Contents Chapter Topic Page Neonatology Respiratory Cardiology
Contents Chapter Topic Page Neonatology Respiratory Cardiology
Contents Chapter Topic Page Neonatology Respiratory Cardiology
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
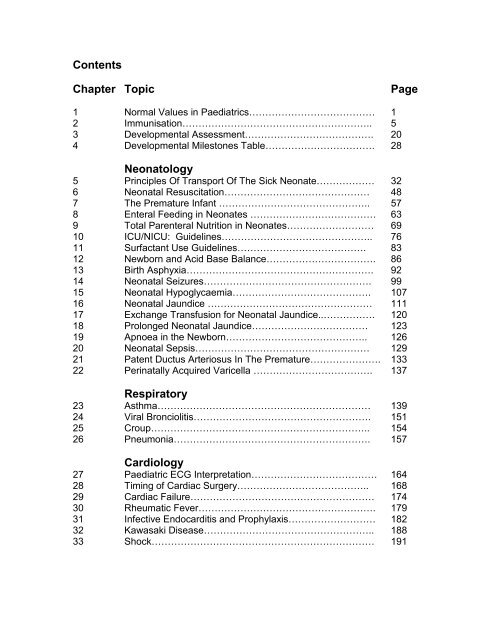
<strong>Contents</strong><br />
<strong>Chapter</strong> <strong>Topic</strong> <strong>Page</strong><br />
1 Normal Values in Paediatrics………………………………… 1<br />
2 Immunisation………………………………………………….. 5<br />
3 Developmental Assessment…………………………………. 20<br />
4 Developmental Milestones Table……………………………. 28<br />
<strong>Neonatology</strong><br />
5 Principles Of Transport Of The Sick Neonate……………… 32<br />
6 Neonatal Resuscitation……………………………………… 48<br />
7 The Premature Infant ……………………………………….. 57<br />
8 Enteral Feeding in Neonates ………………………………… 63<br />
9 Total Parenteral Nutrition in Neonates……………………… 69<br />
10 ICU/NICU: Guidelines……………………………………….. 76<br />
11 Surfactant Use Guidelines…………………………………. 83<br />
12 Newborn and Acid Base Balance……………………………. 86<br />
13 Birth Asphyxia…………………………………………………. 92<br />
14 Neonatal Seizures……………………………………………. 99<br />
15 Neonatal Hypoglycaemia……………………………………. 107<br />
16 Neonatal Jaundice …………………………………………… 111<br />
17 Exchange Transfusion for Neonatal Jaundice..……………. 120<br />
18 Prolonged Neonatal Jaundice……………………………… 123<br />
19 Apnoea in the Newborn…………………………………….. 126<br />
20 Neonatal Sepsis……………………………………………… 129<br />
21 Patent Ductus Arteriosus In The Premature…………………. 133<br />
22 Perinatally Acquired Varicella ………………………………. 137<br />
<strong>Respiratory</strong><br />
23 Asthma………………………………………………………… 139<br />
24 Viral Bronciolitis………………………………………………. 151<br />
25 Croup………………………………………………………….. 154<br />
26 Pneumonia……………………………………………………. 157<br />
<strong>Cardiology</strong><br />
27 Paediatric ECG Interpretation………………………………… 164<br />
28 Timing of Cardiac Surgery………………………………….. 168<br />
29 Cardiac Failure………………………………………………… 174<br />
30 Rheumatic Fever………………………………………………. 179<br />
31 Infective Endocarditis and Prophylaxis……………………… 182<br />
32 Kawasaki Disease…………………………………………….. 188<br />
33 Shock…………………………………………………………… 191
Neurology<br />
34 Febrile Convulsions……………………………………………. 192<br />
35 Epilepsy…………………………………………………………. 196<br />
36 Meningitis……………………………………………………….. 204<br />
37 Child with Altered Consciousness…………………………… 210<br />
38 Brain Death…………………………………………………… 217<br />
Endocrinology<br />
39 Diabetes Mellitus ……………………………………………… 223<br />
40 Congenital Hypothyroidism…………………………………… 234<br />
41 Ambiguous Genitalia………………………………………… 240<br />
42 Congenital Adrenal Hyperplasia……………………………. 246<br />
Nephrology<br />
43 Acute Glomerulonephritis…………………………………….. 251<br />
44 Acute Renal Failure………………………………………….. 257<br />
45 Acute Peritoneal Dialysis…………………………………….. 266<br />
46 Nephrotic Syndrome………………………………………….. 271<br />
47 Urinary Tract Infection……………………………………….. 279<br />
48 Vesico-ureteric Reflux………………………………………… 285<br />
49 Antenatal Hydronephrosis…………………………………… 288<br />
50<br />
Hematology / Oncology<br />
The Anaemic Child ……………………………………………. 294<br />
51 Haemophilia…………………………………………………….. 298<br />
52 Immune Thrombocytopenic Purpura………………………… 305<br />
53 Thalassaemia…………………………………………………… 311<br />
54 Oncologic Emergencies……………………………………… 317<br />
55 General Guidelines for Acute Lymphoblastic Leukaemia<br />
Maintenance Therapy…………………………………………. 328<br />
Gastroenterology<br />
56 Acute Gastroenteritis…………………………………..………. 332<br />
57 Acute Hepatic Failure………………………………………….. 343<br />
58 Gastrointestinal Bleed…………………………………………. 346<br />
Infections Diseases<br />
59 Sepsis / Septic Shock………………………………………….. 348<br />
60 Paediatric HIV………………………………………………….. 355<br />
61 Malaria…………………………………………………………… 369<br />
62 Tuberculosis……………………………………………………. 374<br />
63 BCG Lymphadenitis…………………………………………… 381<br />
64 Dengue Fever………………………………………………….. 384<br />
65 Congenital Syphilis…………………………………………….. 393<br />
66 Ophthalmia Neonatorum………….……................................ 396
Dermatology<br />
67 Atopic Dermatitis……………………………………………… 399<br />
68 Impetigo……………………………………………………….. 404<br />
69 Scabies…………………………………………………………… 405<br />
70 Steven-Johnson Syndrome…………………………………. 407<br />
71<br />
Metabolic / Genetics<br />
General Approach to Inborn Errors Of Metabolism……….. 410<br />
72 Algorithm For The Sick Infant to Screen for Treatable<br />
IEM………………………………………………………………<br />
73 Approach to Hyperammonemia……………………………….. 419<br />
74 Approach to Hypoglycaemia…………………………………. 423<br />
75 Approach to Metabolic Acidosis…………………………….. 426<br />
76 Down Syndrome……………………………………………….. 430<br />
Surgical <strong>Topic</strong>s<br />
77 Appendicitis……………………………………………………… 438<br />
78 Persistent Vomiting in the Neonate and Child………………. 442<br />
79 Intussusception………………………………………………… 448<br />
80 Inguinal Hernias, Hydroceles………………………………… 452<br />
81 Undescended Testis…………………………………………… 454<br />
82 The Acute Scrotum……………………………………………... 456<br />
83 Penile Conditions ……………………………………………… 459<br />
Rheumatology<br />
84 Juvenile Idiopathic Arthritis……………………………………. 461<br />
Poisons and Toxins<br />
85 Snake Bites……………………………………………………… 468<br />
86 Common Poisons………………………………………………. 476<br />
87 Anaphylactic Reactions………………………………………. 484<br />
Appendix<br />
88 Ward Procedures………………………………………………. 486<br />
Drug Dosages…………………………………………………. 513<br />
Growth Charts…………………………………………………. 565<br />
Pediatric Advanced Life Support Algorithms……………….. 577<br />
416
Dr. Angeline Wan<br />
Consultant Paediatrician<br />
Hospital Muar<br />
Ms. Anne John<br />
Consultant Paediatric Surgeon<br />
Sarawak General Hospital<br />
A/Prof Bina Menon<br />
A/Professor of Paediatrics<br />
Universiti Putra Malaysia<br />
Dr. Chan Lee Gaik<br />
Consultant Paediatric Neonatologist<br />
& Head, Dept. of Pediatrics<br />
Sarawak General Hospital,<br />
Dr. Chew Thean Meng<br />
Consultant Paediatrician<br />
Selayang Hospital<br />
Dr. Chieng Chae Hee<br />
Paediatrician,<br />
Hospital Sibu<br />
Dr. Chin Choy Nyok<br />
Consultant Paediatric Neonatologist<br />
& Head Dept. of Pediatrics<br />
Hospital Kuantan<br />
Dr. Choy Yew Sing<br />
Consultant Paediatric Geneticist<br />
Hospital Kuala Lumpur<br />
Dr. Eni Juraida<br />
Consultant Paediatric Oncologist<br />
Hospital Kuala Lumpur<br />
Dr. Fong Siew Moy<br />
Consultant Paediatric Infectious Disease<br />
Specialist<br />
Hospital Queen Elizabeth<br />
Kota Kinabalu<br />
Dr. Fuziah Md. Zain<br />
Consultant Paediatric Endocrinologist<br />
& Head Dept. of Pediatrics<br />
Hospital Putrajaya<br />
Contributors<br />
Dr. Hishamshah b. Mohd Ibrahim<br />
Consultant Paediatric Oncologist<br />
Hospital Kuala Lumpur<br />
Dr. Hung Liang Choo.<br />
Consultant Paediatric Cardiologist<br />
Hospital Kuala Lumpur<br />
Dr. Hussain Imam B. Hj Muhammad Ismail<br />
Consultant Paediatric Neurologist<br />
& Head Dept of Pediatrics<br />
Hospital Kuala Lumpur<br />
Dr. Irene Cheah<br />
Consultant Paediatrician<br />
Hospital Kuala Lumpur<br />
Datuk Dr. Jimmy Lee Kok Foo<br />
Consultant Paediatrician<br />
& Head Dept of Pediatrics<br />
Hospital Kuala Terengganu<br />
Dr. Kamarul Razali<br />
Consultant Paediatric Infectious Disease<br />
Specialist<br />
Hospital Kuala Lumpur<br />
Dr. Khoo Teik Beng<br />
Consultant Paediatric Neurologist<br />
Hospital Kuala Lumpur<br />
Dr. Kok Juan Loong<br />
Consultant Paediatrician<br />
Sarawak General Hospital<br />
Dr. Lee Ming Lee<br />
Consultant Paediatric Nephrologist<br />
Hospital Seremban<br />
Dr. Leow Poy Lee<br />
Consultant Paediatrician<br />
Hospital Malacca<br />
Dr. Liew Siaw Phin<br />
Private Paediatrician<br />
Kuching<br />
Dr. Lim Chooi Bee<br />
Consultant Paediatric Gastroenterologist<br />
Hospital Kuala Lumpur
Dato’ Dr. Lim Nyok Ling<br />
Consultant Paediatric Neonatologist<br />
& Head Dept of Pediatrics<br />
Selayang Hospital<br />
Dr. Lim Poi Giok<br />
Consultant Paediatrician<br />
Hospital Kuala Lumpur<br />
Dr. Lim Yam Ngo<br />
Consultant Paediatric Nephrologist<br />
Hospital Kuala Lumpur<br />
Dr. Lynster Liaw<br />
Consultant Paediatric Nephrologist<br />
Department of Paediatrics<br />
Hospital Pulau Pinang<br />
Dr. Mardziah bt Alias<br />
Consultant Paediatric Dermatologist<br />
Hospital Kuala Lumpur<br />
Dr. Mohd Hanifah bin Mohd Jamil<br />
Consultant Neonatologist<br />
& Head Dept. of Pediatrics<br />
Hospital Kota Baru<br />
Dr Neoh Siew Hong<br />
Consultant Neonatologist<br />
Hospital Taiping<br />
Dr. Ng Hoong Phak<br />
Consultant Paediatrician,<br />
Sarawak General Hospital<br />
Dr. Ngu Lock Hock<br />
Consultant Paediatrician,<br />
Hospital Kuala Lumpur<br />
Dr. Nik Khairulddin<br />
Consultant Paediatric Infectious Disease<br />
Specialist<br />
Hospital Kota Baru<br />
Dr. Norzila Bt. Mohd Zainudin<br />
Paediatric <strong>Respiratory</strong> Disease Specialist<br />
Hospital Kuala Lumpur<br />
Dr. Ong Gek Bee<br />
Consultant Paediatric Oncologist,<br />
Hospital Melaka<br />
Prof. Dr. Ong Lai Choo.<br />
Consultant Paediatric Neurologist<br />
Hospital University Kebangsaan Malaysia<br />
Dr. Revathy Nallusamy<br />
Consultant Paediatric Infectious Disease<br />
Specialist & Head Dept of Pediatrics<br />
Hospital Pulau Pinang<br />
Dr. Rosalie Yip CW,<br />
Lecturer in Paediatrics,<br />
Universiti Putra Malaysia<br />
Dr. Shirley Wong Siew Ling<br />
Private Paediatrician,<br />
Kuching<br />
Dr. Shyam Puthucheary<br />
Community Paediatrician<br />
Hospital Ipoh<br />
Dr. Susan Pee<br />
Consultant Paediatric Nephrologist<br />
Hospital Sultanah Aminah, Johor Bharu<br />
Dr. Tan Kah Kee<br />
Consultant Paediatric Infectious Disease<br />
Specialist & Head Dept of Pediatrics<br />
Hospital Seremban<br />
Prof. Dr. Tang Swee Fong<br />
Consultant Paediatric Intensivist<br />
Hospital University Kebangsaan Malaysia<br />
Dr. Tang Swee Ping<br />
Consultant Paediatric Rheumatologist<br />
Hospital Selayang<br />
Dr. Teh Keng Hwang<br />
Consultant Paediatric Intensivist<br />
& Head Dept of Pediatrics<br />
Hospital Alor Setar<br />
Dr. Wan Jazilah Wan Ismail<br />
Consultant Paediatric Nephrologist<br />
Hospital Selayang<br />
Dr. Wilson Pau<br />
Paediatric Clinical Specialist<br />
Sarawak General Hospital<br />
Dr. Zuraidah Bt Abdul Latif<br />
Consultant Neonatologist<br />
Hospital Kuala Lumpur
Paediatric Protocols<br />
For Malaysian Hospitals<br />
1st Edition 2005<br />
Hussain Imam Hj Muhammad Ismail<br />
Ng Hoong Phak<br />
MINISTRY OF HEALTH MALAYSIA
ISSN 1823-3856<br />
Printed by:<br />
Perniagaan MMD<br />
No. 3A, Jalan Kenangan Utama,<br />
Taman Kenangan, Batu 6, Gombak,<br />
53100 Gombak, Selangor,<br />
Darul Ehsan.<br />
Tel: 03-6188 4419 Fax : 03-6188 4419<br />
Contect persons: 019-2766123
Foreword<br />
By Director General of Health, Malaysia<br />
MALAYSIA is a young country with a relatively young population. One third of<br />
Malaysians are under 15 years of age. While many children live in urban areas<br />
with ready access to specialist care, many still live in rural areas, where services<br />
are largely provided by medical officers. It is essential that these children receive<br />
timely and appropriate treatment when they present at government clinics and<br />
hospitals.<br />
Over the years the Ministry has taken many steps to ensure that doctors serving<br />
in the rural areas are prepared for their placement and have regular continuous<br />
professional development. Nonetheless, there are still some doctors who are<br />
posted to the rural area before completing their pediatric rotation. As specialist<br />
supervision is not always present, these doctors need ready access to treatment<br />
protocols covering pediatric conditions, especially emergencies, commonly<br />
encountered locally. Such protocols may have to be relatively didactic for use by<br />
those on the ground.<br />
Such a set of pediatric protocols has been available for some time for the state of<br />
Sarawak. Now pediatricians from all parts of the country have contributed to a<br />
more comprehensive manual, addressing topics covering the whole range of<br />
pediatrics.<br />
I hope that this manual will be widely circulated and utilized with the aim of<br />
improving the care of children through out the country.<br />
Thank you.<br />
Yours sincerely,
Foreword<br />
One of the maxims of science is that what is right today is wrong tomorrow. This seems<br />
to apply to clinical medicine more than many other areas of science. Hence one of the<br />
concerns of preparing a manual of clinical protocols is that some parts of the publication<br />
may well be outdated by the time the document finally sees the light of day. Nonetheless<br />
many institutions have found having a set of clinical protocols useful especially where<br />
the turnover of doctors is frequent. In Malaysia this was pioneered in Sarawak in the<br />
days when one pediatrician served the whole state, in an attempt to standardize practice<br />
in different hospitals. Pediatric service has come a long way since then. However now<br />
more than ever before is there a need to establish practice parameters based on current<br />
best practice and evidenced based medicine. Many young doctors are often<br />
overwhelmed by the myriad of options available when they search the internet and it is<br />
not always easy separating the wheat from the chaff.<br />
At a meeting of senior pediatricians in the MOH in February 2004, it was decided that we<br />
should all work together to produce a manual of pediatric protocols addressing clinical<br />
problems commonly encounter in local practice. The topics to be covered were proposed<br />
by those present and topics were allocated to various individuals to work on. We must<br />
say that everybody involved in the task has given their best. Many a time we have gone<br />
back to the authors of various section requesting modifications and the response has<br />
always been positive.<br />
After almost 11 months the final document was ready for printing. This has truly been a<br />
team effort involving colleagues from all over the country and we are very grateful to all<br />
the contributors who have made this manual a reality.<br />
This manual cannot cover all the problems we meet in our wards but we sincerely hope<br />
that we have covered the important ones. We hope, God willing, to revise this manual<br />
every 4 years and we welcome feedback and suggestions from all who happen to use<br />
this edition.<br />
We would like to thank Dr. Tan Poh Tin who started the first edition of the Paediatric<br />
Protocols for Sarawak Hospital; the third edition of which this manual was based. In<br />
addition to our local colleagues we would like to say a special word of thanks to Prof.<br />
Frank Shann of Melbourne for allowing us to incorporate part of his well established drug<br />
dosage booklet into our manual.<br />
This book is dedicated to the children of Malaysia and we pray it makes a difference to<br />
them.<br />
Hussain Imam Hj Muhammad Ismail<br />
Ng Hoong Phak
A. Vital Signs<br />
Normal <strong>Respiratory</strong> Rate<br />
Infant 30 - 40<br />
Toddler 24 - 40<br />
School Age 18 - 30<br />
Adolescent 12 - 16<br />
Normal Heart Rate (from Gillette<br />
1989) 2<br />
NORMAL VALUES IN PAEDIATRICS<br />
Awake<br />
Mean Sleeping<br />
< 3 months 85 - 205 140 80 - 160<br />
3 mo to 2 yr. 100 - 190 130 75 - 160<br />
2 yr. to 10 yr. 60 - 140 80 60 - 90<br />
> 10 yr. 60 - 100 75 50 - 90<br />
Any age HR > 220 consider SVT.<br />
Extra Tables for Abnormal Vital Signs:<br />
Normal Blood Pressure (from Hazinski MF 1992) 1<br />
Systolic Diastolic<br />
Day 1 (< 1000g)39 - 59 16 - 36<br />
Day 1 (> 3000g)50 - 70 25 - 45<br />
Neonate 60 - 90 20 - 60<br />
Infant 87 - 105 53 - 66<br />
Toddler 95 - 105 53 - 66<br />
> 7 years 97 - 122 57 - 71<br />
> 15 years 112 - 128 66 - 80<br />
Hypotension: Simple and rapid estimation to see if Hypotension is<br />
present:<br />
Age BP (Lower limit (5th centile) systolic value)<br />
0 - 1 month > 60<br />
1 mo - 1 yr. > 70<br />
Older > 70 + (2 x age in years)<br />
Blood Pressure in Hypertension<br />
Significant Hypertension Severe Hypertension<br />
1 week Systolic 96 Systolic 106<br />
7d - 1 mo Systolic 104 Systolic 110<br />
Infant Systolic 112 Systolic 118<br />
Diastolic 74 Diastolic 82<br />
3 - 5 years Systolic 116 Systolic 124<br />
Diastolic 76 Diastolic 86<br />
6 - 9 years Systolic 122 Systolic 130<br />
Diastolic 78 Diastolic 86<br />
10 - 12 years Systolic 126 Systolic 134<br />
Diastolic 82 Diastolic 90<br />
13 - 15 years Systolic 136 Systolic 144<br />
Diastolic 86 Diastolic 92<br />
16 - 18 years Systolic 142 Systolic 150<br />
Diastolic 92 Diastolic 98
B. Anthropometric Measurements<br />
a) Head Circumference<br />
Gestational Age Weekly increase cm/wk (1 - 8 wk)<br />
30 - 33 wk. 1.1<br />
34 - 37 wk. 0.8<br />
Rate of growth approximates that of term infant when chronological age reaches term.<br />
Term Increase in OFC<br />
< 3 mo. 2 cm per mo. First yr. 12 cm<br />
4 - 6 mo. 1 cm per mo. Second yr. 2 cm<br />
6 - 12 mo. 0.5 cm per mo.<br />
1 - 2 yr. 2 cm per yr.<br />
2 - 7 yr. 0.5 cm per yr.<br />
7 - 12 yr. 1/3 cm per yr.<br />
Age in months 1st 3 months 2nd 3 months Next 6 months<br />
Head growth (cm) 6 3 3<br />
Rate of CSF production : 0.35 ml/min = 500 ml/day<br />
b) Weight<br />
First 7 - 10 days lose 10 - 15% body weight.<br />
Regain birth weight by 7 - 10th day.<br />
First 3 month weight gain 25 gm/day.<br />
Double Birth Weight by 5 month.<br />
Triple Birth Weight by 1 year of age.<br />
As a rough guide: Year 0 1 5 10<br />
Wt in kg 3.5 10.0 20.0 30.0<br />
To calculate: 1 - 9 yr. Wt (kg) = (Age in yr. + 4) x 2<br />
7 - 12 yr. Wt (kg) = Age in yr. x 3<br />
b) Length and Height<br />
Length at birth 50 cm<br />
6 month 68 cm<br />
1 year 75 cm<br />
2 yr. 85 cm<br />
3 yr. 95 cm<br />
4 yr. 100 cm<br />
5-12 yr. 5 cm/yr.
C. Haematology<br />
a) Routine Haematological Values<br />
Age Hb (g/dL) PCV (%) Retics MCV (fL) MCH (pg/cell). TWBC Neu Lymp<br />
Lowest Lowest (x1000) (Mean) (Mean)<br />
Cord<br />
Blood<br />
13.7–20.1 45-65 5.0 110 9-30 61 31<br />
2 wk 13.0–20.0 42-66 29 5-21 40 63<br />
3 mo 9.5–14.5 31-41 27 6-18 30 48<br />
6 mo – 10.5–14.0 33-42 70-74 25-31 6-15 45 48<br />
6 yr<br />
1.0<br />
7-12 yr 11.0–16.0 34-40<br />
76-80 26-32 4.5-13.5 55 38<br />
Adult 14.0–18.0 42-52 27-32<br />
Male<br />
1.6 80<br />
5-10 55 35<br />
Adult<br />
Female<br />
12.0–16.0 37-47<br />
26-34<br />
Eosinophils: 2-3%<br />
Monocytes: 6-9 %<br />
Platelets are mildly decreased in 1st few months, by 6 months have reached 250 - 300 x 10 9 .<br />
ESR should be < 16 in childhood provided PCV at least 35%.<br />
b) Differential WBC<br />
< 7 days - neutrophils > lymphocytes<br />
1 w - 4 yr. - lymphocytes > neutrophils<br />
4 - 7 yr. - neutrophils = lymphocytes<br />
> 7 yr. - neutrophils > lymphocytes<br />
Hb electrophoresis – look under Thalassaemia protocol.<br />
D. Others<br />
Body Surface Area (BSA) (m 2 ) = Ht (cm) x Wt (Kg)<br />
3600<br />
Other normal values are found in the relevant chapters of the protocol.<br />
1 Nelson Textbook of Pediatric 15 th Edition<br />
2 Pediatric Advanced Life Support Textbook 1994.
Immunisation<br />
1. Immunisation schedule for Malaysia<br />
Immunisation<br />
Table 1: The current Immunisation Schedule<br />
Age (months)<br />
Age (Years)<br />
0 1 2 3 5 6 12 18 6 12 15<br />
BCG* 1 if no scar<br />
Hep B 1 2 3<br />
DPT 1 2 3 4 DT T<br />
OPV* 1 2 3 4 5<br />
Hib 1 2 3<br />
Measles* Sabah<br />
MMR* 1 2<br />
1.1 Vaccine/s available in KKM but not listed in the above schedule<br />
1.1.1 Pneumococcal vaccine : Pneumococcal polysaccharide vaccine -<br />
Protective efficacy ranges from 56 - 81%. Not recommended for children <<br />
2 years old as vaccine is not effective in this group (conjugate vaccine is<br />
immunogenic in these infants but currently not widely available). Single<br />
dose. Booster 3 - 5 years only for high risk persons.<br />
Category A (specialist prescription)<br />
1.1.2 Meningococcal A , C, Y & W-135 (Does not cover B).<br />
Polysaccharide vaccine : Immunogenic in children 2 years or older.<br />
Single dose. Immunity up to 3 years.<br />
Category C (medical officers)<br />
1.1.3 Cholera : Killed whole cell vaccine : 2 doses 4 weeks apart (minimum 1<br />
week). Booster every 6 months. Not highly effective & short duration of<br />
protection < 6 months.<br />
First dose given SC/IM; second dose and boosters given ID to reduce<br />
systemic side effects. Protects only 50% of vaccines (for 3 – 6 months).<br />
Vaccine is not recommended for infants < 6 months of age.<br />
Category B (MO)<br />
1.1.4 Japanese B encephalitis vaccine. 3 doses. Dose 1 and 2 at 2 – 4 weeks<br />
interval then Dose 3 at 1 year after that. This vaccine is given in Sarawak<br />
as part of the MOH vaccination program at 9, 10 and 18 months of age. A<br />
booster is then given at 4 year of age.<br />
1.1.5 Rabies: IM/SC (available in KKM as HDC~ human diploid cell vaccine)<br />
Pre-exposure immunisation: 3 doses at Day 0, 7 and 28. Then<br />
boosters every 2-3 years.<br />
Post-exposure treatment:<br />
o Fully immunised: 2 doses at Day 0 and Day 3 or 7. Rabies<br />
specific Ig unnecessary.<br />
o Unimmunised: 6 doses at Day 0, 3, 7, 14 and 30. Rabies<br />
specific Ig (20 IU/kg given half around the wound and the rest<br />
IM).<br />
Category B
1.1.6 Typhoid: a) Vi polysaccharide vaccine : Single dose. Seroconversion in ><br />
90% of vaccines and confers 60 – 80% protection commencing within 14<br />
days from vaccination. Boosters every 3 years. Immunogenicity < 2 years<br />
of age has not been established.<br />
b)Oral typhoid vaccine(Ty21a vaccine)* (three doses two days apart) and<br />
whole cell typhoid vaccines are also available.<br />
Category B<br />
1.2 Other Vaccines available in Malaysia but not yet in KKM’s program:<br />
1.2.1 Varicella zoster * 70 – 90 % effectiveness.<br />
From 12 months to 12 years: single dose.<br />
> 12 years old : 2 doses at least 28 days apart.<br />
Two vaccines are currently available in Malaysia:<br />
-Varivax (MSD)<br />
-Varilrix (GSK)<br />
Children who have not had chicken pox by 12 years of age are<br />
encouraged to receive the vaccine as the illness is more severe in<br />
older age groups.<br />
Considered for children with asymptomatic or mildly symptomatic<br />
HIV infection; two doses with a 3 month interval are recommended.<br />
Children with leukaemia & are in remission for at least 1 year, &<br />
have > 700/ml circulating lymphocytes may receive vaccination<br />
under supervision of the attending paediatrician<br />
1.2.2 Hepatitis A : 3 doses. Dose 1 and 2 at 2 - 4 weeks apart then Dose 3 at 6<br />
– 12 months later. Adults need 2 doses 6 – 12 months apart.<br />
Seroconversion rate almost 100%. Booster every 10 years. Approved for<br />
children > 1-2 years of age<br />
Missed second dose: If a child misses the second dose at 2 – 4 weeks<br />
then:<br />
If > 1 month and < 5 months from 1st dose just give the second<br />
dose.<br />
If > 5 months have elapsed from 1st dose repeat whole course.<br />
1.2.3 Influenza: Indications and recommended vaccine will vary between<br />
countries. Unprimed individuals will require a second dose 4 to 6 weeks<br />
after the first dose. Yearly revaccination with the latest recommended<br />
vaccine composition by WHO is required in countries at risk, e.g.<br />
temperate climate<br />
Recommendations:<br />
chronic decompensated disorders of respiratory or cardiovascular<br />
systems : e.g. cyanotic heart diseases, chronic lung diseases<br />
HIV infection. In advanced disease, vaccination may not induce<br />
protective antibody levels.<br />
* Live-vaccines – usually only one dose is required to produce long term immunity (except<br />
Yellow Fever for travel purposes (vaccination may be obtained at IMR & respective state health<br />
departments. An International Certificate of Vaccination will be issued, valid for 10 years<br />
commencing from 10 days after vaccination) and oral poliovirus vaccine which contains 3<br />
different components and more doses are required to ensure an adequate response to each<br />
component).
