receiving ongoing treatment from the terminating provider<br />
o Have a child younger than age 3 who is receiving services from the terminating provider<br />
o Are scheduled for surgery<br />
If the member has not selected a new PCP by the termination date, a new PCP will be assigned<br />
to the member. The PCDA is responsible for the actual system reassignment. The member<br />
receives a new membership card identifying their new PCP. In addition to the new membership<br />
card, a notice is provided stating that the terminating PCP is no longer available. If the member<br />
desires a different PCP than the one assigned, they are instructed to contact the Customer Care<br />
Center.<br />
By the date of termination, all PCDA databases and mainframe systems reflect that the<br />
physician is not a participating PCP. In addition, PCDA notifies Case Management of the<br />
provider termination and supplies Case Management with the member roster so they can<br />
identify any Continued Access to Care/Continuity of Care cases.<br />
Every effort is made to send the member notification prior to the termination date. If proper<br />
termination notice is not provided to Anthem and advance notification to members cannot be<br />
achieved, Anthem will send Member Notification Letters as soon as practicably possible. PCDA<br />
will terminate the PCP and reassign the members to a new PCP.<br />
• Individually Contracting FFS Specialist (SCP) Terminations<br />
In order to identify Anthem members being treated by a terminating individually contracted<br />
specialist, PCDA requests a claims report from the Anthem Reporting Department that identifies<br />
all of the Anthem members seen by the terminating SCP within the past 6 months.<br />
Once the report has been prepared, PCDA sends an approved Member Notification Letter to<br />
affected members. The letter instructs the member to contact his or her PCP as soon as possible<br />
in order to receive a referral to a new specialist. Additionally, the letter instructs the member to<br />
contact Anthem if they:<br />
o Have any questions<br />
o Are pregnant<br />
o Are receiving ongoing treatment from the terminating provider
SECTION<br />
Medi-Cal _X_<br />
Provider Network<br />
Hlthy Fam HMO _X_<br />
Hlthy Fam EPO ___<br />
MRMIP ___ AIM _X_<br />
SUBJECT<br />
Provider Termination - Member Notification<br />
(Physicians and Hospitals)<br />
Policy Number: PNXX_303<br />
QOC Approval Date: 04/22/09<br />
PAGE 9 OF 10<br />
o Have a child younger than age 3 who is receiving services from the terminating provider<br />
o Are scheduled for surgery or other procedure<br />
Every effort is made to send the member notification prior to the termination date. However, if<br />
proper termination notice is not provided to Anthem and prior notification to members of the<br />
termination cannot be achieved, Anthem will send the Member Notification Letter as soon as<br />
practicably possible, advising members to contact their PCP or the Customer Care Center for<br />
referral to a contracted specialist. PCDA will then terminate the SCP.<br />
By the date of termination, all PCDA databases and mainframe systems reflect that the physician is<br />
not a participating SCP. In addition, PCDA notifies Case Management of the provider termination<br />
and supplies Case Management with the member roster so they can identify any Continued Access<br />
to Care/Continuity of Care cases.<br />
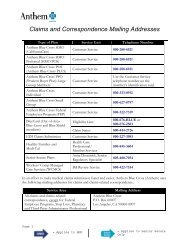
REFERENCES<br />
Anthem Policy & Procedure UMXX_097 - Transition of Care (and subsequent) Corporate Policy<br />
2.13 and Addendum - Utilization Management/Transition Assistance and Continuity of<br />
Care/Transition Assistance<br />
Anthem Policy & Procedure PNXX_017 - DHCS Notification of Terminations and Resignations<br />
California Assembly Bill 1286/ California Senate Bill 244<br />
Group or Hospital Termination Worksheet<br />
Medi-Cal Managed Care Participating Physician Agreement<br />
Member Notification Letter<br />
MMCD All Plan Letter 06007<br />
Title 22, Sections 53212 & 53852<br />
DHCS GMC Sacramento Contract, Section 8.12.5<br />
DHCS CV/BA Contract, Section 6.9.8<br />
DHCS Stanislaus Contract, Section 6.9.8<br />
DHCS Tulare Contract, Section 6.9.8<br />
LA Care Contract, Article IV, Section 4.02e<br />
LA Care Plan Partner Manual, Section 3.8, Page 6, Notice to Members Regarding Change in<br />
Covered Services<br />
Senate Bill 244, Section 3.B.<br />
Attachments – Sample Letters<br />
Ca_pnxx_303_sample letters.zip<br />
RESPONSIBLE DEPARTMENTS<br />
Anthem PCDA<br />
Compliance<br />
Case Management
SECTION<br />
Medi-Cal _X_<br />
Provider Network<br />
Hlthy Fam HMO _X_<br />
Hlthy Fam EPO ___<br />
MRMIP ___ AIM _X_<br />
SUBJECT<br />
Provider Termination - Member Notification<br />
(Physicians and Hospitals)<br />
Reporting<br />
Corporate Legal<br />
Network Development<br />
Credentialing<br />
Provider Contracting and Database Administration<br />
Policy Number: PNXX_303<br />
QOC Approval Date: 04/22/09<br />
PAGE 10 OF 10