Seanchara Community Unit, 515, nursing home inspection ... - hiqa.ie
Seanchara Community Unit, 515, nursing home inspection ... - hiqa.ie
Seanchara Community Unit, 515, nursing home inspection ... - hiqa.ie
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
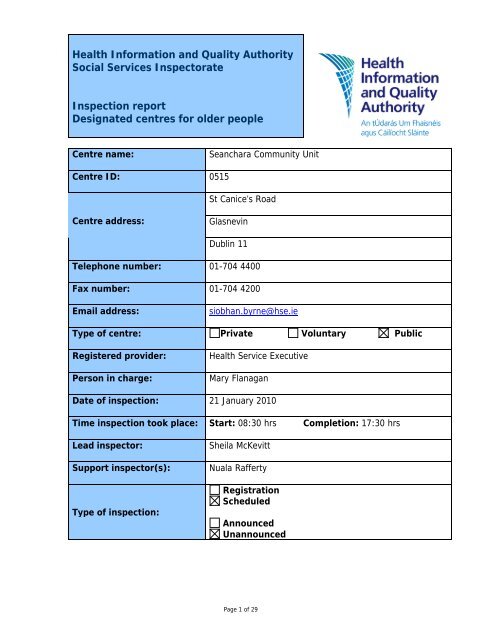
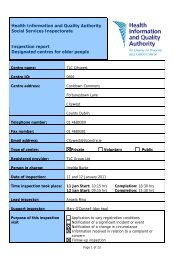
Health Information and Quality Authority<br />
Social Services Inspectorate<br />
Inspection report<br />
Designated centres for older people<br />
Centre name: <strong>Seanchara</strong> <strong>Community</strong> <strong>Unit</strong><br />
Centre ID:<br />
Centre address:<br />
0<strong>515</strong><br />
St Canice’s Road<br />
Glasnevin<br />
Dublin 11<br />
Telephone number: 01-704 4400<br />
Fax number: 01-704 4200<br />
Email address: siobhan.byrne@hse.<strong>ie</strong><br />
Type of centre: Private Voluntary Public<br />
Registered provider: Health Service Executive<br />
Person in charge: Mary Flanagan<br />
Date of <strong>inspection</strong>: 21 January 2010<br />
Time <strong>inspection</strong> took place:<br />
Lead inspector: Sheila McKevitt<br />
Support inspector(s): Nuala Rafferty<br />
Type of <strong>inspection</strong>:<br />
Start: 08:30 hrs Completion: 17:30 hrs<br />
Registration<br />
Scheduled<br />
Announced<br />
Unannounced<br />
Page 1 of 29
About <strong>inspection</strong><br />
The purpose of <strong>inspection</strong> is to gather evidence on which to make judgments about<br />
the fitness of the registered provider and to report on the quality of the service. This<br />
is to ensure that providers are complying with the requirements and conditions of<br />
their registration and meet the standards; that they have systems in place to both<br />
safeguard the welfare of service users and to provide information and evidence of<br />
good and poor practice.<br />
In assessing the overall quality of the service provided, inspectors examine how well<br />
the provider has met the requirements of the Health Act 2007, the Health Act 2007<br />
(Care and Welfare of Residents in Designated Centres for Older People) Regulations<br />
2009 and the National Quality Standards for Residential Care Settings for Older<br />
People in Ireland under the following topics:<br />
1. Governance and leadership: how well the centre is organised.<br />
2. The quality of the service.<br />
3. How well the healthcare needs of residents are met.<br />
4. Premises and equipment: appropriateness and adequacy.<br />
5. Communication: information provided to residents, relatives and staff.<br />
6. Staffing: the recruitment, supervision and competence of staff.<br />
This report summarises the findings of the <strong>inspection</strong> under some or all of these<br />
topics, highlighting areas of good practice as well as areas where improvements<br />
were required as follows:<br />
Evidence of good practice – this means that an acceptable standard was reached<br />
and the provider demonstrated a culture of rev<strong>ie</strong>w and improvement and aimed to<br />
drive forward best practice.<br />
Some improvements required – this means that practice was generally<br />
satisfactory but there were areas that need attention.<br />
Significant improvements required – this means that unacceptable practice was<br />
found.<br />
The report also identif<strong>ie</strong>s minor issues, where applicable, to which the provider<br />
should give consideration to enhance the quality of the service.<br />
The report is available to residents, relatives, providers of services and members of<br />
the public, and is published on our website www.<strong>hiqa</strong>.<strong>ie</strong>.<br />
Acknowledgements<br />
The inspectors wish to acknowledge the cooperation and assistance of the residents,<br />
relatives, provider and staff during the <strong>inspection</strong>.<br />
Page 2 of 29
About the centre<br />
Description of services and premises<br />
Claremont Residential and <strong>Community</strong> Services are based in Dublin North Central.<br />
The services are divided into three units and <strong>Seanchara</strong> <strong>Community</strong> <strong>Unit</strong> is one of<br />
these.<br />
Clarehaven Home, Anam Chara housing care unit and a day care facility are all<br />
situated on the same site. The latter two are directly accessible via a lift from<br />
<strong>Seanchara</strong> <strong>Community</strong> <strong>Unit</strong>.<br />
<strong>Seanchara</strong> <strong>Community</strong> <strong>Unit</strong> is a 48-bedded purpose-built single-storey residential unit<br />
for people over the age of 65 years.<br />
There are six single bedrooms, five twin rooms and eight four-bedded rooms spread<br />
over two wings. Four of the single rooms share two en suites showers and toilets.<br />
There are three large sitting rooms, two of which are also used as dining space.<br />
There is one large dining room accessible directly from one of the sitting rooms.<br />
There is one main kitchen and a kitchenette for each wing. Staff have their own<br />
restaurant, rest room and changing facilit<strong>ie</strong>s.<br />
Other facilit<strong>ie</strong>s include an oratory, a visitors’ room, an activit<strong>ie</strong>s room, a snozelen<br />
room, a physiotherapy room, a complimentary therapy room, a reception area, a<br />
porters desk and administration offices.<br />
There are two enclosed gardens, one accessible off each wing which residents can<br />
access freely.<br />
There are ample car parking around the building.<br />
Location<br />
<strong>Seanchara</strong> <strong>Community</strong> <strong>Unit</strong> is situated in parish of Ballygall, Glasnevin, Dublin. It is<br />
located in a residential area.<br />
Dependency level of<br />
current residents<br />
Number of residents<br />
Management structure<br />
Max High Medium Low<br />
16 12 7 2<br />
The nominee on behalf of the Health Service Executive (HSE) is Gerry Reid who<br />
reports to the Local Health Officer, Mary Maguire. Jim O’ Riordan, Manager of<br />
Services, Pat Lane, Administration Manager and Mary Flanagan, the Person in Charge<br />
all report to Gerry Reid. The Assistant Director of Nursing, the Practice Development<br />
Page 3 of 29
Officer and the Catering Manager, report to the Person in Charge. Administration<br />
staff report to Pat Lane.<br />
The Assistant Director of Nursing and the Practice Development Officer are<br />
supported by two Clinical Nurse Managers grade II and two Clinical Nurse Managers<br />