2 General Notes<br />
2.1 Many vaccines (inactivated or life) can be given together simultaneously (does not impair<br />
antibody response or increase adverse effect). But they are to be given at different sites unless<br />
given in combined preparations. Many vaccines are now packaged in combinations so that the<br />
child is not subjected to multiple injections.<br />
2.2 Site of administration<br />
2.2.1 Oral – OPV<br />
2.2.2 Deep SC & IM injections. (ALL vaccines EXCEPT BCG and OPV)<br />
a) anterolateral aspect of thigh – preferred site in children.<br />
b) upper arm – preferred site in adults<br />
c) upper outer quadrant of buttock - is associated with reduced antibody level production.<br />
2.2.3 Intradermal (ID) - BCG & rabies. Left deltoid area (proximal to insertion deltoid muscle)<br />
2.3 A person who has been immunised using OPV can subsequently use IPV for booster and vice<br />
versa.<br />
2.4 Repeat dose of OPV if child vomits soon after administration.<br />
2.5 PRP-T (Act Hib) and PRP-OMP (Pedvax) (H. influenzae b vaccines) used in the primary series<br />
are interchangeable. Children partially immunized in the private sector with one particular type<br />
may be immunized with another type in the KKM schedule.<br />
2.6 MMR can be given irrespective of previous history of measles, mumps or rubella infection.<br />
3 Immunisation : Contraindications<br />
3.1 Postponed during acute febrile illness. Minor infection without fever or<br />
systemic upset are NOT contraindication. Polio (OPV) postpone if severe<br />
diarrhoea and vomiting (to avoid decrease take).<br />
3.2 A relative contraindication: do not give a vaccine within 2 weeks of an elective<br />
surgery.<br />
3.3 Live vaccine: Absolute contraindication<br />
3.3.1 Immunosuppressed -malignancy; irradiation, leukaemia, lymphoma,<br />
primary immunodeficiency syndromes (but NOT asymptomatic HIV).<br />
3.3.2 On chemotherapy (< 6 months after last dose).<br />
3.3.3 High dose steroid: Prednisolone 2 mg/kg/day for > 7 days or low dose<br />
systemic > 2 wk.; (delay vaccination for 3 months).<br />
If tropical or inhaled steroids OR low dose systemic < 2 weeks or<br />
EOD for > 2 weeks can give live vaccine.<br />
3.3.4 If another LIVE vaccine including BCG had been given < 3 wk. ago.<br />
(Either give live vaccines simultaneously or if cannot then separately<br />
with a 3 week interval).<br />
3.3.5 Within 3 months following IV Immunoglobulin. (except yellow fever or<br />
oral polio).
3.3.6 Pregnancy (live vaccine theoretical risk to foetus) UNLESS there is<br />
significant exposure to serious conditions like polio or yellow fever in<br />
which case the importance of vaccination may outweigh the possible<br />
risk to the foetus.<br />
3.4 Killed vaccines are generally safe.<br />
The only Absolute contraindications are SEVERE local (induration involving ><br />
2/3 of the limbs) or severe generalised reaction in the previous dose (i.e.<br />
Temp > 39°C, anaphylaxis, persistent screaming, convulsions).<br />
3.5 Specific Contraindications<br />
3 Weeks 3 Months<br />
Live Vaccine HNIG Live Vaccine<br />
3.5.1 BCG - Not to be given to symptomatic HIV infected children.<br />
3.5.2 Hep B vaccine – Severe hypersensitivity to aluminium or thiomersal.<br />
(Not needed for HBsAg or Ab positive)<br />
3.5.3 Pertussis<br />
Progressive neurological diseases like infantile spasm, tuberous<br />
sclerosis.<br />
Severe reaction to previous dose i.e.<br />
a. Anaphylaxis b. Collapse or shock-like states<br />
c. Hyporesponsive states d. Fits and fever within 72 hr<br />
e. Fever > 40.5 C within 48 hours e. Encephalitis within 7 days<br />
f. Severe local reaction involving 2/3 of limbs.<br />
Static neurological diseases, developmental delay, personal or<br />
family history of fits are NOT contraindications.<br />
Severe hypersensitivity to aluminium and thiomersal. And point 3.4<br />
as above<br />
3.5.4 Diphtheria & Tetanus: Severe hypersensitivity to aluminium and<br />
thiomersal. And point 3.4 as above.<br />
3.5.5 Polio<br />
Diarrhoea & vomiting.<br />
Hypersensitivity to penicillin, neomycin, streptomycin or<br />
polymycin.<br />
Within 3 week from a proposed tonsillectomy (remote risk of<br />
vaccine induced bulbar polio).<br />
Polio (IPV) is to be used for immunocompromised children, their<br />
siblings and household contacts. OPV if given to<br />
immunosuppressed or HIV positive children tend to cause<br />
prolonged excretion of the OPV and be hazardous to care givers.
3.5.6 Rubella - Contraindicated in pregnancy (even though no reported cases<br />
of congenital rubella syndrome due to vaccine).<br />
3.5.7 Measles - If < 9 months old presence of maternal Ab may decrease<br />
immunogenecity. Avoid in persons hypersensitive to neomycin,<br />
polymyxin OR anaphylaxis to egg ingestion.<br />
3.5.8 MMR and Influenza – severe reaction to hen’s eggs or neomycin.<br />
3.5.9 Pneumococcal – children less than 2 years old; revaccination within 3<br />
years has high risk of adverse reaction; avoid during chemotherapy or<br />
radiotherapy and less than 10 days prior to commencement of such<br />
therapy – antibody response is poor. Pregnancy.<br />
3.5.10 Hepatitis A: Severe hypersentivity to aluminium hydroxide,<br />
phenoxyethanol or neomycin.<br />
3.5.11 Typhoid (whole-cell) and Cholera: patients with chronic illness such as<br />
multiple sclerosis, rheumatoid arthritis, diabetes and compensated<br />
cardiac conditions may suffer a relapse.<br />
3.5.12 Meningococcus A, C, Y & W-135: polysaccharide vaccine : Not useful<br />
in children < 2 years old.<br />
3.5.13 Japanese B: contraindicated in immunodeficiency and malignancy,<br />
diabetes, acute exacerbation of cardiac, hepatic and renal conditions.<br />
3.6 The following are NOT contraindications to vaccination in<br />
Children<br />
3.6.1 Mild illness without fever e.g. mild diarrhoea, cough, running nose.<br />
3.6.2 Asthma, eczema, hay fever, impetigo, heat rash, etc.(avoid injection in<br />
area of skin lesion).<br />
3.6.3 Treatment with antibiotics or locally acting steroids.<br />
3.6.4 Child's mother is pregnant.<br />
3.6.5 Breast fed child (does not affect polio uptake).<br />
3.6.6 Neonatal jaundice.<br />
3.6.7 Underweight or malnourished.<br />
3.6.8 Over the recommended age.<br />
3.6.9 Past history of pertussis, measles or rubella (unless confirmed<br />
medically).<br />
3.6.10 Non progressive, stable neurological conditions like Cerebral palsy,<br />
Down’s syndrome, simple febrile convulsions, controlled epilepsy.<br />
mental retardation.<br />
3.6.11 Family history of convulsions.<br />
3.6.12 History of heart disease, acquired or congenital.<br />
3.6.13 Prematurity (give immunisation according to schedule irrespective of<br />
gestational age).
4 Vaccination: Possible Side Effects<br />
4.1 Diphtheria and Tetanus vaccine.<br />
Swelling, redness and pain<br />
A small painless nodule may at injection site – harmless.<br />
Transient fever, headaches, malaise, rarely anaphylactic reaction.<br />
Neurological reactions rare.<br />
4.2 DPT<br />
Local swelling and redness within 24 – 72 hours lasting 1 – 2 weeks.<br />
Acute encephalopathy (0 – 10.5 per million)<br />
Shock and ‘unusual shock-like state (3.5 to 250 cases per 100 000)<br />
Anaphylaxis (2 per 100 000 doses)<br />
Protracted crying (0.1 to 6%)<br />
4.3 OPV<br />
Vaccine associated paralytic polio (VAPP)<br />
risk at 1 case/ 5.3 million doses<br />
highest risk after 1 st dose estimated at 1 case / 1 million contacts of first<br />
dose recipients.<br />
risk for subsequent doses is greatly reduced. It is important that contacts<br />
of children receiving OPV are themselves fully immunized.<br />
4.4 IPV<br />
No serious side effects have been documented, apart from local reaction.<br />
Indicated for children with severe immunocompromised conditions e.g.<br />
immunodeficiency states (1 o and 2 o such HIV infection, malignancy & organ<br />
transplantation)<br />
4.5 HiB (Haemophilus influenzae b) vaccine<br />
Local swelling, redness and pain soon after vaccination and last up to 24<br />
hours in 10% of vaccines<br />
Malaise, headaches, fever, irritability, inconsolable crying. Very rarely<br />
seizures.<br />
4.6 Measles:<br />
Transient rash in 5% of cases.<br />
Fever between D5 and D12 post vaccination lasting for 1-3 days (5 to 15%<br />
of doses of vaccines).<br />
URTI symptoms.<br />
Febrile convulsions (D6 to D14) in 1 in 1000 – 9000 doses of vaccine.<br />
(Natural infection 1:200)<br />
Encephalopathy within 30 days in 1 in 1,000,000 doses of vaccines.<br />
(Natural infection 1:1000 - 5000)<br />
SSPE may occur in 1 in 1,000,000 doses. (Incidence in natural infection is<br />
6 to 22 per 1,000,000).<br />
4.7 Mumps<br />
Rarely transient rash, pruritis and purpura.<br />
Parotitis in 1% of vaccines, 3 or more weeks after vaccination.<br />
Orchitis and retro bulbar neuritis very rare.<br />
Meningoencephalitis is mild and rarely occur. (1 in 800,000 doses).<br />
(Natural infection 1 in 400).
4.8 Rubella<br />
May have rash, fever, lymphadenopathy, thrombocytopenia, transient<br />
peripheral neuritis.<br />
Arthritis and arthralgia occurs in up to 3% of children and 20% of adults<br />
who receive the vaccine.<br />
Rarely polyneuropathy (like Guillain-Barre syndrome can occur).<br />
4.9 BCG<br />
Local reaction :a papule at site of vaccination occurs within 2 to 6 weeks.<br />
This grows and flattens with scaling and crusting. Occasionally a<br />
discharging ulcer may occur. This heals leaving a BCG scar of at least 4<br />
mm in successful vaccination.<br />
BCG adenitis may occur.<br />
4.10 Influenza and Rabies<br />
Transient swelling, redness, pain and induration locally.<br />
Myalgia, malaise and fever for 1 – 2 days starting within a few hours post<br />
vaccination. Very rarely neurological or anaphylactic reaction occurs.<br />
4.11 Pneumococcal<br />
Local reaction. Fever and myalgia in less than 1% of vaccines. Rarely<br />
neurological disorder (Guillain-Barre), glomerulonephritis, ITP or<br />
anaphylaxis.<br />
4.12 Hepatitis A<br />
Local reaction. Flu-like symptoms lasting 2 days in 10% of vaccines.<br />
4.13 Hepatitis B<br />
Local reaction. Fever and flu-like symptoms in 1 st 48 hours. Rarely<br />
erythema multiforme or urticaria.<br />
4.14 Typhoid (Typhim Vi):<br />
Local reaction. Myalgia, malaise, nausea, headaches and fever in 3% of<br />
recipients.<br />
4.15 Cholera<br />
Local reaction. Headache, fever and malaise for 1 – 2 days. Rarely<br />
anaphylactic reaction, neurological symptoms including cerebral and<br />
meningeal irritation may occur.<br />
Repeated vaccination over a few years can result in hypersensitivity to the<br />
protein components.<br />
4.16 Meningococcus A, C, Y & W-135<br />
Local reaction. Irritability, fever and rigors for 1 – 2 days. Very rarely<br />
anaphylaxis.
5 Vaccination : Special Circumstances<br />
5.1 What to do if a measles case is admitted to the Paediatric Ward?<br />
5.1.1 Protect all immunocompromised children with immunoglobulin (HNIG)<br />
0.2 mls/kg (32 mg/kg). (Measles is the major cause of mortality in<br />
leukaemia in remission.)<br />
5.1.2 Check the status of the other children with regards with measles<br />
immunisation. If they are not immunised then give the measles<br />
monocomponent vaccine within 24 hours of exposure. Vaccination<br />
within 72 hours can abort clinical measles in 75% of contacts.<br />
5.1.3 Discharge uncomplicated measles case.<br />
5.2 Immunisation in HIV infected children<br />
5.2.1 With or without symptoms should receive :<br />
live vaccines (WHO recommends BCG for asymptomatic cases)<br />
Inactivated vaccines<br />
5.2.2 Give immunoglobulin if exposed to measles or chicken pox.<br />
5.2.3 IPV is to be used.<br />
5.3 In patients with past history or family history of fits, neurological or<br />
developmental abnormalities that would predispose to febrile fits :-<br />
5.3.1 Febrile fits can occur 5 – 10 days after measles (or MMR) vaccination<br />
or within the first 72 hours following pertussis immunisation.<br />
5.3.2 Give Paracetamol (120 mg or ¼ tablet) prophylaxis after immunisation<br />
(esp. DPT) 4 hourly for 48 hours regardless of whether the child is<br />
febrile or not. This can reduce the incidence of high fever, febrile<br />
convulsions, fretfulness, crying, anorexia and local inflammation.<br />
5.3.3 Rectal Diazepam may need to be given on stand by.<br />
5.4 Maternal Chicken Pox during perinatal period. Rash appearing within 5 days<br />
before and 2 days after delivery.<br />
5.4.1 Isolate mother from baby and other patients. Isolate baby.<br />
5.4.2 Immunoglobulin to be given :-<br />
Human immunoglobulin (400u/kg) OR<br />
ZIG (125µ/kg) within 48 hours<br />
5.4.3 Because severe varicella may develop in new-borns despite ZIG, some<br />
investigators recommend Acyclovir prophylaxis. Neonates with VZ<br />
infection should be treated with IV Acyclovir 10 mg/kg every 8 hrs for<br />
10 days.
5.5 Close contacts of immuno-deficient children and adults must be immunized,<br />
particularly against measles and polio (use IPV).<br />
5.6 In cases of contact with a patient with invasive Haemophilus influenzae B<br />
disease:<br />
5.6.1 Close contacts in a household, nursery or kindergarden under the age<br />
of 4 years should be immunised.<br />
5.6.2 Rifampicin prophylaxis should be given to all household contacts at 20<br />
mg/kg once daily (Maximum 600 mg) for 4 days (except pregnant<br />
women - one IM dose of ceftriaxone )<br />
5.6.3 Index case should be immunised irrespective of age.<br />
5.7 Asplenia (Elective or emergency splenectomy; asplenic syndromes; sickle cell<br />
anaemia) – susceptible to encapsulated bacteria and malaria.<br />
5.7.1 Pneumococcal, Meningococcal A, C, Y & W-135 and Haemophilus<br />
influenza b vaccines should be given.<br />
5.7.2 For elective splenectomy (and also chemotherapy or radiotherapy); it is<br />
preferable to give the vaccines 2 or more weeks before the procedure.<br />
However they can be given even after the procedure.<br />
5.7.3 Penicillin prophylaxis should continue even after vaccination. Ideally for<br />
life. If not until 16 years old for children or 5 years post splenectomy in<br />
adults.<br />
5.8 Babies born to mothers who are HbeAg OR HbsAg positive should be given<br />
Hepatitis B immunoglobulin (200 IU) and vaccinated with the Hepatitis B<br />
vaccine at within 12 hours and not later than 48 hours. Given in different<br />
syringes and at different sites.
6. Recommended Immunisation Schedule for Infants and Children Not<br />
Immunised at the Recommended Time<br />
Time of Immunisation<br />
Age at first visit<br />
Between 6 weeks and 9<br />
months<br />
9 months and older<br />
1st visit BCG, DPT-Hib1, OPV1 & BCG, DPT1-Hib, OPV1<br />
HBV1<br />
measles in Sabah at 9<br />
months of age<br />
MMR at 12 months of age<br />
2nd visit (1 month later) DPT-Hib2, OPV2, HBV2 or DPT2, OPV2, HBV1<br />
3rd visit (1 month later) DPT-Hib3, OPV3, HBV2 DPT3, OPV3, HBV2<br />
1 month later HBV3 HBV3<br />
2-8 months later DPT & OPV (booster)<br />
measles in Sabah at 9<br />
months of age<br />
MMR at 12 months of age<br />
DPT & OPV (booster)<br />
Subsequent booster doses: follow "Recommended Immunisation Schedule for Infants &<br />
Children”<br />
For infants aged less than 6 weeks, use "Recommended Immunisation Schedule for Infants &<br />
Children".<br />
Note that measles vaccine should be given only after 9 months.<br />
Omit pertussis vaccine if child is aged 7 years or older at first contact. In this situation , adult<br />
dTap (lowered antigen) may be considered.<br />
For special groups of children with no regular contact with Health Services and with no<br />
immunisation records, BCG, OPV, DPT, HBV and measles can be given simultaneously at<br />
different sites at first contact.<br />
It is not necessary to restart a primary course of immunisation irrespective of the period<br />
that has elapsed since the last dose was given. Only the subsequent course that has<br />
been missed need be given. (Example. An infant who has been given OPV1 and then 9<br />
months later comes for follow-up, the OPV1 need not be repeated. Go on to OPV2.). Except<br />
Hepatitis A.<br />
Reference:<br />
1. Ministry Of Health Malaysia<br />
2. Immunization Precautions and Contraindications (2 nd Edition) – George C. Kassianos. Blackwell<br />
Scientific Publications. 1994.<br />
3. Health Technology Assessment Expert Committee report on immunisation (MOH Malaysia).<br />
4. Malaysian Immunisation Manual. College of Paediatrics, Academy of Medicine of Malaysia.<br />
2001<br />
5. Canadian Immunization Guide.(6 th Edition). 2002.<br />
6. Cholera vaccines. WHO position paper ; Weekly Epidemiol Rec 2001;76:117-124<br />
7. Typhoid vaccines. WHO position paper ; Weekly Epidemiol Rec. 2000;32:257-64.
Developmental Assessment<br />
Development is the progressive, orderly, acquisition of skills and abilities as a child grows.<br />
It is influenced by genetic, neurological, physical, environmental and emotional factors.<br />
Important points to note:-<br />
1. Child must be co-operative, not tired, fretful, hungry nor sick.<br />
2. Full allowance must be made for prematurity up to two years.<br />
3. Take note of parental account of what child can/cannot do. If parent says the child<br />
has a squint, there is a high chance that he has. Similarly, note comments on<br />
abnormal gait, speech defects, etc.<br />
4. Normal development is highly dependent on the integrity of child's hearing and<br />
vision.<br />
5. A normal pattern of speech and language development is essential for a normal<br />
social, intellectual and emotional development.<br />
6. Advanced motor development does not signify mental superiority,<br />
manipulative skills are a more reliable guide, as well as interest in surrounding,<br />
responsiveness, alertness and powers of concentration.<br />
7. Always assess vision, hearing, language and social development in addition to<br />
gross and fine motor skills.<br />
8. Retardation may be global i.e. affecting all areas equally, or otherwise normal<br />
except in specific areas e.g. speech (Always exclude deafness).<br />
9. Always rule out hypothyroidism in all cases of global retardation.<br />
Warning Signs<br />
A. General<br />
1. Head size out of proportion with length or crossing centile lines (too large or too<br />
small).<br />
2. Abnormal rates of growth in weight and height.<br />
3. Congenital anomalies, odd facies, symmetrical defects of hands and feet.<br />
4. Unusual hairs or hairline.<br />
5. Persistence of primitive reflexes after 6 months of age.<br />
6. Fisting or adducted thumb after the second month of age.
B. Gross Motor<br />
5 mo Does not roll over<br />
8 mo Does not sit without support<br />
10 mo Does not stand while holding on<br />
18 mo Not walking unaided<br />
2 yr Not climbing up or down stairs<br />
2 ½ yr Not jumping with both feet<br />
3 yr Unable to stand on one foot<br />
momentarily<br />
4 yr Not hopping<br />
5 yr Unable to walk a straight line<br />
back and forth or balance on one<br />
foot<br />
C. Fine Motor<br />
5 mo Unable to hold rattle<br />
7 mo Unable to hold an object in each<br />
hand<br />
12 mo Absence of pincer grasp<br />
15 mo Unable to put in or take out<br />
2 yr Not scribbling<br />
2 ½ yr Not turning a single page of a<br />
book<br />
3 yr Unable to draw a straight line<br />
4 yr Unable to copy a circle<br />
5 yr Unable to copy a cross<br />
D. Language<br />
6 mo Not babbling<br />
9 mo Not saying “da” or “ba”<br />
11 mo Not saying “dada” or “baba”<br />
18 mo Has < 3 words with meaning<br />
2 yr No two-word phrases<br />
2 ½ yr Speech unintelligible to parents<br />
3 yr Speech unintelligible to<br />
strangers.<br />
Gestures used instead of speech.<br />
4 yr No ‘Why?’ or ‘What?’ questions.<br />
Can’t tell a simple story.<br />
Poor social play.<br />
Poor word / sentence structures.<br />
5 yr Still gets words, sentences or<br />
ideas jumbled up.<br />
Articulation problems<br />
E. Psychosocial<br />
3 mo No social smile<br />
6-8 mo Not laughing in playful situation<br />
1 yr Hard to console, stiffens when<br />
approached<br />
18 mo Not pointing to indicate wants<br />
2 yr Kicks, bites, and screams easily<br />
and without provocation<br />
Rocks back and forth.<br />
No eye contact.<br />
3-5 yr In constant motion.<br />
Resists discipline.<br />
Does not play with other kids.<br />
F. Cognitive<br />
3 mo Not alert to mother<br />
9 mo No interest in peek-a-boo<br />
12 mo Does not search for hidden object<br />
18 mo No interest in cause-and-effect<br />
games<br />
2 yr Does not know categories<br />
3 yr Does not know own full name<br />
4 yr Cannot pick shorter or longer of<br />
two lines<br />
4 ½ yr Cannot count sequentially<br />
5 yr Does not know colours or any<br />
letters
Hearing Assessment<br />
Warning signs for hearing<br />
Child appears not to hear or<br />
does not attempt to listen.<br />
Child by 12 months of age<br />
does not respond to his name<br />
or understand "No" or make<br />
response to clue words like<br />
"Shoe"<br />
Also those with warning signs<br />
for speech / language delay<br />
Normal Hearing<br />
Auditory Tests<br />
At Risk Groups<br />
Prematurity.<br />
Intrauterine Infection (TORCHES)<br />
Severe Neonatal jaundice<br />
Use of ototoxic drugs e.g. gentamicin.<br />
Meningitis, HIE<br />
Trauma.<br />
Chronic Secretory Otitis Media<br />
Family history of deafness (exclude Otitis media) -<br />
at least 10 different genes are responsible for<br />
deafness.<br />
Abnormal looking babies, abnormal external ears.<br />
Newborn Sudden loud noise induces blinking, startle or cry.<br />
Stilling to voice, change in breathing pattern<br />
4 months Consistent head turning towards sound.<br />
5-6 months Turns head to sound at level of ears.<br />
7 months Turns to sound source below ear level<br />
8 months Turns to sound source above ear level.<br />
12 months Looks up to sound above head<br />
7 - 9 months Distraction Tests. Baby held sitting facing forwards on mother's lap. A<br />
toy is held in front by one team member to give visual distraction. Second<br />
team member makes soft sounds 2-3 feet from either ear. The first team<br />
member decides on the child’s response.<br />
21mths - Voice Triggered Conditioning Test. Child conditioned to do a task<br />
2 yr. when a sound is heard i.e. put a brick in the container. Voice sounds<br />
or an audiometer are used.<br />
> 18 mths Toy Tests. Child identifies toys when their names are spoken quietly.<br />
4 yr. Pure tone audiometry. (Requires cooperation).<br />
All ages Brainstem Auditory Evoked Response (BAER).
