ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
ANTHEM BLUE CROSS STATE SPONSORED BUSINESS POLICY ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
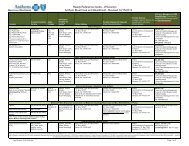
SECTION<br />
Medi-Cal _X_<br />
Provider Network<br />
Hlthy Fam HMO _X_<br />
Hlthy Fam EPO ___<br />
MRMIP ___ AIM _X_<br />
SUBJECT<br />
Provider Termination - Member Notification<br />
(Physicians and Hospitals)<br />
Policy Number: PNXX_303<br />
QOC Approval Date: 04/22/09<br />
PAGE 7 OF 10<br />
Contract Managers will be participate in all meetings related to large group or hospital<br />
terminations to facilitate contracts with alternative primary care and specialty providers.<br />
It is Anthem ’s practice to cease contract negotiations with a terminating medical<br />
group/IPA once the member notification has been sent. However, in the rare event an<br />
agreement is reached with a terminating medical group/IPA after the member notice has<br />
been sent, but within 30 days after the effective date of termination, Anthem will send a<br />
second notice to members (Attachment B) telling them that a new contract has been<br />
agreed upon and advising that if they would like to return to their prior PCP or medical<br />
group/IPA, then they may contact Blue Cross and request the change. Member notices<br />
advise that members may change PCPs or medical groups/IPAs by contacting Blue<br />
Cross.<br />
By the date of termination, all PCDA databases and mainframe systems reflect that the<br />
provider is no longer a participating provider.<br />
DMHC Waiver<br />
When a provider termination is immediate (due to death or illness of a provider; insolvency of a<br />
provider; or Anthem is provided with inadequate advance notice of the termination), Anthem can<br />
request a waiver of the 60 day notice requirement due to exigent circumstances. All previously<br />
outlined steps apply when a waiver is being requested (i.e., impact analysis and submission to<br />
Anthem Legal). The Q/I Compliance Analyst will submit the waiver to Anthem Legal for approval.<br />
Once Legal has approved the waiver request, the Q/I Compliance Analyst will submit the waiver<br />
request to the DMHC for approval.<br />
Tracking and Communication<br />
The QI/Compliance Analyst is responsible for tracking and maintaining all information regarding<br />
the termination. In addition, the QI/Compliance Analyst coordinates with Associate Development<br />
and Training (AD&T) to ensure that Anthem associates are made aware of information surrounding<br />
the terminations.<br />
AD&T provides communications to Anthem associates and provides any necessary training.<br />
Monthly Meetings<br />
The QI/Analyst conducts monthly meetings with all departments to discuss contract terminations;<br />
operational issues, and other critical information related to the provider/hospital termination<br />
process.<br />
Fee-for-Service (FFS) Physician Terminations<br />
Anthem’s contracts with fee-for-service physicians (PCPs and SCPs) require those physicians to<br />
notify Anthem at least 90 days prior to the termination date. Notification of the intent to terminate<br />
is received by PCDA. PCDA coordinates all aspects of the member notification for individual<br />
physician terminations. PCDA identifies the affected members and sends a Member Notification<br />
letter at least 30 days prior to the termination, indicating the effective date of the termination.