INTRODUCTION Granulomatous inflammation is a distinctive ...
INTRODUCTION Granulomatous inflammation is a distinctive ...
INTRODUCTION Granulomatous inflammation is a distinctive ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
the appearance of pulmonary lesions <strong>is</strong> relatively specific for sarcoidos<strong>is</strong>. Sites of <strong>inflammation</strong><br />
can be accessed for directed biopsy. The combination of gallium 67 scanning and Serum ACE<br />
levels yields a specificity of 83% to 99%, thus making the combination an excellent, minimally<br />
invasive evaluation for sarcoidos<strong>is</strong> (Corse and stem, 1990).<br />
Ultimately, in cases where the diagnos<strong>is</strong> of neurosarcoidos<strong>is</strong> <strong>is</strong> in doubt despite the above<br />
evaluation, t<strong>is</strong>sue biopsy from neural lesions should be considered. The common sites for biopsy<br />
are the meninges and mass lesions. The sensitivity of meningeal biopsy improves if there <strong>is</strong><br />
enhancement on contrast imaging. In the case of focal meningeal enhancement, the imaging<br />
studies should be used to choose the site for biopsy. In case the biopsy from a cerebral mass lesion<br />
shows evidence of noncaseating granulomata, cultures should be obtained to rule out infection as a<br />
cause. A generous sample of t<strong>is</strong>sue should be obtained, because granulomatous changes can be<br />
seen around primary cerebral tumors (Peeples et al., 1991).<br />
Treatment<br />
Unlike pulmonary sarcoidos<strong>is</strong>, where a period of observation <strong>is</strong> recommended for mild and<br />
asymptomatic cases (Hunninghake et al., 1994), neurosarcoidos<strong>is</strong> patients almost always should be<br />
treated on diagnos<strong>is</strong>. Much of the information regarding specific treatment of neurosarcoidos<strong>is</strong><br />
comes from multiple case reports and small case series. Otherw<strong>is</strong>e, most treatment choices are<br />
made based on studies of systemic sarcoidos<strong>is</strong> (Agbougu et al., 1995).<br />
Immunosuppression <strong>is</strong> the principal method of controlling the d<strong>is</strong>ease, and corticosteroids are the<br />
cornerstone of therapy. Spontaneous rem<strong>is</strong>sion has been observed. Relapses may respond poorly,<br />
however, requiring chronic steroid therapy. Before initiating immunosuppressive therapy, an<br />
infectious etiology for the symptoms must be excluded (Bucurescu, 2006).<br />
Role of lmmunotherapies<br />
Treatment with corticosteroids has shown impressive responses in many cases. Postulated<br />
mechan<strong>is</strong>ms of action include inhibition of lymphocyte and mononuclear phagocytic activity,<br />
inhibition of transcription of proinflammatory cytokines, down regulation of important cellular<br />
receptors, and interference with collagen synthes<strong>is</strong>. Although steroids have a biological use in<br />
sarcoidos<strong>is</strong>, there <strong>is</strong> no evidence that they change the natural h<strong>is</strong>tory and outcome of the illness.<br />
The main goal of treatment <strong>is</strong> to salvage t<strong>is</strong>sue function and prevent progression of the d<strong>is</strong>ease,<br />
especially fibros<strong>is</strong> and <strong>is</strong>chemia. Corticosteroids should be started in high doses and, after a<br />
clinical response occurs, gradually tapered, similar to their use in other inflammatory conditions<br />
(Chapelon et al., 1990). Complete withdrawal can be attempted if the clinical course permits. In<br />
case of relapse, a repeat course of high-dose steroid treatment should be attempted. Patients<br />
should be monitored for complications and treated appropriately. It <strong>is</strong> very important to reduce<br />
the morbidity related to the treatment to avoid d<strong>is</strong>continuation of the medication because of side<br />
effects. In one study, only 29% of patients with neurosarcoidos<strong>is</strong> continued long-term steroids; the<br />
remainder d<strong>is</strong>continued treatment because of intolerable side effects or failure to respond. (Lower<br />
et al., 1997)<br />
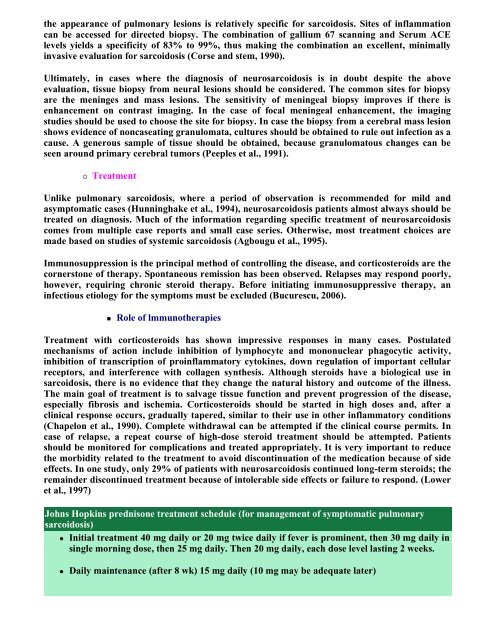
Johns Hopkins predn<strong>is</strong>one treatment schedule (for management of symptomatic pulmonary<br />
sarcoidos<strong>is</strong>)<br />
Initial treatment 40 mg daily or 20 mg twice daily if fever <strong>is</strong> prominent, then 30 mg daily in<br />
single morning dose, then 25 mg daily. Then 20 mg daily, each dose level lasting 2 weeks.<br />
Daily maintenance (after 8 wk) 15 mg daily (10 mg may be adequate later)