Pilocarpine Tablets for the Treatment of Dry Mouth and Dry Eye ...
Pilocarpine Tablets for the Treatment of Dry Mouth and Dry Eye ...
Pilocarpine Tablets for the Treatment of Dry Mouth and Dry Eye ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Pilocarpine</strong> <strong>Tablets</strong> <strong>for</strong> <strong>the</strong> <strong>Treatment</strong> <strong>of</strong> <strong>Dry</strong> <strong>Mouth</strong> <strong>and</strong><br />
<strong>Dry</strong> <strong>Eye</strong> Symptoms in Patients With Sjögren Syndrome<br />
A R<strong>and</strong>omized, Placebo-Controlled, Fixed-Dose, Multicenter Trial<br />
Frederick B. Vivino, MD; Ibtisam Al-Hashimi, PhD; Zafrulla Khan, DDS; Francis G. LeVeque, DDS;<br />
Paul L. Salisbury III, DDS; Tram K. Tran-Johnson, PharmD, PsyD; Charles C. Muscoplat, PhD;<br />
Madhu Trivedi, PhD; Barry Goldlust, PhD; Susan C. Gallagher, MS; <strong>for</strong> <strong>the</strong> P92-01 Study Group<br />
Background: Patients with Sjögren syndrome (SS) experience<br />
slowly progressive infiltration <strong>of</strong> lacrimal <strong>and</strong><br />
salivary gl<strong>and</strong>s by mononuclear cells. This leads to diminished<br />
secretions, with resultant symptoms <strong>of</strong> xerostomia<br />
<strong>and</strong> xerophthalmia. Although pilocarpine hydrochloride<br />
tablets are currently indicated <strong>for</strong> <strong>the</strong> treatment<br />
<strong>of</strong> radiation-induced xerostomia, <strong>the</strong>ir effects on dry<br />
mouth or dry eyes in patients with SS are unclear.<br />
Objective: To assess <strong>the</strong> safety <strong>and</strong> efficacy <strong>of</strong> pilocarpine<br />
(Salagen) tablets as symptomatic treatment <strong>for</strong> dry<br />
mouth <strong>and</strong> dry eyes caused by SS in a multicenter, doubleblind,<br />
placebo-controlled trial.<br />
Methods: After providing written in<strong>for</strong>med consent, 373<br />
patients with primary or secondary SS <strong>and</strong> clinically significant<br />
dry mouth <strong>and</strong> dry eyes were r<strong>and</strong>omized to receive<br />
2.5-mg pilocarpine, 5-mg pilocarpine, or placebo<br />
tablets 4 times daily <strong>for</strong> 12 weeks. Symptoms were assessed<br />
by questionnaires with visual analog scales or cat-<br />
The affiliations <strong>of</strong> <strong>the</strong> authors<br />
<strong>and</strong> <strong>the</strong> names <strong>of</strong> <strong>the</strong> members<br />
<strong>of</strong> <strong>the</strong> P92-01 Study Group<br />
appear in <strong>the</strong> acknowledgment<br />
section at <strong>the</strong> end <strong>of</strong> article.<br />
Downloaded From: http://173.193.11.201/ on 04/10/2013<br />
ORIGINAL INVESTIGATION<br />
SJÖGREN SYNDROME (SS) is a<br />
chronic, autoimmune, rheumatic<br />
disorder characterized<br />
by lymphocyte-mediated<br />
destruction <strong>of</strong> exocrine<br />
gl<strong>and</strong>s <strong>and</strong> internal organ involvement that<br />
occur in association with autoantibody<br />
production or as a complication <strong>of</strong> a preexisting<br />
connective tissue disorder. Over<br />
time, progressive infiltration <strong>of</strong> lacrimal<br />
<strong>and</strong> salivary gl<strong>and</strong>s by mononuclear cells<br />
leads to diminished secretions, with resultant<br />
xerostomia (dry mouth) <strong>and</strong> xerophthalmia<br />
(dry eyes) being <strong>the</strong> most<br />
prevalent symptoms. 1,2<br />
Morbidity from salivary <strong>and</strong> lacrimal<br />
gl<strong>and</strong> hyp<strong>of</strong>unction results from alteration<br />
<strong>of</strong> mucosal <strong>and</strong> ocular surfaces <strong>and</strong><br />
breakdown <strong>of</strong> <strong>the</strong> normal host barriers to<br />
infection. In addition to significant discom<strong>for</strong>t<br />
from dryness, untreated dry<br />
mouth <strong>and</strong> dry eyes may also lead to complications,<br />
including stomatopyrosis<br />
(burning mouth), oral ulcers, malnutri-<br />
ARCH INTERN MED/ VOL 159, JAN 25, 1999<br />
174<br />
egorical checkboxes. Whole-mouth salivary flow rates<br />
were measured.<br />
Results: A significantly greater proportion <strong>of</strong> patients<br />
in <strong>the</strong> 5-mg pilocarpine group showed improvement compared<br />
with <strong>the</strong> placebo group (P.01) in global assessments<br />
<strong>of</strong> dry mouth, dry eyes, <strong>and</strong> o<strong>the</strong>r symptoms <strong>of</strong><br />
dryness (P.05). Salivary flow was significantly increased<br />
2- to 3-fold (P.001) after administration <strong>of</strong> <strong>the</strong><br />
first dose <strong>and</strong> was maintained throughout <strong>the</strong> 12-week<br />
study. The most common adverse effect was sweating,<br />
<strong>and</strong> no serious drug-related adverse experiences were reported.<br />
Conclusion: Administration <strong>of</strong> 5-mg pilocarpine tablets<br />
4 times daily (20 mg/d) was well tolerated <strong>and</strong> produced<br />
significant improvement in symptoms <strong>of</strong> dry mouth<br />
<strong>and</strong> dry eyes <strong>and</strong> o<strong>the</strong>r xeroses in patients with SS.<br />
Arch Intern Med. 1999;159:174-181<br />
©1999 American Medical Association. All rights reserved.<br />
tion, weight loss, oral c<strong>and</strong>idiasis, bacterial<br />
sialadenitis, sleep disruption, accelerated<br />
dental caries, periodontal disease,<br />
corneal ulceration or per<strong>for</strong>ation, <strong>and</strong> bacterial<br />
conjunctivitis. 3-5 Use <strong>of</strong> currently<br />
available treatments, including tear <strong>and</strong> saliva<br />
substitutes, provides transient relief<br />
at best <strong>and</strong> <strong>of</strong>ten fails to prevent complications.<br />
In addition, patients <strong>of</strong>ten find<br />
<strong>the</strong>se over-<strong>the</strong>-counter remedies costly, ineffective,<br />
inconvenient, or irritating.<br />
<strong>Pilocarpine</strong> is a naturally occurring<br />
compound derived from <strong>the</strong> South American<br />
shrub Pilocarpus jabor<strong>and</strong>i. This plant<br />
alkaloid is a cholinergic parasympathomimetic<br />
agonist that binds to muscarinic-M3<br />
receptors <strong>and</strong> can cause pharmacological<br />
smooth muscle contraction in<br />
humans <strong>and</strong> stimulation <strong>of</strong> various exocrine<br />
gl<strong>and</strong>s. 6 <strong>Pilocarpine</strong> hydrochloride<br />
(Salagen) tablets are currently indicated<br />
<strong>for</strong> treatment <strong>of</strong> radiation-induced dry<br />
mouth. 7 In 2 previous multicenter, doubleblind,<br />
placebo-controlled trials, 8,9 use <strong>of</strong>
PATIENTS AND METHODS<br />
PATIENTS<br />
Written <strong>of</strong> in<strong>for</strong>med consent was obtained from all potential<br />
study participants as <strong>the</strong> first stage <strong>of</strong> screening <strong>and</strong> be<strong>for</strong>e<br />
admission to <strong>the</strong> study. Study patients were older than<br />
18 years <strong>and</strong> had a diagnosis <strong>of</strong> primary or secondary SS<br />
consistent with <strong>the</strong> European Cooperative Community classification<br />
criteria <strong>for</strong> SS. 10 The diagnosis <strong>of</strong> SS was confirmed<br />
at screening by positive test results <strong>for</strong> at least 1 <strong>of</strong><br />
<strong>the</strong> following: marker autoantibodies against SS-A or SS-B,<br />
rheumatoid factor or antinuclear antibodies at a titer <strong>of</strong> 1:<br />
160 or greater (or equivalent), or a positive labial minor<br />
salivary gl<strong>and</strong> biopsy sample. If a lip biopsy sample was used<br />
to support admission to <strong>the</strong> study, a representative slide<br />
<strong>of</strong> <strong>the</strong> biopsy sample was read by an external evaluator<br />
(T. E. Daniels, DDS, MS, Oral Pathology Laboratory, School<br />