Visual Assessment<br />
Warning signs for Poor Vision<br />
Does not fix on face of mother while<br />
feeding by 6 weeks.<br />
If the child's eyes wander from one corner<br />
of the eye to the other after 6 weeks.<br />
If leukocoria (white eye reflex) is noted at<br />
any age.<br />
Child holds objects very close to eye.<br />
Squint in one of his eyes after 6 months of age.<br />
Strong objection to covering one eye (good eye), but not the other (bad eye).<br />
Blind mannerisms, abnormal head postures.<br />
Development of Vision<br />
When assessing vision in a young baby it is important to know the normal visual<br />
attainment that can be expected at each age.<br />
At birth Turn head towards source of light, follow face of mother if very<br />
close, optokinetic nystagmus.<br />
At 4 weeks Should follow light, dangling object < 90 o , visual acuity 6/60 at this<br />
stage.<br />
8 weeks Fixation, convergence, focusing.<br />
12 weeks Hand regard. Dangling object 180 o . Visual acuity 6/18 - 6/12.<br />
16 weeks Reach for any object in its view.<br />
20 weeks Smile at mirror image.<br />
8 months See Smartie or raisins, look for fallen toy.<br />
10 months 100s and 1000s.<br />
> 18 months Picture charts.<br />
21mths/2 yr. Sheriden letters.<br />
41mths/2-5yrs Snellen chart<br />
At risk<br />
Prematurity.<br />
Small for Gestation.<br />
Family history of cataract, retinoblastoma,<br />
squint.<br />
NB. If vision improves when child reads through pinhole, refer to optician for<br />
spectacles.<br />
Corneal reflection test for squint<br />
Refer funny looking eyes, abnormal eye movements/head posture.
Global Developmental Delay<br />
History<br />
Consanguinity<br />
Pregnancy: Drugs, Alcohol or Illnesses.<br />
Delivery: Premature or Birth Asphyxia<br />
Neonatal: Severe NNJ or Hypoglycaemia<br />
Family History<br />
Do<br />
Refer for eye and hearing test.<br />
T4 / TSH<br />
Chromosomal Analysis<br />
MRI brain<br />
(if not available, CT scan)<br />
KIV<br />
o Other genetic studies if available (Methylation PCR for PWS / Angelman,<br />
Subtelomeric rearrangements, Fragile X screen, MECP2) or get a genetic<br />
consultation.<br />
o Metabolic screen (VBG, serum lactate, ammonia, serum amino acids, urine<br />
organic acids screen)<br />
o Serum CPK in boys<br />
o EEG if history suggestive of possible seizures<br />
Isolated Speech Delay<br />
History<br />
Congenital Rubella<br />
Perinatal Drugs<br />
Severe Neonatal Jaundice<br />
Family History<br />
Ear Infection<br />
Ask for Quality and Quantity of speech<br />
Consider<br />
1. Hypothyroidism<br />
2. Chromosomal anomaly e.g. Down or<br />
Fragile X<br />
3. Structural Brain Disorder<br />
4. Cerebral Palsy<br />
5. Congenital Infection<br />
6. Specific Syndromes including tuberous<br />
sclerosis or neurofibromatosis.<br />
7. Inborn error of metabolism<br />
8. Postnatal causes like head injury,<br />
intracranial bleed, CNS infections.<br />
9. Muscular Dystrophies<br />
10. Autism<br />
Consider<br />
1. Hearing Impairment<br />
2. Familial or Genetic causes<br />
3. Social Cultural Deprivation<br />
4. IQ Low (Mental Retardation)<br />
5. Language Confusion<br />
6. Autism<br />
7. Hypothyroidism<br />
Do<br />
Check ears and tonsils<br />
Distraction Test<br />
T4 / TSH<br />
Referral to ENT / Audiologist for formal hearing test<br />
Referral to Speech therapist<br />
KIV<br />
o Chromosomal Analysis and other genetic testing.<br />
o Metabolic screen<br />
o EEG if there is language regression (Landau Kleffner syndrome)
Delayed Motor Development<br />
Consider<br />
1. Normal or Familial variation<br />
2. Previous Chronic Illness<br />
3. Cerebral Palsy<br />
4. Neuromuscular Diseases e.g.<br />
Duchenne Muscular Dystrophy<br />
5. Orthopaedic Problems<br />
6. Emotional Neglect<br />
Learning Difficulties In School<br />
Consider<br />
1. Previous developmental delay<br />
2. Medical Problems<br />
Hypothyroidism<br />
Iron deficiency anaemia<br />
Chronic lead poisoning<br />
Epilepsy (eg Absence Seizures)<br />
3. Specific Learning Difficulty (Dyslexia)<br />
References:-<br />
1. RS. Illingworth. The Development of the Infant and Young Child.<br />
2. Nelson’s Textbook of Pediatrics.<br />
3. First LR, Palfrey JS. The infant or young child with developmental delay. NEJM 1994;330:478-483<br />
4. Shevell M et al. Practice parameter: Evaluation of the child with global developmental delay.<br />
Neurology 2003;60:367-380
Developmental Milestones Table<br />
AGE Gross Motor Vision & Fine Motor Speech & Language Personal Social<br />
6 weeks Pull to sit: Head lag and rounded back. Fixates and follows to 90 Vocalising by 8/52 Smiles responsively.<br />
Ventral Suspension: Head momentarily in<br />
Quiets to sound. Startles<br />
same plane as body.<br />
Prone: Pelvis high but knees no longer<br />
under abdomen. Chin raised occasionally.<br />
to sound.<br />
3 months Pull to sit: Only slight head lag. Head Hand regard.<br />
Squeals with delight. Laughs.<br />
occasionally bobs forward.<br />
Follows object from side to Turns head to sound.<br />
Ventral Suspension: Head above plane of side (180°)<br />
body.<br />
Hands held loosely.<br />
Prone: Pelvis flat. Lifts head up 45° - 90°. Grasp object placed in<br />
hand. Not reaching out.<br />
5 months Pull to sit: NO head lag and sits with Reaches for objects.<br />
Mouthing.<br />
straight back.<br />
Lying supine : Feet to mouth.<br />
Plays with toes.<br />
6 months Pulls to sit: Lifts head off couch in<br />
Palmar grasp of cube with<br />
anticipation.<br />
ulnar approach.<br />
Sits with support.<br />
Moves head and eyes in all<br />
Bears full weight on legs.<br />
directions.<br />
Prone: Supports weight on hands with<br />
chest and upper abdomen off couch.<br />
Rolls prone to supine.<br />
No squint (after 4 months).<br />
7 months Sits with hands on couch for support.<br />
Rolls from supine to prone.<br />
Feeds self with biscuits.<br />
Transfers objects form hand<br />
to hand.<br />
Rakes at pea.<br />
Babbling in single<br />
syllables.<br />
Babbling in combined<br />
syllables at 8 months.<br />
Distraction Test.<br />
Stranger anxiety.
AGE Gross Motor Vision & Fine Motor Speech & Language Personal Social<br />
9 months Sits steadily. Leans forward but cannot<br />
pivot.<br />
Stands holding on.<br />
Pulls self to stand.<br />
10 months Crawls on abdomen.<br />
Pull self to sit.<br />
11 months Creeping on all FOURS<br />
Pivoting.<br />
Cruising.<br />
Walks with 2 hands held.<br />
1 year Gets from lying to sitting to crawling to<br />
standing.<br />
Walks like a bear.<br />
Walks with ONE hand held.<br />
Walks well (13 months).<br />
Stands alone.<br />
15 months Creeps upstairs.<br />
Stoops for toy and stands up without<br />
support. (best at 18 months)<br />
18 months Gets up and down stairs holding on to<br />
rail or with one hand held.<br />
Pulls toy or carries doll.<br />
Throws ball without falling.<br />
Sits on a chair.<br />
Inferior pincer grasp.<br />
(Scissors grasp).<br />
Index approach. Uses index<br />
finger to poke at pea.<br />
Able to let go of cube in<br />
hand.<br />
Neat pincer grasp.<br />
Bangs 2 cubes.<br />
Sees and picks up<br />
hundreds and thousands.<br />
Tower of 2 cubes.<br />
Scribbles spontaneously<br />
(15-18 months)<br />
Tower of 3 cubes.<br />
Scribbles spontaneously.<br />
Visual test: Picture charts.<br />
Handedness (18 - 14<br />
months).<br />
Localises sound at 3 feet,<br />
above and below the ear<br />
level.<br />
Feeds with spoon<br />
occasionally.<br />
Looks for fallen toys.<br />
Understands “NO!”<br />
Waves “Bye bye”<br />
Plays “Pat-a-Cake”<br />
ONE word with meaning. Plays “peek-a-boo”<br />
Understands phases.<br />
(e.g. where is your<br />
shoes).<br />
2 - 3 words with<br />
meaning.<br />
Localising sound above<br />
head.<br />
More words.<br />
Points to objects he<br />
wants.<br />
Continual jabber and<br />
jargon.<br />
Points to 2 - 3 body parts.<br />
Picture Cards - identify<br />
one.<br />
Casting (13 months)<br />
Less mouthing.<br />
Shy.<br />
Takes off shoe.<br />
Feeds self with cup (able<br />
to pick up and put down)<br />
and spoon (but spills).<br />
Mouthing stops.<br />
Imitates housework.<br />
Toilet trained.<br />
Uses spoon well.<br />
Casting stops.
AGE Gross Motor Vision & Fine Motor Speech & Language Personal Social<br />
2 years Goes up and down stairs alone, 2 feet per<br />
step.<br />
Walks backwards (21 months)<br />
Runs.<br />
Picks up toy without falling.<br />
Able to throw and kick ball without falling.<br />
2 1/2<br />
years<br />
Jumps on both feet.<br />
Walks on tip toes.<br />
3 years Goes up stairs one foot per step.<br />
Down stairs 2 feet per step.<br />
Jumps off bottom step.<br />
Stands on 1 foot for seconds.<br />
Rides tricycle.<br />
3 1/2<br />
years<br />
4 years Goes up and down stairs one foot per step.<br />
Skips on one foot.<br />
Hops on one foot.<br />
4 1/2<br />
years<br />
Tower of 6 cubes<br />
Imitates cube of train with<br />
no chimney.<br />
Imitates straight line.<br />
Visual test: Snellen chart.<br />
Tower of 8.<br />
Imitates train with<br />
chimney.<br />
Holds pencil well.<br />
Imitates and .<br />
Tower of 9.<br />
Imitates bridge.<br />
with cubes:<br />
Copies <br />
Imitates<br />
Draw a man test. (3 - 10y)<br />
Copies bridge.<br />
Imitates gate with cubes.<br />
Copies<br />
Goodenough test 4.<br />
Copies gate with cubes.<br />
Copies square.<br />
Draws recognisable man<br />
and house.<br />
Joins 2 - 3 word in a<br />
sentence.<br />
Uses ‘you’ ‘me’ ‘I’.<br />
Picture cards - Names 3<br />
objects.- Points to 5.<br />
Obeys 4 simple<br />
commands.<br />
Points to 4 body parts.<br />
Knows FULL name and<br />
sex.<br />
Names one colour.<br />
Can count to 10<br />
Names 2 colours.<br />
Nursery rhymes.<br />
Understands “on”, “in”,<br />
“under”.<br />
Names 3 colours.<br />
Fluent conversation.<br />
Understands “in front of”,<br />
“between”, behind”.<br />
Puts on shoes, socks,<br />
pants.<br />
Dry by day.<br />
Play near other children<br />
but not with them.<br />
Unbuttons.<br />
Dresses and undresses<br />
fully if helped with buttons<br />
and advised about correct<br />
shoe.<br />
Dry by night.<br />
Plays with others.<br />
Buttons clothes fully.<br />
Attends to own toilet<br />
needs.
AGE Gross Motor Vision & Fine Motor Speech & Language Personal Social<br />
5 years Skips on both feet.<br />
Copies ‘X’ (5 years)<br />
Knows AGE.<br />
Ties shoelaces.<br />
Runs on toes.<br />
Names 4 colours. Dresses and undresses<br />
Copies (5½ years) triangle. Triple order preposition. alone.<br />
Goodenough test 8.<br />
Tell time.<br />
6 years Walks heel to toe<br />
Kicking, throwing, climbing.<br />
Copies<br />
Goodenough test 12.<br />
Imitates or copies<br />
steps with 10 cubes:<br />
1. Goodenough test: 3 + a/4 years (a = each feature recorded in his picture).<br />
2. 10% still not dry by day or night at 5 years.<br />
3. Draw the following: 8 years 10 years 12 years.
Principles of Transport of the Sick Neonate<br />
• Transport of neonates involves pre-transport intensive care level resuscitation<br />
and stabilisation and continuing intra-transport care to ensure that the child<br />
arrives in a stable state.<br />
• Organized neonatal transport teams bring the intensive care environment to<br />
critically ill infants before and during inter-hospital or intra-hospital transport.<br />
• The basis of a safe and timely transport is good communication and<br />
coordination between the referring and receiving hospital to ensure adequate<br />
stabilisation pre-transport and continuing intra-transport care.<br />
• There is a rare need for haste.<br />
• There must be a balance between anticipated clinical complications that may<br />
arise due to delay in definitive care and the benefits of further stabilisation.<br />
1. Special Considerations in Neonates<br />
Apnoea – Premature and septic babies are especially prone to apnoea<br />
Bradycardia – In the newborn, hypoxia causes bradycardia followed by heart block and<br />
asystole<br />
Oxygen toxicity to the lungs and retina - especially important in the premature baby<br />
Reversal to fetal circulation (Persistent pulmonary hypertension of the neonate PPHN)<br />
– Can be precipitated by hypoxia, hypercarbia, acidosis and sepsis<br />
Hypothermia – The mechanisms of thermoregulation are less developed and the child<br />
has a larger body surface area: mass ratio. Non shivering thermogenesis is induced by<br />
the oxidation of brown fat. If the bowels are exposed, the heat and fluid loss are<br />
compounded by evaporation. The effects of hypothermia are acidosis and subsequent<br />
Primary Pulmonary Hypertension, impaired immune function and delayed wound<br />
healing.<br />
Hypoglycemia – The neonate lacks the glycogen store in the liver and fat deposits.<br />
Jaundice – worsen in the baby with sepsis or intestinal obstruction.<br />
2. Mode of transport<br />
Careful consideration must be made as to the mode of transport.<br />
• The best mode of transfer is “in utero” as far as possible. E.g. a mother in<br />
premature labour should be managed in a centre with NICU facilities or if a<br />
surgical anomaly has been detected antenatally, the mother should be advised to<br />
deliver at a centre with paediatric surgical facilities.<br />
• For post natal transfers, the advantages and disadvantages of road, air<br />
(helicopter / commercial airlines) and riverine transport must be considered in<br />
each child. If air transport is chosen, then the effects of decreased atmospheric<br />
pressure on closed cavities and the lack of working space must be taken into<br />
account. Transport incubators with monitors, ventilators and suction equipment<br />
are ideal.<br />
2.1 Air Transport<br />
A number of patients are transported by either the commercial airlines with<br />
pressurised cabins flying at higher altitudes or by helicopters flying at lower altitudes<br />
but without pressurised cabins. There are special problems associated with air<br />
transport:
• Changes in altitude – Physiologic changes associated with altitude are due<br />
to the decreased atmospheric pressure causing a decreased oxygen<br />
concentration and expansion of gases. This becomes especially important in<br />
children with air trapped in closed cavities e.g. pneumothorax,<br />
pneumoperitoneum, volvulus and intestinal obstruction. These cavities must<br />
be drained before setting off as the gases will expand and cause<br />
respiratory distress. Children requiring oxygen may have an increased<br />
requirement and become more tachypnoeic at the higher altitude.<br />
Assessment of hypoxia can be difficult due to poor lighting.<br />
• Noise and Vibration – In addition to causing stress to the baby and the<br />
transport team, there is usually interference with the monitors especially<br />
pulse oximeters. It is also impossible to perform any procedures.<br />
• Limited cabin space – Prevents easy access to the baby especially in the<br />
helicopters. The commercial aircraft and current helicopters also are not able<br />
to accommodate the transport incubators. The baby is thus held in the arms<br />
of a team member.<br />
• Weather conditions and availability of aircraft – Speed of transfer maybe<br />
compromised “waiting” for the availability of aircraft/flight or for the weather to<br />
change. Stress and safety to the baby and team during poor weather<br />
conditions needs to be considered.<br />
• Take off and landing areas – special areas are required and there will be<br />
multiple transfers, e.g. hospital – ambulance – helicopter – ambulance -<br />
hospital<br />
• Finances – Air transport is costly<br />
3. Pre-transport Stabilisation<br />
Transport of the neonate is a significant stress on the child and they can easily<br />
deteriorate during the journey. The presence of hypothermia, hypotension and<br />
metabolic acidosis has a significant negative impact on the eventual patient<br />
outcome. It is also almost impossible to do any significant procedures well during the<br />
actual transport. Therefore, stabilisation pre-transport is critical to ensure a good patient<br />
outcome.<br />
The principles of initial stabilisation of the neonate follow the widely recognised ABC’s of<br />
resuscitation.<br />
Airway<br />
Breathing<br />
Circulation/ {Communication}<br />
Drugs/ {Documentation}<br />
Environment/ {Equipment}<br />
Fluids – Electrolytes/ Glucose<br />
Gastric decompression
3.1 Airway Management<br />
Establish a patent airway<br />
Evaluate the need for oxygen, frequent suction (Oesophageal atresia) or<br />
an artificial airway (potential splinting of diaphragm).<br />
Security of the airway – The endotracheal tubes (ETT) must be secure to<br />
prevent intra-transport dislodgement<br />
Chest X-ray – to check position of the ETT<br />
3.2 Breathing<br />
The need for intra-transport ventilation has to be assessed:<br />
• Requires FiO2 60% to maintain adequate oxygenation<br />
• ABG – PaCO2 >60mmHg<br />
• Tachypnoea and expected respiratory fatigue<br />
• Recurrent apnoeic episodes<br />
• Expected increased abdominal/bowel distension during air<br />
transport<br />
If there is a possibility that the child may require to be ventilated<br />
during the transfer, it is safer to electively intubate and ventilate<br />
before setting off.<br />
However, there may be certain conditions where it may be preferable not<br />
to ventilate if possible, e.g. tracheo-oesophageal fistula. If in doubt, the<br />
receiving surgeon should be consulted. If manual ventilation is to be<br />
performed throughout the journey, due consideration must be taken about<br />
fatigue and possible erratic nature of ventilation.<br />
3.3 Circulation<br />
Assessment:<br />
Heart rate and perfusion (Capillary refill) are good indicators of the<br />
hydration status of the baby. The blood pressure in a neonate drops just<br />
before the baby decompensates. The urine output should be a minimum<br />
of 1-2 mls/kg /hr. The baby can be catheterised or the nappies weighed<br />
(1g = 1 ml urine)<br />
A reliable intravenous access (at least 2 cannulae) must be ensured<br />
before setting off.<br />
If the child is dehydrated, the child must be rehydrated before<br />
leaving.<br />
3.3.1 Fluid Therapy<br />
Resuscitation Fluid<br />
Rate – 10 – 20 mls/kg aliquots given as boluses over up to 2<br />
hours according to the clinical status<br />
Type – Hartmann’s solution<br />
5% Albumin in Normal saline<br />
Fresh Frozen plasma<br />
Blood
This fluid is also used to correct ongoing measured (e.g.<br />
orogastric) or third space losses as required. The perfusion and<br />
heart rates are reliable indicators of the hydration.<br />
Maintenance Fluid<br />
Rate – D1 – 60 mls/kg<br />
D2 – 90 mls/kg<br />
D3 – 120 mls/kg<br />
D4 onwards – 150 mls/kg<br />
Type – In the surgical neonate, the recommended solution is ½<br />
Saline + 10% D/W.<br />
Watch out for hyponatraemia and hypoglycemia.<br />
3.4 Communication<br />
Good communication between the referring doctor, transport team and the<br />
neonatologist / paediatric surgeon will help better coordination of the transfer,<br />
stabilisation of the baby before the transfer and the timing of the transfer, and<br />
preparedness of the receiving hospital.<br />
• Inform the receiving specialist and the emergency department of the<br />
receiving hospital<br />
• Name and telephone contact of the referring doctor and hospital<br />
• Patient details<br />
• History/ physical findings/provisional diagnosis/investigations<br />
• Current management and status of the baby<br />
• Mode of transport/ Expected Times of Departure and Arrival at referral<br />
centre<br />
• Destination of the patient (e.g. A&E, NICU, Ward)<br />
3.5 Drugs as required<br />
• Antibiotics – Most sick neonates will require antibiotics<br />
• Analgesia/ Sedation – especially if the baby has peritonitis or is intubated<br />
• Inotropes<br />
• Vitamin K<br />
• Sodium bicarbonate<br />
3.6 Documentation<br />
History including antenatal and birth history/ Physical Findings/ Diagnosis<br />
Previous and current management<br />
Previous operative and histopathology notes, if any<br />
Input/output charts<br />
Investigation results/ X-rays<br />
Consent – informed and signed by parents especially if high risk<br />
and parents are not escorting<br />
Parents’ contact address and telephone numbers, if not escorting<br />
Mother’s blood – about 5-10 mls for cross match, if the mother cannot<br />
escort the child
3.7 Environment<br />
Neutral Thermal Environment – environmental temperature at which an<br />
infant can sustain a normal temperature with minimal metabolic activity<br />
and oxygen consumption.<br />
Optimal temperature for the neonate (axilla) – 36.5 – 37.0 C<br />
Prevention of heat loss<br />
As the mechanisms of heat loss are radiation, conduction, convection<br />
and evaporation, prevention of heat loss involves maintaining an optimal<br />
ambient temperature as well as covering the exposed surfaces.<br />
• Transport Incubator – would be ideal<br />
• Wrap the body and limbs of the baby with cotton, metal foil or plastic.<br />
• Do not forget a cotton-lined cap for the head.<br />
• Care of the exposed membranes (See section on Abdominal wall<br />
Defects)<br />
• Warm the intravenous fluids<br />
3.8 Equipment<br />
(Please see table at the end of chapter)<br />
Check all equipment - their completeness and function before leaving the<br />
hospital<br />
• Monitors- Cardiorespiratory monitor/ Pulse oximeter for transport would<br />
be ideal. However, if unavailable or if affected by vibration, perfusion, a<br />
praecordial stethoscope and a finger on the pulse will be adequate.<br />
• Syringe and/or infusion pumps with adequately charged batteries<br />
• Intubation and ventilation equipment and endotracheal tubes of varying<br />
sizes<br />
• Oxygen tanks – ensure adequacy for the whole journey<br />
• Suction apparatus and catheters and tubings<br />
• Anticipated medication and water for dilution and injection<br />
• Intravenous fluids and tubings. Pre-draw fluids/ medication into syringes if<br />
required during the journey<br />
3.9 Gastric Decompression<br />
An orogastric tube will be required in nearly all surgical neonates<br />
especially if the baby has intestinal obstruction, congenital diaphragmatic<br />
hernia or abdominal wall defects. The oral route is preferred as a larger<br />
bore tube can be inserted without compromising the nasal passages<br />
(neonates are obligatory nasal breathers). However, the orogastric tube<br />
can easily dislodge and the position needs to be checked regularly. 4<br />
hourly aspiration and free flow of the gastric contents is recommended.
