ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
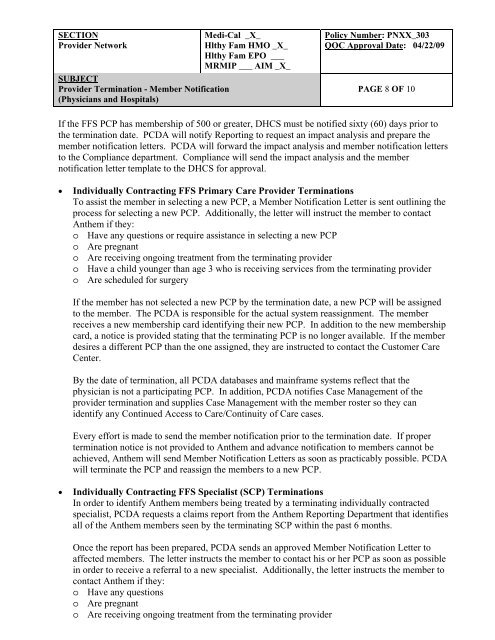
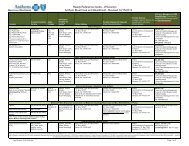
SECTION<br />
Medi-Cal _X_<br />
Provider Network<br />
Hlthy Fam HMO _X_<br />
Hlthy Fam EPO ___<br />
MRMIP ___ AIM _X_<br />
SUBJECT<br />
Provider Termination - Member Notification<br />
(Physicians and Hospitals)<br />
Policy Number: PNXX_303<br />
QOC Approval Date: 04/22/09<br />
PAGE 8 OF 10<br />
If the FFS PCP has membership of 500 or greater, DHCS must be notified sixty (60) days prior to<br />
the termination date. PCDA will notify Reporting to request an impact analysis and prepare the<br />
member notification letters. PCDA will forward the impact analysis and member notification letters<br />
to the Compliance department. Compliance will send the impact analysis and the member<br />
notification letter template to the DHCS for approval.<br />
• Individually Contracting FFS Primary Care Provider Terminations<br />
To assist the member in selecting a new PCP, a Member Notification Letter is sent outlining the<br />
process for selecting a new PCP. Additionally, the letter will instruct the member to contact<br />
Anthem if they:<br />
o Have any questions or require assistance in selecting a new PCP<br />
o Are pregnant<br />
o Are receiving ongoing treatment from the terminating provider<br />
o Have a child younger than age 3 who is receiving services from the terminating provider<br />
o Are scheduled for surgery<br />
If the member has not selected a new PCP by the termination date, a new PCP will be assigned<br />
to the member. The PCDA is responsible for the actual system reassignment. The member<br />
receives a new membership card identifying their new PCP. In addition to the new membership<br />
card, a notice is provided stating that the terminating PCP is no longer available. If the member<br />
desires a different PCP than the one assigned, they are instructed to contact the Customer Care<br />
Center.<br />
By the date of termination, all PCDA databases and mainframe systems reflect that the<br />
physician is not a participating PCP. In addition, PCDA notifies Case Management of the<br />
provider termination and supplies Case Management with the member roster so they can<br />
identify any Continued Access to Care/Continuity of Care cases.<br />
Every effort is made to send the member notification prior to the termination date. If proper<br />
termination notice is not provided to Anthem and advance notification to members cannot be<br />
achieved, Anthem will send Member Notification Letters as soon as practicably possible. PCDA<br />
will terminate the PCP and reassign the members to a new PCP.<br />
• Individually Contracting FFS Specialist (SCP) Terminations<br />
In order to identify Anthem members being treated by a terminating individually contracted<br />
specialist, PCDA requests a claims report from the Anthem Reporting Department that identifies<br />
all of the Anthem members seen by the terminating SCP within the past 6 months.<br />
Once the report has been prepared, PCDA sends an approved Member Notification Letter to<br />
affected members. The letter instructs the member to contact his or her PCP as soon as possible<br />
in order to receive a referral to a new specialist. Additionally, the letter instructs the member to<br />
contact Anthem if they:<br />
o Have any questions<br />
o Are pregnant<br />
o Are receiving ongoing treatment from the terminating provider