ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
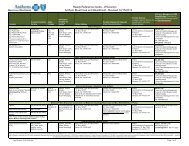
SECTION<br />
Medi-Cal _X_<br />
Provider Network<br />
Hlthy Fam HMO _X_<br />
Hlthy Fam EPO ___<br />
MRMIP ___ AIM _X_<br />
SUBJECT<br />
Provider Termination - Member Notification<br />
(Physicians and Hospitals)<br />
Policy Number: PNXX_303<br />
QOC Approval Date: 04/22/09<br />
PAGE 5 OF 10<br />
Once the impact analysis is complete, PCDA Reporting submits the analysis to the<br />
QI/Compliance Analyst, PCDA, and Compliance. Additionally, PCDA Reporting<br />
submits the provider information (i.e., PCP numbers, medical group TIN) to PCDA<br />
Reporting and the QI/Compliance Analyst.<br />
For SCP medical group terminations, PCDA Reporting provides the list of impacted<br />
SCPs. The QI/Compliance Analyst requests a claims report from PCDA Reporting that<br />
identifies all of the Anthem members seen by the terminating SCP within the past 6<br />
months.<br />
• PCDA Reporting: For impending terminations, PCDA Reporting identifies all affected<br />
members based on the request (i.e. members located within the selected zip codes,<br />
members assigned to the PCP or members seen by the terminating SCP) and submits the<br />
member mailing information to the QI/Compliance Analyst.<br />
• QI/Compliance Analyst: Once the QI/Compliance Analyst has all required data<br />
elements (worksheets, proposed Member Notification Letter, impact analysis and<br />
affected member mailing list), s/he submits all required information to Anthem Legal at<br />
least 85 days prior to the impending termination. Once Anthem Legal approves the<br />
filing, the QI/Compliance Analyst submits the filing to the DMHC at least 75 days prior<br />
to the impending termination date. The QI/Compliance Analyst notifies Anthem Legal,<br />
PCDA, Contract Manager, Network Management, Medical Management, Operations<br />
and Compliance of approvals and the member notification mailing is sent.<br />
• Compliance. Compliance submits the required information to the QI/Compliance<br />
Analyst and Anthem Legal for filing.<br />
For medical group/IPA terminations, Anthem Legal reviews the DMHC enrollee transfer filing and<br />
sends the filing along with the proposed Member Notification Letter back to the QI/Compliance<br />
Analyst for submission to the DMHC<br />
For hospital terminations, pursuant to the DMHC’s revised position on member<br />
notification and filings for hospital terminations (communicated to Anthem via e-mail on<br />
April 16, 2004), Anthem will send a copy of the impact analysis report and voluntary<br />
Member Notification Letter to the DMHC approximately 60 days prior to the effective<br />
date of termination.<br />
• QI/Compliance Analyst: Once the transition plan and proposed Member Notification<br />
Letter are approved by the DMHC, the QI/Compliance Analyst coordinates the Member<br />
Notification Letter mailing with Product Services & Promotions. The mailing is a joint<br />
effort between PCDA, Product Services & Promotions and Mail Services.<br />
For PCP medical group terminations, the 60 day advance Member Notification Letter<br />
will instruct the member to contact Anthem if they:<br />
o Have any questions or require assistance in selecting a new PCP<br />
o Are pregnant