ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
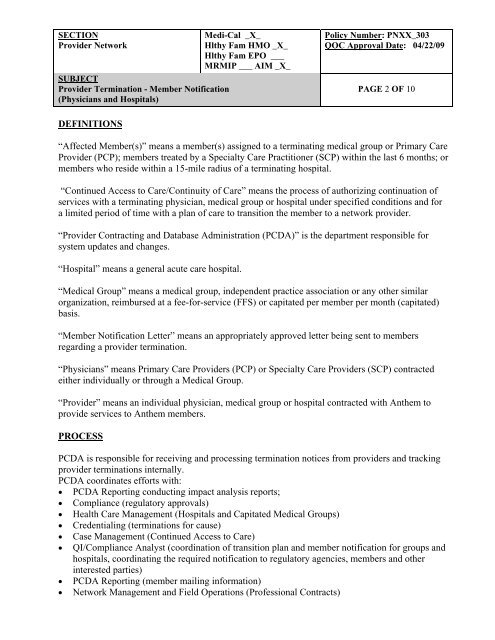
SECTION<br />
Medi-Cal _X_<br />
Provider Network<br />
Hlthy Fam HMO _X_<br />
Hlthy Fam EPO ___<br />
MRMIP ___ AIM _X_<br />
SUBJECT<br />
Provider Termination - Member Notification<br />
(Physicians and Hospitals)<br />
DEFINITIONS<br />
Policy Number: PNXX_303<br />
QOC Approval Date: 04/22/09<br />
PAGE 2 OF 10<br />
“Affected Member(s)” means a member(s) assigned to a terminating medical group or Primary Care<br />
Provider (PCP); members treated by a Specialty Care Practitioner (SCP) within the last 6 months; or<br />
members who reside within a 15-mile radius of a terminating hospital.<br />
“Continued Access to Care/Continuity of Care” means the process of authorizing continuation of<br />
services with a terminating physician, medical group or hospital under specified conditions and for<br />
a limited period of time with a plan of care to transition the member to a network provider.<br />
“Provider Contracting and Database Administration (PCDA)” is the department responsible for<br />
system updates and changes.<br />
“Hospital” means a general acute care hospital.<br />
“Medical Group” means a medical group, independent practice association or any other similar<br />
organization, reimbursed at a fee-for-service (FFS) or capitated per member per month (capitated)<br />
basis.<br />
“Member Notification Letter” means an appropriately approved letter being sent to members<br />
regarding a provider termination.<br />
“Physicians” means Primary Care Providers (PCP) or Specialty Care Providers (SCP) contracted<br />
either individually or through a Medical Group.<br />
“Provider” means an individual physician, medical group or hospital contracted with Anthem to<br />
provide services to Anthem members.<br />
PROCESS<br />
PCDA is responsible for receiving and processing termination notices from providers and tracking<br />
provider terminations internally.<br />
PCDA coordinates efforts with:<br />
• PCDA Reporting conducting impact analysis reports;<br />
• Compliance (regulatory approvals)<br />
• Health Care Management (Hospitals and Capitated Medical Groups)<br />
• Credentialing (terminations for cause)<br />
• Case Management (Continued Access to Care)<br />
• QI/Compliance Analyst (coordination of transition plan and member notification for groups and<br />
hospitals, coordinating the required notification to regulatory agencies, members and other<br />
interested parties)<br />
• PCDA Reporting (member mailing information)<br />
• Network Management and Field Operations (Professional Contracts)