grade I to whom all staff nurses and care assistants report. The catering staff report<br />
to the catering manager.<br />
A contract cleaning company supply the cleaning staff and they report to a company<br />
supervisor.<br />
Staff<br />
designation<br />
Number of<br />
staff on duty<br />
on day of<br />
<strong>inspection</strong><br />
Person<br />
in<br />
Charge<br />
1 9<br />
Nurses Care<br />
staff<br />
3 7<br />
Page 4 of 29<br />
Catering<br />
staff<br />
Cleaning<br />
and<br />
laundry<br />
staff<br />
6<br />
Admin<br />
staff<br />
2<br />
Other<br />
Staff<br />
4
Summary of findings from this <strong>inspection</strong><br />
The <strong>inspection</strong> was unannounced and took place over the course of one day. It was<br />
the first <strong>inspection</strong> of this centre by the Health Information and Quality Authority<br />
(the Authority).<br />
Residents received appropriate healthcare including access to all<strong>ie</strong>d heath<br />
professionals. Attention to assessment was good and the involvement of residents<br />
and their famil<strong>ie</strong>s in the care planning process was evident. Nursing documentation<br />
was of a good standard. There were facilit<strong>ie</strong>s in place to support end of life care<br />
including the facility for family members to stay over night.<br />
Staff demonstrated their respect for the privacy and dignity of residents and staff<br />
supported residents to maximise their independence. Daily routines and care<br />
practices encouraged the residents to exercise choice. There were a var<strong>ie</strong>ty of<br />
organised and informal activit<strong>ie</strong>s which made the day interesting and fulfilling for<br />
residents. Religious practice was facilitated.<br />
Inspectors found that staffing levels and skills mix were adequate to meet the needs<br />
of residents. Staff were supported in their work by ongoing training, supervision, and<br />
opportunit<strong>ie</strong>s for professional development, including access to a staff library.<br />
However, at the time of <strong>inspection</strong> not all staff had completed training in elder<br />
abuse.<br />
Good levels of cleanliness and hyg<strong>ie</strong>ne were maintained and infection control<br />
measures were thorough. Bedrooms were personalised and communal areas were<br />
nicely decorated with soft furnishings and residents’ art work. Excellent signage<br />
supported those residents who were cognitively impaired. However, there were<br />
insuffic<strong>ie</strong>nt numbers of showers/bathrooms to meet the needs of residents.<br />
There were a number of other areas which required improvement. There was no risk<br />
management plan in place although two areas of risk were identif<strong>ie</strong>d on <strong>inspection</strong>.<br />
These relate to radiators that were very hot and posed a risk to residents and the<br />
storage of medication. Improvements were also needed to ensure that all<br />
documentation was comprehensive, met the requirements of regulation, and where<br />
appropriate, was made available to residents. More robust recording of residents’<br />
finances was required. These issues are discussed in the report and included in the<br />
action plan at the end of the report.<br />
Residents’ and relatives’ comments<br />
Inspectors spoke to 11 residents over the course of the <strong>inspection</strong>. These residents<br />
spoke very highly of staff, particularly of their pat<strong>ie</strong>nt and kind approach.<br />
A number of residents stated that they enjoyed living in <strong>Seanchara</strong> and that even<br />
though they had good fun between themselves, there was no place like their own<br />
<strong>home</strong>.<br />
Page 5 of 29
Residents stated that they had choice over their daily routine and how they lived<br />
their lives.<br />
One issue raised during <strong>inspection</strong> was that some residents felt that lunch was<br />
served too early. This issue was brought to the attention of the person in charge at<br />
the feedback meeting.<br />
Page 6 of 29
Overall findings<br />
1. Governance: how well the centre is organised<br />
Outcome: The centre is well organised and managed and compl<strong>ie</strong>s with the<br />
requirements of the Health Act 2007, the regulations and standards.<br />
Good governance involves the effective and effic<strong>ie</strong>nt deployment of<br />
resources in accordance with the stated purpose and function of the<br />
centre. Governance includes setting clear direction for the service, a<br />
commitment to continual improvement and having a system in place to<br />
effectively assess and manage risk.<br />
Evidence of good practice<br />
The person in charge demonstrated good leadership and was actively involved in the<br />
day to day operation of the centre.<br />
A clear organisational structure was in place. All staff interv<strong>ie</strong>wed demonstrated a<br />
good understanding of their roles and responsibilit<strong>ie</strong>s and were able to describe the<br />
staff structure and the reporting mechanisms in place to ensure appropriate<br />
delegation, supervision and competence in the delivery of care to residents.<br />
There was a very clear and concise emergency plan in place. The responsibilit<strong>ie</strong>s of<br />
staff in the event of an emergency was precise. Staff spoken to displayed a good<br />
understanding of their role in the plan.<br />
The health and safety statement was assessed as being in line with the regulatory<br />
requirement. The health and safety committee, which comprised staff, met on a<br />
regular basis.<br />
The quality of care provided was audited monthly by management on the following<br />
areas of practice: falls sustained by residents, forms of restraint used, pressure<br />
ulcers, residents with infections and any other new infections. Information from the<br />
audit was then used to inform future practice.<br />
Some improvements required<br />
The statement of purpose did not meet the legislative requirement. A draft format<br />
was rev<strong>ie</strong>wed by inspectors. However, it did not contain all the information required<br />
as per schedule one of the Health Act 2007 (Care and Welfare of Residents in<br />
Designated Centres for Older People) Regulations 2009.<br />
Page 7 of 29
Significant improvements required<br />
A risk management policy was not available.<br />