4. Immediately Before Departure<br />
Check vital signs and condition of the baby<br />
Check and secure all tubes<br />
Check the completeness and function of equipment<br />
Recommunicate with receiving doctor about the current status and the expected time of<br />
arrival<br />
5. Intra-transport Care<br />
• Staff –Ideally, there should be a specialised neonatal transport team. If not, the<br />
medical escort should be a neonatal trained doctor with/without a neonatal<br />
trained staff nurse. A minimum of 2 escorts will be required for the<br />
ventilated/critically ill baby. The team should be familiar with resuscitation and<br />
care of a neonate. They should also be able to handle critical incidents. The team<br />
members should preferably not be prone to travel sickness!<br />
• Safety of the team must be a priority. Insurance, life jackets and survival<br />
equipment should be made available for the escort team and parents.<br />
• Monitoring – Regular monitoring of the vital signs, oxygenation and perfusion of<br />
the should be performed<br />
• Fluids – Intravenous fluids must be given to the ill child to prevent dehydration<br />
and acidosis during the transport. Boluses need to be given as necessary<br />
depending on the assessment of the perfusion and heart rate of the child. If<br />
catheterised, the urine output can be monitored. The orogastric tube should be<br />
aspirated as required.<br />
• Temperature Regulation – A check on the baby’s temperature should be made.<br />
Wet clothes should be changed if required especially in the child with abdominal<br />
wall defects. Disposable diapers and one way nappy liners can be very useful<br />
here.<br />
• Critical Incidents – Preoperative preparation is to minimise the critical incidents<br />
as these can cause loss of life and stress to the transport team.<br />
Edge et al (Critical Care Medicine, 1994) showed that the number of critical incidents<br />
that occurred during the transport by a nonspecialised team was 10 times the<br />
occurrence when transported by a specialised team. E.g.<br />
Airway – Blocked /dislodged endotracheal tube<br />
Oxygen Supply – exhausted<br />
Loss of IV Access<br />
Deterioration in patient’s condition<br />
Loss of life or injury to patient /co-worker<br />
6. Arrival at the Receiving Hospital<br />
Reassessment of the baby<br />
Handover to the resident team
7. Special Surgical Conditions<br />
7.1 Oesophageal Atresia with /without Tracheo-oesophageal fistula<br />
(These babies have a risk of aspiration of saliva as well as reflux of the gastric contents<br />
through the distal fistula)<br />
• Evaluation for other anomalies e.g. cardiac, pneumonia, intestinal atresias<br />
• Suction of the upper oesophageal pouch – A Replogle (sump suction) tube<br />
should be inserted and continuous low pressure done if possible. Otherwise,<br />
frequent intermittent (every 10-15 mins) suction of the oropharynx is done<br />
throughout the journey to prevent aspiration pneumonia.<br />
• Ventilation only if absolutely necessary if there is a tracheo-oesophageal fistula<br />
as it may lead to intubation of the fistula, insufflation of the GI tract, and possible<br />
perforation if there is a distal atresia of the bowel.<br />
• Warmth<br />
• Fluids - Maintenance fluids and resuscitation fluids as required<br />
• Position - Lie the baby lateral or prone to minimise aspiration of the saliva and<br />
reflux<br />
• Monitoring – Pulse oximetry and cardiorespiratory monitoring<br />
7.2 Congenital Diaphragmatic Hernia<br />
• Evaluation for associated anomalies and persistent pulmonary hypertension of<br />
the newborn (PPHN)<br />
• Ventilation - Intubation and ventilation may be required pre-transport. Ventilation<br />
with a mask should be avoided and low ventilatory pressures used. A<br />
contralateral pneumothorax or PPHN need to be considered if the child<br />
deteriorates. If the baby is unstable or on high ventilatory settings, the baby<br />
should not be transported. Frequent consultation with a Paediatric Surgeon will<br />
be helpful to decide when to transport the baby. If a chest tube has been<br />
inserted, it should not be clamped during the journey<br />
• Orogastric Tube –– Gastric decompression is essential here and a Size 6 or 8 Fr<br />
tube is inserted, aspirated 4 hourly aspiration and placed on free drainage.<br />
• Fluids – Caution required as dehydration and overload can precipitate PPHN<br />
• Monitoring<br />
• Warmth<br />
• Consent - High risk<br />
• Position – lie baby lateral with the affected side down to optimise ventilation<br />
• Air transport considerations<br />
7.3 Abdominal Wall Defects<br />
Exomphalos and Gastroschisis are the more common abdominal wall defects.<br />
Fluid loss and hypothermia are important considerations in these babies.<br />
Gastroschisis - defect in the anterior abdominal wall about 2-3 cm diameter to the<br />
right of the umbilicus with loops of small and large bowel prolapsing freely<br />
without a covering membrane.<br />
Exomphalos -Defect of anterior abdominal wall of variable size (diameter of<br />
base) It has a membranous covering (amnion, Wharton’s jelly, peritoneum) and<br />
the umbilical cord is usually attached to the apex of the defect. The content of the
large defect is usually liver and bowel but in the small defect the content is just<br />
bowel loops.<br />
• Evaluation – for associated syndromes and cardiac anomalies (more<br />
commonly in babies with exomphalos.<br />
• Fluids – Intravenous fluids are essential as the losses are tremendous<br />
especially from the exposed bowel. Boluses (10-20 mls/kg) of normal saline/<br />
Hartmann’s solution must be given frequently to keep up with the ongoing<br />
losses. A maintenance drip of ½ Saline + 10% D/W at 60 – 90 mls/kg (Day 1<br />
of life) should also be given. Hypoglycemia can occur in about 50% of babies<br />
with Beckwith-Wiedermann’s Syndrome (exomphalos, macroglossia,<br />
gigantism).<br />
• Orogastric tube – Gastric decompression is essential here and a Size 6 or 8<br />
Fr tube is inserted, aspirated 4 hourly and placed on free drainage.<br />
• Warmth – Particular attention must be paid to temperature control because of<br />
the increased exposed surface area and the fluid exudation causing<br />
evaporation and the baby to be wet and cold. Wrapping the baby’s limbs with<br />
cotton and plastic will help.<br />
• Care of the exposed membranes – The bowel/membranes should be<br />
wrapped with a clean plastic film (Clingwrap/Gladwrap) without<br />
compressing, twisting and kinking the bowel. Please do not use a “warm,<br />
saline soaked gauze” directly on the bowel as the gauze will get cold and<br />
stick to the bowel/membranes. Disposable diapers or cloth nappies changed<br />
frequently will help the keep the child dry. The baby may need to be<br />
catheterised to monitor urine output.<br />
• Position – The baby should be placed in a lateral position to prevent tension<br />
and kinking of the bowel.<br />
7.4 Intestinal Obstruction<br />
May be functional e.g. Hirschsprung’s disease or mechanical e.g. atresias, volvulus.<br />
Fluid loss with dehydration and diaphragm splinting needs to be assessed for.<br />
• Evaluation – for associated syndromes and cardiac anomalies.<br />
• Fluids – Intravenous fluids here are essential, too.<br />
Boluses - 10-20 mls/kg Hartmann’s solution/normal saline to correct<br />
dehydration and replace the measured orogastric losses.<br />
Maintenance - ½ Saline + 10% D/W.<br />
• Orogastric tube – Gastric decompression is essential here and a Size 6 or 8 Fr<br />
tube is inserted, aspirated 4 hourly and placed on free drainage.<br />
• Warmth<br />
• Monitoring – vital signs and urine output<br />
• Air transport considerations<br />
7.5 Necrotising Enterocolitis<br />
• Evaluation – These babies are usually premature and septic with severe<br />
metabolic acidosis, coagulopathy and thrombocytopenia. There may be an<br />
associated perforation of the bowel or gangrenous bowel, initiating the referral to<br />
the surgeon.
• Ventilation – Most of the babies may require intubation and ventilation before<br />
setting out especially if are acidotic.<br />
• Fluids – Aggressive correction of the dehydration, acidosis and coagulopathy<br />
should be done before transporting the baby<br />
• Orogastric tube – Essential<br />
• Drugs – Will require antibiotics and possibly inotropic support that needs to be<br />
continued during the journey<br />
• Peritoneal Drain – If there is a perforation of the bowel, insertion of a peritoneal<br />
drain with/without lavage with normal saline or dialysate solution should be<br />
considered. This can help to improve the ventilation as well as the acidosis.<br />
8. Intrahospital Transport<br />
Supine abdominal X-ray showing free<br />
intraperitoneal gas – loss of liver<br />
shadow, falciform ligament seen and<br />
Wrigler’s sign<br />
Loss of Liver shadow<br />
Falciform ligament seen<br />
Wrigler’s sign<br />
• Use transport incubator if available<br />
• Ensure all parties concerned are ready before transfer<br />
• Send team member ahead to commandeer lifts, clear corridors<br />
• Ensure patient is stable before transport<br />
• Skilled medical and nursing staff should accompany patient<br />
• Ensure adequate supply of oxygen<br />
• Prepare essential equipment and monitors for transport<br />
• Ensure venous lines are patent, well secured<br />
• Infusion pumps should have charged batteries. To decrease bulk of equipment,<br />
infusions like insulin, relaxants maybe ceased temporarily
Pre-departure checklist<br />
Equipment Medication<br />
• transport incubator ( if available )<br />
• airway and intubation equipment are all available and working<br />
( ET tubes of appropriate size, laryngoscope, Magill forceps,<br />
• batteries with spares<br />
• manual resuscitation (Ambu) bags and masks of appropriate<br />
size are available and functions properly<br />
• suction device functions properly<br />
• oxygen cylinders are full<br />
• a spare oxygen cylinder is available<br />
• oxygen tubing<br />
• infusion pumps are functioning properly<br />
• intravenous cannulae of various sizes<br />
• needles of different sizes<br />
• syringes and tubings<br />
• suture material<br />
• adhesive tape, scissors<br />
• gloves, gauze, swabs (alcohol and dry)<br />
• stethoscope, thermometer<br />
• nasogastric tube<br />
• pulse oximeter ( if available ) functions properly, set alarm<br />
limits<br />
• cardiac monitor if indicated<br />
• chest clamps ( if an underwater chest drain is present )<br />
Patient status Document<br />
• airway is secured and patent ( must do post intubation chest<br />
X-ray before departure to make sure ET tube is at correct<br />
position )<br />
• venous access is adequate and patent ( at least 2 iv lines )<br />
• iv drip is running well<br />
• patient is safely secured in transport incubator or trolley<br />
• vital signs are charted<br />
• all drains ( if present ) are functioning and secured<br />
• Intravenous fluids<br />
- normal saline<br />
- Hartmann’s solution<br />
- 5% albumin<br />
- 1/5 D/S<br />
- dextrose 10%<br />
• Inotropes<br />
- dopamine<br />
- dobutamine<br />
- adrenaline<br />
• Sedative<br />
- morphine<br />
- midazolam<br />
• Blood product if indicated<br />
• Others<br />
- Atropine<br />
- Sodium bicarbonate<br />
- sterile water for injection<br />
- normal saline for injection<br />
• Patient notes / referral letter<br />
• X-rays<br />
• Consent form<br />
• Vital signs chart<br />
• Input/Output charts<br />
• Maternal blood (for infant)<br />
References<br />
1) Hatch D, Sumner E and Hellmann J: The Surgical Neonate: Anaesthesia and Intensive Care, Edward<br />
Arnold, 1995<br />
2) McCloskey K, Orr R: Pediatric Transport Medicine, Mosby 1995<br />
3) Ferrara A: Evaluation of efficacy of regional perinatal programs Seminar Perinatol. 1: 303-308, 1977<br />
4) Chance GW, O’ Brien MJ, Swyer PR: Transportation of sick neonates 1972: An unsatisfactory aspect<br />
of medical care. Can Med Assoc J 109:847-852, 1973<br />
5) Chance GW, Matthew JD, Gash J et al: Neonatal Transport: A controlled study of skilled assisstance J<br />
Pediatrics 93: 662-666,1978<br />
6) Vilela PC, et al: Risk Factors for Adverse Outcome of Newborns with Gastroschisis in a Brazilian<br />
hospital. J Pediatr Surg 36: 559-564, 2001<br />
7) Pierro A: Metabolism and Nutritional Support in the Surgical neonate. J Pediatr Surg 37: 811-822, 2002<br />
8) Lupton BA, Pendray MR: Regionalized neonatal emergency transport. Seminars in <strong>Neonatology</strong> 9:125-<br />
133, 2004<br />
9) Insoft RM: Essentials of neonatal transport<br />
10) South Carolina Guidelines for air and ground transport<br />
11) Holbrook PR: Textbook of Paediatric Critical Care, Saunders, 1993
Neonatal Resuscitation<br />
High Risk Deliveries<br />
A person trained in neonatal resuscitation is usually called to be present for the following<br />
deliveries:<br />
1. Antepartum factors<br />
• Maternal diabetes<br />
• Pregnancy induced hypertension<br />
• Chronic hypertension<br />
• Anaemia or Rhesus isoimmunisation<br />
• Previous fetal or neonatal death<br />
• Bleeding in second or third trimester<br />
• Maternal infection<br />
• Maternal cardiac, renal, pulmonary,<br />
thyroid or neurological disease<br />
• Oligo/polyhydramnios<br />
• Prolonged rupture of membranes<br />
• Premature rupture of membranes<br />
2. Foetal factors<br />
• Emergency Caesarean section<br />
• Breech or other abnormal presentation<br />
• Premature labour<br />
• Precipitous labour<br />
• PROM > 18 hrs. before delivery<br />
• Prolonged labour (>24 hours)<br />
• Prolonged second stage of labour (>2<br />
hours)<br />
• Fetal bradycardia<br />
Apgar Score<br />
Apgar score<br />
Colour<br />
(Appearance)<br />
0 1 2<br />
Blue or<br />
Pale<br />
Pink centrally.<br />
Blue<br />
extremities<br />
Completely<br />
Pink<br />
Heart Rate Absent < 100/min > 100/min<br />
Response to nasal No Grimace Cough or<br />
stimuli (Grimace)<br />
sneeze<br />
Tone (Activity) Limp Some flexion Active<br />
movement<br />
Breathing<br />
Absent Slow,<br />
Vigorous<br />
(Respiration)<br />
irregular Cry cry<br />
• Post-term gestation<br />
• Multiple pregnancy<br />
• Size-dates discrepancy<br />
• Drug therapy<br />
• Maternal substance abuse<br />
• Fetal Malformation<br />
• Diminished fetal activity<br />
• No prenatal care<br />
• Maternal age < 16 or > 35 years<br />
• Non-reassuring FHR patterns<br />
• Use of general anaesthesia<br />
• Uterine tetany<br />
• Narcotics to mum within 4 hours of<br />
delivery<br />
• Meconium-stained liquor<br />
• Prolapsed cord<br />
• Abruptio placentae<br />
• Placenta praevia<br />
While the Apgar score at birth may not be useful for decision-making at the<br />
beginning of resuscitation, it is helpful for assessing the infant’s condition and<br />
identifying the infant with a problem. Subsequent Apgar scores help in the<br />
assessment of the effectiveness of the resuscitative effort.
5 minutes Apgar score is useful to indicate response to resuscitation and is a rough prognostic indicator. If a<br />
baby scores 100 mmHg)<br />
10. Suction catheters (F5 - F12)<br />
11. Stethoscope – paediatric/ neonatal<br />
12. Umbilical catheterization set with F3.5 and F5 catheters.<br />
13. Endotracheal tubes, size 2.5, 3.0, 3.5, 4.0 mm internal diameter<br />
14. Meconium aspirators<br />
15. Sterile syringes and needles: 1, 2, 5, 10 mls, G21, G23, G25, G19<br />
16. Drugs:<br />
• Volume Expanders (Normal Saline or Ringer’s lactate)<br />
• Adrenaline 1:10000 ( dilute with distilled water 1ml of 1:1000<br />
adrenaline to 10 ml)<br />
• NaHCO3 4.2% ( dilute 8.4% NaHCO3 with equal volume of distilled<br />
water)<br />
• Naloxone (0.4mg/ml preparation)<br />
17. Prewarmed dry towels ( put under radiant warmer)<br />
18. Sterile umbilical catheterisation tray<br />
Before each resuscitation, ensure the following (which would depend on the<br />
estimated size or gestation of the baby):<br />
• Heater is switched on,<br />
• Warm towels have been prepared.<br />
• Oxygen tank is full or nearly full.<br />
• Suction apparatus is working.<br />
• Proper sized masks, ETT tubes, suction catheters are prepared<br />
• Correct sized laryngoscope blade is chosen and the laryngoscope is working.<br />
• Check that the resuscitation bag-valve mask device is functioning properly<br />
including the pop-off valve.
• Drugs are available (and prepared if history suggestive of need). (See the<br />
preparations used in section of drugs)<br />
RESUSCITATION<br />
1. Place infant on preheated radiant warmer<br />
2. If thick or particulate meconium is in the amniotic fluid, perform a tracheal suctioning.<br />
(See notes on Meconium stained liquor).<br />
3. Position the infant with neck slightly extended and suction the mouth first and then<br />
the nose. Suction should be gentle, brief and not too deep (may cause reflex<br />
bradycardia).<br />
4. Dry amniotic fluid thoroughly from the baby and remove the wet linen from contact<br />
with infant.<br />
5. Evaluate the respiration, heart rate and colour.<br />
6. NG tube insertion after 2 minutes of Bag-valve-mask PPV.<br />
7. Indications for Endotracheal Intubation:<br />
When prolonged PPV is required.<br />
When bag-and mask ventilation is ineffective<br />
When tracheal suctioning is required.<br />
When diaphragmatic hernia is suspected.<br />
8. It is important to minimise hypoxia during intubation. Steps to do so include:<br />
Providing free-flow oxygen during intubation without interfering with the<br />
procedure.<br />
Limiting intubation attempts to 20 seconds.<br />
Providing appropriate ventilation with bag and mask using 100% O2 before and<br />
between intubation attempts.<br />
9. Vascular Access – peripheral IV line; umbilical vein or intraosseous.
Can attempt tactile stimulation<br />
once only and briefly. Slap foot,<br />
flick heel, or rub back.<br />
None or gasping<br />
Bag-mask-valve PPV with 100 % O2 for 30<br />
seconds. O2 at 5 L/min. Rate of 40-60/min<br />
(10-15 in 15 sec).<br />
• Infant's neck slightly extended to<br />
ensure open airway.<br />
• Ensure gentle chest rise with bagging.<br />
• If no chest rise:<br />
• Reapply mask<br />
• Reposition head<br />
• Check for secretions, suction if<br />
present.<br />
• Ventilate with mouth slightly open<br />
• Increase pressure slightly<br />
After 30 secs of PPV with 100 % O2<br />
Evaluate Heart Rate<br />
Below 60<br />
• Continue<br />
ventilation<br />
• Chest<br />
Compressions<br />
Initiate medications if<br />
HR below 60 after 30<br />
secs of PPV with<br />
100% oxygen and<br />
chest compressions.<br />
Reevaluate every 30 secs<br />
1. Evaluate Respiration *<br />
< 100/min<br />
60-100<br />
⇒ Discontinue chest compressions<br />
⇒ Continue ventilation<br />
Pink or peripheral<br />
cyanosis<br />
Spontaneous<br />
2. Evaluate Heart Rate<br />
(Count for 6 seconds,X10)<br />
Observe and<br />
monitor<br />
> 100/min<br />
3. Evaluate Colour<br />
Blue<br />
Provide free flow<br />
O2 by using<br />
oxygen tubing<br />
and cupped hand<br />
method with flow<br />
rate of at least 5<br />
L/min until pink.<br />
Withdraw slowly.<br />
Above 100<br />
• Watch for spontaneous<br />
respiration (and do<br />
appropriate bagging if nil)<br />
• Once spontaneous<br />
respiration is established<br />
discontinue ventilation.<br />
Notes on Chest Compressions:<br />
• Provide firm surface or support for the back.<br />
• Locate compression area. It is at the lower third of the sternum<br />
just below an imaginary line drawn between the nipples.<br />
• Compress sternum at a rate of 3 compressions and 1<br />
ventilation per 2 secs, giving 90 compressions and 30<br />
ventilations in 1 minute.<br />
• Compression depth is 1/3 of AP diameter.<br />
• After 30 seconds, stop compressions and check HR for 6<br />
seconds X10<br />
• Complications can occur if technique of chest compressions is<br />
poor e.g. broken ribs, lacerated liver and pneumothorax.
Meconium stained liquor:<br />
Meconium in amniotic fluid<br />
Suction the mouth, pharynx and nose at delivery of<br />
the head (before delivery of shoulders) using a 10F<br />
or larger suction catheter.<br />
Tracheal suctioning can be done by<br />
Infant vigorous?<br />
- Good respiration<br />
- HR > 100/min<br />
- Good muscle tone<br />
NO<br />
As soon as the infant is on radiant warmer and<br />
before drying:<br />
• Residual meconium in the hypopharynx<br />
should be removed by suctioning under direct<br />
vision.<br />
• The trachea must be intubated and meconium<br />
suctioned from the lower airway and repeated<br />
until clear.<br />
Resuscitate as<br />
needed<br />
a) Applying suction (100 mmHg) directly to the ET tube with a meconium<br />
aspirator adapter. Continuous suction is applied to the tube as it is<br />
withdrawn. Reintubation followed by suctioning should be repeated until<br />
returns are nearly free of meconium. DO NOT attempt to suction thick<br />
meconium with a suction catheter through an ET tube (catheter size too<br />
small).<br />
b) Alternatively use a large bore suction catheter (at least 12F) with an end<br />
hole and side hole inserted directly into the trachea. The catheter is rotated<br />
and continuous suction applied as it is being withdrawn. This is the<br />
recommended method in places with no meconium aspirator adapter.<br />
Continuous suction should not be applied for longer than 3 – 5 seconds.<br />
If baby is severely depressed with heart rate < 60/min., positive pressure<br />
ventilation may be needed even if some meconium remains in the airway.<br />
After tracheal suctioning, the stomach should be suctioned to prevent aspiration of<br />
meconium containing gastric contents. This should be done when the child is fully<br />
resuscitated and vital signs are stable.<br />
YES
Medications used in Neonatal Resuscitation:<br />
Type Indications Concentration<br />
to Administer<br />
Adrenaline 1) HR < 60/min<br />
despite a<br />
1:10 000<br />
minimum of 30 (The only<br />
seconds of preparation<br />
adequate available is<br />
ventilation with 1:1000. Dilute<br />
100 % O2 and 1ml of<br />
chest<br />
Adrenaline<br />
compressions. 1:1000 with<br />
2) Heart rate is distilled water<br />
zero.<br />
to 10ml)<br />
Volume<br />
Expanders<br />
Sodium<br />
Bicarb.<br />
Naloxone<br />
HCl<br />
1) Prolonged arrest<br />
not responding to<br />
resuscitation<br />
2)Evidence or<br />
suspicion of acute<br />
blood loss with signs<br />
of hypovolaemia<br />
1)Severe metabolic<br />
acidosis is<br />
suspected or<br />
proven by blood<br />
analysis;<br />
2)Prolonged arrest<br />
not responding to<br />
resuscitation<br />
Severe respiratory<br />
depression and a<br />
history of maternal<br />
narcotics<br />
administered within<br />
the past 4 hours.<br />
Normal Saline<br />
Ringer's lactate<br />
0.5 mEq/ml<br />
(4.2% solution)<br />
0.4 mg/ml<br />
(dilution that is<br />
usually<br />
available)<br />
1.0 mg/ml<br />
Prepara- Dosage/<br />
tion Route<br />
1 ml 0.01-0.03<br />
mg/kg. 0.1-<br />
0.3 ml/kg. IV<br />
or ET<br />
40 ml 10 ml/kg<br />
IV<br />
20 ml or<br />
two 10mlprefilled<br />
syringes<br />
1 ml<br />
2 mEg/Kg<br />
IV only.<br />
(4 ml/kg)<br />
0.1 mg/kg<br />
(0.25 ml/kg)<br />
IV ET IM SC<br />
0.1 mg/kg<br />
(0.1 ml/kg)<br />
IV ET IM SC<br />
Rate/<br />
Precautions<br />
Give rapidly.<br />
May dilute with<br />
normal saline to<br />
1-2 ml if giving<br />
via ET.<br />
Give over 5 – 10<br />
minutes.<br />
Give by syringe<br />
or IV drip.<br />
Give slowly,<br />
over at least 2<br />
minutes.<br />
Give only if<br />
infant is being<br />
effectively<br />
ventilated.<br />
Give rapidly.<br />
IV, ET<br />
preferred. IM,<br />
SC acceptable.
Summary: Use of medications during neonatal resuscitation:<br />
Prolonged arrest that does<br />
not respond to other<br />
therapy?<br />
Give sodium bicarbonate<br />
Post Resuscitation Care<br />
CXR<br />
ABG<br />
Correct metabolic acidosis<br />
BP monitoring<br />
Volume replacement if BP low<br />
Correct Hypocalcaemia & Hypoglycaemia<br />
Treat seizures<br />
Document the resuscitation.<br />
Begin:<br />
• HR zero OR<br />
• HR < 60/min after 30 secs. PPV and<br />
chest compressions.<br />
Give adrenaline<br />
HR above<br />
100?<br />
No<br />
Evidence of continuing depression?<br />
Yes<br />
Evidence or suspicion of acute<br />
blood loss with signs of<br />
hypovolaemia<br />
Give volume expander<br />
Yes<br />
1. Consider other causes, e.g.<br />
Pneumothorax<br />
Diaphragmatic hernia<br />
Persistent pulmonary hypertension (PPHN)<br />
2. Consider starting dopamine<br />
3. Obtain consultation.<br />
Severe respiratory depression and a history<br />
of maternal narcotics administered within the<br />
past 4 hours<br />
May be<br />
repeated every<br />
3-5 minutes if<br />
required<br />
Discontinue<br />
medications<br />
May be<br />
repeated if<br />
signs of<br />
hypovolaemia<br />
persist<br />
Give Naloxone hydrochloride.
Special Circumstances in Resuscitation of the Newly Born Infant<br />
Condition History/Clinical Signs Actions<br />
Meconium or mucus<br />
blockage<br />
Mechanical blockage of the airway<br />
Meconium-stained amniotic<br />
fluid.<br />
Poor chest wall movement.<br />
Choanal Atresia Pink when crying, cyanotic<br />
when quiet<br />
Pharyngeal airway<br />
Persistent retractions, poor<br />
malformation<br />
air entry<br />
Impaired lung function<br />
Pneumothorax Asymmetrical breath<br />
sounds.<br />
Persistent cyanosis /<br />
bradycardia<br />
Pleural effusion / ascites Diminished air movement.<br />
Persistent cyanosis /<br />
bradycardia<br />
Congenital diaphragmatic<br />
hernia<br />
Asymmetrical breath<br />
sounds.<br />
Persistent<br />
cyanosis/bradycardia.<br />
Scaphoid abdomen<br />
Pneumonia/sepsis Diminished air movement.<br />
Persistent cyanosis /<br />
bradycardia<br />
Impaired cardiac function<br />
Congenital heart disease Persistent cyanosis /<br />
Foetal / maternal<br />
haemorrhage<br />
bradycardia<br />
Pallor; poor response to<br />
resuscitation<br />
Intubation for suctioning /<br />
ventilation<br />
Oral airway.<br />
Endotracheal intubation<br />
Prone positioning, posterior<br />
nasopharyngeal tube<br />
Needle thoracentesis<br />
Immediate intubation.<br />
Needle thoracentesis,<br />
paracenteris.<br />
Possible volume expansion.<br />
Endotracheal intubation.<br />
Placement of orogastric<br />
catheter<br />
Endotracheal intubation.<br />
Possible volume expansion<br />
Diagnostic evaluation<br />
Volume expansion, possibly<br />
including red blood cells.<br />
Reference:<br />
1. Textbook of Neonatal Resuscitation from the American Academy of Paediatrics and AHA 2000.<br />
2. International Guideline for Neonatal Resuscitation Consensus (PEDIATRICS Vol. 106 No. 3<br />
September 2000).
Definition<br />
Premature infant: < 37 weeks gestation<br />
THE PREMATURE INFANT<br />
Low Birth Weight (LBW): < 2500 g<br />
Very Low Birth Weight (VLBW): < 1500 g<br />
Extremely Low Birth Weight (ELBW): < 1000 g<br />
Small for Gestational Age: < 10th centile of Birth Weight for age.<br />
Complications in premature infants<br />
a) Perinatal Asphyxia<br />
b) Hypothermia<br />
c) <strong>Respiratory</strong> (RDS and apnoea)<br />
d) CVS (Hypotension, PDA)<br />
e) Neurological: Intraventricular haemorrhage and Periventricular leukomalacia<br />
f) Gastrointestinal (Paralytic ileus, NEC)<br />
g) Hypoglycaemia and hyperglycaemia<br />
h) Neonatal Jaundice<br />
i) Hypoprothrombinaemia<br />
j) Fluid and Electrolyte imbalance (hyponatraemia, hyperkalemia, metabolic acidosis)<br />
k) Anaemia<br />
l) Neonatal Sepsis<br />
m) Rickets<br />
n) Oxygen therapy: ROP, CLD<br />
o) Neuro-developmental disabilities<br />
p) Psychosocial problems<br />
Management<br />
A. Before and During Labour<br />
Prewarmed incubator and appropriate equipment for neonatal intensive care<br />
should always be kept ready in NNU.<br />
B. Adequate Resuscitation<br />
C. Transfer from Labour Room (LR) to NNU (Neonatal Unit)<br />
a) Use prewarmed transport incubator if available. If not the baby must be wiped dry<br />
and wrapped in dry linen before transfer.<br />
b) If the infant's respiration is inadequate, keep the infant INTUBATED and<br />
AMBUBAGGED with oxygen during the transfer.<br />
D. Admission Routine<br />
- Ensure thermoneutral temperature for infant. An incubator or radiant warmer is<br />
necessary for more premature and ill babies.<br />
- Ventilation is often necessary if ventilated during transfer.<br />
- If oxygen saturation is < 90%, oxygen therapy should be given.<br />
- Head circumference (OFC), length measurements and bathing can be omitted.<br />
- Quickly and accurately examine and weigh the infant.
