ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
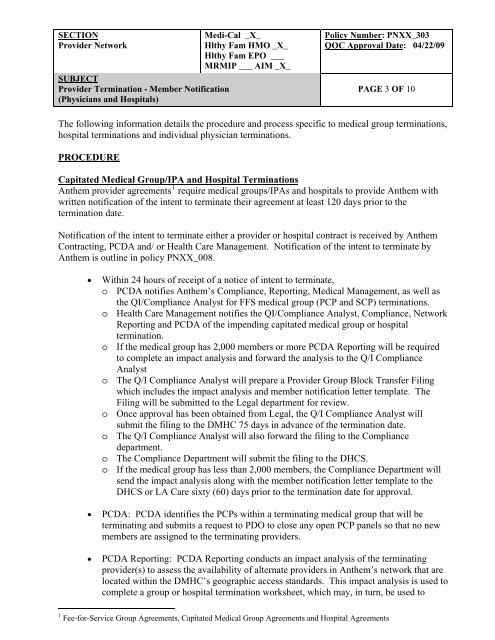
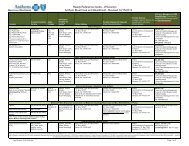
SECTION<br />
Medi-Cal _X_<br />
Provider Network<br />
Hlthy Fam HMO _X_<br />
Hlthy Fam EPO ___<br />
MRMIP ___ AIM _X_<br />
SUBJECT<br />
Provider Termination - Member Notification<br />
(Physicians and Hospitals)<br />
Policy Number: PNXX_303<br />
QOC Approval Date: 04/22/09<br />
PAGE 3 OF 10<br />
The following information details the procedure and process specific to medical group terminations,<br />
hospital terminations and individual physician terminations.<br />
PROCEDURE<br />
Capitated Medical Group/IPA and Hospital Terminations<br />
Anthem provider agreements 1 require medical groups/IPAs and hospitals to provide Anthem with<br />
written notification of the intent to terminate their agreement at least 120 days prior to the<br />
termination date.<br />
Notification of the intent to terminate either a provider or hospital contract is received by Anthem<br />
Contracting, PCDA and/ or Health Care Management. Notification of the intent to terminate by<br />
Anthem is outline in policy PNXX_008.<br />
• Within 24 hours of receipt of a notice of intent to terminate,<br />
o PCDA notifies Anthem’s Compliance, Reporting, Medical Management, as well as<br />
the QI/Compliance Analyst for FFS medical group (PCP and SCP) terminations.<br />
o Health Care Management notifies the QI/Compliance Analyst, Compliance, Network<br />
Reporting and PCDA of the impending capitated medical group or hospital<br />
termination.<br />
o If the medical group has 2,000 members or more PCDA Reporting will be required<br />
to complete an impact analysis and forward the analysis to the Q/I Compliance<br />
Analyst<br />
o The Q/I Compliance Analyst will prepare a Provider Group Block Transfer Filing<br />
which includes the impact analysis and member notification letter template. The<br />
Filing will be submitted to the Legal department for review.<br />
o Once approval has been obtained from Legal, the Q/I Compliance Analyst will<br />
submit the filing to the DMHC 75 days in advance of the termination date.<br />
o The Q/I Compliance Analyst will also forward the filing to the Compliance<br />
department.<br />
o The Compliance Department will submit the filing to the DHCS.<br />
o If the medical group has less than 2,000 members, the Compliance Department will<br />
send the impact analysis along with the member notification letter template to the<br />
DHCS or LA Care sixty (60) days prior to the termination date for approval.<br />
• PCDA: PCDA identifies the PCPs within a terminating medical group that will be<br />
terminating and submits a request to PDO to close any open PCP panels so that no new<br />
members are assigned to the terminating providers.<br />
• PCDA Reporting: PCDA Reporting conducts an impact analysis of the terminating<br />
provider(s) to assess the availability of alternate providers in Anthem’s network that are<br />
located within the DMHC’s geographic access standards. This impact analysis is used to<br />
complete a group or hospital termination worksheet, which may, in turn, be used to<br />
1 Fee-for-Service Group Agreements, Capitated Medical Group Agreements and Hospital Agreements