The radiators on the corridors posed a potential risk to residents as they were very<br />
hot to touch.<br />
Access to the key of the safe, where residents’ money was stored, was not secure.<br />
The receptionist stated the key was stored in a locked filing cabinet. The key of the<br />
filing cabinet was kept in an unlocked drawer within a key-coded office. However, a<br />
number of staff members had access to this office and therefore had access to the<br />
key.<br />
The record of residents’ money was not being kept in an accurate or confidential<br />
manner. A large brown envelope with columns for cash in, out, running total and<br />
received by, was in place for each individual resident who had cash held in the safe.<br />
The inspector rev<strong>ie</strong>wed residents’ individual brown envelopes and found what was<br />
written on the envelope did not accurately reflect the amount of cash within the<br />
envelope.<br />
Residents whose relatives collected their weekly cash allowance were requested to<br />
sign on a pre-printed sheet of paper. This sheet of paper showed details of other<br />
residents’ names and weekly cash allowance and therefore did not maintain their<br />
privacy.<br />
Insurance documentation was available for <strong>inspection</strong>. However, it did not include<br />
the name of the centre; the inspector could not identify the centre by the code on<br />
the insurance document. It did not state that liability to any resident shall not exceed<br />
€1,000 for any one item except where the property was deposited.<br />
A draft contract of care was available for rev<strong>ie</strong>w, however a contract of care had not<br />
been sent to individual residents. The person in charge stated that this document<br />
was being finalised and would be given out to residents as soon as it was completed.<br />
Page 8 of 29
2. Quality of the service<br />
Outcome: Residents receive a good standard of service, appropriate<br />
treatment and are treated with courtesy and respect.<br />
A quality service is one where residents are protected from harm or abuse,<br />
where practice is person-centred, where rights are protected, where<br />
residents are enabled to play an active part in the centre and where<br />
management, staff and residents work together towards continuous<br />
improvement.<br />
Evidence of good practice<br />
Residents stated that staff were very courteous towards them. They called them by<br />
their name and respected their dignity and privacy. Inspectors observed staff<br />
drawing curtains around beds in shared rooms prior to attending to residents, and<br />
ensuring that the shower door was closed prior to assisting the resident within.<br />
Cleaning staff were observed knocking on bedroom doors prior to entering.<br />
Staff promoted residents’ independence. Inspectors observed staff providing<br />
assistance to residents at lunch time. This was done in a very relaxed, unrushed<br />
manner. Staff were seen to observe some residents closely allowing them the<br />
opportunity to be independent or offering assistance as required. All condiments<br />
were within residents’ reach so independence could be maintained.<br />
Residents could exercise choice in their daily routines. They could stay in bed if they<br />
so wished. One lady who was in bed stated she “worked hard enough” - some days<br />
she got up and some days she stayed in bed, “it was her liking”. Another resident<br />
said they had a choice of meals and staff came around prior to meal time to check<br />
the residents’ preference.<br />
Residents informed inspectors that sometimes they were offered a plain omelette,<br />
burger or pancake and then were given a choice of ingred<strong>ie</strong>nts to garnish them with.<br />
They enjoyed this choice as “you could have what filling you liked”.<br />
Residents’ religious needs were catered for. Residents had their own oratory. Daily<br />
mass was transmitted from the parish church across the road to a flat screen<br />
television. Funerals and other religious events were also relayed and residents<br />
informed inspectors that they enjoyed this service.<br />
Two residents informed the inspector that they lead the rosary together every<br />
evening in the sitting room. The chaplain stated that she offered Holy Communion to<br />
residents on a weekly basis.<br />
The chaplain, a member of the local community, provided support to residents and<br />
their famil<strong>ie</strong>s whenever required. On the day of <strong>inspection</strong>, the chaplain was<br />
supporting the family of a resident who was receiving end-of-life care. Staff stated<br />
Page 9 of 29
that the chaplain provided a great service as she lived locally and was able to attend<br />
the centre within a short period of time. The chaplain informed inspectors that she<br />
ran a monthly family support group meeting which was well attended by residents’<br />
famil<strong>ie</strong>s and also provided bereavement support to residents’ relatives.<br />
Some improvements required<br />
Privacy of residents’ documents was not being maintained. Residents’ care plans<br />
were stored over their beds in their shared bedrooms.<br />
There was no advocate or advocacy service available to residents.<br />
Significant improvements required<br />
Residents informed inspectors that they had monthly meetings and if they wanted<br />
anything done, this was raised at these meetings. Inspectors rev<strong>ie</strong>wed minutes and<br />
noted that previous meeting minutes were not revisited. Two residents informed<br />
inspectors that they felt lunch was too early and that they had brought up the issue<br />
in September 2009. However, they had heard nothing since then and lunch continues<br />
to be served at noon.<br />
Page 10 of 29
3. Healthcare needs<br />
Outcome: Residents’ healthcare needs are met.<br />
Healthcare is integral to meeting individual’s needs. It requires that<br />
residents’ health, personal and social care needs are assessed and<br />
rev<strong>ie</strong>wed on an on-going basis, within a care planning process, that is<br />
person centred. Emphasis is firmly placed on health promotion,<br />
independence and meaningful activity.<br />
Evidence of good practice<br />
The <strong>nursing</strong> documentation was of a good standard. Each resident was fully assessed<br />
on admission and re-assessed three monthly thereafter. Inspectors rev<strong>ie</strong>wed some<br />