- Assess the gestational age with Dubowitz or Ballard score when stable (see end<br />
of chapter for score).<br />
- Monitor temp, HR, RR, BP and SaO2.<br />
E. Immediate Care for Symptomatic babies<br />
Investigations are necessary as indicated and include:<br />
Blood gases.<br />
Blood glucose (dextrostix).<br />
Full blood count with differential WBC and IT ratio (if possible)<br />
Blood culture.<br />
CXR (if respiratory signs and symptoms are present)<br />
a) Start on 10% dextrose drip.<br />
b) Correct anaemia.<br />
c) Correct hypotension (keep MAP > gestational age in weeks)<br />
Correct Hypovolaemia: Give 10 ml/kg over 20-30 minutes<br />
i) Normal saline<br />
ii) Albumin 5% (If a 25% solution, use 2 - 4 ml/kg diluted to 20 ml/kg<br />
with 0.9 % NaCl.)<br />
iii) Fresh blood if anaemic.<br />
d) Start inotrope infusion if hypotension persists after volume correction.<br />
e) Start antibiotics after taking cultures e.g. Penicillin and Gentamycin<br />
f) Start iv aminophylline in premature babies < 34 weeks if not mechanically<br />
ventilated<br />
g) Maintain SaO2 at 90-95% and PaO2 at 50 –80 mmHg<br />
F. General Measures for all Premature infant and SGA<br />
1. Monitor vitals signs (i.e. colour, temperature, apex beat and respiratory rate) for all<br />
babies. Observe for signs of respiratory distress (i.e. cyanosis, grunting,<br />
tachypnoea, nasal flaring, chest recession and apnoea). In VLBW and ill babies<br />
pulse oximetry and blood pressure monitoring are necessary.<br />
2. Check Dextrostix (see Hypoglycaemia protocol for schedule).<br />
3. Keep warm (Asymptomatic premature babies can be dressed up even while still in<br />
incubator)<br />
4. Feeding (See <strong>Chapter</strong> 8 and 9)<br />
5. Provide parental counselling and allow free parental access.<br />
6. Infection control : observe strict hand washing practices<br />
7. Immunisation:<br />
a. Hep B vaccine is given at birth if infant is stable and BW is >1.8 kg.<br />
Otherwise give when weight reaches 1.8 kg or just before discharge.<br />
b. BCG on discharge if infant has reached at least 1.8 kg and term gestation.<br />
Otherwise ensure that BCG is given at a later date.<br />
c. For long stayers other immunisation should generally follow the schedule<br />
according to chronological rather than corrected age.<br />
In the presence of acute illnesses immunisation is usually deferred.
8. Supplements:<br />
a. At birth : Vitamin K IM (0.5 mg for BW= 2.5 kg)<br />
b. Starting on Day 8 of life if enteral feed volume is more than 2mls/hr , and<br />
infant is not on parenteral nutrition with added vitamins:<br />
Multivitamin 0.5 mls OD ( to be continued for till fully established weaning<br />
diet)<br />
Folic acid 0.1 mg OD.<br />
c. Starting on Day 30 of life:<br />
Elemental Iron 2-3 mg/kg/day – to be continued for 3-4 months<br />
(Dose of ferrous fumerate needed 3 x 2 mg/kg/day.)<br />
G. ICU care and Criteria for Replacement Transfusion in Neonates<br />
See relevant chapter.<br />
H. Discharge<br />
Cranial Ultrasound for premature babies ≤ 30 weeks recommended at:<br />
a. within 72 hours<br />
b. around day 7 to look for IVH<br />
c. around day 28 to look for PVL<br />
d. as clinically indicated<br />
ROP screening at 34 - 36 weeks’ gestation or at 4-6 weeks of age is recommended for<br />
a. all babies < 32 weeks gestation at birth or birth weight
SCORE<br />
Neuromuscular:<br />
Physical:<br />
TOTAL:<br />
BALLARD MATURATIONAL ASSESSMENT OF GESTATIONAL AGE<br />
SCORE<br />
-1 0 1 2 3 4 5<br />
Score<br />
Neuromuscular Maturity Sign<br />
Posture<br />
MATURITY<br />
RATING<br />
Score Weeks<br />
Square Window<br />
(Wrist)<br />
Arm Recoil<br />
-10 20<br />
Popliteal Angle<br />
-5 22<br />
0 24<br />
Scarf Sign<br />
5 26<br />
Heel To Ear<br />
10 28<br />
TOTAL NEUROMUSCULAR MATURITY SCORE<br />
15 30<br />
Score<br />
20 32<br />
25 34<br />
30 36<br />
35 38<br />
40 40<br />
45 42<br />
50 44<br />
Physical Maturity Sign<br />
Skin sticky, friable, gelatinous, red, smooth pink, superficial cracking, pale parchment, deep leathery,<br />
transparent translucent visible veins peeling &/or areas, rare veins cracking, no cracked,<br />
rash, few veins<br />
vessels<br />
wrinkled<br />
Lanugo none sparse abundant thinning bald areas mostly bald<br />
Plantar Surface heel-toe >50 mm faint red marks anterior creases ant. 2/3 creases over entire<br />
40-50 mm: -1 no crease<br />
transverse<br />
sole<br />
Enteral Feeding in Neonates<br />
1. Introduction<br />
• The goal of nutrition is to achieve as near to normal weight gain and growth as<br />
possible.<br />
• Enteral feeding should be introduced as soon as possible. This means starting in<br />
the labor room itself for the well infant.<br />
•<br />
Breast milk is the milk of choice. All mothers should be encourage to give breast<br />
milk to their newborn babies.<br />
• The calorie requirement : Term infants 110 kcal/kg/day<br />
Preterm infants 120 – 140 kcal/kg/day.<br />
2. Type of milk for newborn feeding<br />
There are three choices:<br />
• Expressed breast milk<br />
• Normal infant formula<br />
• Preterm infant formula<br />
2.1 Breast Milk<br />
Breast milk is preferred as studies have shown that babies on breast milk had<br />
low risk for NEC and have better development quotient. 1<br />
However EBM might not be adequate for the nutritional needs of the very<br />
preterm infant as it:.<br />
•<br />
does not have enough calories to ensure optimal early growth at 20<br />
kcal/30mls. 1<br />
• does not have enough sodium to compensate for the high renal sodium<br />
losses of the preterm infant.<br />
• does not have enough calcium or phosphate which will predispose to<br />
osteopenia of prematurity. 2<br />
• deficient in vitamins and iron relative to the needs of a preterm infant.<br />
Human Milk Fortifier (HMF)<br />
• It is recommended to add HMF to EBM in babies < than 32 weeks or<br />
< 1500 grams.<br />
• HMF will give extra calories, vitamins, calcium and phosphate.<br />
• HMF should be added to EBM only when the baby is on feeding at ><br />
140 mls/kg/day.<br />
• 1 sachet (25g) added to 100 mls of EBM increases its strength to 81<br />
cal/100mls.<br />
2.2 Infant Formula<br />
Infant formula should only be given if there is no supply of EBM. There are 2<br />
types of infant formula: Preterm formula and Normal Term Formula.<br />
• Preterm formula : for babies born < 32 weeks or < 1500 grams.<br />
• Normal infant formula : for babies born > 31 weeks or > 1500 grams.
Composition of various milks<br />
Cow’s Standard Preterm Mature<br />
milk formula formula breastmilk<br />
Carbohydrate<br />
(g/100ml)<br />
4.6 7.5 8.6 7.4<br />
Fat<br />
(g/100ml)<br />
3.9 3.6 4.4 4.2<br />
Protein<br />
(g/100ml)<br />
3.4 1.5 2.0 1.1<br />
Casein/<br />
4:1 2:3 2:3 2:3<br />
lactalbumin ratio<br />
Calories /100ml 67 67 80 70<br />
Na+ (mmol/L) 23 16 33 15<br />
K+ (mmol/L) 40 65 33 64<br />
Ca++ (mg%) 124 46 77 35<br />
PO4 (mg %) 98 33 41 15<br />
Fe++ (mg%) 0.05 0.8 0.67 0.08<br />
3. Strategies of administering enteral feeding<br />
3.1. Orogastric Route : Because neonates are obligate nose breathers<br />
nasogastric tube can obstruct the nasal passage and compromise the baby’s<br />
breathing. Thus orogastric route should be use for babies on tube feeding..<br />
3.2. Continuous vs. intermittent bolus feeding: Studies have shown that bolus<br />
fed babies tolerated their feeds better and gain weight faster. 3 Babies on<br />
continuous feeding have been shown to take longer time to reach full feeding but<br />
there is no difference in days of discharge, somatic growth and incidence of<br />
NEC. 4<br />
3.3. Cup feeding : if baby is able to suckle and mother is not with the baby, cup<br />
feeding is preferable to bottle feeding to prevent nipple confusion (if breast<br />
feeding is intended as the final mode of feeding).<br />
4. When to start milk?<br />
As soon as possible for the well term babies<br />
However in the very preterm infant there is a concern of increase risk of NEC if feeding<br />
is started too early. Studies have suggested that rapid increment in feeding has a higher<br />
risk for NEC than the time at which feeding was started. 5<br />
In the very preterm infant MINIMAL ENTERAL FEEDING (MEN) has been<br />
recommended. The principle behind this is to commence very low volume enteral feeds<br />
on day 1 to 3 of life (i.e. at 5 to 25 mls/kg/day ) for both EBM and formula milk. MEN<br />
enhances DNA gut synthesis hence promotes gastrointestinal growth. This approach<br />
allows earlier establishment of full enteral feeds and shorter hospital stays, without any<br />
concomitant increase in NEC. 6
32 weeks Well babies Start milk immediately<br />
29 – 32 weeks Well babies IVD + slow increase enteral feed from<br />
day 1<br />
< 29 weeks Use MEN approach. Start feed on day<br />
2 or 3 at 1 mls 3 hourly with EBM<br />
> 28 weeks Sick babies Feed when clinically appropriate with<br />
EBM<br />
5. How much to increase?<br />
• Generally rate of increment of enteral feeding is about 20 to 30 mls/kg/day.<br />
• Well term babies should be given breast feed on demand.<br />
Milk requirements for babies on full enteral feed from birth:<br />
Day 1 60 mls/kg/day<br />
Day 2 – 3 90 mls/kg/day<br />
Day 4 – 6 120 mls/kg/day<br />
Day 7 onwards 150 mls/kg/day<br />
Add 15% if the babies is under phototherapy<br />
• In babies requiring IV fluids at birth: The rate of increment need to be<br />
individualized to that baby. Babies should be observed for feeding intolerance<br />
(vomit/large aspirate) and observe for any abdominal distention before<br />
increasing the feed.<br />
6. What is the maximum volume?<br />
• The target weight gain should be around 15g/kg/day (range 10-25g/kg/day).<br />
Less than this suggests calories need increasing. More than this should raise<br />
the possibility of fluid overload particularly in babies with chronic lung disease.<br />
Preterm infants • Increase feed accordingly to 180 to 200 mls/kg/day.<br />
• If on EBM, when at 150 mls/kg/day add HMF<br />
Term infant<br />
• Allow demand feeding<br />
o Study by Kuschel et al, a randomised trial in babies born before 30<br />
weeks comparing remaining at a final feed volume of 150 ml/kg/day (120<br />
cal/kg/day) to advancing to 200 mls/kg/day. About half the 200 group had<br />
to be cut back (to a mean of 180 mls/kg/day) due to feed intolerance or<br />
fluid overload. 7<br />
o Infants that require high calories due to increase energy expenditure e.g.<br />
chronic lung disease, should consider adding polycose and MCT.
7. When to stop HMF or Preterm Formula?<br />
Consider changing preterm to standard formula and stopping adding HMF to<br />
EBM when babies reach 1800 grams in weight.<br />
8. Vitamin and mineral supplementation.<br />
Vitamins: A premature infant’s daily breast milk/ breast milk substitute intake will<br />
not supply the daily vitamin requirement. Multivitamin can be commence after<br />
day 7 of life. Vitamin supplements at 0.5 mls daily to be continued for 3-4 months<br />
post discharge.<br />
Iron: Premature infants have been deprived of the intra uterine accumulation of<br />
iron and can become rapidly depleted of iron when active erythropoiesis<br />
resumes. Therefore babies born with a birth weight < 2000g should receive iron<br />
supplements. Iron is given at a dose of 3 mg/kg elemental iron per day. Ferric<br />
Ammonium Citrate (400mg/5mls) contains 86 mg/5 mls of elemental iron. Start<br />
on day 42. Continue until baby is 3-4 months post discharge or until review by<br />
doctor .<br />
Special Cases<br />
1. IUGR babies with reversed end-diastolic flows on antenatal Doppler: Studies<br />
have shown that these babies are at risk of NEC. Thus feeds should be introduced<br />
8, 9<br />
slowly and initially use only EBM.<br />
2. Pregestamil : contain glucose, MCT and protein as casein hydrolysate. Used in<br />
malabsorptive state in infants e.g. Post surgery, biliary obstruction and disaccharide<br />
deficiency<br />
References<br />
1. Lucas A, Gore SM, Cole TJ et al. Multicentre trial on feeding low birthweight infants: effects of diet<br />
on early growth. Arch Dis Child 1984; 59: 722-730.<br />
2. Lyon AJ. McIntosh N. Calcium and phosphorus balance in extremely low birthweight infants in the<br />
first six weeks of life. Arch Dis Child 1984; 59: 1145-50<br />
3. Schandler RJ, Shulman RJ, LauC, Smith EO, Heitkemper MM. Feeding strategies for premature<br />
infants: randomized trial of gastrointestinal priming and tube feeding method. Pediatrics 1999; 103:<br />
492-493.<br />
4. Premji S. & Chessel L. Continuous nasogastric milk feeding versus intermittent bolus milk feeding<br />
for premature infants less than 1500 grams. Cochrane Database of Systematic Reviews. Issue 1,<br />
2002<br />
5. Anderson DM, Kliegman RM. The relationship of neonatal alimentation practices to the occurrence<br />
of endemic necrotizing enterocolitis. Am J Perinatol 1991; 8: 62-7.<br />
6. Tyson JE, Kennedy KA. Minimal enteral nutrition to promote feeding tolerance and prevent<br />
morbidity in parenterally fed neonates (Cochrane Review). In: The Cochrane Library, Issue 1, 1999.<br />
Oxford: Update Software.<br />
7. Kuschel C, Evans N, Askie L, Bredermeyer S, Nash J, Polverino J. A Randomised trial of enteral<br />
feeding volumes in infants born before 30 weeks. Arch Dis Child<br />
8. McDonnell M, Serra-Serra V, Gaffney G, Redman CW, Hope PL. Neonatal outcome after<br />
pregnancy complicated by abnormal velocity waveforms in the umbilical artery. Arch Dis Child<br />
1994; 70: F84-9.<br />
9. Malcolm G, Ellwood D, Devonald K, Beilby R, Henderson-Smart D. Absent or reversed end<br />
diastolic flow velocity in the umbilical artery and necrotising enterocolitis. Arch Dis Child 1991; 66:<br />
805-7.
Total Parenteral Nutrition for Neonates<br />
1. Introduction<br />
Total parenteral nutrition (TPN) is the intravenous infusion of all nutrients<br />
necessary for metabolic requirements and growth<br />
The earlier introduction and more aggressive advancement of TPN was shown to<br />
be safe and effective, even in the smallest and most immature infants.<br />
Premature infants tolerate TPN from day 1 of post-natal life.<br />
The goal of TPN is to :<br />
provide sufficient nutrients to prevent negative energy and nitrogen balance and<br />
essential fatty acid deficiency<br />
support normal rates growth without increased significant morbidity.<br />
Indication for TPN:<br />
gastrointestinal tract abnormalities(omphalocele, gastroschisis, Tracheoesophageal<br />
fistula, malrotation with volvulus, etc).<br />
necrotizing enterocolitis (NEC),<br />
respiratory distress syndrome / BPD patients who are unable to tolerate feedings<br />
extreme prematurity,<br />
sepsis,<br />
malabsorption.<br />
2. Components of TPN<br />
The essential components of parenteral nutrition are:<br />
fluids;<br />
carbohydrate;<br />
electrolytes;<br />
protein;<br />
lipids;<br />
vitamins; and<br />
trace minerals.<br />
When a baby is on parenteral nutrition, our ultimate goal is to provide at least 100-110<br />
cal/kg/day. This will be achieved if we can deliver (for example) 150 cc/kg/day of 12.5%<br />
dextrose, 2.5 g/kg/day of synthetic amino acids, and 3.0 g/kg/day of intravenous lipids.<br />
2.1 Fluid<br />
Fluid is an essential component of parenteral nutrition.<br />
Fluids are usually started at 80-100 ml/kg/day (if newborn), or at whatever<br />
stable fluid intake the baby is already receiving.<br />
Volumes are increased over the first 7 days in line with the fluids and<br />
electrolytes protocol with the aim to deliver 150 ml/kg/day by day 7.<br />
2.2 Amino acids<br />
Amino acids prevents catabolism<br />
Prompt introduction of amino-acids via TPN achieves an early positive nitrogen<br />
balance for the infant
It also decreases the frequency and severity of neonatal hyperglycaemia by<br />
stimulating endogenous insulin secretion and stimulating growth by enhancing<br />
the secretion of insulin and insulin-like growth factors.<br />
Protein is usually started at 1g/kg/day of crystalline amino acids and<br />
subsequently advanced, by 3 rd to 4 th postnatal day, to 3.0 g/kg/day of protein in<br />
term and 3.7 to 4.0 g/kg/day in the extremely low birthweight (ELBW) infants.<br />
Reduction in dosage may be needed in critically ill, significant hypoxaemia,<br />
suspected or proven infection and high dose steroids.<br />
Adverse effects of excess protein include a rise in urea and ammonia and high<br />
levels of potentially toxic amino acids such as phenylalanine.<br />
2.3 Glucose<br />
There is a relatively high energy requirement in the ELBW because of relatively<br />
large body proportion of metabolically active organs i.e. head, liver kidney and<br />
brain and a large and continuous source of glucose is required for energy<br />
metabolism.<br />
In the ELBW minimum supply rate is 6 mg/kg/min to maintain adequate energy<br />
for the brain and an additional 25 cal/kg or 2-3 mg/kg/min of glucose per gram of<br />
protein intake is necessary to support protein deposition. The maximum rate is<br />
12 to 13 mg/kg/min (lower if lipid is administered concurrently) but in practice<br />
glucose administration is often limited by development of hyperglycaemia which<br />
is reported in 20-80% of ELBW infants. This is attributed to peripheral and<br />
hepatic insulin resistance presumably due to glucagon, catecholamine and<br />
cortisol release and decreased insulin secretion.<br />
Strategies for the management of hyperglycaemia in the ELBW include<br />
decreasing glucose administration, administering intravenous amino acids (which<br />
increases insulin secretion) and infusing exogenous insulin infusion.<br />
Glucose administration is usually initiated at 6 mg/kg/min advancing to 10 to 12<br />
mg/kg/min. If hyperglycaemia develops glucose infusion is decreased and if it still<br />
occurs at 3 to 4 mg/kg/min insulin is started.<br />
2.4 Lipid<br />
This is the most controversial of the major intravenous substrate. It is needed to<br />
prevent essential fatty acid deficiency, serve as energy substrate and<br />
improve delivery of fat soluble vitamins.<br />
LBW infants may have immature mechanisms for fat metabolism. A number of<br />
clinical conditions inhibit lipid clearance e.g. infection, stress and malnutrition.<br />
Lipid is usually started at 1g/kg/day and this is gradually increased to a limit of 3<br />
g/kg/day (sometimes up to 3.5g/kg/day in the ELBW)<br />
It is infused continuously over as much of the 24 hour period as practical and<br />
smaller doses are used in patients with infection, compromised pulmonary<br />
function or hyperbilirubinaemia.<br />
In the presence of jaundice requiring phototherapy the higher concentrations of<br />
lipid (>2g/kg/day) should be avoided.<br />
Preparation of 20% emulsion is better than 10% as higher phospholipid value in<br />
10% interferes with triglyceride (TG) clearance leading to higher TG and<br />
cholesterol values<br />
Enzymes responsible for lipid clearance are lipoprotein lipase, hepatic lipase and<br />
lecithin cholesterol acyltransferase. Activation of enzymes can be induced with<br />
the administration of low-dose heparin
Clearance is usually monitored by measuring plasma triglyceride levels. Maximal<br />
plasma triglyceride (TG) concentration ranges from 150 mg/dl to 200 mg/dl.<br />
It has been suggested that exogenous lipid interferes with respiratory function.<br />
Suggested mechanisms include impaired gas exchange from pulmonary<br />
intravascular accumulation or impaired lymph drainage resulting in oedema.<br />
There are reports of increased pulmonary vascular resistance of a dose and time<br />
dependent nature which suggest lipid may aggravate pulmonary hypertension in<br />
susceptible individuals .<br />
2.5 Electrolytes<br />
The usual sodium need of the newborn infant is 2-3 mEq /kg/day in the term and<br />
4-5 mEq/kg/day in the preterm.<br />
Potassium needs are 2-3 mEq/kg/day in both term and preterm infants.<br />
2.6 Minerals, Calcium (Ca), Phosphorus (P) And Magnesium<br />
Presently the premature infant is by no way able to maintain the intrauterine<br />
accretion rate of Ca and P when parenterally fed.<br />
Several methods to prevent precipitation of dibasic calcium phosphate in PN<br />
solutions have been proposed to circumvent this but until now the optimal<br />
retention of calcium and phosphate remains limited to half of the intrauterine<br />
accretion.<br />
Monitoring for osteopaenia of prematurity is important especially when PN is<br />
given for prolonged periods.<br />
A normal magnesium level is a prerequisite for a normal calcaemia. In well<br />
balanced formulations, however, magnesium does not give rise to major<br />
problems.<br />
2.7 Trace Elements<br />
Is indicated if PN is administered for more than 1 week or longer. Commercial<br />
preparations for paediatric use are available.<br />
2.8 Vitamins<br />
Both fat and water soluble vitamins are essential. It should be added to the to fat<br />
infusion instead of amino-acid glucose mixture to reduce loss during<br />
administration<br />
3. Administration<br />
TPN should be delivered where possible through central lines.<br />
Peripheral lines are only suitable for TPN of less than 3 days duration and<br />
dextrose concentration of less than 12.5%.<br />
Peripheral lines is also limited by the osmolality (not more than 600 mOsm/L) of<br />
solutions that can be used to prevent phlebitis.<br />
Usually a percutaneous central line is placed with the position of the tip of the<br />
catheter confirmed on x-ray prior to use.<br />
A strict aseptic technique in preparation and administration of the TPN is<br />
essential.<br />
Ideally, breakage of the central line through which the TPN is infused should be<br />
avoided, though compatible drugs can be administered if necessary.
Cautions<br />
Hyperkalaemia. Addition of potassium is rarely required in first three days of life<br />
unless the serum potassium is < 4.00 mmol/l. Also use caution when prescribing<br />
in renal impairment. A minimal amount is inevitable in TPN because of the type<br />
of amino acid formulation used.<br />
Hypocalcaemia. May result from inadvertent use of excess phosphate. Corrects<br />
with reduction of phosphate.<br />
NEVER add bicarbonate, it will precipitate calcium carbonate out.<br />
NEVER add extra calcium to the burette, it will precipitate out the phosphate.<br />
4. Complications<br />
4.1. Delivery<br />
The line delivering the TPN may be compromised by;<br />
Sepsis, minimized by maintaining strict sterility of the line during and<br />
after insertion.<br />
Malposition, x-ray mandatory before infusion commences.<br />
Thrombophlebitis, with peripheral lines, requiring close observation of<br />
infusion sites.<br />
Extravasation into the soft tissue, with resulting tissue necrosis.<br />
4.2. Metabolic complications<br />
Hyperglycaemia<br />
Hyperlipidaemia<br />
Cholestasis<br />
5. Monitoring<br />
TPN administration requires careful clinical and laboratory monitoring<br />
Before starting an infant on parenteral nutrition, investigation required:<br />
full blood count /haematocrit,<br />
renal profile<br />
liver function test<br />
random blood sugar/dextrostix<br />
serum bilirubin<br />
While on TPN, monitoring required :<br />
5.1. Laboratory<br />
Full blood count, renal profile.<br />
Required daily for 1 week then 3 times a week<br />
Plasma calcium, magnesium, and phosphate.<br />
Twice a week until stable then weekly<br />
Lipid levels.<br />
Twice a week first week then weekly unless complication arises<br />
(sepsis etc)<br />
Long term TPN (> 2 weeks duration) requires, liver function tests.<br />
5.2 Clinical<br />
Blood sugar / dextrostix, 4-6 hrly first 3 days, twice a day once stable.
Daily weight<br />
Meticulous care of the catheter site and monitoring of infection.<br />
This protocol is adapted from :<br />
1 .Feeding in the Neonatal Unit<br />
Dato Dr.Lim Nyok Ling, Consultant Neonatologist, Hospital Selayang.<br />
2. Total Parenteral Nutrition for Neonates.<br />
Department of Neonatal Medicine Protocol Book<br />
Royal Prince Alfred Hospital.<br />
3. Total Parenteral Nutrition for Premature Infants<br />
Elizabeth Brine, MMSc, RD; Judith A. Ernst, DMSc, RD<br />
4. <strong>Neonatology</strong> on the Web<br />
Teaching Files: Parenteral Nutrition (PN) for Neonate<br />
Ray Duncan, MD, Staff Neonatologist, Cedars-Sinai Medical Center, Los Angeles, California.
ICU/NICU: Guidelines. General Pointers for Care and Review of<br />
Infants in NICU<br />
A. Checklist for Review of infant in Intensive Care<br />
i) Age of infant, if 72 hours : 150 ml/kg/day<br />
Generally a 10% dextrose is started on the 1 st day and sodium and potassium is<br />
added on the second day. Empirically a<br />
Preterm baby needs 4-5 mmol/kg/day of sodium and 2-3 mmol/kg/day of<br />
potassium and a<br />
Term infant 2-3 mmol/kg/day of both sodium and potassium<br />
Fluid and electrolyte therapy will be influenced by the child’s underlying illness<br />
and complications and adjustments will have to be made based these conditions,<br />
the child’s intake output, his weight, and blood urea and electrolytes.