<strong>of</strong> Dentistry, University <strong>of</strong> Cali<strong>for</strong>nia, San Francisco). Positive<br />
biopsy samples required a focus score <strong>of</strong> greater than<br />
1 focus per 4 mm 2 tissue area. 3,11 The presence <strong>of</strong> clinically<br />
significant dry mouth <strong>and</strong> dry eye symptoms was confirmed<br />
by screening questionnaires. Patients who indicated<br />
mild symptoms by responding in <strong>the</strong> upper quartile<br />
<strong>of</strong> <strong>the</strong> screening questionnaire (100-mm visual analog scale<br />
[VAS]) did not qualify <strong>for</strong> entry. Patients were required to<br />
discontinue, <strong>for</strong> at least 6 weeks be<strong>for</strong>e screening procedures,<br />
use <strong>of</strong> any electrical device <strong>for</strong> salivary stimulation.<br />
At screening, patients were required to demonstrate some<br />
residual salivary function by demonstrating any level <strong>of</strong> saliva<br />
production. In <strong>the</strong>se analyses, an unstimulated wholemouth<br />
salivary flow rate <strong>of</strong> less than 0.4 mL/min was classified<br />
as salivary hyp<strong>of</strong>unction. 12 Patients were instructed<br />
to discontinue, at least 7 days be<strong>for</strong>e admission, taking any<br />
medication reported to produce significant dry mouth. 13,14<br />
Schirmer tear test results <strong>and</strong> Rose Bengal staining 15 were<br />
also recorded during screening. A Schirmer score <strong>of</strong> 7 mm<br />
per 5 minutes <strong>and</strong> staining <strong>of</strong> 3 were each considered indicative<br />
<strong>of</strong> dry eyes. These screening requirements were<br />
modified from <strong>the</strong> European classification criteria <strong>for</strong> SS, 10<br />
which requires a patient to meet 4 <strong>of</strong> <strong>the</strong> following 6 criteria:<br />
ocular symptom, oral symptom, ocular sign, histopathologic<br />
feature, objective salivary gl<strong>and</strong> involvement,<br />
<strong>and</strong> presence <strong>of</strong> autoantibodies.<br />
Prospective patients were excluded if <strong>the</strong>y had clinically<br />
significant cardiopulmonary, renal, or gastrointestinal<br />
tract disease; diabetes mellitus; multiple sclerosis; hypersensitivity<br />
to pilocarpine use; or clinically significant<br />
ocular disease, including narrow-angle glaucoma, peripheral<br />
retinopathies, or o<strong>the</strong>r conditions in which ocular<br />
(topical) pilocarpine use would be contraindicated. Female<br />
patients <strong>of</strong> childbearing potential were required to<br />
pilocarpine tablets provided significant relief to patients<br />
with radiation-induced dry mouth. In <strong>the</strong>se 2 studies, use<br />
<strong>of</strong> pilocarpine tablets significantly improved symptoms<br />
<strong>of</strong> intraoral dryness, oral discom<strong>for</strong>t, <strong>and</strong> dysphonia <strong>and</strong><br />
patients’ global assessment <strong>of</strong> dry mouth as well as reduced<br />
<strong>the</strong> need <strong>for</strong> administration <strong>of</strong> oral com<strong>for</strong>t agents<br />
such as artificial saliva, water, <strong>and</strong> hard c<strong>and</strong>y. Patients<br />
treated with pilocarpine tablets also demonstrated a statistically<br />
significant increase in saliva production, mea-<br />
Downloaded From: http://173.193.11.201/ on 04/10/2013<br />
use medically acceptable contraceptive methods throughout<br />
<strong>the</strong> study.<br />
TREATMENT PROTOCOL<br />
At <strong>the</strong> admission visit, patients were r<strong>and</strong>omly assigned to 1<br />
<strong>of</strong> 3 treatment groups <strong>for</strong> <strong>the</strong> duration <strong>of</strong> <strong>the</strong> study:2.5-mg pilocarpine,5-mgpilocarpine,orplacebotablets.Alltabletswere<br />
identicalinappearance<strong>and</strong>weresuppliedbyMGIPharmaInc,<br />
Minnetonka, Minn. Site personnel instructed patients to take<br />
1 tablet <strong>of</strong> <strong>the</strong> study drug with water 4 times a day at mealtimes<br />
<strong>and</strong> bedtime, with a minimum <strong>of</strong> 3 hours between doses <strong>for</strong><br />
<strong>the</strong> duration <strong>of</strong> <strong>the</strong> 12-week study. In addition, patients were<br />
instructed to record missed doses <strong>and</strong> adverse experiences in<br />
a diary. Patients recorded <strong>the</strong>ir responses to <strong>the</strong> dryness questionnaires<br />
be<strong>for</strong>e receiving <strong>the</strong> first dose <strong>of</strong> <strong>the</strong> test drug. At<br />
this visit, patients who took nothing by mouth <strong>for</strong> at least 90<br />
minutes be<strong>for</strong>e <strong>the</strong> start <strong>of</strong> salivary procedures were given <strong>the</strong><br />
first dose <strong>of</strong> test drug with 180 mL (6 oz) <strong>of</strong> water. They were<br />
<strong>the</strong>n monitored <strong>for</strong> an additional 90 minutes, during which<br />
timesalivasampleswereobtained(see<strong>the</strong>“Methods”section).<br />
All baseline measurements were recorded <strong>for</strong> each patient be<strong>for</strong>e<br />
administration <strong>of</strong> this first dose <strong>of</strong> test drug. Patients returnedto<strong>the</strong>studysiteatweeks6<strong>and</strong>12<strong>for</strong>efficacy<strong>and</strong>safety<br />
evaluations.<br />
METHODS<br />
Efficacy Assessment<br />
Efficacy was evaluated at each visit by (1) response to questionnaires<br />
<strong>and</strong> (2) measurement <strong>of</strong> salivary flow. Primary<br />
variables were <strong>the</strong> global assessments <strong>of</strong> dry mouth <strong>and</strong> dry<br />
eyes at study end point. End point was defined as <strong>the</strong> last<br />
available postdose observation <strong>for</strong> each patient. In addition,<br />
specific symptoms associated with dry mouth <strong>and</strong> dry<br />
eyes were assessed, as was change in dryness associated with<br />
extraoral <strong>and</strong> extraocular symptoms, such as dryness <strong>of</strong> <strong>the</strong><br />
skin, vagina, <strong>and</strong> nasal passages.<br />
Questionnaires<br />
ARCH INTERN MED/ VOL 159, JAN 25, 1999<br />
175<br />
©1999 American Medical Association. All rights reserved.<br />
Patients completed questionnaires at <strong>the</strong> admission (baseline),<br />
week 6, <strong>and</strong> week 12 visits. Questions were presented<br />
in 2 <strong>for</strong>mats: (1) a 100-mm VAS, with responses ranging<br />
from <strong>the</strong> negative (0 mm = extremely dry) on <strong>the</strong> left<br />
to <strong>the</strong> positive on <strong>the</strong> right, <strong>and</strong> (2) 3-point categorical questions<br />
(increase in, no change, or decrease in symptoms). 8,9<br />
For assessment <strong>of</strong> primary measures <strong>of</strong> efficacy—<br />
global improvement <strong>of</strong> dry mouth <strong>and</strong> dry eyes—patients<br />
were asked at each week 6 <strong>and</strong> week 12 visit to indicate on<br />
Continued on next page<br />
sured as ei<strong>the</strong>r whole-mouth or parotid salivary flow. It<br />
is through this mechanism that cholinergic stimulation<br />
<strong>of</strong> residual-functioning exocrine gl<strong>and</strong>ular tissue in patients<br />
with SS could potentially alleviate symptoms <strong>of</strong> dry<br />
mouth, dry eyes, or o<strong>the</strong>r symptoms associated with SS.<br />
There<strong>for</strong>e, <strong>the</strong> present study was undertaken to investigate<br />
<strong>the</strong> efficacy <strong>and</strong> safety <strong>of</strong> pilocarpine tablets <strong>for</strong> <strong>the</strong><br />
treatment <strong>of</strong> symptoms associated with dry mouth <strong>and</strong><br />
dry eyes in patients with SS.