residents’ care plans which reflected their social and personal needs and these were<br />
rev<strong>ie</strong>wed on a three-monthly basis. The involvement of residents and their famil<strong>ie</strong>s in<br />
the care planning process was evident.<br />
There was evidence that residents received appropriate medical care. Medical<br />
records indicated that residents were rev<strong>ie</strong>wed on a regular basis. Evidence of<br />
hospital appointments and investigation results were available in their records. Staff<br />
nurses and the medical practitioner rev<strong>ie</strong>wed medications on a three-monthly basis.<br />
Residents stated that they saw the doctor whenever they wanted.<br />
End-of-life care was well managed. Personnel from the local hospice had provided<br />
training on end-of-life care to staff. Services from this hospice were available to, and<br />
often sought for, residents in <strong>Seanchara</strong>.<br />
There was a portable bed available in the visitors’ room for residents’ famil<strong>ie</strong>s to stay<br />
over if they so requested. Famil<strong>ie</strong>s had the option to have their relative waked in the<br />
oratory if this was their preference. Residents told inspectors that when a person<br />
d<strong>ie</strong>d, they rested overnight in the chapel.<br />
There was a physiotherapist, an occupational therapist, a speech and language<br />
therapist and a d<strong>ie</strong>tician employed and available to residents on referral.<br />
Significant improvements required<br />
Medications were not securely stored. The door of the storage room where the drug<br />
trolleys were stored did not close fully and the drug trolleys were not secured to the<br />
wall of the storeroom.<br />
The process of documentation relating to resuscitation was not been practiced<br />
according to the units’ policy. Records of discussions between residents, their<br />
relatives, doctors and nurses, did not state who attended or exactly what was<br />
discussed.<br />
Page 11 of 29
4. Premises and equipment: appropriateness and adequacy<br />
Outcome: The residential care setting provides premises and equipment<br />
that are safe, secure and suitable.<br />
A good physical environment is one that enhances the quality of life for<br />
residents and is a pleasant place to live. It meets residents’ individual and<br />
collective needs in a comfortable and <strong>home</strong>ly way, and is accessible, safe,<br />
clean and well maintained. Equipment is provided in response to the<br />
assessed needs of each of the residents and maintained appropriately.<br />
Evidence of good practice<br />
There was a good standard of hyg<strong>ie</strong>ne. All areas were seen to be extremely clean,<br />
tidy and clutter-free.<br />
There was excellent signage to help residents or<strong>ie</strong>ntate themselves. Doors had large<br />
pictures of the facilit<strong>ie</strong>s provided within the room and/or large written words<br />
attached.<br />
There was a choice of activit<strong>ie</strong>s available on a daily basis as well as evening and<br />
weekend activit<strong>ie</strong>s. The activit<strong>ie</strong>s timetable was displayed on notice boards in each<br />
wing and in the main corridor. Fourteen residents were observed playing skittles with<br />
the activit<strong>ie</strong>s co-ordinator. One resident said she liked the hand massage, another<br />
resident stated that she loved the skittles and bingo. One resident informed the<br />
inspector that she was going shopping in Finglas the following day with the activit<strong>ie</strong>s<br />
co-ordinator.<br />
The infection control measures in place were thorough. Personal protective clothing<br />
was available for staff in each sluice, cleaning room and outside the rooms of<br />
residents who had infections. Inspectors observed that adequate hand-washing<br />
facilit<strong>ie</strong>s and sterilising hand gel were available for staff. Staff were seen washing<br />
their hands between caring for residents.<br />
The kitchen was kept in pristine condition. The inspector observed a large and<br />
diverse amount of dry, fresh and frozen food stored for residents’ use.<br />
Corridors, communal sittings and dining rooms were nicely decorated with soft<br />
furnishings and residents’ art work. Residents’ bedrooms had personal photos and<br />
pictures hanging on their walls. Residents in shared bedrooms had their bed areas<br />
personalised.<br />
Significant improvements required<br />
The centre is not fit for purpose in regard to the provision of sanitary facilit<strong>ie</strong>s for<br />
residents. There are an insuffic<strong>ie</strong>nt number of showers/bathrooms to meet the<br />
required needs of residents.<br />
Page 12 of 29
5. Communication: information provided to residents, relatives<br />
and staff<br />
Outcome: Information is relevant, clear and up to date for residents.<br />
Information is accessible, accurate, and appropriate to residents’ and staff<br />
needs. Feedback is actively sought from residents and relatives and this<br />
informs future planning and service provision. Information is recorded and<br />
maintained in accordance with legal requirements and best practice and is<br />
communicated to staff on a need to know basis to ensure residents’<br />
privacy is respected.<br />
Evidence of good practice<br />
There was lots of literature on services available to residents, an information booklet<br />
for Claremount residential and <strong>Community</strong> Services was available to residents, which<br />
included information about <strong>Seanchara</strong> <strong>Community</strong> <strong>Unit</strong>. A brochure was also<br />
available.<br />
There was a stand near the porters’ desk which contained numerous leaflets on<br />
services and information available to older persons.<br />
A var<strong>ie</strong>ty of books were available and residents had access to televisions in each of<br />
the sitting rooms and in some of the bedrooms.<br />
A folder with information for relatives was available at the front desk by the visitors’<br />
sign-in book. This included a booklet on dementia and Alzheimer’s care, end-of-life<br />
care, and a booklet on mental health.<br />
There was a notice board for residents on each wing and on the main corridor. These<br />
contained information about the next residents’ committee meeting, bereavement<br />