Monitor BUSE and correct any imbalances after considering the underlying<br />
cause.<br />
Ensure the urine output is > 1 ml/kg/hr.<br />
vi) Infection<br />
Is there a possibility of infection? Is the child on antibiotics. Fungal infection<br />
should be considered if the infant has been given multiple courses of antibiotics,<br />
is very premature or on central venous catheters and parenteral nutrition<br />
vii) Feeding<br />
Parenteral nutrition should be started in VLBW infants who are unwell as soon as<br />
possible. Bigger babies may be started on parenteral nutrition if not able to be fed<br />
enterally for 3-4 days. Enteral feeds can be given via oro or nasogastric tube.<br />
Encourage expressed breast milk.<br />
viii) Temperature Control<br />
Ensure thermoneutral environment. Covering the open area of open hoods<br />
with cling wrap and increasing water content with a humidifier will help in<br />
temperature control and fluid regulation of the ELBW infant.<br />
ix) Skin care<br />
This is a vital component of care especially for the premature infants.<br />
Avoid direct plastering onto skin and excessive punctures for blood<br />
taking and setting up of infusion lines. Meticulous attention must be<br />
given to avoid extravasation of infusion fluid and medication which can is<br />
to lead to phlebitis, ulceration and septicaemia.<br />
x) CNS<br />
Check for fontanel tension and size, condition of sutures i.e. overriding or<br />
separated, OFC (when indicated e.g. in a case of subaponeurotic<br />
haemorrhage)<br />
Sensorium, tone, movement, responses to procedures e.g. suctioning of<br />
pharynx, and presence or absence of seizure should be assessed.<br />
xi) Ventilation<br />
Check if the ventilation adequate. Is the child maintaining the optimum blood<br />
gases? Can we start weaning the child off the ventilator?
Criteria for Replacement Transfusion in Neonates<br />
B. ETT Care<br />
Clinical Status of the neonate Consider transfusion of 15-20 ml/kg<br />
of packed cells if<br />
Ventilated Hb < 14 g% or vHct < 40%<br />
Symptomatic<br />
(apnoeic spells, poor weight<br />
gain, poor feeding, tachypnoea<br />
tachycardia or oxygen<br />
dependent)<br />
At 1 -2 weeks of life<br />
Hb < 12 g% or vHct < 36%<br />
At 3 - 5 weeks of life<br />
Hb < 10 g% or vHct < 30%<br />
Asymptomatic Hb < 8 g or vHct < 25%<br />
ETT size 3000g size 3.5-4.0<br />
One month - 1 year size 4<br />
1- 2 years size 5<br />
> 2 years size = Age + 4<br />
4<br />
ETT position<br />
a) Oral ETT the "tip-to-lip" distance<br />
1 kg = 7 cm<br />
2 kg = 8 cm<br />
3 kg = 9 cm<br />
or weight in kg + 6<br />
b) Nasal ETT: add 2 cm respectively.<br />
c) Check X-ray after intubation.<br />
Ensure the tip of the ETT is at T2<br />
d) ETT should be shortened if more than 4 cm extends from the lips<br />
Suction of ETT<br />
- Should be done on a prn basis, as it is associated with desaturation and<br />
bradycardia. During suction the FiO2 may need to be increased as guided<br />
by the SaO2 monitor during suctioning. Remember to reduce to the level<br />
needed to keep SaO2 89-95%.
C. UAC and UVC care<br />
UAC position<br />
Length to be inserted measured from the abdominal wall is 3 X BW(kg) + 9<br />
cm. This usually put the tip above the diaphragm. Confirm with X-ray to<br />
ensure that the tip of the UAC is above T12 or below L4.<br />
Wash hands before taking blood from the UAC. Ensure sterile procedure<br />
when handling the hub or 3 way tap of the line.<br />
The UAC is kept patent with a heparin infusion (1U/ml) at 1 ml/hr and can<br />
be attached to the intra-arterial blood pressure monitor.<br />
UVC position<br />
½ UAC +1 cm<br />
D. Ventilation<br />
a) Initial Ventilator Setting (in most situations):<br />
Total Flow: 8 - 10 litres/min<br />
Peak Inspiratory Pressure (PIP): 20-25 mmHg (lower in ELBW infants)<br />
Positive End Expiratory Pressure (PEEP): 4 - 5 mmHg<br />
Inspiration Time:0.4- 0.5 sec<br />
Ventilation rate:40- 60 / min<br />
FiO2: 60 to 70%<br />
The ventilator setting is then adjusted according to the clinical picture, pulse<br />
oximetry reading and ABG which is usually done within the 1st hour.<br />
Note:<br />
1. The inspiration time is usually kept at 1) unless ordered specifically by a<br />
specialist.<br />
3. Tailor the ventilation settings to the baby’s ABG.<br />
Keep: pH 7.35 - 7.45.<br />
PaO2 50 - 80 for premature babies<br />
60 - 100 for term babies<br />
PaCO2 40 - 60 (NB. the trend is not to ‘chase’ the PaCO2<br />
by increasing ventilator settings unless there is<br />
respiratory acidosis).<br />
SaO2 89 - 95%
) Changing of Ventilator settings:<br />
1. To produce an increase in pO2 either: -<br />
a) Increase FiO2 concentration.<br />
b) Increase PEEP.<br />
c) Increase PIP (increases minute volume).<br />
d) RARELY Increase I/E ratio (prolong inspiration)<br />
2. To produce a decrease in pCO2 either: -<br />
a) Increase Rate (increases minute volume)<br />
b) Decrease I/E ratio (prolong expiration)<br />
c) Increase PEEP in worsening lung disease. Decrease PEEP in<br />
recovery phase.<br />
3. Do the opposite to decrease paO2 or to increase paCO2.<br />
Minute volume = tidal volume (volume per breath) x rate per minute<br />
With volume-limited ventilators minute volume can be calculated (use tidal volume = 4-6<br />
ml/kg)<br />
With pressure-limited respirators - increasing peak inspiratory pressure results in increased<br />
minute volume.<br />
e) Sedation and Ventilation<br />
Avoid paralysing the child (e.g. with pancuronium) as far as possible. Paralysing<br />
has been shown to result in poorer lung function and other complications.<br />
Use morphine infusion or intermittent bolus as an analgesia and sedative.<br />
d) Complications of ventilation<br />
Consider the following if the child deteriorates on ventilation:<br />
ETT Dislodged;<br />
Obstructed.<br />
Pneumothorax<br />
Esophagus position<br />
Ventilator tubes disconnected.<br />
Ventilator malfunction<br />
Intraventricular Haemorrhage<br />
Worsening of the primary condition.
HIGH FREQUENCY OSCILLATORY VENTILATION<br />
Indications<br />
• When conventional ventilation fails HFOV should be considered. This is to be<br />
discussed with the specialist.<br />
Practical management<br />
Switching from conventional ventilation to HFOV :<br />
A. Initial setting<br />
1. Leave FiO2 at that on CMV<br />
2.MAP - start at 2 cm H2O above the MAP of conventional ventilation<br />
3.Amplitude - 50-100%; watch thorax vibration<br />
4.Frequency - 10Hz<br />
5.Tidal volume - about 2 to 2.5ml/kg<br />
B. Continuation of HFOV<br />
1. CXR after 30-60 minutes . aim at 8-9 rib level<br />
2. Hypoxia - increase MAP<br />
3. Hyperoxia - reduce FiO2 or decrease MAP<br />
4. Hypercapnia<br />
- increase amplitude<br />
- decrease frequency<br />
- increase MAP<br />
5. Hypocapnia<br />
- decrease amplitude<br />
- increase frequency<br />
- decrease MAP<br />
6. Overinflation<br />
1. reduce MAP<br />
2. decrease frequency<br />
3. discontinue HFOV<br />
C. Weaning<br />
1. Reduce FiO2 to 0.3-0.5<br />
2. Reduce MAP by 1 to 2 mbar per hour until 8 to 9 mbar<br />
3. Reduce amplitude<br />
4. Extubate to head box/CPAP or change to PTV/ SIMV
Guidelines for the Use of Surfactant<br />
Surfactant is expensive, however evidence for its effectiveness is very strong. A systemic<br />
review of 35 randomised controlled trials on surfactant administration over 6000 infants<br />
showed there was a reduction in mortality of 30-40% and there was a reduction in<br />
pulmonary air leak 1,2 . Therefore it is important that a guideline be made available allowing<br />
for optimum usage at minimal expense.<br />
1. All Infants who are require mechanical ventilation for respiratory distress<br />
syndrome (RDS), which is due to surfactant deficiency, should ideally be given<br />
surfactant. However because of the high cost of the drug it is often only given<br />
readily to these infants if they are preterm of 32 weeks and below or birth weight<br />
of 1.5 kg and below. More mature or larger infants should also be given surfactant<br />
if the RDS is severe i.e. arterial alveolar (a/A) PO2 ratio of 0.5<br />
Calculation for a/A PO2 ratio : PaO2 (mmHg)<br />
_________________________<br />
(760-47)FiO2 –PaCO2 (mmHg)<br />
2. Timing of therapy<br />
First dose should be given as early as possible to all preterm infants on<br />
mechanical ventilation for RDS. There is no benefit in administering surfactant<br />
after 24 hours of age. It has been shown that infants who received surfactant<br />
before 2 hours of age had reduced mortality and decreased long term oxygen<br />
dependence and there was no benefit in using more that 2 doses 3 .<br />
3. Types of surfactant and dosage<br />
Survanta, a natural surfactant is the only available surfactant in Malaysia currently.<br />
Dose : 4 ml/kg per dose. Give the 1st dose as soon as possible preferably within<br />
first 2 hours. Repeat at 6 hours later if needed.<br />
Onset of action within minutes.<br />
4. Method of administration<br />
Surfactant is delivered as a bolus directly through an ETT over 15 minutes period,<br />
either via<br />
i) a catheter inserted into the ETT in 2 aliquots via a side port in the ventilator<br />
circuit adjacent to ETT or on the ETT adaptor without the need of removing the<br />
infant from ventilator or<br />
ii) into the side port on ETT adaptor<br />
Rapid installation over 5 minutes is not recommended as it results in an increase in CBFV<br />
(Cerebral Blood Flow Velocity) and PCO2 compared to slower 15-minute bolus 5,6<br />
Infant who remained connected to ventilator during surfactant installation has been shown<br />
to experience less oxygen desaturation compared to those who were disconnected. This<br />
also result in more homogenous distribution of surfactant within the lung
6. Infants must be monitored closely with a pulse oximeter and regular blood gas<br />
measurements. An indwelling intra-arterial line will be useful. Ventilator settings<br />
must be promptly wound down to reduce the risk of pneumothorax.<br />
7. A single dose may be sufficient if after dosing , the oxygen requirement falls<br />
below 30%.<br />
8. Cost effectiveness<br />
Studies on the cost-effectiveness of surfactant therapy show that in spite of the<br />
high cost of drug, its use reduces cost per survivor 7,8 .<br />
References<br />
1. Soll RF and McQueen MC. <strong>Respiratory</strong> distress syndrome. In: Effective Care of Newborn<br />
Infant. Sinclair JC, Bracken MB(eds). Oxford University Press. 1992 pp 325-355<br />
2. Jobe AH. Pulmonary surfactant therapy. New Eng Journal Med 1993; 328(12):861-68<br />
3. OSIRIS Collaborative Group. Early versus delayed administration of a synthetic surfactant:<br />
the judgement of OSIRIS. Lancet 1992;340: 1363-1369<br />
4. Broadbent R, Fok TF, Dolovich M, et al. Chest position and pulmonary deposition of<br />
surfactant in surfactant depleted rabbits. Arch Dis Child 1995; 72: F84-9<br />
5. Saliba EW, Nashashibi M. Vaillant M-C,et al. Instillation rate effects.Exosurf on cerebral<br />
and cardiovascular haemodynamics in preterm neonates. Arch Dis Child 1994;71: F174-8<br />
6. Skinner J. The effects of surfactant on haemodynamics in hyaline membrabe disease. Arch<br />
Dis Child 1997;76:F67-9<br />
7. Mugford M, Piercy J, Chalmers I. Cost implications of different approaches to prevent<br />
respiratory distress syndrome. Arch Dis Child 1991; 66; 757-64<br />
8. Mauskopf JA, Backhouse ME, Jones D, Wold DE, Mammel MC, Mullet M, Guthries R Long<br />
WA. Synthetic surfactant for rescue treatment of RDS in preterm infants weighing from<br />
700-1350g: Impact of hospital resource use and charges. J Paedtr 1995;126:94-101<br />
9. Clinical Practice Guidelines in Perinatology, first edition; 1998:pg 21-28.
Newborn and Acid Base Balance<br />
Rate of metabolism in infants is 2 times as great in relation to body mass as in adult,<br />
which means 2 times as much acid is normally formed which leads to a tendency toward<br />
acidosis. Functional development of kidneys is not complete until the end of the first<br />
month and hence renal regulation of acid base may not be optimum<br />
A. Causes of Acidosis<br />
1. <strong>Respiratory</strong> Acidosis<br />
i) Asphyxia : Damage to respiratory<br />
centre<br />
ii) Obstruction to respiratory tract e.g.<br />
secretions, blocked endotracheal<br />
tube<br />
iii) <strong>Respiratory</strong> conditions :<br />
<strong>Respiratory</strong> distress syndrome<br />
(RDS)<br />
Pneumonia<br />
Pulmonary oedema<br />
Apnoea<br />
2. Metabolic Acidosis<br />
i) Renal failure<br />
ii) Septicaemia<br />
iii) Hypoxia<br />
iv) Hypothermia<br />
v) Hypotension<br />
vi) Cardiac failure<br />
vii) Dehydration<br />
viii) Hyperkalaemia<br />
C. Effects of acidosis and alkalosis in the body<br />
ix) Hyperglycaemia<br />
x) Anaemia<br />
xi) Intraventricular haemorrhage<br />
xii) Drugs (e.g. acetazolamide which is<br />
a carbonic anhydrase inhibitor)<br />
xiii) Metabolic disorders (often<br />
associated with hypoglycaemia)<br />
B. Causes of Alkalosis<br />
1. <strong>Respiratory</strong> alkalosis<br />
i) Asphyxia –over stimulation of<br />
respiratory centre<br />
ii) Over ventilation while on mechanical<br />
ventilation<br />
2. Metabolic alkalosis<br />
i) Administration of sodium<br />
bicarbonate<br />
ii) Pyloric stenosis<br />
iii) Hypokalaemia<br />
iv) Use of diuretics like thiazides and<br />
frusemide<br />
1. Acidosis<br />
i) Depression of central nervous system (CNS)<br />
ii) Disorientation and coma<br />
iii) Increased depth and rate of respiration in metabolic acidosis and depressed<br />
respiration in respiratory acidosis<br />
iv) High PaCO2 in respiratory acidosis increases cerebral blood flow and risk of<br />
intraventricular haemorrhage<br />
2. Alkalosis<br />
i) Over excitability of the CNS<br />
ii) Decreased cerebral blood flow cerebral ischaemia convulsions<br />
D. Measurement of Acid Base Status<br />
Done by analyzing following parameters in an arterial blood gas sample:
pH , PaCO2, PaO2, HCO3 - , Bases Excess<br />
Normal values are:<br />
pH 7.34-7.45<br />
PaCO2<br />
4.7-6.0 kpa (35-45 mmHg)<br />
HCO3 -<br />
20-25 mmol/L<br />
PaO2<br />
8-10 kpa (60-75 mmHg)<br />
BE ± 5 mmol/L<br />
E. Interpretation of Blood Gases<br />
1. pH 7.45 alkalosis<br />
If PaCO2 is low respiratory alkalosis<br />
If HCO3 - and base excess are high metabolic alkalosis<br />
Acidosis and alkalosis may sometimes be compensated partially or fully by the<br />
opposite mechanism for example a metabolic acidosis compensated by respiratory<br />
alkalosis will be associated with a low bicarbonate and PaCO2 but pH will be almost<br />
(partially compensated) or completely (fully compensated) normal<br />
3. Low paCO2 hypocarbia<br />
High PaCO2 hypercarbia<br />
4. Low PaO2 Hypoxaemia<br />
High PaO2 Hyperoxaemia<br />
F. Management of Metabolic Acidosis and Alkalosis<br />
1. Prevention of risk factors for acidosis is important<br />
2. A base deficit of > 5 mmol/L (BE of > -5 mmol/l) in a very sick and premature ( 10 mmol/L usually would need correction in most infants<br />
4. Sodium Bicarbonate (NaHCO3) is the alkali normally used. To prevent the corrosive<br />
effects of hypertonic solutions, Na HCO3 must be diluted with equal parts of distilled<br />
sterile water (i.e. use 4.2% solution)<br />
5. To prevent the toxic effects from large changes in osmolality, smaller dose of<br />
NaHCO3 is used. Since the acid base status is in a dynamic situation the specific<br />
amount of bicarbonate cannot be calculated from any formula but has to be<br />
determined by serial blood gas studies. As a start however the amount to be given<br />
can be based on the following calculation. (8.4% NaHCO3 contains 1 mmol of<br />
bicarbonate per ml)
Dose in mmol of NaHCO3 = Base deficit (mmol/L) x Body weight (kg) x 0.4<br />
6. The underlying cause of acidosis must be sought and treated. For e.g. if the cause is<br />
hypotension the primary treatment is to correct the basic problem and alkali is the<br />
adjunct<br />
7. For metabolic alkalosis treatment is that of the underlying condition<br />
G. Treatment of respiratory acidosis and alkalosis<br />
1. A steadily rising PCO2 at any stage in the disease is an indication that ventilatory<br />
assistance is likely to be needed<br />
2. A sudden rise may be an indication of acute changes in the infant’s condition e.g.<br />
pneumothorax, collapsed lobes, misplaced endotracheal tube<br />
3. A swift rise in PaCO2 often accompanied by hypoxia following weaning is often an<br />
indication that the infant is not ready.<br />
4. A gradual rise in PaCO2 at the end of the first week in a LBW infant on ventilator may<br />
be an indicator of the presence of a patent ductus arteriosus<br />
5. In a child on ventilator, low PaCO2 means the child is likely to be overventilated,<br />
hence treatment is to wean down the ventilation. However in some conditions like<br />
persistent hypertension or cerebral oedema a slightly low PaCO2 may be necessary<br />
in the treatment.<br />
H. Examples of Arterial Blood Gas (ABG) Interpretation<br />
1. A 20 weeks’ gestation and 1.1 kg BW infant has RDS. He is 20 hours old and is being<br />
nursed on nasal CPAP. His ABG shows:<br />
pH 7.21<br />
PaCO2 6.6 kpa<br />
PaO2 7.5 kpa<br />
HCO3 -<br />
20 mmol/L<br />
BE -4 mmol/L<br />
Question (Q) : What does the ABG show?<br />
Answer (A) : Mild respiratory acidosis due to worsening RDS<br />
Q: What is the next appropriate mode of therapy?<br />
A : Mechanical ventilation<br />
2. Below is the ABG of a 10 hour old 28 weeks’ gestation infant<br />
pH 7.22<br />
PaCO2 7 kpa<br />
PaO2 10 kpa<br />
HCO3 -<br />
17 mmol/L<br />
BE -8 mmol/L<br />
Q. What does the ABG show<br />
A. Mixed respiratory and metabolic acidosis
Q. Name a likely diagnosis<br />
A. RDS<br />
3. The following is the ABG of a 40 day old 26 weeks’ gestation baby<br />
pH 7.38<br />
PaCO2 8 kpa<br />
PaO2 8 kpa<br />
HCO3 -<br />
35 mmol/L<br />
BE +10 mmol/L<br />
Q. What does the ABG show?<br />
A. Fully compensated respiratory acidosis by metabolic alkalosis<br />
Q, What is a likely diagnosis?<br />
A. Chronic lung disease<br />
4. An infant of 30 weeks’ gestation and BW 1.3 kg is being ventilated . ABG shows:<br />
pH 7.35<br />
PaCO2 3 kpa<br />
PaO2 15 kpa<br />
HCO3 -<br />
12 mmol/L<br />
BE -12 mmol/L<br />
Q. Interpret the ABG<br />
A. Fully compensated metabolic acidosis by respiratory alkalosis and hyperoxaemia<br />
Q What is your next course of action?<br />
A. Reduce FiO2, administer a small dose of NaHCO3, treat any other contributory<br />
cause of acidosis and wean down ventilation setting<br />
5. A term infant is being ventilated for meconium aspiration. His ABG is as follows :<br />
pH 7.16<br />
PaCO2 10 kpa<br />
PaO2 6 kpa<br />
HCO3 -<br />
16 mmol/L<br />
BE -10 mmol/L<br />
Q. What is likely to have happened?<br />
A. Pneumothorax<br />
Q. What is your interpretation of the ABG<br />
A. Mixed respiratory and metabolic acidosis with hypoxaemia
6. A 6 day old infant is being ventilated for a cyanotic heart disease. ABG shows :<br />
pH 6.8<br />
PaCO2 4.5 kpa<br />
PaO2 3.0 kpa<br />
HCO3 -<br />
8 mmol/L<br />
BE -24 mmol/L<br />
Q. What does the ABG show?<br />
A. Severe metabolic acidosis with severe hypoxaemia<br />
Q. What is your next course of action ?<br />
A. Administer sodium bicarbonate, consider prostaglandin infusion, confirm heart defect<br />
and consider surgery
A. Definition<br />
Birth Asphyxia<br />
There is no accepted definition. It is a result of a combination of hypoxia and<br />
hypoperfusion and affects many organ systems of which the cerebral complication is the<br />
most devastating.<br />
B. Incidence of Birth Asphyxia<br />
C. Diagnosis<br />
Depends on definition used and ranges from 3.7 to 9/1000 livebirths (average of<br />
6/1000 LBs)<br />
Depression of Apgar score of 5 in 5 min. is 4/1000 (Levene 1986)<br />
Hypoxic ischaemic Encephalopathy (HIE) 5-6/1000 term infants and<br />
1 per 1000 dies or survives with neurological damage. 1<br />
1. Meconium staining of amniotic fluid may be an indicator of foetal distress or<br />
intrapartum hypoxia.<br />
2. Abnormal CTG tracing is sometimes present.<br />
3. Acidosis. A low umbilical cord pH is a better indicator of perinatal asphyxia than the<br />
Apgar score 2-4 A pH of
Staging of Neonatal /Hypoxic Ischaemic Encephalopathy (HIE)<br />
MILD (Stage I)<br />
subtle abnormality <br />
days<br />
Irritable with exaggerated<br />
and frequent Moro’s.<br />
Hyperalert (look of<br />
hunger, wide eye gaze,<br />
failure to fixate.<br />
Normal tone<br />
Weak suck ( NG)<br />
Sympathetic dominance<br />
with tachycardia and<br />
mydriasis.<br />
No seizure clinically<br />
No Impairment<br />
Important to note:<br />
Only constant in term infants or > 35 weeks. Not consistent in Prems.<br />
MODERATE<br />
ENCEPHALOPATHY<br />
(Stage II)<br />
Lethargy with <br />
spontaneous movement<br />
Moro’s and other<br />
primitive reflexes lost in<br />
early stages, tendon jerks<br />
exaggerated.<br />
Differential tone with<br />
LL>UL and neck<br />
extensors>flexors<br />
Seizures ++ (lip<br />
smacking, sucking, tonic<br />
or clonic seizures.)<br />
Poor suck (NG required)<br />
Parasympathetic<br />
dominance with<br />
bradycardia and<br />
constricted pupils.<br />
25% Impaired<br />
SEVERE<br />
ENCEPHALOPATHY<br />
(Stage III)<br />
Comatose with little<br />
spontaneous movement<br />
Seizures prolonged and<br />
frequent. In very severely<br />
asphyxiated babies no<br />
seizures clinically or EEG<br />
due to completely<br />
exhausted brain energy)<br />
Severely hypotonic<br />
initially with lost of<br />
reflexes<br />
Death<br />
If recovers there is<br />
excessive hypertonia.<br />
Persistent abnormal<br />
neurological signs beyond<br />
6 weeks means CP.<br />
92% Impaired .<br />
i) Absence of encephalopathy does not mean infant has not suffered significant intrapartum<br />
asphyxia (kidney and heart may be affected).<br />
ii) Encephalopathy can be caused by hypoglycaemia or cerebral haemorrhage and therefore have<br />
to be excluded before diagnosing HIE.<br />
D. Complications of Birth Asphyxia<br />
Brain: Periventricular haemorrhage and periventricular leukomalacia. Intracranial<br />
haemorrhage (subdural (5%), subarachnoid (some), choroid plexus, cerebellum<br />
and thalamus). Cerebral oedema occurs after 24-28 hours.<br />
Kidney: Acute tubular necrosis; oliguria; usually recovers with supportive Rx. Rule<br />
out acute urinary retention.<br />
Heart: Hypoxic ischaemic damage (cardiogenic shock, hypotension, heart failure<br />
with atrioventricular valve regurgitation, arrhythmia).<br />
Lungs: Meconium aspiration common<br />
GIT:stress gastric ulcer, feed intolerance and NEC<br />
Metabolic: SIADH (secondary to head injury) , hypoglycaemia, hypocalcaemia,<br />
hypomagnesaemia<br />
Haematological : DIVC
E. Management<br />
I. Good intrapartum care<br />
II. Adequate and effective resuscitation<br />
III. ICU monitoring for complications. Regular BP, respiratory, urine output, acidosis etc.<br />
IV. General measures:<br />
a) Nurse in thermoneutral environment. Avoid high environmental temperature as<br />
fever is associated with adverse outcome<br />
b) Avoid hypo or hyperglycaemia<br />
c) Adequate ventilation and avoid hypoxaemia and hypercarbia or hypocarbia<br />
d) Review infection risk and Rx with antibiotics<br />
e) Maintain adequate hydration but do not dehydrate or overhydrate<br />
f) Treat jaundice as necessary<br />
V. CVS Rx hypotension with plasma expanders and inotrope support.<br />
Renal Careful assessment of fluid status; if output < 1ml/kg/hr start renal<br />
failure regime; peritoneal dialysis if needed.<br />
Lungs IPPV<br />
Metabolic In SIADH, restrict fluids. Rx hypoglycaemia.<br />
DIVC No specific Rx. Replace with fresh frozen plasma., cryoprecipitate,<br />
platelet or packed cell as indicated<br />
Nutrition Enteral feeding is preferable to parenteral but avoid rapid increase in<br />
feeding to decrease risk of NEC<br />
VI. Brain Orientated Management.<br />
a) Cerebral perfusion: Maintain BP (Mean Arterial Pressure > 40 mmHg)<br />
b) Seizure (Also see chapter on Neonatal Seizures)<br />
o frequent convulsion ( over 3 per hour) or prolonged convulsion ( lasting 3<br />
or more minutes) should be treated 4,5<br />
o Phenobarbitone (loading dose 20 mg/kg with another 20mg/kg for<br />
persistent seizures , and 5 mg/kg OD maintenance dose)<br />
o Clonazepam, lignocaine or phenytoin for persistent seizure. Phenytoin best<br />
avoided for maintenance.<br />
o Prophylactic barbiturate therapy did not show any benefit<br />
c) Intracranial Hypertension<br />
o Fluid restriction and give enough fluid to keep infant on dry side of normal.<br />
(usually less 20 % of daily fluid requirement).<br />
o If full fontanel and seizures give 20% mannitol at 1 g/kg over 20 min.<br />
Mannitol contraindicated in oliguria. Can repeat 6 hourly for maximum<br />
2 - 3 doses.<br />
o Ventilate and keep PaCO2 at 35-45 mmHg. Keeping the PaCO2 less<br />
than this as it can cause cerebral ischaemia. Maintain for 24 - 48 hours<br />
only.<br />
o Steroids are of no use. 6
F. Prognosis<br />
a) Apgar score and mortality.<br />
Mortality in the first year of life for premature babies.<br />
Babies < 2500g : mortality > 80% if Apgar is 0 - 3 at 15 min.<br />
mortality > 95% if Apgar is 0 - 3 at 20 min.<br />
Babies > 2500 g: mortality is 50% if Apgar is 0 - 3 at 15 min.<br />
mortality is 60% if Apgar 0 - 3 at 20 min.<br />
Mortality very high in infants who do not breathe spontaneously at 30 min.<br />
Risk of CP. is 60% for BW > 2500 g if Apgar is 0 - 3 at 20 min.<br />
93% of babies with Apgar 0 at 1 min. and 0-3 at 5 min. were entirely normal<br />
on follow-up. Therefore 15 min and 20 min score is important.<br />
b) Severity of HIE and outcome (most accurate predictor)<br />
No infant with mild HIE alone developed impairment. Mild encephalopathy<br />
carries an excellent prognosis irrespective of Apgar score and parents<br />
should be strongly reassured of excellent outcome.<br />
The median risk for impairment is 25% in moderate NE and 92% in severe<br />
NE.<br />
c) CT scans done after 1st week of life.<br />
Extensive areas of low attenuation with apparent brightness of basal ganglia<br />
are associated with very poor prognosis.<br />
d) Doppler U/S appears to be an accurate predictor for full term babies done after 24<br />
hours of life.<br />
Decrease Pourcelot’s resistivity index (PRI 3 SD of the<br />
normal mean has a +ve predictive value for adverse outcome of 94%.<br />
e) U/S of head can be done at discharge and at 2 - 3 weeks of life to look for<br />
periventricular haemorrhage or periventricular leukomalacia.<br />
f) EEG:<br />
severe abnormalities include burst suppression, low voltage or isoelectric EEG.<br />
moderate abnormalities include slow activity<br />
The overall risks for death or disability were 95% for severely abnormal EEG,<br />
64% for moderately abnormal EEG and 3 % for normal or mildly abnormal EEG 7,8<br />
Continuous EEG monitoring in the first 6-12 hours after birth has been shown to<br />
identify infants at risk of subsequent brain damage 9<br />
Long term :<br />
a. Phenobarbitone will be taken off on discharge if the child is neurologically normal<br />
and feeds normally (by day 7-10).<br />
b. If CNS is abnormal - the duration of phenobarbitone use is controversial.<br />
Probably 3-6 mths. (Longer if EEG abnormal)
c. All doctors managing such infants should never reassure the parents the child is<br />
"Normal" unless on prolonged follow up (at least up to 2yrs) - the milestones are<br />
within normal limits (including normal speech - suspect deafness/mental<br />
retardation if speech delayed).<br />
References<br />
1.Levene ML, Sands C, Grindulis H, Moore JR. Comparison of 2 methods of predicting outcome in perinatal<br />
asphyxia. Lancet 1986;1:67-71<br />
2. Silverman F, Suidan J, Wasserman J, Antoine C, Young BK. The Apgar score: Is it enough? Obstet Gynae<br />
1985;66:331-6<br />
3. Low JA, Panagiotopoulos C, Derick EJ. Newborn complications afterintrapartumasphyxia with metabolic<br />
acidosis in term fetus. Am J Obstet Gynecol 1994;170:1081-7<br />
4.LeveneML. Management of asphyxiated full term infant. Arch Dis Child 1993;68:612-6<br />
5. Evan D, Levene M. Neonatal seizures. Arch Dis Child 1998;78:F70-5<br />
6. Levene MI, Evan DH Medical management of raised intracranial pressure after severe asphyxia. Arch Dis<br />
Child 1985; 60:12-6<br />
7Holme G ,Rowe J, Hafford J, Schmidt R. Prognostic value of EEG in neonatal asphyxia. Electroenceph Clin<br />
Neurophysiol 1982;53: 60-72<br />
8. Thornberg E. Ekstrom-Jodal B. Cerebral function monitoring: a method of predicting outcome in term<br />
neonates after severe perinatal asphyxia .Acta paediatr 1994;83:596-601<br />
9.Helllstorm-Westas L, Rosen I, Svenningsen NW. Predictive value of early continuous amplitude integrated<br />
EEG recording on outcome after severe birth asphyxia in full term infants. Arch Dis Child 1995; 72: F34-8
NEONATAL SEIZURES<br />
Seizures are the most frequent manifestation of neonatal neurological diseases.<br />
It is important to recognize seizures, determine their etiology and treat them because:<br />
1. the seizures may be related to significant diseases and may require specific<br />
treatment<br />
2. the seizures may interfere with supportive measures e.g. feeding and assisted<br />
respiration for associated disorders<br />
3. the seizures per se may be a cause of brain injury.<br />
Clinical<br />
A seizure is defined as a paroxysmal alteration in neurologic function that is behavioral,<br />
motor or autonomic function. This includes clinical phenomena that are associated with<br />
or without surface recorded EEG seizure activity.<br />
Epileptic phenomena can be generated at subcortical (deep limbic, diencephalic, brain<br />
stem) levels in the absence of surface recorded EEG discharges.<br />
Classification of Neonatal Seizures<br />
Clinical seizure EEG seizures Manifestation<br />
Subtle<br />
Clonic<br />
Common Ocular phenomena<br />
- tonic horizontal deviation of eyes common in term infants<br />
- sustained eye opening with fixation common in preterm infants<br />
- blinking<br />
Oral-buccal-lingual movements<br />
- chewing common in preterm infants<br />
- lip smacking, cry-grimace<br />
Limb movements<br />
- pedaling, stepping, rotary arm movements<br />
Apneic spells common in term infants<br />
Focal<br />
Common Well localized clonic jerking, infant usually not unconscious<br />
Multifocal<br />
Tonic<br />
Focal<br />
Generalized<br />
Myoclonic<br />
Focal ,<br />
Multifocal<br />
Generalized<br />
Common<br />
Common<br />
Uncommon<br />
Uncommon<br />
Common<br />
Multifocal clonic movements; simultaneous or in sequence<br />
or non-ordered ( non-Jacksonian) migration<br />
Sustained posturing of a limb, asymmetrical posturing of trunk or<br />
neck<br />
Tonic extension of upper and lower limbs (mimic decerebrate<br />
posturing)<br />
Tonic flexion of upper limbs and extension of lower limbs( mimic<br />
decorticate posturing)<br />
Those with EEG correlates; autonomic phenomena e.g.<br />
increased blood pressure are prominent features.<br />
Well localized, single or multiple, migrating jerks usually of limbs<br />
Single or several bilateral synchronous jerks or flexion<br />
movement occurring more in upper than lower limbs.