a VAS question <strong>the</strong>ir overall change in mouth <strong>and</strong> eye dryness<br />
compared with how <strong>the</strong>y felt at study admission (baseline).<br />
Responses on <strong>the</strong> VAS were classified as follows: less<br />
than 45 mm indicates nonresponder (worsened); 45 to 55<br />
mm, nonresponder (no change); <strong>and</strong> greater than 55 mm,<br />
responder (improved).<br />
The remaining VAS questions, also recorded at each<br />
visit, were designed to measure <strong>the</strong> intensity <strong>of</strong> specific<br />
symptoms <strong>of</strong> dryness as <strong>of</strong> <strong>the</strong> study visit <strong>and</strong> included (1)<br />
mouth: dryness <strong>of</strong> <strong>the</strong> mouth <strong>and</strong> discom<strong>for</strong>t <strong>of</strong> <strong>the</strong> mouth;<br />
(2) eye: overall ocular problems, change in tear flow, eye<br />
discom<strong>for</strong>t, sensitivity to light, visual blurring, discharge<br />
or draining, itching, redness, matting, sense <strong>of</strong> <strong>for</strong>eign body,<br />
use <strong>of</strong> tear substitutes, difficulty focusing, <strong>and</strong> difficulty with<br />
night driving; <strong>and</strong> (3) o<strong>the</strong>r symptoms <strong>of</strong> xeroses: dryness<br />
<strong>of</strong> <strong>the</strong> skin, vagina, <strong>and</strong> nasal passage <strong>and</strong> ability to produce<br />
mucus. These questions were compared with baseline<br />
ratings <strong>and</strong> required an improvement <strong>of</strong> 25 mm or more<br />
above <strong>the</strong> baseline score to be defined as responders.<br />
There were 5 questions using a 3-point categorical <strong>for</strong>mat<br />
that measured an increase, no change, or a decrease<br />
in symptoms. The oral questions included ability to speak<br />
without using water, ability to sleep without awakening <strong>for</strong><br />
water, <strong>and</strong> use <strong>of</strong> saliva substitutes. The ocular questions<br />
included difficulty focusing eyes after taking <strong>the</strong> study medication<br />
<strong>and</strong> difficulty driving after taking <strong>the</strong> study medication.<br />
For <strong>the</strong>se 5 questions, patients with improvement<br />
in symptoms were classified as responders, <strong>and</strong> those with<br />
no change or worsening symptoms were classified as nonresponders.<br />
Saliva Collections<br />
As noted above with reference to patient screening, an unstimulated<br />
whole-mouth salivary flow rate <strong>of</strong> less than 0.4<br />
mL/min was classified as salivary hyp<strong>of</strong>unction. 12 At admission,<br />
week 6, <strong>and</strong> week 12 visits, salivary flow was measured<br />
in patients who took nothing by mouth <strong>for</strong> 90 minutes<br />
or longer be<strong>for</strong>e initiation <strong>of</strong> saliva measurements. Fiveminute<br />
saliva samples were collected be<strong>for</strong>e dosing <strong>and</strong> 30,<br />
60, <strong>and</strong> 90 minutes after patients received 1 tablet <strong>of</strong> <strong>the</strong>ir<br />
assigned test drug with 180 mL (6 oz) <strong>of</strong> water. For <strong>the</strong><br />
collection procedure, <strong>the</strong> patients kept <strong>the</strong>ir heads tilted<br />
<strong>for</strong>ward <strong>and</strong> swallowed once to clear <strong>the</strong> mouth <strong>of</strong> excess<br />
saliva. At this point, <strong>the</strong> 5-minute collection period was initiated.<br />
Patients <strong>the</strong>n expectorated, as needed, any saliva<br />
that accumulated in <strong>the</strong> mouth into a preweighed 50cm<br />
3 centrifuge tube. Samples were weighed on an analytical<br />
balance to determine <strong>the</strong> volume (1 g = 1 mL) <strong>of</strong><br />
saliva obtained. During this collection period, patients<br />
continued not taking anything by mouth o<strong>the</strong>r than <strong>the</strong><br />
prescribed test medication, leaving <strong>the</strong>m without fluids<br />
<strong>for</strong> 180 minutes.<br />
RESULTS<br />
Of <strong>the</strong> 373 patients with SS enrolled in <strong>the</strong> study at 17<br />
sites, 125 were r<strong>and</strong>omized to <strong>the</strong> placebo group, 121 to<br />
<strong>the</strong> 2.5-mg pilocarpine group, <strong>and</strong> 127 to <strong>the</strong> 5-mg pilocarpine<br />
group. Demographic characteristics were similar<br />
among <strong>the</strong> treatment groups (Table 1). Patients with<br />
SS are predominantly female, 11,17 which is consistent with<br />
enrollment in this study (95.7% women). Ninety-four per-<br />
Downloaded From: http://173.193.11.201/ on 04/10/2013<br />
Safety<br />
Safety evaluations were based on results <strong>of</strong> laboratory tests<br />
(liver <strong>and</strong> kidney function tests, urinalysis, <strong>and</strong> complete<br />
blood cell counts with differential <strong>and</strong> platelet counts) conducted<br />
at each visit, results <strong>of</strong> electrocardiograms <strong>and</strong> physical<br />
examinations conducted be<strong>for</strong>e study admission <strong>and</strong> at<br />
<strong>the</strong> end <strong>of</strong> <strong>the</strong> study, <strong>and</strong> all adverse experience reports.<br />
An adverse experience was defined as any clinically significant<br />
change in physical signs or symptoms or a significant<br />
laboratory test result change occurring in any phase<br />
<strong>of</strong> <strong>the</strong> study regardless <strong>of</strong> its relationship to study drug. Safety<br />
assessment was done <strong>for</strong> any patient who withdrew from<br />
<strong>the</strong> study be<strong>for</strong>e week 12.<br />
STATISTICAL ANALYSES<br />
ARCH INTERN MED/ VOL 159, JAN 25, 1999<br />
176<br />
©1999 American Medical Association. All rights reserved.<br />
The sample <strong>of</strong> calculations was based on 1 <strong>of</strong> <strong>the</strong> 2 primary<br />
efficacy variables, particularly, response to treatment with respect<br />
to dryness <strong>of</strong> <strong>the</strong> mouth. A 2-sided 2 test, with = .05,<br />
was used. Assuming a 30% response rate in <strong>the</strong> placebo group<br />
<strong>and</strong> a 50% response rate in <strong>the</strong> high-dose pilocarpine group,<br />
100 persons per treatment would result in a power <strong>of</strong> 80%<br />
<strong>for</strong> this comparison. Efficacy results are presented <strong>for</strong> <strong>the</strong> intent-to-treat<br />
cohort. All patients who received at least 1 dose<br />
<strong>of</strong> <strong>the</strong> study drug <strong>and</strong> who had at least 1 efficacy assessment<br />
after administration <strong>of</strong> <strong>the</strong> first dose were included in this cohort.<br />
The safety cohort included all patients who took at least<br />
1 dose <strong>of</strong> <strong>the</strong> study drug. Analyses were per<strong>for</strong>med using <strong>the</strong><br />
end point observation, ie, <strong>the</strong> last-available postdose observation<br />
<strong>for</strong> a patient. Differences in <strong>the</strong> proportion <strong>of</strong> responders<br />
among treatment groups were evaluated using a logistic<br />
regression model.<br />
Based on <strong>the</strong> pharmacokinetic pr<strong>of</strong>ile <strong>for</strong> this drug, 16 <strong>the</strong><br />
peak salivary flow was anticipated to occur approximately 60<br />
minutes after administration <strong>of</strong> a single 5-mg pilocarpine tablet.<br />
There<strong>for</strong>e, <strong>the</strong> comparison <strong>of</strong> changes in salivary flow focused<br />
on <strong>the</strong> 60-minute postdose collection. Statistical significance<br />
was defined at P.05 <strong>for</strong> <strong>the</strong> determination <strong>of</strong> an<br />
overalltreatmenteffect.Foranalysis<strong>of</strong>symptomaticresponse,<br />
if <strong>the</strong>re was an overall treatment effect, specific pairwise comparisonsbetween<strong>the</strong>placebo<strong>and</strong><strong>the</strong>5-mgpilocarpinegroups<br />
were made using a logistic regression model. For analysis <strong>of</strong><br />
salivary flow, if <strong>the</strong>re was an overall treatment effect, specific<br />
pairwise comparisons between placebo <strong>and</strong> 5-mg pilocarpine<br />
tablets, <strong>and</strong> comparison between placebo <strong>and</strong> 2.5-mg pilocarpine<br />
tablets, were made using a 2-sided t test.<br />
The demographic <strong>and</strong> safety results are presented using<br />