support group, family support group and activit<strong>ie</strong>s timetable.<br />
Communication between staff was good. Staff meetings took place on a monthly<br />
basis, minutes of which were rev<strong>ie</strong>wed by inspectors. There was a multi-disciplinary<br />
managers meeting on a monthly basis. Prior to this meeting there was a journal club<br />
where a staff member presented a research paper to the group, to which all staff<br />
were invited.<br />
Some improvements required<br />
The good practice in relation to communication was not supported with a policy for<br />
the provision of information to residents. The Residents’ Guide did not include all the<br />
information required.<br />
Page 13 of 29
Significant improvements required<br />
There were no telephone facilit<strong>ie</strong>s which residents could access in private. If a<br />
resident wanted to make a call, they had to ask a member of staff for use of the<br />
portable telephone or alternatively, they could use a public phone available on the<br />
corridor.<br />
Page 14 of 29
6. Staff: the recruitment, supervision and competence of staff<br />
Outcome: Staff are competent and recruited in suffic<strong>ie</strong>nt numbers to meet<br />
residents’ needs<br />
Staff numbers and skill-mix are determined by the size and complexity of<br />
the service and there should be suffic<strong>ie</strong>nt competent staff on duty, both<br />
day and night, to meet the needs of residents. Robust recruitment and<br />
selection procedures ensure the appointment of suitably qualif<strong>ie</strong>d and<br />
exper<strong>ie</strong>nced staff. Staff are supported in their work by ongoing training<br />
and supervision.<br />
Evidence of good practice<br />
Three staff files were rev<strong>ie</strong>wed by the inspector all contained the required documents<br />
together with a contract of employment and a job description.<br />
There was good <strong>nursing</strong> supervision. Each wing had a clinical nurse manager on duty<br />
every day and they were supported by the Assistant Director of Nursing. A number of<br />
staff nurses and care assistants working on each wing supported the clinical nurse<br />
managers. Catering and domestic staff both had supervisors to support them.<br />
Inspectors found that staffing levels and skill mix were adequate to meet the needs<br />
of residents.<br />
The unit facilitated both pre and post registration students from two different<br />
colleges. There was a staff library containing a number of research journals and<br />
relevant textbooks available to staff and students. This ensured that staff working<br />
with residents had access to the theory to support the <strong>nursing</strong> care they provided.<br />
All staff had received moving and handling, fire and cardio-pulmonary resuscitation<br />
(CPR) training. Evidence that staff had received training on continence promotion,<br />
prevention of constipation, medication, care planning, falls prevention, nutrition, nonviolent<br />
crisis intervention together with phlebotomy training and preceptor training<br />
was provided to inspectors.<br />
A number of staff had received elder abuse training. Names of those who had<br />
attended recent training was available to inspectors and dates of future planned<br />
training was also provided.<br />
There were a number of working groups established. These included:<br />
continence promotion<br />
restraint<br />
activit<strong>ie</strong>s<br />
falls<br />
Page 15 of 29
dementia.<br />
health, safety and quality<br />
policy committee.<br />
New staff were supernumerary for their first week of employment. They were<br />
provided with an introduction folder and checklist. This had to be completed by the<br />
end of their probationary period which was usually three months.<br />
Staff had professional development plans completed on an annual basis. Inspectors<br />
noted completed plans in staff files.<br />
Changing facilit<strong>ie</strong>s were available for staff. Staff had there own separate restaurant<br />
and rest room.<br />
Some improvements required<br />
A number of staff had received elder abuse training. Names of those who had<br />
attended recent training was available to inspectors and dates of future planned<br />
training was provided to inspectors. However, a number of staff have yet to receive<br />
this training.<br />
Minor issues to be addressed<br />
There was a high use of agency staff. On the day of <strong>inspection</strong> eight agency staff<br />
had signed the agency sign-in book v<strong>ie</strong>wed by the inspector. All agency staff could<br />
not be identif<strong>ie</strong>d on the staff rota.<br />
Report compiled by:<br />
Sheila McKevitt<br />
Inspector of Social Services<br />
Social Services Inspectorate<br />
Health Information and Quality Authority<br />
26 January 2010<br />
Page 16 of 29
Health Information and Quality Authority<br />
Social Services Inspectorate<br />
Action Plan<br />
Provider’s response to <strong>inspection</strong> report<br />
Centre: <strong>Seanchara</strong> <strong>Community</strong> Centre<br />
Centre ID: 0<strong>515</strong><br />
Date of <strong>inspection</strong>:<br />
Date of response:<br />
Requirements<br />
21 January 2010<br />
22 February 2010<br />
These requirements set out what the registered provider must do to meet the Health<br />
Act 2007, the Health Act 2007 (Care and Welfare of Residents in Designated Centres<br />
for Older People) Regulations 2009 and the National Quality Standards for<br />
Residential Care Settings for Older People in Ireland.<br />
1. The provider is failing to comply with a regulatory requirement in the<br />
following respect:<br />
The statement of purpose does not meet the regulatory requirements.<br />
Action required:<br />
Rev<strong>ie</strong>w the statement of purpose and ensure it specifically reflects the centre, its aims,<br />
objectives and ethos together with all items outlined in schedule one of the Health Act<br />
2007(Care and Welfare of Residents in Designated Centres for Older People) Regulations<br />
2009.<br />
Reference:<br />
Health Act, 2007<br />
Regulation 5: Statement of Purpose<br />
Standard 28: Purpose and Function<br />
Page 17 of 29
Please state the actions you have taken or are planning to<br />
take with timescales:<br />
Provider’s response:<br />
The statement of purpose and function is currently being rev<strong>ie</strong>wed<br />
