INTRODUCTION Granulomatous inflammation is a distinctive ...
INTRODUCTION Granulomatous inflammation is a distinctive ...
INTRODUCTION Granulomatous inflammation is a distinctive ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Extraparenchymal space-occupying lesions are derived from the meninges or choroid plexus.<br />
They mostly occur in patients with concomitant lesions in the hypothalamic-pituitary ax<strong>is</strong> and<br />
may also be associated with neurodegenerative lesions. Symptoms depend on the site and size of<br />
the lesions and include headaches, seizures, vomiting, papilledema, optic nerve compression, or<br />
other focal symptoms (Martin et al., 2006)<br />
Affection of cerebellum, puns, basal ganglia or the cerebral grey and white matter <strong>is</strong> observed in<br />
1% of the overall LCH population and <strong>is</strong> associated with a neurodegenerative syndrome of highly<br />
variable severity and course. The symptoms range from subtle tremor or coordination problems<br />
to severe ataxia, dysarthria, and dysphagia, sometimes combined with intellectual impairment or<br />
behavioral changes. Eventually progressive neurological degeneration renders the patients<br />
wheelchair bound and severely d<strong>is</strong>abled and may lead to a fatal deterioration in the worst cases.<br />
Neuropsychological sequelae are frequently seen in LCH patients with CNS changes on MRI.<br />
Global cognitive deficits, as well as more specific changes in memory, concentration and attention<br />
have been observed. (Daniela et al., 2004)<br />
Investigations<br />
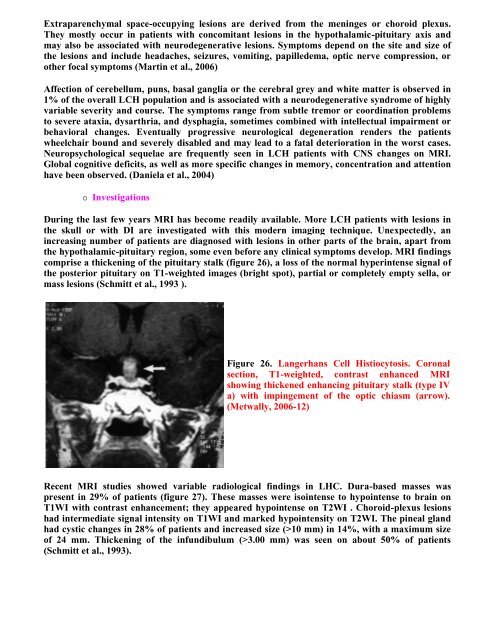
During the last few years MRI has become readily available. More LCH patients with lesions in<br />
the skull or with DI are investigated with th<strong>is</strong> modern imaging technique. Unexpectedly, an<br />
increasing number of patients are diagnosed with lesions in other parts of the brain, apart from<br />
the hypothalamic-pituitary region, some even before any clinical symptoms develop. MRI findings<br />
compr<strong>is</strong>e a thickening of the pituitary stalk (figure 26), a loss of the normal hyperintense signal of<br />
the posterior pituitary on T1-weighted images (bright spot), partial or completely empty sella, or<br />
mass lesions (Schmitt et al., 1993 ).<br />
Figure 26. Langerhans Cell H<strong>is</strong>tiocytos<strong>is</strong>. Coronal<br />
section, T1-weighted, contrast enhanced MRI<br />
showing thickened enhancing pituitary stalk (type IV<br />
a) with impingement of the optic chiasm (arrow).<br />
(Metwally, 2006-12)<br />
Recent MRI studies showed variable radiological findings in LHC. Dura-based masses was<br />
present in 29% of patients (figure 27). These masses were <strong>is</strong>ointense to hypointense to brain on<br />
T1WI with contrast enhancement; they appeared hypointense on T2WI . Choroid-plexus lesions<br />
had intermediate signal intensity on T1WI and marked hypointensity on T2WI. The pineal gland<br />
had cystic changes in 28% of patients and increased size (>10 mm) in 14%, with a maximum size<br />
of 24 mm. Thickening of the infundibulum (>3.00 mm) was seen on about 50% of patients<br />
(Schmitt et al., 1993).