overall comparisons <strong>for</strong> all 3 groups. Pairwise comparisons<br />
<strong>of</strong> <strong>the</strong> placebo group vs <strong>the</strong> 5-mg pilocarpine group<br />
are presented <strong>for</strong> efficacy results. A s<strong>of</strong>tware program (SAS<br />
version 6.09 or greater, SAS Institute Inc, Cary, NC) was<br />
used <strong>for</strong> statistical analyses.<br />
cent <strong>of</strong> patients met criteria similar to <strong>the</strong> European classification<br />
10 <strong>of</strong> SS (Table 2). Most patients (87%) completed<br />
this 3-month study (Table 3). Medications used<br />
by this patient population were monitored throughout<br />
<strong>the</strong> study. The most frequently used (10%) medications<br />
were consistent with those expected in this population,<br />
ie, analgesic or anti-inflammatory drugs (aspirin,<br />
ibupr<strong>of</strong>en, naproxen, acetaminophen, <strong>and</strong><br />
prednisone), antirheumatic drugs (hydroxychloro
Table 1. Demographic Characteristics<br />
<strong>of</strong> <strong>the</strong> Study Population*<br />
Characteristic<br />
Placebo<br />
<strong>Tablets</strong><br />
(n = 125)<br />
<strong>Pilocarpine</strong> <strong>Tablets</strong><br />
(n = 248)<br />
2.5 mg<br />
(n = 121)<br />
quine sulfate <strong>and</strong> methotrexate), gastrointestinal tract<br />
agents (omeprazole), hormonal replacement drugs (conjugated<br />
estrogen <strong>and</strong> medroxyprogesterone acetate), <strong>and</strong><br />
thyroid preparations (levothyroxine sodium). Use <strong>of</strong> <strong>the</strong>se<br />
medications was balanced across treatment groups.<br />
CLINICAL OUTCOMES<br />
5mg<br />
(n = 127)<br />
Overall P<br />
Age, y 54.6 ± 13.6 54.0 ± 12.5 55.4 ± 13.6 .72<br />
Height, cm 162.3 ± 7.6 161.5 ± 7.4 162.0 ± 7.8 .75<br />
Weight, kg<br />
Sex<br />
65.2 ± 14.5 65.4 ± 15.1 66.6 ± 14.5 .64<br />
Female<br />
Male<br />
Race<br />
118 (94.4)<br />
7 (5.6)<br />
116 (95.9)<br />
5 (4.1)<br />
123 (96.9)<br />
4 (3.2)<br />
.63<br />
White 97 (77.6) 96 (79.3) 104 (81.9)<br />
Black<br />
Asian<br />
5 (4.0)<br />
18 (14.4)<br />
1 (0.8)<br />
20 (16.5)<br />
3 (2.4)<br />
14 (11.0)<br />
.62<br />
O<strong>the</strong>r 5 (4.0) 4 (3.3) 6 (4.7)<br />
*Data are given as mean ± SD <strong>and</strong> number (percentage).<br />
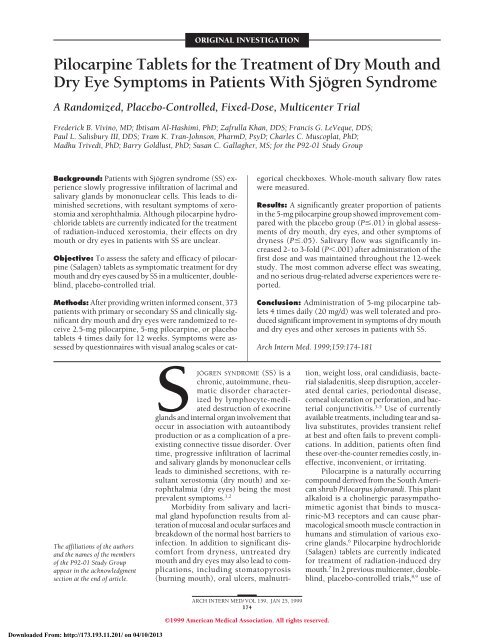
Primary Outcomes—<strong>Dry</strong> <strong>Mouth</strong> <strong>and</strong> <strong>Dry</strong> <strong>Eye</strong>s<br />
The primary measures <strong>of</strong> efficacy were <strong>the</strong> assessments<br />
<strong>of</strong> <strong>the</strong> global, or overall, improvement in symptoms <strong>of</strong><br />
dry mouth <strong>and</strong> dry eyes in <strong>the</strong> end-point analyses<br />
(Figure 1, left). For global improvement <strong>of</strong> dry mouth,<br />
a significantly (P.001) greater proportion <strong>of</strong> patients<br />
in <strong>the</strong> 5-mg pilocarpine group (61.3%) responded to<br />
<strong>the</strong>rapy compared with <strong>the</strong> placebo group (31.1%). For<br />
global improvement <strong>of</strong> dry eyes, a statistically significant<br />
(P.009) benefit was also observed in <strong>the</strong> 5-mg pilocarpine<br />
group (42.0%) compared with <strong>the</strong> placebo group<br />
(26.1%). The 2.5-mg pilocarpine group did not demonstrate<br />
differences in symptomatic relief <strong>of</strong> oral or ocular<br />
symptoms compared with <strong>the</strong> placebo group.<br />
Supportive Outcomes—<strong>Dry</strong> <strong>Mouth</strong> <strong>and</strong> <strong>Dry</strong> <strong>Eye</strong>s<br />
Additional questions assessed posttreatment benefits <strong>for</strong><br />
specific symptoms associated with SS. Responses to 4 <strong>of</strong><br />
<strong>the</strong> 5 dry mouth questions showed a statistically significant<br />
increase in <strong>the</strong> proportion <strong>of</strong> responders in favor <strong>of</strong><br />
5-mg pilocarpine tablets (Figure 1, right). In addition to<br />
improved mouth com<strong>for</strong>t (P.004) <strong>and</strong> mouth dryness<br />
(P.02), patients also experienced an improved ability<br />
to sleep because <strong>of</strong> reduced nocturnal fluid ingestion<br />
(P.04) <strong>and</strong> reduced use <strong>of</strong> saliva substitutes (P.02).<br />
The difference between <strong>the</strong> 5-mg pilocarpine group <strong>and</strong><br />
<strong>the</strong> placebo group in <strong>the</strong> ability to speak without drinking<br />
water was not significant (P.06). For ocular symptoms,<br />
a significantly greater proportion <strong>of</strong> patients taking<br />
5-mg pilocarpine tablets also showed clinically<br />
significant improvement compared with those taking pla-<br />
Downloaded From: http://173.193.11.201/ on 04/10/2013<br />
Table 2. Patient Disease Characteristics*<br />
Variable<br />
Placebo<br />
<strong>Tablets</strong><br />
(n = 125)<br />
<strong>Pilocarpine</strong> <strong>Tablets</strong><br />
(n = 248)<br />
2.5 mg<br />
(n = 121)<br />
5mg<br />
(n = 127)<br />
Symptomatic dry mouth 124 (99.2) 121 (100.0) 124 (97.6)<br />
Symptomatic dry eyes 121 (96.8) 119 (98.3) 117 (92.1)<br />
Positive serologic marker 117 (96.8) 114 (94.2) 118 (92.9)<br />
Patients with positive<br />
biopsy samples<br />
3 (2.4) 4 (3.3) 3 (2.4)<br />
Ocular signs 93 (74.4) 96 (79.3) 94 (74.0)<br />
Reduced salivary flow rate 117 (93.6) 111 (91.7) 113 (89.0)<br />
Patients meeting diagnosis<br />
<strong>of</strong> Sjögren syndrome†<br />
119 (95.2) 117 (96.7) 116 (91.3)<br />
*Data are given as number (percentage).<br />
†Patients meeting at least 4 <strong>of</strong> 6 diagnostic criteria listed above (see <strong>the</strong><br />
“Methods” subsection <strong>of</strong> <strong>the</strong> “Patients <strong>and</strong> Methods” section).<br />
Table 3. Patient Disposition*<br />
Status<br />
ARCH INTERN MED/ VOL 159, JAN 25, 1999<br />
177<br />
©1999 American Medical Association. All rights reserved.<br />
Placebo<br />
<strong>Tablets</strong><br />
(n = 125)<br />
<strong>Pilocarpine</strong> <strong>Tablets</strong><br />
(n = 248)<br />
2.5 mg<br />
(n = 121)<br />
5mg<br />
(n = 127)<br />
Completed study 112 (89.6) 102 (84.3) 110 (86.6)<br />
Discontinued study 13 (10.4) 19 (15.7) 17 (13.4)<br />
Reason <strong>for</strong> discontinuation†<br />
Adverse experience 7 (5.6) 9 (7.4) 9 (7.1)<br />
Death 0 1 (1.0) 0<br />
Lost to follow-up 0 0 1 (1.0)<br />
Miscellaneous/compliance 6 (4.8) 9 (7.4) 7 (5.5)<br />
*Data are given as number (percentage).<br />
†Adverse event whe<strong>the</strong>r or not related to use <strong>of</strong> <strong>the</strong> study drug. As a<br />
subset <strong>of</strong> <strong>the</strong>se numbers, withdrawals due to drug-related adverse events<br />
were 1% <strong>for</strong> <strong>the</strong> 2.5-mg group <strong>and</strong> 3.1% <strong>for</strong> <strong>the</strong> 5-mg group.<br />
cebo <strong>for</strong> overall improvement in ocular problems<br />
(P.004), ability to focus <strong>the</strong>ir eyes during reading<br />
(P.04), <strong>and</strong> reduced severity <strong>of</strong> blurred vision (P.02).<br />
No benefit was observed <strong>for</strong> <strong>the</strong> remaining ocular symptoms<br />
(sensitivity to light, severity <strong>of</strong> itching, tiredness,<br />
redness, difficulty with night driving, discharge or draining,<br />
difficulty focusing in general, <strong>for</strong>eign body sensation,<br />
discom<strong>for</strong>t, reduced use <strong>of</strong> artificial tears, matting,<br />
<strong>and</strong> change in tear flow).<br />
In addition to <strong>the</strong> responder analyses reported above,<br />
a statistical analysis <strong>of</strong> mean VAS scores in <strong>the</strong> placebo<br />
vs <strong>the</strong> 5-mg pilocarpine group indicated a significant benefit<br />
<strong>of</strong> pilocarpine treatment. Both primary end points—<br />
global improvement <strong>of</strong> dry mouth (P.001) <strong>and</strong> dry eyes<br />
(P.01)—were significant. In addition, <strong>for</strong> relief <strong>of</strong> specific<br />
dry mouth symptoms, both VAS questions (dryness<br />
<strong>of</strong> mouth <strong>and</strong> discom<strong>for</strong>t <strong>of</strong> mouth) were significant<br />
(P.01). For relief <strong>of</strong> dry eye symptoms, 2 <strong>of</strong> 3 VAS<br />
questions <strong>for</strong> specific dry eye symptoms (overall change<br />
in eye problems <strong>and</strong> severity <strong>of</strong> visual blurring) that were<br />
significant by <strong>the</strong> responder analyses were also significant<br />
(P.03) when measured by mean increase in VAS<br />
scores.