to ensure that it specifically reflects the unit and contains all items<br />
outlined in schedule one of the Health Act 2007 (Care and Welfare<br />
of Residents in Designated Centres for Older People) Regulations<br />
2009.<br />
Page 18 of 29<br />
Timescale:<br />
February 2010<br />
2. The provider is failing to comply with a regulatory requirement in the<br />
following respect:<br />
There is no advocate or advocate service available for residents’ use.<br />
Action required:<br />
Put in place a mechanism where residents have access to an advocate or advocacy<br />
service.<br />
Reference:<br />
Health Act, 2007<br />
Regulation 10: Residents’ Rights, Dignity and Consultation<br />
Standard 3: Privacy and Dignity<br />
Please state the actions you have taken or are planning to<br />
take with timescales:<br />
Provider’s response:<br />
The unit management recognised this gap existed and advised the<br />
inspectors on the day of the <strong>inspection</strong> that the Director of Nursing<br />
cancelled an appointment that day with the programme manager of<br />
the National Advocacy Programme. She has since met with her and<br />
a volunteer advocate has been identif<strong>ie</strong>d. The volunteer advocate<br />
has commenced her training programme and will start her work<br />
placement in the unit in March.<br />
Timescale:<br />
March 2010
3. The provider is failing to comply with a regulatory requirement in the<br />
following respect:<br />
All reasonable measures have not been taken to protect the residents from abuse.<br />
Action required:<br />
Ensure every member of staff has received training in elder abuse.<br />
Reference:<br />
Health Act, 2007<br />
Regulation 6: General Welfare and Protection<br />
Standard 8: Protection<br />
Please state the actions you have taken or are planning to<br />
take with timescales:<br />
Provider’s response:<br />
All nurse managers attended elder abuse training in November 2009<br />
and a scheduled role-out of training which was given to the<br />
inspectors has commenced early in 2010. The person in charge will<br />
expedite this schedule to ensure every member of staff has received<br />
training.<br />
Page 19 of 29<br />
Timescale:<br />
End of March<br />
2010<br />
4. The provider is failing to comply with a regulatory requirement in the<br />
following respect:<br />
Records regarding resuscitation discussions with residents and / or their famil<strong>ie</strong>s were<br />
not kept in a complete and accurate manner.<br />
Action required:<br />
Ensure all records regarding resuscitation are kept in a complete and accurate manner.<br />
Reference:<br />
Health Act, 2007<br />
Regulation 22: Maintenance of Records<br />
Standard 16: End of Life Care<br />
Please state the actions you have taken or are planning to<br />
take with timescales:<br />
Provider’s response:<br />
On the day of the <strong>inspection</strong>, the records seen by the inspectors did<br />
not reflect the communication processes that had been undertaken<br />
Timescale:<br />
April 2010
with the famil<strong>ie</strong>s. In one case, a single family member attended the<br />
meeting to represent the entire family and their v<strong>ie</strong>ws; however this<br />
was not made clear to the inspectors.<br />
The guidelines for cardio-pulmonary resuscitation are currently<br />
under rev<strong>ie</strong>w and will reflect the actions required by the inspectors.<br />
5. The provider is failing to comply with a regulatory requirement in the<br />
following respect:<br />
Written operational polic<strong>ie</strong>s and procedures for the provision of information to residents<br />
were not available.<br />
Action required:<br />
Develop and implement a policy for the provision of information to residents.<br />
Reference:<br />
Health Act, 2007<br />
Regulation 21: Provision of Information to Residents<br />
Standard 1: Information<br />
Please state the actions you have taken or are<br />
planning to take with timescales:<br />
Provider’s response:<br />
This policy has now been drafted and following consultation<br />
shall be implemented in the unit.<br />
Page 20 of 29<br />
Timescale:<br />
March 2010<br />
6. The provider is failing to comply with a regulatory requirement in the<br />
following respect:<br />
The residents’ guide did not include all the information required.<br />
Action required:<br />
Develop a residents’ guide which includes all the information outlined in the legislation<br />
referenced below.<br />
Action required:<br />
Provide a copy of the residents’ guide to each resident.<br />
Reference:<br />
Health Act, 2007<br />
Regulation 21: Provision of Information to Residents<br />
Standard 1:Information
Please state the actions you have taken or are<br />
planning to take with timescales:<br />
Provider’s response:<br />
The residents’ guide will be updated to reflect all the<br />
regulatory requirements.<br />
Page 21 of 29<br />
Timescale:<br />
March 2010<br />
7. The provider has failed to comply with a regulatory requirement in the<br />
following respect:<br />
The insurance certificate provided did not include the name of the centre and did not<br />
state that liability to any resident shall not exceed €1,000 for any one item.<br />
Action required:<br />
Rev<strong>ie</strong>w the insurance policy to ensure the name of the building insured is clearly<br />
identif<strong>ie</strong>d on the insurance certificate.<br />
Action required:<br />
Ensure that the insurance policy clearly outlines that the liability to any resident shall not<br />
exceed €1,000 for any one item.<br />
Reference:<br />
Health Act, 2007<br />
Regulation 26: Insurance Cover<br />
Standard 31: Financial Procedures<br />
Please state the actions you have taken or are planning to<br />
take following the <strong>inspection</strong> with timescales:<br />
Provider’s response:<br />
A corporate response on the issues outlined above has been sought.<br />
Attached is communication received from the states claims agency.<br />
Timescale:<br />
Feb 2010<br />
8. The provider has failed to comply with a regulatory requirement in the<br />
following respect:<br />
All records of money or valuables deposited, received, returned or used at the request of<br />
the resident must be accurately recorded.<br />
Action required:<br />
Ensure an accurate and private record is kept of all individual residents’ financial affairs<br />
managed by the centre.