Etiology<br />
Determination of etiology is critical because it gives the opportunity to treat specifically<br />
and also to make a meaningful prognosis.<br />
The most important etiology, their usual time of onset and relative frequency in preterm<br />
and term infants are shown in the table below.<br />
Major Etiologies of Neonatal Seizures in Relation to Time of Seizure Onset<br />
and Relative Frequency<br />
Time of onset * Relative frequency #<br />
Etiology 0-3 days > 3days Premature Full term<br />
Hypoxic –ischemic encephalopathy + +++ +++<br />
Intracranial hemorrhage + + ++ +<br />
Intracranial infections + + ++ ++<br />
Developmental defects + + ++ ++<br />
Hypoglycaemia + + +<br />
Hypocalcaemia + + + +<br />
Other metabolic disturbances & IEM + +<br />
Epileptic Syndromes + + +<br />
* postnatal age<br />
# relative frequency of seizures among all etiologies: +++ most common, ++ less common, +least common<br />
( From JJ Volpe: Neurology of the Newborn 4 th edition. <strong>Page</strong> 190)<br />
Notes:<br />
Hypoxic –ischemic encephalopathy (HIE)<br />
Usually 2º to perinatal asphyxia. Most common cause of neonatal seizures in both preterm and term<br />
infant<br />
Characteristically seizures occur in the first 24 hours of life<br />
Present with subtle seizures; multifocal clonic or focal clonic seizures. If focal clonic seizures may<br />
indicate associated focal cerebral infarction.<br />
Intracranial hemorrhage<br />
Hemorrhages are principally germinal matrix-intraventricular (GM-IVH), often with periventricular<br />
hemorrhagic (PVH) infarction in the premature infant.<br />
- Premature infants with severe GM-IVH; onset of seizures in first 3 days, usually generalized tonic type<br />
with subtle seizures.<br />
- Those with associated PVH usually develop seizures after 3 days of life.<br />
In term infants intracranial hemorrhages are principally subarachnoid and subdural hemorrhage.<br />
Subarachnoid hemorrhages may occur in association with HIE. Subdural hemorrhage is often<br />
associated with a traumatic event and present with focal seizures usually in the first 2 days of life.<br />
Intracranial Infection<br />
Intracranial bacterial infections commonly 2º group B streptococci and E. coli.<br />
Nonbacterial infections include toxoplasmosis, herpes simplex, coxsackie B, rubella and<br />
cytomegalovirus.<br />
Developmental Defects<br />
Commonly due to a disturbance in neuronal migration resulting in cerebral cortical dysgenesis e.g.<br />
lissencephaly, pachygyria and polymicrogyria.<br />
Metabolic Disturbances<br />
Hypoglycemia common in SGA infants and infants of diabetic mothers<br />
- occurrence of neurological symptoms is determined by the duration of hypoglycemia. This is more<br />
common in SGA infants compared to IDM<br />
- neurological symptoms include jitteriness, stupor, hypotonia, apnea and seizures.<br />
- often to establish that hypoglycemia is the cause of seizures because of frequently associated<br />
perinatal asphyxia, hypocalcaemia, hemorrhage.
Hypocalcaemia has 2 major peaks of incidences.<br />
1st peak in first 2 to 3 days of life, usually in low birth weight infants, IDM and infants with HIE of<br />
perinatal asphyxia. A therapeutic response to intravenous calcium is helpful in determining low<br />
serum calcium as a cause of the seizures. It is much more common for early hypocalcaemia to be<br />
an association of early seizures rather than a cause.<br />
Later -onset of hypocalcaemia are associated with endocrinopathy ( maternal hypoparathyroidism,<br />
neonatal hypoparathyroidism) and heart disease ( with or without Di George Syndrome), rarely with<br />
nutritional type ( cow’s milk, high phosphorus synthetic milk). Hypomagnesemia is a frequent<br />
accompaniment.<br />
Other metabolic disturbances include neonatal intoxication with lidocaine, hyponatraemia,<br />
hypernatraemia, amino acidopathy ( nonketotic hyperglycinemia), organic acidopathy,<br />
hyperammonemia, mitochondrial disturbance, perioxisomal disorders, pyridoxine dependency<br />
(recalcitrant seizures ceased with intravenous pyridoxine ) and disorder of glucose transport ( low<br />
glucose in CSF but normal blood glucose, treatment with ketogenic diet)<br />
Seizures versus Jitteriness and Other Non-epileptic Movements<br />
Some movements e.g. jitteriness and other normal movement during sleep<br />
(Myoclonic jerks or generalized myoclonic jerks as infant wakes from sleep) or when<br />
awake/ drowsy (roving sometimes dysconjugate eye movements, sucking not<br />
accompanied by ocular fixation or deviation) in newborn may be mistaken for seizures.<br />
Jitteriness versus Seizure<br />
Clinical Features Jitteriness Seizure<br />
Abnormality of gaze or eye movement 0 +<br />
Movements exquisitely stimulus sensitive + 0<br />
Predominant movement tremors* clonic, jerking#<br />
Movements cease with passive flexion of affected limb + 0<br />
Autonomic changes ( tachycardia, ↑ BP, apnea,<br />
0 +<br />
salivation, cutaneous vasomotor phenomena)<br />
* tremors – alternating movements are rhythmical and of equal rate and amplitude<br />
# clonic, jerking – movements with a fast and slow component<br />
( Adapted from JJ Volpe: Neurology in the Newborn 4 th Edition. <strong>Page</strong> 188)<br />
Management.<br />
Selection of the infant to treat with anticonvulsant depends on identification of the<br />
infant with epileptic seizure. Consensus is lacking on necessity for treatment of<br />
minimal or absent clinical phenomena.<br />
Treatment with anticonvulsant is to prevent potential adverse effects on ventilatory<br />
function, circulation and cerebral metabolism ( threat of brain injury)<br />
Controversy regarding identification of adequacy of treatment, elimination of clinical<br />
seizures or electrophysiology seizures. Generally majority attempt to eliminate all or<br />
nearly all clinical seizures.
FLOW CHART: MANAGEMENT OF NEONATAL SEIZURRES<br />
Infant with clinical<br />
seizure<br />
Ensure ventilation and perfusion<br />
adequate (ABC’s)<br />
Dextrostix stat<br />
No Hypoglycemia<br />
Actively convulsing<br />
Hypoglycemia<br />
Phenobarbitone: 20mg/kg IV over 10 -15 minutes<br />
A repeat loading dose of 20mg/kg may be<br />
necessary<br />
Phenytoin: 10mg/kg IV as loading dose<br />
(repeat a 2 nd loading dose if fits recur) via<br />
infusion at 1mg/kg/min – cardiac rate and<br />
rhythm should be monitored during infusion<br />
Actively convulsing<br />
Benzodiazepine:<br />
*Diazepam: 0.3 mg/kg/h IV infusion<br />
*Midazolam:1-4 mcg/kg/min IV infusion<br />
*- limited small study<br />
OTHERS:<br />
Calcium Gluconate, 10% solution: 2 ml/kg, IV<br />
Magnesium sulfate, 50% solution: 0.2 ml/kg, IV<br />
Pyridoxine: 50-100mg IV<br />
Investigations to consider:<br />
Blood sugar, Se Ca, Mg, electrolytes<br />
Septic screen - FBC, Bld C&S, LP, TORCHES<br />
Metabolic screen - blood gas, Se. Ammonia<br />
amino acids, organic acids, other metabolites<br />
Neuroimaging: US,CT Scan brain<br />
EEG<br />
IV 10% Dextrose at<br />
2 ml/kg (200mg/kg)<br />
Then IV glucose infusion<br />
at 8 mg/kg/min infusion<br />
Maintenance therapy:<br />
3-4mg/kg/d q12h, IV or PO<br />
Given 12-24 h after loading<br />
AE: respiratory depression<br />
hypotension<br />
Maintenance therapy:<br />
3-4mg/kg/d q12h, IV<br />
Given 12-24 h after loading<br />
AE: Heart block<br />
hypotension<br />
Maintenance therapy<br />
Midazolam:<br />
AE: respiratory depression, seizure<br />
hypotension, urinary retention
Duration of Anticonvulsant Therapy- Guidelines<br />
(JJ Volpe: Neurology of the Newborn: pg 207)<br />
Optimal duration of therapy relates to the probability of recurrence of seizures if the<br />
drugs are discontinue and the risk of subsequent epilepsy. This can be determined by<br />
considering the neonatal neurological examination, cause of the seizure and the EEG.<br />
Neonatal Period<br />
If neonatal neurological examination becomes normal,<br />
discontinue therapy<br />
If neonatal neurological examination is persistently abnormal<br />
consider etiology and obtain electroencephalogram(EEG)<br />
In most cases – continue phenobarbitone<br />
discontinue phenytoin<br />
reevaluate in a month<br />
One Month after Discharge<br />
If neurological examination has become normal,<br />
discontinue phenobarbitone over 2 weeks<br />
If neurological examination is persistently abnormal, obtain EEG<br />
If no seizure activity or not overtly paroxysmal on EEG, discontinue phenobarbitone<br />
over 2 weeks<br />
If seizure activity is overtly paroxysmal continue phenobarbitone until 3 months of<br />
age and reassess in the same manner.<br />
PROGNOSIS OF NEONATAL SEIZURES<br />
Most important determinant of neurological prognosis is the underlying nature of the<br />
neuropathological process.<br />
Neurological Disease Normal<br />
Development (%)^<br />
Hypoxic Ischemic Encephalopathy 50<br />
Severe Intraventricular Hemorrhage with PVH infarction 10<br />
Primary Subarachnoid Hemorrhage<br />
Hypocalcaemia<br />
Early onset (depends on the prognosis of complicating illness, if no<br />
50<br />
neurological illness present prognosis approaches later onset )<br />
Later onset ( nutritional type)<br />
Hypoglycemia 50<br />
Bacterial Meningitis 50<br />
Developmental defect 0<br />
^ - Prognosis is based on those cases with the stated neurological disease when seizures are a<br />
manifestation. This will differ from overall prognosis of the disease.<br />
(based on JJ Volpe: Neurology in the Newborn:4 th edition. <strong>Page</strong> 202)<br />
References:<br />
1. JJ Volpe: Neurology in the Newborn: Fourth Edition<br />
100
2. Klauss & Fanaroff: Care of The High Risk Neonate: Fifth Edition<br />
3. McDermott CA, Kowalczyk AL, Schnitzler ER et al: Pharmacokinetics of<br />
lorazepam in critically ill neonates with seizures. J Pediar 120: 479- 483,1992<br />
4. Deshmukh a, Wittert W, Schnitzler ER et al: Lorazepam in the treatment of<br />
refractory neonatal seizures: a pilot study.Am J Dis Child140:1042-1044. 1986.<br />
5. MaytalJ, Novak GP, King KC: Lorazepam in the treatment of<br />
refractory neonatal seizures:J Child Neuro6;319-323,1991<br />
6. Hu KC, Chiu NC, Ho CS, Lee ST, Shen EY Continuous midazolam infusion in<br />
the treatment of uncontrollable neonatal seizures. Acta Paediatr Taiwan. 2003<br />
Sep-Oct;44(5):279-81.<br />
7. Ng E, Klinger G, Shah V, Taddio A.Safety of benzodiazepines in Newborns.<br />
Ann Pharmacother. 2002 Jul-Aug;36(7-8):1150-5.<br />
8. Gamstorp I, SedinG; Neonatal convulsions treated with continuous<br />
intravenous infusion of diazepam:Ups J Med Sci87: 143-149, 1982.
NEONATAL HYPOGLYCAEMIA<br />
A. Definition:<br />
Blood sugar < 2.6 mmol/L (approximately 45 mg/dl) in a term or premature infant.<br />
B. Prevention and Early Detection<br />
Anticipation & prevention, when possible, are keys to the management of<br />
hypoglycaemia. Hypoglycaemia may produce long term neurological injury and<br />
the level at which it occurs is controversial.<br />
(i) Identify all high-risk neonates<br />
Prematurity Small for gestational age<br />
Hypothermia Birth Asphyxia / Perinatal Stress<br />
Sepsis Infant of Diabetic Mother<br />
Infant > 4 kg. Polycythaemia<br />
Rhesus disease<br />
(ii) Check glucometer/dextrostix on admission<br />
(iii) Immediate feeding for all well babies who are at risk.<br />
If hypoglycaemic on admission, repeat glucometer 1 hour later after feeding.<br />
Continue monitoring at 2 hours and 4 hours later. (i.e. O,1,2, 4 hours)<br />
If normoglycaemic on admission feed and monitor 6-8 hourly till past stage of<br />
hypoglycaemic risk<br />
(iv) Unwell babies (e.g. birth asphyxia or premature): set up a 10% dextrose drip.<br />
Monitor blood sugar Hourly X 2<br />
Then 2 hourly X 2<br />
Then 4 → 6 → 8 hourly until stable<br />
(v) Clinical features are:<br />
Symptoms are non-specific. For example: apathy, hypotonia, apnoea, poor<br />
sucking, cyanosis, abnormal cry, jitteriness, seizure, lethargy and temperature<br />
instability.<br />
C. If Hypoglycaemia is detected<br />
1. Repeat the glucometer test. Send RBS stat for confirmation.<br />
(Note: monitoring using reagent strip measurement is quick, cheap and easy<br />
but not a precise method)<br />
Check expiry date of test stick!<br />
2. Is the infant symptomatic?<br />
3. When was the last feed given? Is the intravenous drip adequate and running<br />
well? (i.e. not disconnected or extravasated)
D. Asymptomatic Hypoglycaemia<br />
Feed early or bring forward next feed due.<br />
Feed 3 hourly.<br />
Recheck glucometer after 1 hour.<br />
If glucometer still < 2.6 mmol/L and child asymptomatic, can increase<br />
feeds if child can tolerate. Otherwise,<br />
Set up IV D 10% and give at least 72 ml/kg/day<br />
(5 mg/kg/min of glucose)<br />
Continue enteral feeds as tolerated.<br />
Recheck glucometer hourly until stable and then 4-6 hourly.<br />
E. Symptomatic Hypoglycaemia (Glucometer level immaterial)<br />
Give a bolus of 2 ml/kg of IV Dextrose 10% slowly .<br />
Follow-up by an infusion of glucose at 4-6 mg/kg/min (72ml/kg/day<br />
D10%)<br />
Keep nil by mouth<br />
Repeat glucometer after 1/2 to 1 hour and increase the infusion as necessary<br />
to 6-8 mg/kg/min (90 ml/kg/day D10%)<br />
If infection is suspected or there is no alternative explanation for<br />
hypoglycaemia take Blood C&S and treat as sepsis.<br />
Once the blood glucose normalised, feeds can be reintroduced gradually and<br />
infusion tailed off<br />
F. If Hypoglycaemia persists<br />
Take Blood C&S and treat as sepsis if not done yet.<br />
Increase the rate of dextrose infusion if possible (i.e. do not increase beyond<br />
daily requirement).<br />
Increase the concentration of dextrose. Concentrations of 12.5% to 15% may<br />
be needed. If concentration of 12.5% is used, a central line is required<br />
If glucose infusion rates of more than 12mg/kg/min are required,<br />
hyperinsulinism should be seriously considered and investigated accordingly.<br />
Refer specialist<br />
Consider<br />
1. Glucagon 0.2 mg/kg IV (IM) bolus<br />
2. Hydrocortisone 2.5 -5 mg/kg/dose bd IV<br />
3. Diazoxide 5 mg bd orally<br />
4. Adrenaline 500 ng/kg/min IV infusion<br />
5. Somatostatin 1 - 4 microgram SC.<br />
Also need to consider metabolic (See Approach to Hypoglycaemia under<br />
Metabolic section) and endocrine workup.
Key points:<br />
A. Serial blood glucose should be routinely monitored in infants who have risk factors for<br />
hypoglycaemia<br />
B Bolus injections of large volumes of hypertonic glucose solutions should be<br />
avoided - dangerous to neurological function and may be followed by a rebound<br />
hypoglycaemia, cerebral oedema and is caustic to neonatal veins.<br />
C Milk formula provide more energy/ml than 10% dextrose and supply important nonglucose<br />
fuels, which have a glucose sparing role in neurological function.<br />
(Energy content of formula milk is 2750 kJ/l while that of 10% D is 1600 kJ/l). It<br />
promotes ketogenesis and gut maturation.<br />
Breast-feeding should be encouraged as it is more ketogenic.<br />
D. Milk feeds must not be discontinued or reduced when intravenous fluids are given<br />
unless the child develops NEC or other causes of feeding intolerance. The<br />
recommended practice is to feed the baby with as much milk as is tolerated and<br />
to infuse glucose at a rate sufficient to prevent hypoglycaemia. The IV glucose is<br />
then reduced slowly while milk feeds is maintained or increased. May need to<br />
continue over a few days.<br />
E. Ensure volume of intravenous fluid is appropriate for patient, taking into consideration<br />
concomitant problems like cardiac failure, cerebral oedema and renal failure. If unable<br />
to increase volume further, concentration of dextrose to be increased.<br />
Glucose requirement (mg/kg/min) = % of dextrose x rate (ml/hr) x 0.167<br />
------------------------------------------------------wt<br />
(kg)<br />
F. Plasma glucose is 13-18% higher than whole blood glucose. Arterial blood has higher<br />
glucose concentration than venous blood. Capillary sampling can be unreliable in the<br />
presence of poor peripheral circulation.<br />
G. Requirement of >9mg/kg/min suggests hyperinsulinism. Truly hyperinsulinaemic babies<br />
may require 15-20 mg/kg/min<br />
References<br />
Koh G Aynsley-Green A 1988a Neonatal hypoglycaemia- the controversy definition. Arch Dis<br />
Childhood;63:1386-1398<br />
Koh G Aynsley-Green A Tarbit A Etre J 1988b Neural dysfunction during hypoglycaemia. Arch Dis<br />
Childhood;63:1353-1358<br />
DK Pal et al 2000 Neonatal hypoglycaemia in Nepal. Prevalence and risk factors Arch Dis<br />
Childhood;82:F46-52<br />
AA M Moris et al 1996 Evaluation of fast for investigating hypoglycaemia or suspected metabolic disease<br />
Arch Dis Childhood;75:115-119<br />
Gomella, Cunningham ,Eyal and Zenk: Neonatalogy 4 th edition Lange
NEONATAL JAUNDICE<br />
What is jaundice?<br />
Jaundice is apparent clinically when the level of bilirubin in the serum rises above<br />
85µmol/l (5mg/dl). Physiological jaundice is a reflection of the bilirubin load to the liver,<br />
rate of hepatic excretion (liver maturity) and ability of the serum binding protein to retain<br />
the bilirubin within the plasma.<br />
What can go wrong in jaundice?<br />
Elevated serum bilirubin can result in kernicterus, when unconjugated bilirubin is<br />
deposited in the cell wall of neurons in basal ganglia, brain stem and cerebellum<br />
resulting in cell death. Kernicterus is associated with a high mortality, and survivors<br />
usually suffer sequelae like athetoid cerebral palsy, high frequency hearing loss,<br />
paralysis of upward gaze and dental dysplasia. The factors influencing bilirubin toxicity<br />
in the brain cells of the neonate are complex and incompletely understood. There is no<br />
specific level of total serum bilirubin above which kernicterus can be predicted to<br />
happen.<br />
Causes of neonatal jaundice (NNJ)<br />
The following are the recognised causes of NNJ:<br />
• Haemolysis due to ABO or Rh isoimmunisation, G6PD deficiency,<br />
microspherocytosis, drugs<br />
• Physiological jaundice & idiopathic jaundice<br />
• Polycythaemia<br />
• Sepsis e.g. septicaemia, meningitis, urinary tract infection and intra-uterine<br />
infection<br />
• Breastfeeding and breastmilk jaundice<br />
Factors affecting severity of NNJ<br />
The following factors are said to affect the severity of jaundice<br />
• Dehydration<br />
• Large weight loss after birth<br />
• Extravasation of blood, cephalohaematoma, contusion<br />
• Swallowed maternal blood<br />
• Infant of diabetic mother<br />
• Acidosis<br />
• Asphyxia<br />
• Gastrointestinal tract obstruction: increase in enterohepatic circulation<br />
G6PD deficiency<br />
G6PD deficiency is an inherited disorder of the red blood cell, inherited in an x-linked<br />
recessive manner – males are affected while the females are carriers. G6PD is an<br />
enzyme essential in keeping glutathione in the reduced state that in turn is vital to<br />
maintain the integrity of the red cell membrane. In G6PD deficiency the red blood cells<br />
are prone to haemolysis when exposed to oxidants or when certain foods or herbs are<br />
ingested. A list of drugs and herbs that can precipitate haemolysis is provided in Table 1<br />
.