Responders, %<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
P ≤ .001<br />
P ≤ .009<br />
0<br />
<strong>Dry</strong> <strong>Mouth</strong> <strong>Dry</strong> <strong>Eye</strong>s <strong>Mouth</strong><br />
Com<strong>for</strong>t<br />
Extraoral <strong>and</strong> Extraocular Symptoms <strong>of</strong> <strong>Dry</strong>ness<br />
A significantly higher proportion <strong>of</strong> patients in <strong>the</strong> 5-mg<br />
pilocarpine group showed a positive response to <strong>the</strong>rapy<br />
compared with those in <strong>the</strong> placebo group <strong>for</strong> relief <strong>of</strong><br />
symptoms <strong>of</strong> nasal dryness (P.002), skin dryness<br />
(P.01), ability to expectorate mucus (P.02), <strong>and</strong> vaginal<br />
dryness (P.02).<br />
SALIVARY FUNCTION<br />
The measure <strong>of</strong> salivary flow is presented in milliliters<br />
per minute. The change in predose salivary flow over<br />
time was evaluated to determine if <strong>the</strong>re was a carryover<br />
effect <strong>of</strong> pilocarpine <strong>the</strong>rapy. This was assessed by<br />
analyzing <strong>the</strong> mean predose salivary flow <strong>for</strong> each treat-<br />
60<br />
55<br />
50<br />
45<br />
40<br />
35<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
∗<br />
∗<br />
Decreased<br />
Use <strong>of</strong><br />
Saliva<br />
Substitutes<br />
∗<br />
<strong>Mouth</strong><br />
<strong>Dry</strong>ness<br />
∗<br />
Ability<br />
to Sleep<br />
∗<br />
Ocular<br />
Problems<br />
∗<br />
Visual<br />
Blurring<br />
∗<br />
Ability to<br />
Focus <strong>Eye</strong>s<br />
Nasal<br />
<strong>Dry</strong>ness<br />
Skin<br />
<strong>Dry</strong>ness<br />
ment group at each clinic visit. By <strong>the</strong> end <strong>of</strong> <strong>the</strong> study,<br />
<strong>the</strong>re was no change in predose salivary flow rates<br />
(P.10). There<strong>for</strong>e, no adjustment to postdose flow<br />
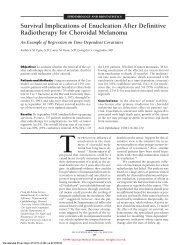
rates was required <strong>for</strong> <strong>the</strong> remaining analyses. As early<br />
as administration <strong>of</strong> <strong>the</strong> first dose <strong>of</strong> test drug at <strong>the</strong><br />
admission visit, <strong>the</strong> 5-mg pilocarpine group demonstrated<br />
a statistically significant increase (P.001) in<br />
salivary flow at all postdose collections (30, 60, <strong>and</strong> 90<br />
minutes) compared with <strong>the</strong> placebo group. This<br />
increase was maintained throughout <strong>the</strong> study. At<br />
admission, <strong>the</strong> mean (±SD) flow rates <strong>for</strong> placebo vs<br />
5-mg pilocarpine <strong>the</strong>rapy, respectively, were 0.11<br />
(±0.14) vs 0.11 (±0.15) mL/min be<strong>for</strong>e dosing; 0.12<br />
(±0.14) vs 0.34 (±0.53) mL/min 30 minutes after dosing;<br />
0.13 (±0.15) vs 0.34 (±0.45) mL/min 60 minutes<br />
after dosing; <strong>and</strong> 0.13 (±0.15) vs 0.27 (±0.34) mL/min<br />
90 minutes after dosing. Throughout <strong>the</strong> study, <strong>the</strong><br />
mean salivary flow rate 60 minutes after dosing was<br />
0.15 (±0.19) vs 0.33 (±0.41) mL/min (P.001) at week<br />
6, 0.17 (±0.13) vs 0.38 (±0.48) mL/min (P.001) at<br />
week 12, <strong>and</strong> 0.17 (±0.19) vs 0.37 (±0.46) mL/min at<br />
end point (P.001). Flow rates comparing <strong>the</strong> placebo<br />
<strong>and</strong> <strong>the</strong> 5-mg pilocarpine groups 60 minutes after dosing<br />
throughout <strong>the</strong> study are presented in Figure 2.<br />
At study end point, <strong>the</strong>re was no statistically significant<br />
difference between <strong>the</strong> 2.5-mg pilocarpine <strong>and</strong><br />
<strong>the</strong> placebo groups in 60-minute postdose mean salivary<br />
flow.<br />
ADVERSE EXPERIENCES<br />
Placebo Group<br />
5-mg <strong>Pilocarpine</strong> Group<br />
Ability to<br />
Expectorate<br />
Figure 1. Percentage <strong>of</strong> patients with Sjögren syndrome with clinically significant improvements in symptoms <strong>of</strong> dryness comparing treatment with 5-mg<br />
pilocarpine tablets 4 times daily (20 mg/d) vs placebo. No difference was noted <strong>for</strong> <strong>the</strong> 2.5-mg pilocarpine group vs <strong>the</strong> placebo group (data not shown). Left,<br />
Percentage <strong>of</strong> patients with Sjögren syndrome with a significant improvement in <strong>the</strong> global assessment <strong>of</strong> dry mouth <strong>and</strong> dry eyes (primary end points). Right,<br />
Percentage <strong>of</strong> patients with Sjögren syndrome with a clinically significant improvement in specific symptoms, including dry mouth, dry eyes, dry skin, dryness<br />
<strong>of</strong> <strong>the</strong> nasal passages, vaginal dryness, <strong>and</strong> ability to expectorate. Asterisk indicates P.04.<br />
Salivary Flow Rates, mL/min<br />
0.40<br />
0.35<br />
0.30<br />
0.25<br />
0.20<br />
0.15<br />
0.10<br />
0.05<br />
0.00<br />
Predose Placebo<br />
Postdose Placebo<br />
∗<br />
∗<br />
5-mg <strong>Pilocarpine</strong> Predose<br />
5-mg <strong>Pilocarpine</strong> Postdose<br />
Admission Visit Week 6 Visit Week 12 Visit End Point<br />
Figure 2. Comparison <strong>of</strong> mean salivary flow rates in patients receiving 5-mg<br />
pilocarpine tablets 4 times daily vs placebo. Predose flow rates across<br />
groups were not statistically different. All postdose saliva collections in <strong>the</strong><br />
5-mg pilocarpine group were statistically significantly (P.003) greater at all<br />
points (30, 60, <strong>and</strong> 90 minutes after dosing) throughout <strong>the</strong> study. The<br />
60-minute postdose collections (P.001) are plotted. No statistically<br />
significant change was noted at end point (<strong>the</strong> last available postdose<br />
observation <strong>for</strong> each patient) <strong>for</strong> <strong>the</strong> 2.5-mg pilocarpine group vs <strong>the</strong> placebo<br />
group (data not shown). Asterisk indicates P.001.<br />
Downloaded From: http://173.193.11.201/ on 04/10/2013<br />
∗<br />
∗<br />
ARCH INTERN MED/ VOL 159, JAN 25, 1999<br />
178<br />
©1999 American Medical Association. All rights reserved.<br />
Vaginal<br />
<strong>Dry</strong>ness<br />
No serious drug-related adverse experiences were reported<br />
in this study. The most frequently reported adverse<br />
experiences (10% in any treatment group) are<br />
shown in Table 4. Sweating was <strong>the</strong> most frequently reported<br />
event. The assessment <strong>of</strong> a possible relationship<br />
between use <strong>of</strong> <strong>the</strong> study medication <strong>and</strong> <strong>the</strong> occurrence<br />
<strong>of</strong> an adverse experience was based on ei<strong>the</strong>r <strong>the</strong><br />
known pharmacologic properties <strong>of</strong> pilocarpine or a statistically<br />
significant increase in incidence in <strong>the</strong> 5-mg pi-<br />
∗<br />
∗<br />
∗<br />
∗
Table 4. Incidence <strong>of</strong> Adverse Experiences<br />
(10% in Any <strong>Treatment</strong> Group)*<br />
Adverse<br />
Experience<br />
Placebo<br />
<strong>Tablets</strong><br />
(n = 125)<br />
<strong>Pilocarpine</strong> <strong>Tablets</strong><br />
(n = 248)<br />
2.5 mg<br />
(n = 121)<br />
5mg<br />
(n = 127)<br />
Overall P<br />
Sweating† 9 (7.2) 13 (10.7) 55 (43.3) .001<br />
Headache 31 (24.8) 25 (20.7) 20 (15.8) .20<br />
Flu syndrome 11 (8.8) 16 (13.2) 18 (14.2) .38<br />
Nausea 11 (8.8) 15 (12.4) 15 (11.8) .62<br />
Rhinitis 7 (5.6) 9 (7.4) 13 (10.2) .38<br />
Dizziness 11 (8.8) 6 (5.0) 13 (‘0.2) .29<br />
Urinary<br />
frequency†<br />
2 (1.6) 13 (10.7) 12 (9.5) .01<br />
*Data are given as number (percentage).<br />
†Events with a probable relationship to pilocarpine use. O<strong>the</strong>r events with<br />
a probable relationship to drug use but with 10% incidence are flushing<br />
(placebo group, 1.6%; 2.5-mg pilocarpine group, 1.7%; <strong>and</strong> 5-mg<br />
pilocarpine group, 9.5%) <strong>and</strong> increased salivation (0%, 0%, <strong>and</strong> 2.4%,<br />
respectively).<br />
locarpine group compared with <strong>the</strong> placebo group. The<br />
adverse experiences meeting 1 or more <strong>of</strong> <strong>the</strong>se criteria<br />
(Table 4) were sweating (placebo group, 7.2%; 2.5-mg<br />
pilocarpine group, 10.7%; <strong>and</strong> 5-mg pilocarpine group,<br />
43.3%), urinary frequency (1.6%, 10.7%, <strong>and</strong> 9.5%, respectively),<br />
flushing (1.6%, 1.7%, <strong>and</strong> 9.5%, respectively),<br />