Reference:<br />
Health Act, 2007<br />
Regulation 22: Maintenance of Records<br />
Standard 9: The Residents’ Finances<br />
Please state the actions you have taken or are planning to<br />
take with timescales:<br />
Provider’s response:<br />
Records have been rev<strong>ie</strong>wed to ensure that accurate and private<br />
record is kept of all individual residents’ financial affairs managed by<br />
the centre. Residents’ cash transactions will be audited bi-monthly<br />
by the administrator.<br />
All residents now have individual records to maintain their privacy.<br />
Page 22 of 29<br />
Timescale:<br />
Completed<br />
Completed<br />
9. The provider is failing to comply with a regulatory requirement in the<br />
following respect:<br />
There is no risk management policy in place in the centre and therefore there is no<br />
precautions in place to control the risks identif<strong>ie</strong>d on <strong>inspection</strong>: radiators too hot to<br />
touch in the main corridors and unsecure safe keeping of safe key.<br />
Action required:<br />
Develop and implement a risk management policy to include precautions in place to<br />
control risks identif<strong>ie</strong>d specif<strong>ie</strong>d risks as outlined in the legislation<br />
Reference:<br />
Health Act, 2007<br />
Regulation 31: Risk Management Procedures<br />
Standard 26: Health and Safety<br />
Standard 9: The Residents’ Finances<br />
Please state the actions you have taken or are planning to<br />
take with timescales:<br />
Provider’s response:<br />
The unit is committed to operating safely and has a number of<br />
measures in place to minimise risks. It is noted that the inspectors<br />
read the units safety statement which refers to risk assessments<br />
appropriate to the unit. These risk assessments which had been<br />
completed could have been made available to the inspectors had<br />
they sought them e.g. pregnant employees, fire, manual handling<br />
etc.<br />
Timescale:
5 staff have received specific training to carry out risk assessments.<br />
Potential and actual risks are identif<strong>ie</strong>d through a number of sources<br />
e.g. incidents and accidents.<br />
A risk assessment on the radiators in the corridors has been carr<strong>ie</strong>d<br />
out and appropriate action instigated. The secure safe keeping of<br />
the safe key has been addressed.<br />
The local risk management polic<strong>ie</strong>s will be rev<strong>ie</strong>wed by the Health &<br />
Safety committee to reflect the requirements of the Health Act<br />
2007.<br />
Page 23 of 29<br />
Completed<br />
March 2010<br />
10. The provider is failing to comply with a regulatory requirement in th<br />
e following respect:<br />
There was no contract of care agreed with individual residents.<br />
Action required:<br />
Decide on a final contract of care and provide one to each individual resident for<br />
agreement.<br />
Reference:<br />
Health Act, 2007<br />
Regulation 28: Contract of Provision of Services<br />
Standard 7: Contract/Statement of Terms and Conditions<br />
Please state the actions you have taken or are planning to<br />
take with timescales:<br />
Provider’s response:<br />
Final contract of care has been approved and provided to each<br />
resident / representative.<br />
Timescale:<br />
February 2010<br />
11. The provider is failing to comply with a regulatory requirement in the<br />
following respect:<br />
Facilitate, insofar as is reasonably practicable, consultation and participation in the<br />
organisation of the designated centre.<br />
Action required:<br />
Ensure issues raised by residents’ at monthly meeting are re-visited at the next and<br />
feedback is provided.
