INTRODUCTION Granulomatous inflammation is a distinctive ...
INTRODUCTION Granulomatous inflammation is a distinctive ...
INTRODUCTION Granulomatous inflammation is a distinctive ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
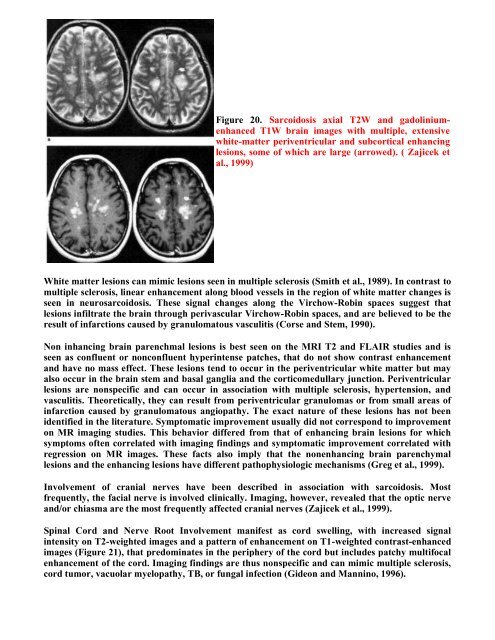
Figure 20. Sarcoidos<strong>is</strong> axial T2W and gadoliniumenhanced<br />
T1W brain images with multiple, extensive<br />
white-matter periventricular and subcortical enhancing<br />
lesions, some of which are large (arrowed). ( Zajicek et<br />
al., 1999)<br />
White matter lesions can mimic lesions seen in multiple scleros<strong>is</strong> (Smith et al., 1989). In contrast to<br />
multiple scleros<strong>is</strong>, linear enhancement along blood vessels in the region of white matter changes <strong>is</strong><br />
seen in neurosarcoidos<strong>is</strong>. These signal changes along the Virchow-Robin spaces suggest that<br />
lesions infiltrate the brain through perivascular Virchow-Robin spaces, and are believed to be the<br />
result of infarctions caused by granulomatous vasculit<strong>is</strong> (Corse and Stem, 1990).<br />
Non inhancing brain parenchmal lesions <strong>is</strong> best seen on the MRI T2 and FLAIR studies and <strong>is</strong><br />
seen as confluent or nonconfluent hyperintense patches, that do not show contrast enhancement<br />
and have no mass effect. These lesions tend to occur in the periventricular white matter but may<br />
also occur in the brain stem and basal ganglia and the corticomedullary junction. Periventricular<br />
lesions are nonspecific and can occur in association with multiple scleros<strong>is</strong>, hypertension, and<br />
vasculit<strong>is</strong>. Theoretically, they can result from periventricular granulomas or from small areas of<br />
infarction caused by granulomatous angiopathy. The exact nature of these lesions has not been<br />
identified in the literature. Symptomatic improvement usually did not correspond to improvement<br />
on MR imaging studies. Th<strong>is</strong> behavior differed from that of enhancing brain lesions for which<br />
symptoms often correlated with imaging findings and symptomatic improvement correlated with<br />
regression on MR images. These facts also imply that the nonenhancing brain parenchymal<br />
lesions and the enhancing lesions have different pathophysiologic mechan<strong>is</strong>ms (Greg et al., 1999).<br />
Involvement of cranial nerves have been described in association with sarcoidos<strong>is</strong>. Most<br />
frequently, the facial nerve <strong>is</strong> involved clinically. Imaging, however, revealed that the optic nerve<br />
and/or chiasma are the most frequently affected cranial nerves (Zajicek et al., 1999).<br />
Spinal Cord and Nerve Root Involvement manifest as cord swelling, with increased signal<br />
intensity on T2-weighted images and a pattern of enhancement on T1-weighted contrast-enhanced<br />
images (Figure 21), that predominates in the periphery of the cord but includes patchy multifocal<br />
enhancement of the cord. Imaging findings are thus nonspecific and can mimic multiple scleros<strong>is</strong>,<br />
cord tumor, vacuolar myelopathy, TB, or fungal infection (Gideon and Mannino, 1996).