<strong>and</strong> increased salivation (0%, 0%, <strong>and</strong> 2.4%, respectively).<br />
These events were typically <strong>of</strong> mild or<br />
moderate intensity <strong>and</strong> occurred in roughly dosedependent<br />
fashion. The events reported with severe intensity<br />
were sweating (4 patients) <strong>and</strong> urinary frequency<br />
(1 patient), all <strong>of</strong> which were in <strong>the</strong> 5-mg<br />
pilocarpine group. A review <strong>of</strong> adverse experiences in patients<br />
who entered <strong>the</strong> study with a history <strong>of</strong> respiratory<br />
abnormalities, including asthma (placebo group,<br />
n = 31; 2.5-mg pilocarpine group, n = 27; <strong>and</strong> 5-mg pilocarpine<br />
group, n = 27), showed a comparable incidence<br />
<strong>of</strong> adverse events as that reported in <strong>the</strong> total population.<br />
In <strong>the</strong> 5-mg pilocarpine group, <strong>the</strong> most commonly<br />
reported events (10%) vs placebo, respectively,<br />
were sweating (55.6% vs 12.9%), headache (14.8%<br />
vs 22.6%), nausea (22.2% vs 12.9%), flu syndrome (14.8%<br />
vs 6.5%), diarrhea (11.1% vs 3.2%), dizziness (11.1% vs<br />
6.5%), <strong>and</strong> dyspepsia (0% vs 12.9%). One case <strong>of</strong> bronchitis<br />
was reported during this study in a patient receiving<br />
5-mg pilocarpine tablets 4 times daily.<br />
Two percent (5/248) <strong>of</strong> <strong>the</strong> patients taking pilocarpine<br />
tablets withdrew from <strong>the</strong> study because <strong>of</strong> 1 or more<br />
drug-related adverse experiences, ie, 1 patient receiving<br />
2.5-mg pilocarpine tablets (urinary frequency) <strong>and</strong> 4<br />
patients receiving 5-mg pilocarpine tablets (sweating, 4<br />
patients; flushing, 1 patient; <strong>and</strong> hypersalivation, 1 patient).<br />
Of <strong>the</strong> total population, a comparable proportion<br />
<strong>of</strong> patients from each treatment group (5.6%-7.4%) withdrew<br />
because <strong>of</strong> adverse experiences, whe<strong>the</strong>r or not related<br />
to use <strong>of</strong> <strong>the</strong> study drug (Table 3). Of <strong>the</strong> remaining<br />
reasons <strong>for</strong> withdrawal, none differed among treatment<br />
groups by more than 1 patient. One patient, in <strong>the</strong> 2.5-mg<br />
pilocarpine group, died during <strong>the</strong> study because <strong>of</strong> complications<br />
<strong>of</strong> a probable pulmonary embolus <strong>and</strong> Clos-<br />
Downloaded From: http://173.193.11.201/ on 04/10/2013<br />
ARCH INTERN MED/ VOL 159, JAN 25, 1999<br />
179<br />
©1999 American Medical Association. All rights reserved.<br />
tridium difficile enterocolitis. The investigator <strong>and</strong> treating<br />
physician did not consider <strong>the</strong>se events to have any<br />
relationship to use <strong>of</strong> <strong>the</strong> study drug.<br />
Two VAS questions were asked to assess <strong>the</strong> potential<br />
adverse effects <strong>of</strong> pilocarpine tablets on vision after<br />
administration <strong>of</strong> <strong>the</strong> study drug: difficulty with night driving<br />
<strong>and</strong> difficulty reading (visual acuity). No exacerbation<br />
<strong>of</strong> <strong>the</strong>se symptoms was noted during <strong>the</strong> study after<br />
use <strong>of</strong> 2.5- or 5-mg pilocarpine tablets (P = .64 <strong>and</strong> P = .63,<br />
respectively).<br />
COMMENT<br />
Saliva is a chemically complex fluid containing several<br />
organic <strong>and</strong> inorganic components, all <strong>of</strong> which play an<br />
essential role in maintaining oral health. 18 Saliva is not<br />
only required to preserve <strong>the</strong> dentition <strong>and</strong> mucosal surfaces<br />
but also to facilitate digestion, phonation, mastication,<br />
deglutition, <strong>and</strong> gustation. There<strong>for</strong>e, <strong>the</strong> oral consequences<br />
<strong>of</strong> salivary gl<strong>and</strong> hyp<strong>of</strong>unction extend beyond<br />
those <strong>of</strong> a dry mouth. Common oral symptoms in SS can<br />
also include dysphonia, dysphagia, stomatopyrosis (burning<br />
mouth), dysgeusia (altered taste), oral ulcers, <strong>and</strong> sleep<br />
disruption caused by nocturnal fluid ingestion. 5,19 Attempts<br />
to treat <strong>the</strong>se symptoms with replacement <strong>the</strong>rapy<br />
using artificial salivas <strong>and</strong> oral lubricants have been largely<br />
unsuccessful, <strong>and</strong> patient satisfaction <strong>and</strong> compliance have<br />
been low. 20<br />
For <strong>the</strong> treatment <strong>of</strong> symptoms associated with dry<br />
eyes in primary <strong>and</strong> secondary SS, <strong>the</strong>re is a plethora <strong>of</strong><br />
artificial tear <strong>and</strong> lubricant preparations available. However,<br />
<strong>the</strong> frequency with which <strong>the</strong>y must be applied suggests<br />
<strong>the</strong> need <strong>for</strong> novel <strong>the</strong>rapeutic interventions. Ultimately,<br />
tear preservation by punctal occlusion or cautery<br />
is <strong>the</strong> last resort to solve this problem. To date, no artificial<br />
tear or saliva preparation has successfully duplicated<br />
<strong>the</strong> physiochemical properties <strong>of</strong> <strong>the</strong> body’s own<br />
fluids well enough to provide a comparable degree <strong>of</strong><br />
benefit.<br />
The medicinal properties <strong>of</strong> pilocarpine, including<br />
its ability to stimulate salivation, have been recognized<br />
<strong>for</strong> many centuries by <strong>the</strong> Tupi Indian tribe <strong>of</strong> nor<strong>the</strong>rn<br />
Brazil, who named this indigenous shrub “jabor<strong>and</strong>i,” or<br />
<strong>the</strong> “slobber-mouth plant.” In 1888, a British physician<br />
21 described a 65-year-old woman with xerostomia<br />
<strong>and</strong> xerophthalmia who probably had SS <strong>and</strong> who responded<br />
symptomatically to treatment with tincture <strong>of</strong><br />
jabor<strong>and</strong>i, administered orally <strong>and</strong> subcutaneously. The<br />
benefit <strong>of</strong> pilocarpine tablets <strong>for</strong> treatment <strong>of</strong> symptoms<br />
<strong>of</strong> dry mouth from various causes, including SS, has been<br />
previously suggested in smaller studies <strong>and</strong> case reports.<br />
22-26 Data from <strong>the</strong> present multicenter trial indicate<br />
that <strong>the</strong> use <strong>of</strong> 5-mg pilocarpine tablets administered<br />
4 times daily (20 mg/d) provides significant<br />
symptomatic relief <strong>of</strong> dry mouth caused by SS <strong>and</strong> significantly<br />
increases saliva production in measurable quantities.<br />
Regular use <strong>of</strong> pilocarpine tablets at this dosage significantly<br />
improves o<strong>the</strong>r specific symptoms <strong>of</strong> salivary<br />
gl<strong>and</strong> hyp<strong>of</strong>unction in patients with SS, such as oral discom<strong>for</strong>t,<br />
nocturnal fluid ingestion, <strong>and</strong> <strong>the</strong> need <strong>for</strong> saliva<br />
substitutes. Some benefit <strong>for</strong> dysphonia may also occur,<br />
as evidenced by <strong>the</strong> trend toward statistically
significant improvement in <strong>the</strong> 5-mg pilocarpine group<br />
<strong>for</strong> this symptom.<br />
Although <strong>the</strong> data show that pilocarpine-induced<br />
stimulation <strong>of</strong> salivary flow occurred within 30 minutes<br />
<strong>of</strong> ingestion <strong>of</strong> <strong>the</strong> first dose <strong>and</strong> was maintained through<br />
week 12, <strong>the</strong> onset <strong>of</strong> subjective benefit <strong>for</strong> various symptoms<br />
took 6 to 12 weeks. Because dry mouth develops<br />
ra<strong>the</strong>r insidiously in most patients with SS, 27 it is not unreasonable<br />
to expect that improvement or reversal <strong>of</strong><br />
symptoms after treatment would be delayed. This observation<br />
suggests that a patient’s symptoms on a given day<br />
may reflect not only <strong>the</strong> quantity <strong>of</strong> saliva but also <strong>the</strong><br />
cumulative effect <strong>of</strong> chronic tissue dehydration. For this<br />
reason, it seems that a prolonged treatment course with<br />
pilocarpine tablets (eg, 6-12 weeks) should be recommended<br />
to patients to allow sufficient time <strong>for</strong> symptomatic<br />
