Excimer laser refractive surgery : corneal wound ... - Helda - Helsinki.fi
Excimer laser refractive surgery : corneal wound ... - Helda - Helsinki.fi
Excimer laser refractive surgery : corneal wound ... - Helda - Helsinki.fi
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
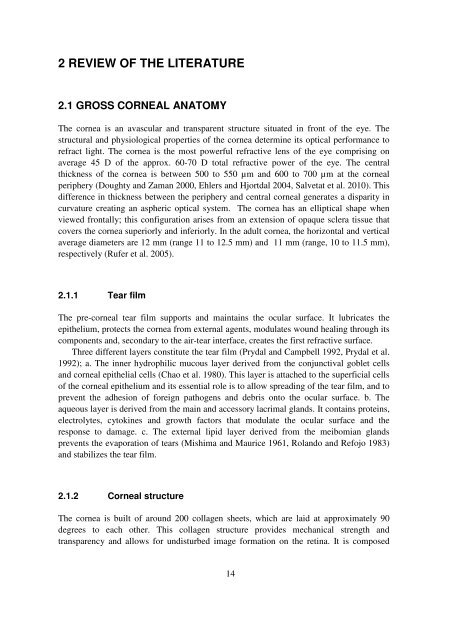
2 REVIEW OF THE LITERATURE<br />
2.1 GROSS CORNEAL ANATOMY<br />
The cornea is an avascular and transparent structure situated in front of the eye. The<br />
structural and physiological properties of the cornea determine its optical performance to<br />
refract light. The cornea is the most powerful <strong>refractive</strong> lens of the eye comprising on<br />
average 45 D of the approx. 60-70 D total <strong>refractive</strong> power of the eye. The central<br />
thickness of the cornea is between 500 to 550 µm and 600 to 700 µm at the <strong>corneal</strong><br />
periphery (Doughty and Zaman 2000, Ehlers and Hjortdal 2004, Salvetat et al. 2010). This<br />
difference in thickness between the periphery and central <strong>corneal</strong> generates a disparity in<br />
curvature creating an aspheric optical system. The cornea has an elliptical shape when<br />
viewed frontally; this con<strong>fi</strong>guration arises from an extension of opaque sclera tissue that<br />
covers the cornea superiorly and inferiorly. In the adult cornea, the horizontal and vertical<br />
average diameters are 12 mm (range 11 to 12.5 mm) and 11 mm (range, 10 to 11.5 mm),<br />
respectively (Rufer et al. 2005).<br />
2.1.1 Tear <strong>fi</strong>lm<br />
The pre-<strong>corneal</strong> tear <strong>fi</strong>lm supports and maintains the ocular surface. It lubricates the<br />
epithelium, protects the cornea from external agents, modulates <strong>wound</strong> healing through its<br />
components and, secondary to the air-tear interface, creates the <strong>fi</strong>rst <strong>refractive</strong> surface.<br />
Three different layers constitute the tear <strong>fi</strong>lm (Prydal and Campbell 1992, Prydal et al.<br />
1992); a. The inner hydrophilic mucous layer derived from the conjunctival goblet cells<br />
and <strong>corneal</strong> epithelial cells (Chao et al. 1980). This layer is attached to the super<strong>fi</strong>cial cells<br />
of the <strong>corneal</strong> epithelium and its essential role is to allow spreading of the tear <strong>fi</strong>lm, and to<br />
prevent the adhesion of foreign pathogens and debris onto the ocular surface. b. The<br />
aqueous layer is derived from the main and accessory lacrimal glands. It contains proteins,<br />
electrolytes, cytokines and growth factors that modulate the ocular surface and the<br />
response to damage. c. The external lipid layer derived from the meibomian glands<br />
prevents the evaporation of tears (Mishima and Maurice 1961, Rolando and Refojo 1983)<br />
and stabilizes the tear <strong>fi</strong>lm.<br />
2.1.2 Corneal structure<br />
The cornea is built of around 200 collagen sheets, which are laid at approximately 90<br />
degrees to each other. This collagen structure provides mechanical strength and<br />
transparency and allows for undisturbed image formation on the retina. It is composed<br />
14