ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
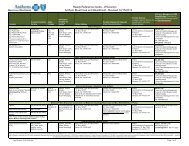
SECTION<br />
Medi-Cal _X_<br />
Provider Network<br />
Hlthy Fam HMO _X_<br />
Hlthy Fam EPO ___<br />
MRMIP ___ AIM _X_<br />
SUBJECT<br />
Provider Termination - Member Notification<br />
(Physicians and Hospitals)<br />
Policy Number: PNXX_303<br />
QOC Approval Date: 04/22/09<br />
PAGE 4 OF 10<br />
prepare an enrollee transfer filing for the DMHC (for medical group terminations). It is<br />
also used to notify regulatory agencies, as necessary or required, of any changes to the<br />
composition of the Anthem network that could materially reduce member’s access to<br />
care.<br />
For hospital terminations, the impact analysis includes an assessment of the availability<br />
of alternate contracting hospitals in the same geographic area, with the same range of<br />
services as the terminating facility. It also includes, among other things, the number of<br />
providers with exclusive admitting privileges at the terminating hospital; the number of<br />
members assigned to providers with exclusive admitting privileges at the terminating<br />
hospital; the number of specialists affiliated with the terminating hospital; the number of<br />
alternate hospitals located in the county; and the percentage of members with and<br />
without access to a hospital within 15 miles. Anthem will verify that the alternate<br />
hospitals comply with the DMHC’s geographic access standards for members. Anthem<br />
will also verify that its contracting physicians/medical groups can admit members to an<br />
alternate hospital that is geographically accessible and has the same range of services as<br />
the terminating hospital.<br />
When a hospital terminates, members are not “block transferred” to another hospital<br />
because Anthem members are not assigned to a particular hospital. Members may<br />
obtain services from any Anthem contracting hospital to which their physician or<br />
medical group maintains admitting privileges. Anthem’s network physicians and<br />
medical groups/IPAs are contractually obligated to admit Anthem members to<br />
contracting hospitals (physicians/medical groups/IPAs are not obligated to admit<br />
members to a particular or designated facility).<br />
In summary, Anthem shall:<br />
A. Provide written notification to the appropriate regulatory agency in compliance with<br />
termination guidelines<br />
B. Submit a full impact analysis to the regulatory agency as to how Anthem will fulfill<br />
the agency’s member access requirements.<br />
C. Notify in writing, all affected members at least and providers of the impending<br />
termination.<br />
D. Ensure that provider and member letters are approved by proper regulatory agency<br />
(DHCS/DMHC/LA CARE) at least 60 days prior to use.<br />
For medical group/IPA terminations, if members will be reassigned to another<br />
contracted medical group (rather than an individually contracting fee for service<br />
physician); Anthem will verify the receiving group’s financial and administrative<br />
capacity to accept the additional membership.