benefits to occur. In this study, <strong>the</strong> most dramatic<br />
response occurred in patients who took 5-mg<br />
pilocarpine tablets 4 times daily. Although salivary flow<br />
rates were measured during only <strong>the</strong> first 90 minutes <strong>of</strong><br />
<strong>the</strong> dosing interval, results <strong>of</strong> previous studies 16 in healthy<br />
participants indicate that <strong>the</strong> pilocarpine effect on flow<br />
rates lasts 3 to 5 hours. Optimal <strong>the</strong>rapeutic benefit can<br />
<strong>the</strong>re<strong>for</strong>e be best achieved through a 4-times-daily dosing<br />
regimen.<br />
Results <strong>of</strong> this study also indicate symptomatic relief<br />
<strong>of</strong> dry eyes after use <strong>of</strong> 5-mg pilocarpine tablets 4 times<br />
daily. Significantly more patients reported improvement<br />
in <strong>the</strong>ir global assessment <strong>of</strong> dry eyes, blurred vision,<br />
ability to focus <strong>the</strong> eyes during reading, <strong>and</strong> ocular<br />
problems in <strong>the</strong> higher-dose (5-mg) treatment group compared<br />
with <strong>the</strong> placebo group. However, some ocular<br />
symptoms did not significantly change. This could be due<br />
to a differential degree <strong>of</strong> cholinergic stimulation by pilocarpine<br />
on <strong>the</strong> eyes compared with <strong>the</strong> mouth or could<br />
reflect <strong>the</strong> need <strong>for</strong> higher doses or a longer treatment<br />
period to achieve maximal benefit. As noted in a second<br />
study 28 <strong>of</strong> pilocarpine tablet use <strong>for</strong> patients with SS, which<br />
used doses up to 30 mg/d, statistically significant response<br />
<strong>for</strong> relief <strong>of</strong> ocular symptoms was observed in 8<br />
<strong>of</strong> 9 measures in <strong>the</strong> pilocarpine group compared with<br />
<strong>the</strong> placebo group.<br />
As one could predict from pilocarpine’s pharmacological<br />
effect, this investigation also suggests that pilocarpine<br />
tablets, at doses <strong>of</strong> 20 mg/d, can stimulate exocrine<br />
gl<strong>and</strong> secretion in o<strong>the</strong>r organ systems besides <strong>the</strong><br />
eyes <strong>and</strong> mouth. At study end point, statistically significant<br />
improvement was also observed in o<strong>the</strong>r sicca symptoms<br />
associated with SS, including nasal dryness, dry skin,<br />
vaginitis sicca, <strong>and</strong> <strong>the</strong> ability to expectorate. These data<br />
<strong>the</strong>re<strong>for</strong>e suggest that treatment with pilocarpine tablets<br />
not only <strong>of</strong>fers relief <strong>of</strong> symptoms <strong>of</strong> dry mouth <strong>and</strong><br />
dry eyes but <strong>of</strong> whole-body dryness as well.<br />
In this multicenter trial, <strong>the</strong> incidence <strong>of</strong> adverse effects<br />
related to <strong>the</strong> use <strong>of</strong> pilocarpine tablets reflected <strong>the</strong><br />
cholinergic activity <strong>of</strong> this drug. 6,29 The most common<br />
drug-related adverse experiences included sweating, urinary<br />
frequency, <strong>and</strong> flushing. Despite a relatively high<br />
incidence <strong>of</strong> sweating, this <strong>and</strong> o<strong>the</strong>r adverse effects were<br />
perceived as minor by most patients, <strong>and</strong> <strong>the</strong> withdrawal<br />
rate due to drug-related adverse experiences was<br />
low (2%). No significant differences between treatment<br />
Downloaded From: http://173.193.11.201/ on 04/10/2013<br />
ARCH INTERN MED/ VOL 159, JAN 25, 1999<br />
180<br />
©1999 American Medical Association. All rights reserved.<br />
groups were observed <strong>for</strong> alterations in blood pressure<br />
or heart rate, <strong>and</strong> no drug-related serious events were reported,<br />
including hematopoietic, renal, or hepatotoxic<br />
effects. No significant drug interactions were noted. This<br />
study did not demonstrate any pulmonary safety issues<br />
in this patient population. However, <strong>the</strong> package insert<br />
16 <strong>for</strong> Salagen tablets (oral pilocarpine) does note that<br />
pilocarpine should be administered with caution <strong>and</strong> under<br />
close supervision to patients with controlled asthma,<br />
chronic bronchitis, or chronic obstructive pulmonary disease<br />
requiring medical <strong>the</strong>rapy.<br />
From a physiologic st<strong>and</strong>point, treatment <strong>of</strong> patients<br />
with SS with a systemic cholinergic agonist such<br />
as pilocarpine to stimulate <strong>the</strong> body’s own multiorgan secretions<br />
not only is <strong>the</strong> most efficacious <strong>and</strong> costeffective<br />
strategy to alleviate multiple symptoms but also<br />
<strong>of</strong>fers <strong>the</strong> best potential treatment <strong>for</strong> prevention <strong>of</strong> longterm<br />
complications caused by severe dryness. Although<br />
<strong>the</strong> efficacy <strong>of</strong> long-term oral pilocarpine <strong>the</strong>rapy <strong>for</strong> dental<br />
caries prophylaxis or prevention <strong>of</strong> oral infections in<br />
humans is not known, data from animal models suggest<br />
such a possible benefit. In a study 30 <strong>of</strong> partially desalivated<br />
rats fed a cariogenic diet, treatment with pilocarpine<br />
reduced <strong>the</strong> incidence <strong>of</strong> sulcal cavities compared<br />
with nontreated controls. These findings did not significantly<br />
correlate with a lower incidence <strong>of</strong> infection by<br />
cariogenic bacteria (eg, Streptococcus sobrinus). However,<br />
in ano<strong>the</strong>r study, 31 <strong>the</strong> incidence <strong>of</strong> oral infection<br />
by S sobrinus in surgically desalivated rats was significantly<br />
reduced after pilocarpine treatment compared with<br />
untreated controls. Fur<strong>the</strong>rmore, stimulation <strong>of</strong> salivary<br />
flow by pilocarpine treatment can reportedly reverse<br />
sucrose-induced fissure caries in albino rats. 32 Consequently,<br />
fur<strong>the</strong>r studies to determine this treatment’s<br />
ability to prevent complications (eg, dental caries) from<br />
dry mouth <strong>and</strong> o<strong>the</strong>r sicca symptoms from SS seem reasonable.<br />
In conclusion, <strong>the</strong> administration <strong>of</strong> 5-mg pilocarpine<br />
tablets 4 times daily (20 mg/d in divided doses) produced<br />
significant benefits <strong>for</strong> <strong>the</strong> symptomatic treatment<br />
<strong>of</strong> dryness associated with SS that clearly outweighed<br />
adverse effects <strong>and</strong> risks in this 12-week study. Patients<br />
experienced improvement in symptoms <strong>of</strong> dry mouth <strong>and</strong><br />
dry eyes, <strong>and</strong> improvement in dryness <strong>of</strong> <strong>the</strong> nose, skin,<br />
<strong>and</strong> vagina <strong>and</strong> <strong>the</strong> ability to expectorate. <strong>Treatment</strong> success<br />
with pilocarpine will most likely depend on existence<br />
<strong>of</strong> residual exocrine gl<strong>and</strong> function. In SS, this may<br />
vary in different organs <strong>and</strong> cannot always be predicted<br />
based on <strong>the</strong> duration <strong>of</strong> symptoms. As data from <strong>the</strong> present<br />
study suggest, use <strong>of</strong> pilocarpine tablets <strong>of</strong>fers a wide<br />
range <strong>of</strong> potential <strong>the</strong>rapeutic effects <strong>for</strong> patients with SS.<br />
There<strong>for</strong>e, at <strong>the</strong> present time, almost any patient with<br />
SS with some degree <strong>of</strong> exocrine gl<strong>and</strong> function could<br />
potentially benefit from this treatment depending on <strong>the</strong>rapeutic<br />
goals. As with o<strong>the</strong>r patient groups with rheumatic<br />
conditions, early diagnosis <strong>and</strong> treatment <strong>of</strong>fer <strong>the</strong><br />
best hope <strong>for</strong> a good outcome.<br />
Accepted <strong>for</strong> publication May 19, 1998.<br />
From <strong>the</strong> Division <strong>of</strong> Rheumatology, University <strong>of</strong> Pennsylvania<br />
Health System, Philadelphia (Dr Vivino); Department<br />
<strong>of</strong> Periodontics, Baylor College <strong>of</strong> Dentistry, Dallas,
Tex (Dr Al-Hashimi); Department <strong>of</strong> Dental Oncology <strong>and</strong><br />