Reference:<br />
Health Act, 2007<br />
Regulation 10: Resident’ Rights, Dignity and Consultation<br />
Standard 2: Consultation and Participation<br />
Please state the actions you have taken or are planning to<br />
take with timescales:<br />
Provider’s response:<br />
The Assistant Director of Nursing will attend the beginning of each<br />
residents meeting to ensure that issues raised are revisited and<br />
feedback is provided.<br />
Page 24 of 29<br />
Timescale:<br />
Completed<br />
12. The provider is failing to comply with a regulatory requirement in the<br />
following respect:<br />
Facilitate, insofar as is reasonably practicable, consultation and participation in the<br />
organisation of the designated centre.<br />
Action required:<br />
Rev<strong>ie</strong>w the time lunch is served as requested by the residents.<br />
Reference:<br />
Health Act, 2007<br />
Regulation 10: Resident’ Rights, Dignity and Consultation<br />
Standard 2: Consultation and Participation<br />
Please state the actions you have taken or are planning to<br />
take with timescales:<br />
Provider’s response:<br />
As per the request of the residents, the lunches have been moved<br />
to a later time and residents’ feedback will be sought at the next<br />
Residents Meeting.<br />
Timescale:<br />
Completed
13. The provider is failing to comply with a regulatory requirement in the<br />
following respect:<br />
Residents care plans are stored over the residents’ bed in shared rooms.<br />
Action required:<br />
Consult with residents about the storage of their care plans.<br />
Action required:<br />
Revise the policy on storage of records to reflect the required arrangement decided<br />
upon by residents.<br />
Reference:<br />
Health Act, 2007<br />
Regulation 22: Maintenance of Records<br />
Standard 32: Register and Residents’ Records<br />
Please state the actions you have taken or are planning to<br />
take with timescales:<br />
Provider’s response:<br />
The unit will consult with residents and relatives about the storage<br />
of their care plans and take action accordingly.<br />
Page 25 of 29<br />
Timescale:<br />
March 2010<br />
14. The provider is failing to comply with a regulatory requirement in the<br />
following respect:<br />
There are an insuffic<strong>ie</strong>nt number of assisted showers / bathrooms to meet the needs of<br />
residents.<br />
Action required:<br />
Ensure there are a suffic<strong>ie</strong>nt number of assisted showers / bathrooms having regard to<br />
the number of dependent persons in the centre.<br />
Reference:<br />
Health Act, 2007<br />
Regulation 19: Premises<br />
Standard 25: Physical Environment<br />
Please state the actions you have taken or are planning to<br />
take with timescales:<br />
Timescale:
Provider’s response:<br />
It is noted that an insuffic<strong>ie</strong>nt number of assisted showers /<br />
bathrooms to meet the needs of residents is available in the unit as<br />
per the National Quality Standards for Residential Care settings for<br />
Older People in Ireland. Two unused bathrooms are currently used<br />
as storage. An alternative arrangement will be put in place for<br />
storage and these bathrooms will be reused.<br />
Page 26 of 29<br />
End of 2010<br />
15. The provider is failing to comply with a regulatory requirement in the<br />
following respect:<br />
The centre does not have appropriate and suitable practices and written polic<strong>ie</strong>s for the<br />
storage of medications.<br />
Action required:<br />
Provide a chain and a lock for each individual drug trolley to ensure it can be secured to<br />
the wall of the store room when not in use.<br />
Action required:<br />
Repair the door of the store room to ensure it closes fully.<br />
Action required:<br />
Revise the policy for the storage of medications and ensure all staff nurses are aware of<br />
this change in policy.<br />
Reference:<br />
Health Act, 2007<br />
Regulation 33: Ordering, Prescribing, Storing and Administration of<br />
Medicines<br />
Standard 14: Medication Management<br />
Please state the actions you have taken or are planning to<br />
take with timescales:<br />
Provider’s response:<br />
The policy for storage of medication trolleys has been rev<strong>ie</strong>wed and<br />
the appropriate action taken, i.e. drug trolleys are locked to a fixed<br />
surface.<br />
The door of the store room has been reported to maintenance.<br />
Timescale:<br />
February 2010<br />
February 2010
16. The provider is failing to comply with a regulatory requirement in the<br />
following respect:<br />
Residents have no telephone facility to use in private.<br />
Action required:<br />
Provide telephone facilit<strong>ie</strong>s that each resident can access in private.<br />
Reference:<br />
Health Act, 2007<br />
Regulation 11: Communication<br />
Standard 4: Privacy and Dignity<br />
Please state the actions you have taken or are planning to<br />
take with timescales:<br />
Provider’s response:<br />
The unit has a 2 cordless telephone which can use in private.<br />
However an additional phone is being installed that can be accessed<br />
in private by the residents.<br />
Page 27 of 29<br />
Timescale:<br />
March 2010
Recommendations<br />
These recommendations are taken from the best practice described in the<br />
National Quality Standards for Residential Care Settings for Older People<br />
in Ireland and the registered provider should consider them as a way of<br />
improving the service.<br />
Standard Best practice recommendations<br />
Standard 23:<br />
Staffing<br />
Levels and<br />
Qualifications<br />
Consider rev<strong>ie</strong>wing staff rota to ensure all staff on duty have there<br />
names and hours reflected on the one rota including agency staff.<br />
Consider rev<strong>ie</strong>wing the high use of agency staff on an ongoing basis<br />
Page 28 of 29
Any comments the provider may wish to make:<br />
Provider’s response:<br />
The person in charge and staff at <strong>Seanchara</strong> <strong>Community</strong> unit welcome the inspectors<br />
comments and acknowledge that it highlights areas of good practice and<br />
opportunit<strong>ie</strong>s for improvement in particular as this <strong>inspection</strong> was unannounced and<br />
the first such <strong>inspection</strong> of the unit.<br />
The unit had undertaken a person-centred dementia programme, which was evident<br />
to the inspectors e.g. excellent signage. This has a direct impact on areas of practice<br />
such as communication & activit<strong>ie</strong>s. The staff are implementing the Poole activity<br />
level and the inspectors were made aware of this. The staff are very proud of the<br />
services they deliver to all residents/cl<strong>ie</strong>nts.<br />
We welcome the recommendation in relation to the high use of agency staff in the<br />
unit as this is a cause of concern for the person in charge.<br />
Provider’s name: Gerry Reid<br />
Date: 22 February 2010<br />
Page 29 of 29