Maxill<strong>of</strong>acial Prosthodontics, J. Graham Brown Cancer Center,<br />
Louisville, Ky (Dr Khan); Department <strong>of</strong> Oral Medicine,<br />
Harper Hospital, Detroit, Mich (Dr LeVeque); Department<br />
<strong>of</strong> Dentistry, Bowman Gray School <strong>of</strong> Medicine,<br />
Winston-Salem, NC (Dr Salisbury); Cali<strong>for</strong>nia Neuropsychopharmacology<br />
Clinical Research Institute, San Diego (Dr<br />
Tran-Johnson); <strong>and</strong> MGI Pharma Inc, Minnetonka, Minn<br />
(Drs Muscoplat, Trivedi, <strong>and</strong> Goldlust <strong>and</strong> Ms Gallagher).<br />
This study was supported by grants from MGI Pharma<br />
Inc.<br />
Members <strong>of</strong> <strong>the</strong> P92-01 Study Group are Michael Ellman,<br />
MD, The University <strong>of</strong> Chicago, Chicago, Ill; Robert<br />
I. Fox, MD, Scripps Clinic & Research Foundation, La Jolla,<br />
Calif; Daniel Furst, MD, Virginia Mason Research Center,<br />
Seattle, Wash; W. Leroy Griffing, MD, Mayo Clinic,<br />
Scottsdale, Ariz; Cyril Meyerowitz, DDS, University <strong>of</strong> Rochester,<br />
Rochester, NY; Nelson L. Rhodus, DMD, University<br />
<strong>of</strong> Minnesota, Minneapolis; Stephen Sonis, DMD, Brigham<br />
<strong>and</strong> Women’s Hospital, Boston, Mass; Leo M. Sreebny, DDS,<br />
State University <strong>of</strong> New York at Stony Brook, Stony Brook;<br />
Norman Talal, MD, University <strong>of</strong> Texas Health Science Center,<br />
San Antonio; Frederick Wolfe, MD, Arthritis Research<br />
<strong>and</strong> Clinical Centers, Wichita, Kan; <strong>and</strong> Richard Yee, University<br />
<strong>of</strong> Texas Science Center, Houston.<br />
Reprints: Frederick B. Vivino, MD, Division <strong>of</strong> Rheumatology,<br />
Thomas Jefferson University, 1015 Walnut St,<br />
Suite 613, Philadelphia, PA 19107.<br />
REFERENCES<br />
1. Talal N, Moutsopoulos H, Kassan S, eds. Sjögren’s Syndrome: Clinical <strong>and</strong> Immunological<br />
Aspects. Heidelberg, Germany: Springer-Verlag; 1987.<br />
2. Fox RI, Kang H. Sjögren’s syndrome. In: Kelly WM, Harris ED, Ruddy S, Sledge<br />
CB, eds. Textbook <strong>of</strong> Rheumatology. 4th ed. Philadelphia, Pa: WB Saunders Co;<br />
1993:931-942.<br />
3. Daniels TE, Fox PC. Salivary <strong>and</strong> oral components <strong>of</strong> Sjögren’s syndrome. Rheum<br />
Dis Clin North Am. 1992;18:571-589.<br />
4. Friedlaender MH. Ocular manifestations <strong>of</strong> Sjögren’s syndrome: keratoconjunctivitis<br />
sicca. Rheum Dis Clin North Am. 1992;18:591-608.<br />
5. Vivino FB, Katz WA. Sjögren’s syndrome: clinical picture <strong>and</strong> diagnostic tests.<br />
J Musculoskel Med. 1995;12:40-52.<br />
6. Taylor P. Cholinergic agonists. In: Gilman AG, Rall TW, Nies AS, Taylor P, eds.<br />
Goodman <strong>and</strong> Gilman’s: The Pharmacologic Basis <strong>of</strong> Therapeutics. 8th ed. New<br />
York, NY: Pergamon Press Inc; 1990:122-130.<br />
7. Wiseman LR, Faulds D. Oral pilocarpine: a review <strong>of</strong> its pharmacological properties<br />
<strong>and</strong> clinical potential in xerostomia. Drugs. 1995;49:143-155.<br />
8. Johnson JT, Ferretti GA, Ne<strong>the</strong>ry WJ, et al. Oral pilocarpine <strong>for</strong> post-radiation<br />
xerostomia in patients with head <strong>and</strong> neck cancer. N Engl J Med. 1993;329:390-<br />
395.<br />
9. LeVeque FG, Montgomery M, Potter D, et al. A multicenter, r<strong>and</strong>omized, doubleblind,<br />
placebo-controlled dose titration study <strong>of</strong> oral pilocarpine <strong>for</strong> treatment <strong>of</strong><br />
Downloaded From: http://173.193.11.201/ on 04/10/2013<br />
ARCH INTERN MED/ VOL 159, JAN 25, 1999<br />
181<br />
©1999 American Medical Association. All rights reserved.<br />
radiation-induced xerostomia in head <strong>and</strong> neck cancer patients. J Clin Oncol. 1993;<br />
11:1124-1131.<br />
10. Vitali A, Bombardieri S, Moutopoulos HM, et al. Preliminary criteria <strong>for</strong> <strong>the</strong> classification<br />
<strong>of</strong> Sjögren’s syndrome. Arthritis Rheum. 1993;36:341-347.<br />
11. Daniels TE. Labial salivary gl<strong>and</strong> biopsy in Sjögren’s syndrome: assessment as<br />
a diagnostic criteria in 362 suspected cases. Arthritis Rheum. 1984;27:147-<br />
156.<br />
12. Skopouli FN, Siouna-Fatourou HI, Ziciadis C, Moutsopoulos HM. Evaluation <strong>of</strong><br />
unstimulated whole saliva flow rate <strong>and</strong> stimulated parotid flow as confirmatory<br />
tests <strong>for</strong> xerostomia. Clin Exp Rheumatol. 1989;7:127-129.<br />
13. PDR Guide to Interactions, Side Effects, Indications, Contraindications. 48th <strong>and</strong><br />
49th eds. Montvale, NJ: Medical Economics Books; 1994 <strong>and</strong> 1995.<br />
14. Sreebny LM, Schwartz SS. A reference guide to drugs <strong>and</strong> dry mouth. Gerodontology.<br />
1986;5:75-99.<br />
15. Van Bijsterveld OP. Diagnostic tests in <strong>the</strong> sicca syndrome. Arch Ophthalmol.<br />
1969;82:10-14.<br />
16. Salagen tablets. In: Physicians’ Desk Reference. 51st ed. Montvale, NJ: Medical<br />
Economics Books; 1997:1546-1547.<br />
17. Talal N. What is Sjögren’s syndrome? In: Harris E, Carsons S, Sciubba JJ, Talal<br />
N, eds. Sjögren’s Syndrome H<strong>and</strong>book. Port Washington, NY: Sjögren’s Syndrome<br />
Foundation Inc; 1989:3-9.<br />
18. M<strong>and</strong>el ID. The role <strong>of</strong> saliva in maintaining oral homeostasis. J Am Dent Assoc.<br />
1989;119:298-304.<br />
19. Rhodus NL. Xerostomia <strong>and</strong> glossodynia in patients with autoimmune disorders.<br />
Ear Nose Throat J. 1989;58:791-794.<br />
20. Vivino FB, Shore JS, Huang CH, May RM. Sjögren’s syndrome patient preferences<br />
<strong>for</strong> xerostomia treatments [abstract]. Arthritis Rheum. 1996;39(suppl):<br />
S63.<br />
21. Hadden WB. On dry mouth, or suppression <strong>of</strong> <strong>the</strong> salivary <strong>and</strong> buccal secretions.<br />
In: Transactions <strong>of</strong> <strong>the</strong> Clinical Society <strong>of</strong> London. Vol 5. London, Engl<strong>and</strong>:<br />
Longmans Green & Co; 1888:176-179.<br />
22. Fox PC, van der Ven PF, Baum BJ, M<strong>and</strong>el ID. <strong>Pilocarpine</strong> <strong>for</strong> <strong>the</strong> treatment <strong>of</strong><br />
xerostomia associated with salivary gl<strong>and</strong> dysfunction. Oral Surg Oral Med Oral<br />
Pathol Oral Radiol Endod. 1986;61:243-248.<br />
23. Greenspan D, Daniels T. Effectiveness <strong>of</strong> pilocarpine in postradiation xerostomia.<br />
Cancer. 1987;59:1123-1125.<br />
24. Fox PC, Atkinson JC, Macynski AA, et al. <strong>Pilocarpine</strong> treatment <strong>of</strong> salivary gl<strong>and</strong><br />
hyp<strong>of</strong>unction <strong>and</strong> dry mouth (xerostomia). Arch Intern Med. 1991;151:1149-<br />
1152.<br />
25. Rhodus NL, Schuh MJ. Effects <strong>of</strong> pilocarpine on salivary flow in patients with<br />
Sjögren’s syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1991;<br />
72:545-549.<br />
26. Singhal S, Mehta J, Rattenbury H, Treleaven J, Powles R. Oral pilocarpine hydrochloride<br />
<strong>for</strong> <strong>the</strong> treatment <strong>of</strong> refractory xerostomia associated with chronic<br />
graft-versus-host disease. Blood. 1995;85:1147-1148.<br />
27. Moutsopoulos HM. Sjögren’s syndrome. In: Schumacher HR, Klippel JH, Koopman<br />
WJ, eds. Primer <strong>of</strong> <strong>the</strong> Rheumatic Diseases. 10th ed. Atlanta, Ga: Arthritis<br />
Foundation; 1993:131-135.<br />
28. Sherrer Y, Charney M, Golden H, et al. The efficacy <strong>and</strong> safety <strong>of</strong> oral pilocarpine<br />
HCl tablets <strong>for</strong> <strong>the</strong> treatment <strong>of</strong> dry eye symptoms associated with Sjögren’s syndrome:<br />
a dose titration study [abstract]. Arthritis Rheum. 1997;40(suppl):S202.<br />
29. Greco J, Kelman C. Systemic pilocarpine toxicity in <strong>the</strong> treatment <strong>of</strong> angle closure<br />
glaucoma. Ann Ophthalmol. 1993;5:57-59.<br />
30. O’Connell AC, Pearson SK, Bowen WH. <strong>Pilocarpine</strong> alters caries development in<br />
partially desalivated rats. J Dent Res. 1994;73:637-643.<br />
31. Ortiz GC, Pearson SK, Bowen WH. Influence <strong>of</strong> pilocarpine, propranolol, <strong>and</strong> atropine<br />
on susceptibility to infection [abstract]. J Dent Res. 1992;71:129.<br />
32. Leach SA, Connell R. Reversal <strong>of</strong> fissure caries in <strong>the</strong> albino rat by stimulating<br />
salivary flow with pilocarpine. Caries Res. 1990;24:127-129.