Table 1<br />
Agents to be avoided in G6PD Deficiency Patients<br />
1) Foods and Herbs to be avoided<br />
Fava Beans (Kacang Parang)<br />
Documented Chinese herbs/medicine<br />
Chuen Lin<br />
San Chi<br />
13 herbs<br />
12 herbs<br />
Other traditional herbs/medications are also not<br />
to be taken unless with medical advice<br />
2) Other chemicals to be avoided<br />
Naphthalene (moth balls)<br />
Mosquito coils and insect repellants which<br />
contains pyrethium<br />
3) Drugs to be avoided or contraindicated<br />
Acetanilide<br />
Doxorubicin<br />
Furazolidone<br />
Methylene Blue<br />
Nalidixic acid<br />
Niridazole<br />
Nitrofurantoin<br />
Phenazopyridine<br />
Primaquine<br />
Sulfamethoxazole<br />
Bactrim<br />
MANAGEMENT OF NNJ<br />
4) Drugs that can be safely given in<br />
therapeutic doses<br />
Paracetamol<br />
Ascorbic Acid<br />
Aspirin<br />
Chloramphenicol<br />
Chloroquine<br />
Colchicine<br />
Diphenhydramine<br />
Isoniazid<br />
Phenacetin<br />
Phenylbutazone<br />
Phenytoin<br />
Probenecid<br />
Procainamide<br />
Pyrimethamine<br />
Quinidine<br />
Streptomycin<br />
Sulfisoxazole<br />
Trimethoprim<br />
Tripelennamine<br />
Vitamin K<br />
Mefloquine<br />
History:<br />
The following information needs to be obtained:<br />
• Age of onset and rate of progress (both clinically and also if serial serum bilirubin<br />
(SB) results are available)<br />
• Previous infants with NNJ, kernicterus, neonatal death, G6PD deficiency<br />
• Mother’s blood group (from antenatal history)<br />
• Gestation: although term gestation is taken as 37 completed weeks, infants born<br />
at 37- 38 weeks of gestation are more prone to hyperbilirubinaemia, the<br />
incidence of hyperbilirubinaemia increasing with decreasing gestational age.<br />
• Presence of abnormal symptoms such as apnoea, difficulty in feeding, feed<br />
intolerance and temperature instability.
Physical examination<br />
• General condition: ill-looking if jaundice is severe or if there is presence of some<br />
other illnesses e.g. infection. Neurological signs are present if kernicterus<br />
develops.<br />
• Pallor, presence of cephalohaematoma/subaponeurotic haematoma, petechiae,<br />
purpura, ecchymosis , and hepatosplenomegaly implicate a pathological cause<br />
of jaundice<br />
• Cephalo-caudal progression of severity of jaundice may be seen in some infants,<br />
but correlating with levels of bilirubin is often inaccurate<br />
• Intensity of yellow discoloration in skin and mucosa helps with assessment of the<br />
severity of jaundice<br />
When should a neonate be referred for hospital management? (When to worry?)<br />
The following are indications for referral.<br />
1. Jaundice below umbilicus, corresponding to serum bilirubin of 12-15 mg/dl (200-<br />
250 µmol/L).<br />
2. Jaundice up to level of the sole of the feet - likely to need exchange transfusion.<br />
3. Jaundice within 24 hours of life.<br />
4. Rapid rise of serum bilirubin of more than 8.5 µmol/L/hour (>0.5 mg/dl/hour).<br />
5. Prolonged jaundice of more than 14 days - other causes/conditions need to be<br />
excluded e.g. neonatal hepatitis, biliary atresia.<br />
6. Family history of significant haemolytic disease or kernicterus<br />
7. Clinical symptoms/signs suggestive of other diseases e.g. sepsis.<br />
Laboratory diagnosis<br />
Investigations for NNJ include:<br />
• Total serum bilirubin – sufficient in most cases<br />
• Unconjugated & conjugated fractions in specific conditions e.g. prolonged NNJ<br />
• Infant’s blood group, maternal blood group (if not already known)<br />
• Direct Coomb’s test (if blood group incompatibility is suspected)<br />
• G6PD status (if not known yet)<br />
• Full blood count<br />
• Reticulocyte count<br />
• Peripheral blood film<br />
• Blood culture, urine microscopy and culture ( if infection is suspected)<br />
Treatment<br />
PHOTOTHERAPY<br />
The aim of phototherapy is to prevent potentially dangerous indirect bilirubin levels and<br />
to decrease the need for exchange transfusion, since phototherapy changes bilirubin<br />
into more soluble forms to be excreted in the bile or urine. The effectiveness of<br />
phototherapy is affected by the intensity, or irradiance, of the phototherapy light,<br />
increased irradiance producing increased effectiveness, until the saturation dose of 40<br />
µW/cm 2 /nm of appropriate light is reached. The minimum irradiance is 6-12 µW/cm 2 /nm.<br />
Other factors affecting the effectiveness are the spectrum of light delivered by the<br />
phototherapy unit, the surface area of the infant exposed to phototherapy, and the
distance of the light source from the baby, the optimum distance being 35 - 50 cm in<br />
conventional lights.<br />
Types of photolights<br />
Conventional phototherapy<br />
Fibre optic phototherapy (Biliblanket)<br />
Intensified phototherapy<br />
In cases of mild to moderate jaundice conventional and fibre optic phototherapy usually<br />
suffice but where jaundice is significantly high (e.g. >300 umol/L in a 5 day old or 250<br />
umol/L in a 24 hour old infant ) intensified phototherapy should be used.<br />
The methods of providing intensified phototherapy are as follows:<br />
i. high intensity blue lights ( F20 T12 / BB ) with 7 overhead lamps, and 4 lamps<br />
placed below the infant.<br />
ii. combined fibreoptic blanket with standard phototherapy system above, thus<br />
increasing the surface area of the infant exposed to light.<br />
iii. several phototherapy lamps placed around the infant, if a fibreoptic unit is not<br />
available.<br />
iv. placing a white reflecting surface (e.g. sheet) around the bassinet, so that light is<br />
reflected onto the baby's skin when using a single phototherapy unit so as to<br />
increase the area of exposure.<br />
Phototherapy : Practical considerations.<br />
Position light source 35-50 cm from top surface of the infant (when conventional<br />
fluorescent photolights are used.)<br />
Expose infant appropriately<br />
Cover infant's eyes<br />
Turn infant every 2 hours<br />
Monitor serum bilirubin levels as indicated<br />
Monitor infant's temperature 4 hourly to avoid chilling or overheating<br />
Allow parental-infant interaction<br />
Discontinue phototherapy when bilirubin is less than threshold levels and has been<br />
falling for 24 hours. In infants without haemolytic disease, the average bilirubin<br />
rebound after phototherapy is less than 1 mg/dl (17 µmol/dl). Discharge from hospital<br />
need not be delayed in order to observe the infant for rebound, and in most cases,<br />
no further measurement of bilirubin is necessary. However, if phototherapy is<br />
initiated early and discontinued before the infant is 3 to 4 days old, additional<br />
ambulatory follow-up may be necessary<br />
Measure intensity of phototherapy light periodically using irradiance meters<br />
Turn off light during feeding and blood taking<br />
Hydration- there is no evidence to support any influence of excess fluid<br />
administration on serum bilirubin concentration. Some infants admitted with high<br />
bilirubin levels may also be mildly dehydrated, and may need fluid supplementation.<br />
More frequent breastfeeding is recommended because it inhibits the enterohepatic<br />
circulation of bilirubin and thus lowers the serum bilirubin level. Other routine<br />
supplementation e.g. with dextrose water is not indicated
Once the baby is on phototherapy, visual observation as a means of monitoring is<br />
unreliable. Serum bilirubin levels must guide the management.<br />
EXCHANGE TRANSFUSION (ET)<br />
Bilirubin levels beyond which kernicterus may occur if an ET is not carried out have not<br />
been established. The modality of treatment should be based on the clinical history, risk<br />
factors and physical examination of the infants. The table below illustrates the<br />
recommended levels for various modalities of treatment adapted from the American<br />
Academy Pediatrics for infants of 35 or more weeks of gestation based on different<br />
levels of risk. (Pediatrics 2004, 114: 297-316).<br />
Table 2. Guidelines for Phototherapy and ET in Hospitalised Infants of 35 or More<br />
Weeks’ Gestation<br />
Hours<br />
of life<br />
Infants at lower risk (≥ 38<br />
wk and well)<br />
Intensive<br />
Phototherapy<br />
Total Serum Bilirubin levels mg/dL (umol/L)<br />
Infants at medium risk (≥<br />
38 wk + risk factors OR 35-<br />
37 6/7 wk and well)<br />
ET Intensive<br />
Phototherapy<br />
Infants at higher risk (35-<br />
37 6/7 wk + risk factors)<br />
ET Intensive<br />
Phototherapy<br />
< 24*<br />
24 12 (200) 19 (325) 10 (170) 17 (290) 8 (135) 15 (255)<br />
48 15 (255) 22 (375) 13 (220) 19 (325) 11 (185) 17 (290)<br />
72 18 (305) 24 (410) 15 (255) 21 (360) 13 (220) 18.5 (315)<br />
96 20 (340) 25 (425) 17 (290) 22.5 (380) 14 (240) 19 (325)<br />
> 96 21 (360) 25 (425) 18 (305) 22.5 (380) 15 (255) 19 (325)<br />
Note:<br />
1. Immediate exchange transfusion is recommended if infants show signs of acute bilirubin<br />
encephalopathy (hypertonia, arching, retrocollis, opisthotonus, fever, high pitch cry) or if<br />
TSB is ≥ 5 mg/dL (85 umol/L) above the exchange levels stated above.<br />
2. Start conventional phototheraphy at TSB 3 mg/dL (50 umol/L) below the levels for<br />
intensive phototherapy.<br />
3. Risk factors – isoimmune hemolytic disease; G6PD deficiency, asphyxia, significant<br />
lethargy, temperature instability, sepsis, acidosis or albumin < 3.0 g/dL<br />
4. Use total bilirubin. Do not subtract direct reacting or conjugated bilirubin.<br />
5. During birth hospitalisation, ET is recommended if the TSB rises to these levels despite<br />
intensive phototherapy<br />
6. For readmitted infants, if the TSB level is above the ET level repeat the TSB<br />
measurement every 2 to 3 hours and consider ET if the TSB levels remain above the ET<br />
level for 6 hours under intensive phototherapy<br />
7. *Infants jaundiced at < 24 hours of life are not considered healthy and require further<br />
evaluation.<br />
Infants who are of lower gestation will require phototherapy and ET at lower levels,<br />
(please check with your specialist)<br />
ET
Breastfeeding and Breastmilk Jaundice<br />
Two types of NNJ are associated with breastfeeding, the first known as breastfeeding<br />
jaundice is related to inadequate nursing on the breast resulting in dehydration and<br />
otherwise physiological jaundice becoming more intense; and the second is breastmilk<br />
jaundice which is associated with prolonged jaundice extending beyond the first two<br />
weeks of life. One or more substances in breastmilk e.g. beta glucuronidase may be<br />
responsible for breastmilk jaundice.<br />
PREVENTIVE MEASURES for SEVERE NNJ<br />
Evaluation<br />
1. Maternal prenatal testing should include ABO and Rh(D) typing. When the mother is<br />
Rh-negative, a direct Coombs’ test, ABO blood type, and an Rh(D) type on the<br />
infant’s (cord) blood are recommended<br />
2. All infants must have a glucose-6-phosphate dehydrogenase (G6PD) screening done<br />
on cord blood. The results of G6PD screening must be known before discharge.<br />
Babies with G6PD deficiency must be observed in hospital for at least 5 days, the<br />
period of highest risk for severe jaundice. During this period parents should be<br />
educated on the disorder (e.g. avoidance of certain oxidising drugs and foods) and<br />
monitoring of jaundice can be closely observed and monitored. Breastfeeding must<br />
be encouraged and supported but mothers must avoid taking herbs that have not<br />
been found to be safe and certain foods (e.g. fava beans)<br />
3. Infants whose mothers are of O blood group and infants with a strong family history<br />
of severe neonatal jaundice should be observed for at least 24 hours in the ward. If<br />
earlier discharge is necessary, arrangements must be made for these infants to be<br />
reviewed the next day.<br />
4. Mothers must be assisted and provided support to manage breastfeeding<br />
successfully before discharge.<br />
5. Parents must be alerted to the significance of early onset (within 24 hours) and<br />
severe jaundice and advised that in these situations medical attention is necessary.<br />
6. Follow-up should be provided to all neonates discharged less than 48 hours after<br />
birth by a health care professional in an ambulatory setting, or at home within 2-3<br />
days of discharge<br />
7. Approximately one third of healthy breast-fed infants have persistent jaundice after 2<br />
weeks of age. A measurement of total and direct serum bilirubin should be obtained<br />
and a history of dark urine or light stools should be sought. If the history, physical<br />
examination and direct bilirubin results are normal, continued observation is<br />
appropriate.<br />
Treatment of Jaundice Associated with Breast-feeding in the Healthy Term<br />
Newborn<br />
1. Interruption of breastfeeding in healthy term newborns is discouraged and frequent<br />
breast-feeding (at least 8-10 times every 24 hours) should be continued.<br />
2. Supplementation of breast-feeding with formula with or without phototherapy can be<br />
considered. Supplementing with water or dextrose water does not lower bilirubin<br />
level in jaundiced, healthy, breast-feeding infants.
Reference: extracted from MOH publications<br />
1. CPG on Management of Jaundice in Healthy Term Newborns<br />
2. Guideline on Screening and Management of NNJ with Special Emphasis on G6PD Deficiency
Exchange Transfusion (ET) for Neonatal Jaundice<br />
Purpose<br />
1. To lower the serum bilirubin level and reduce the risk of brain damage and kernicterus.<br />
2. To remove the infants’ sensitised red blood cells and the circulating antibodies and reduce<br />
the degree of red cell destruction.<br />
3. To control the blood volume and relieve potential heart failure..<br />
Preparation of infant<br />
a. Ensure pulse, temperature and respiration are stabilised and maintained.<br />
b. Continue feeding the child and omit only the LAST feed before ET. If needed, empty gastric<br />
content by doing NG aspiration before ET.<br />
c. Proper restraint.<br />
d. Check resuscitation equipment.<br />
e. Set a peripheral IV line.<br />
f. Get a signed informed consent from parent (mortality from ET is 1%).<br />
Grouping of Blood to be used<br />
Rh isoimmunisation- ABO compatible, Rh negative<br />
Other conditions - X match with baby and mother's blood<br />
Emergency - 'O' Rh negative<br />
Fresh whole blood collected in citrate phosphate dextrose ( CPD)<br />
Fresh blood not more than 24 hours old for sick or hydropic infants<br />
Not more than 48 hours (definitely not > 5 days) for other neonates.<br />
Procedure<br />
1. Nurse to assist.<br />
2. Connect baby to cardiac monitor if available.<br />
3. Nurse checks the baseline observations (either via monitor or manually) and record down<br />
on the neonatal exchange blood transfusion sheet. The following observations are recorded<br />
every 15 minutes; apex beat, respirations, colour, tone and behaviour. Dextrostix is to be<br />
done hourly,<br />
4. Doctor performs the ET (See Protocol). At the same time the Nurse keeps a record of apex<br />
beat, condition of baby and the amount of blood given or withdrawn. The whole process<br />
takes at least 90 minutes.<br />
5. Doctor to scrub, gown and mask.<br />
6. Drape the umbilical area.<br />
7. Cannulate the umbilical vein to depth NOT > 5-7cm.<br />
8. Aliquot for removal and replacement : < 2kg - 5 mls<br />
2 to 3 kg - 10 mls<br />
> 3kg - 20 mls<br />
Alternatively blood can be replaced as a continuous infusion into a large vein while removing<br />
blood from an arterial catheter. In smaller infant pumps delivering 120mls an hour allowing 10<br />
ml of blood to be removed every 5 mins can be used. Higher rates will be necessary for bigger<br />
infants. .<br />
Points to note<br />
a. Volume of blood to exchange 160mls/kg body weight. Pre-warm blood if possible.
- 1ml of 4.2% NaHCO3 given for every 100mls of blood *<br />
- 1ml of 10% Calcium gluconate for every 160mls of blood exchanged *<br />
* Agitate Blood bag frequently to prevent settling. NEVER give the two solutions<br />
together. Give via peripheral vein and NOT UVC.<br />
b. Rate of exchange 3 minutes/cycle (1 min in, 1 min pause and 1 min out) and total<br />
exchange should be about 90 minutes.<br />
c. Exchange should start with removal of blood, so that there is always a deficit to avoid<br />
cardiac overload.<br />
d. If child anaemic (Hb < 15) give an extra aliquot volume of blood at the end, leaving a<br />
positive balance).<br />
e. Always discard the serum and the last portion of blood remaining in the tubing to avoid<br />
electrolyte imbalance.<br />
f. If initial SB is > 25mg%, DO NOT remove the UVC as ET may need to be repeated.<br />
g. Place back under phototherapy lights after the procedure<br />
h. Feed after 3 hours.<br />
Investigations<br />
a. Pre-exchange (1st volume of blood removed)<br />
i) Serum Bilirubin<br />
ii) FBC<br />
iii) Blood glucose<br />
iv) Serum electrolytes<br />
v) Serum calcium<br />
vi) Blood gases<br />
vii) Others e.g. Blood C&S as indicated<br />
b. Post-exchange (Last volume of blood<br />
removed)<br />
i) Serum Bilirubin<br />
ii) FBC<br />
iii) Blood Sugar<br />
iv) Serum electrolytes<br />
v) Serum Calcium<br />
vi) Blood gases<br />
c. 6 hour post-exchange<br />
i) SB<br />
Complications of ET<br />
1. Catheter related<br />
a. Infection<br />
b. Haemorrhage<br />
c. NEC<br />
d. Portal and splenic vein thrombosis<br />
e. Air embolism<br />
2. Haemodynamic problems<br />
a. Overload cardiac failure<br />
b. Hypovolaemic shock<br />
c. Arrhythmia (Catheter tip near sinus<br />
node in R Atria)<br />
3. Electrolyte imbalance<br />
a. K+<br />
b. Ca<br />
c. or Blood glucose<br />
d. Acidosis (sometimes late alkalosis due<br />
to breakdown of citrate)<br />
Tissue hypoxia (old blood)<br />
Follow-up<br />
1. Review SB at Polyclinic 2 days after discharge.<br />
2. For infant who had exchange transfusion, follow-up for 2 years and discharge if normal.<br />
Look for signs of deafness, cerebral palsy and mental retardation.
PROLONGED NEONATAL JAUNDICE<br />
Definition: Visible jaundice (or serum bilirubin (SB) >100 umol/L) that persists beyond<br />
14 days of life in a term infant or 21 days in a preterm infant<br />
Importance: The early diagnosis of biliary atresia and hypothyroidism is very important<br />
for favourable long-term outcome of the patient.<br />
An investigation as to the underlying cause is a matter of great urgency!<br />
Causes of Prolonged Neonatal Jaundice<br />
Conjugated Hyperbilirubinaemia Unconjugated Hyperbilirubinaemia<br />
Neonatal Hepatitis Syndrome Septicaemia or UTI<br />
Biliary Atresia Haemolysis<br />
Choledochal Cyst Breast milk Jaundice<br />
Septicaemia or UTI Hypothyroidism<br />
Congenital Infection (TORCHES) Galactosaemia<br />
Metabolic Disorders (e.g. galactosaemia<br />
or -1 antitrypsin deficiency).<br />
Post Total Parenteral Nutrition<br />
Initial Management<br />
Child well<br />
Child unwell or<br />
pale stool<br />
Investigate at OPD<br />
Initial Investigations<br />
Total and fractionated SB<br />
Serum T4,TSH.<br />
Urine FEME and C&S.<br />
Urine reducing sugar &<br />
G6PD Status if screening<br />
results not available.<br />
FBC, Retic count and Film<br />
Admit for<br />
investigations<br />
and treatment<br />
Further Ix depends on<br />
whether it is unconjugated or<br />
conjugated<br />
hyperbilirubinaemia<br />
If it is obstructive (conjugated) jaundice admit<br />
For Further<br />
Investigations<br />
as below
a. If unconjugated hyperbilirubinaemia,<br />
Admit if SB is >300umol/L or child unwell. Otherwise follow-up with weekly SB.<br />
Important investigations are; Thyroid Function Tests, Urine FEME, C&S and reducing<br />
sugar, and FBC, Retic count & Film<br />
Exclude UTI and Hypothyroidism.<br />
Congenital Hypothyroidism is a neonatal emergency. (Check Screening TSH<br />
result if done at birth). See protocol on Congenital Hypothyroidism.<br />
FBC to be done for AB0, G6PD deficiency and Rh incompatibility at 6 weeks to look<br />
for anaemia. KIV Haematinics.<br />
Breast milk Jaundice is a diagnosis of exclusion. Child must be well, gaining<br />
weight appropriately, breast-feeds well and stool is yellow. Management is to<br />
continue breast-feeding. There is a need to tell the parents that the jaundice is likely<br />
due to BM but it is usually of no harm and conversely may confer benefit as bilirubin is<br />
a strong anti-oxidant. Rarely, if the SB is too high (i.e. 25 mg%) then withdrawal of BM<br />
for 48 hours may be appropriate after which breast-feeding should continue. In the<br />
meantime the mother should express her milk to ensure her supply does not diminish.<br />
b. If conjugated hyperbilirubinaemia (conjugated bilirubin > 2mg%)<br />
Admit and observe colour of stool for 3 consecutive days. Further investigations<br />
should include LFT, Hep B and C status, TORCHES and VDRL tests<br />
Start phenobarbitone on admission at 5 mg/kg OD for 5 days to prime the liver for<br />
HIDA scan if eventually required.<br />
If the stool is pale over 3 consecutive days, suspect biliary atresia, and refer to<br />
paediatric surgery. Plans should be made for :<br />
a) Ultrasound of liver<br />
Preferably done after 4 hours of fasting, dilated intrahepatic bile ducts and absent<br />
gall bladder is highly suspicious of extra hepatic biliary atresia.<br />
b) HIDA Scan (if available) after 5 days of phenobarbitone.<br />
Slow uptake with normal excretion: Neonatal Hepatitis syndrome.<br />
Normal uptake with absent excretion: EH Biliary Atresia<br />
c) Liver biopsy (hardly ever done now)<br />
With a good pathologist biliary atresia can be confirmed in 85% by biopsy.<br />
Ensure PT and aPTT normal. If not give Vit K 1 mg IV.<br />
Platelet count at least 40 000<br />
d) Operative Cholangiogram followed by definitive surgery if necessary.<br />
This is now the investigation of choice in most centres.
Biliary Atresia<br />
The importance of distinguishing biliary atresia from neonatal hepatitis is that surgery for<br />
the former (Kasai Procedure) may be successful if carried out within the first 2 months of<br />
life.<br />
With early diagnosis and biliary drainage through a Kasai Procedure before 60 days of<br />
age, successful long-term biliary drainage is achieved in >80% of children. In later<br />
surgery good bile flow is achieved only in 20-30%. Liver transplantation is indicated if<br />
there is failure to achieve or maintain bile drainage.<br />
Neonatal Hepatitis Syndrome<br />
Follow up with LFT fortnightly. Watch out for liver failure and bleeding tendency (Vit K<br />
deficiency).<br />
Repeat Hepatitis B & C screening at 6 weeks.<br />
Most infants with neonatal hepatitis make a complete recovery.<br />
Reference:<br />
1. Lactation Management Course.<br />
2. Nelson’s Textbook Of Pediatrics.<br />
3. Arneil and Forfar’s Paediatrics.
APNOEA IN THE NEWBORN<br />
Definition : Pause in breathing lasting > 15 sec (term) or >20sec (preterm) during<br />
which the infant may develop cyanosis (SpO2 < 80%) and bradycardia (heart rate <<br />
100 per min). In very immature infants, shorter duration of apnoea may produce<br />
bradycardia and cyanosis.<br />
Types: Central – absence of respiratory effort with no gas flow<br />
Obstructive – continued ineffective respiratory effort with no gas flow<br />
Mixed central and obstructive<br />
Periodic breathing – Regular sequence of respiratory pauses of 10-20 sec<br />
interspersed with periods of hyperventilation (4-15 sec) and occurring at least 3x/<br />
minute, not associated with cyanosis or bradycardia.<br />
Aetiology<br />
Symptomatic of underlying problems commoner ones of which are:<br />
1. <strong>Respiratory</strong> conditions – RDS, pulmonary haemorrhage, pneumothorax,<br />
Upper airway obstruction, respiratory depression 2 drugs<br />
2. Sepsis<br />
3. Hypoxaemia<br />
4. Hypothermia<br />
5. CNS abnormality e.g. IVH, asphyxia, increased ICP, seizures<br />
6. Metabolic disturbances – hypoglycaemia, hyponatraemia, hypocalcaemia<br />
7. Cardiac failure, congenital heart disease, anaemia<br />
8. Aspiration/ Gastro-oesophageal reflux<br />
9. NEC/ Abdomen distension<br />
10. Vagal reflex: Nasogastric tube insertion, suctioning, feeding<br />
Recurrent apnoea of prematurity<br />
- usually occur after 3 days of life with no other pathological conditions. Most<br />
disappear by 34- 36 weeks, but some may persist even after 40 weeks ‘corrected’<br />
gestation.<br />
Management<br />
1. Immediate resuscitation.<br />
Surface stimulation<br />
(Flick soles, touch baby)<br />
Gentle nasopharyngeal suction<br />
(Be careful: may prolong apnoea)<br />
Ventilate with bag and mask on previous FiO2.<br />
Be careful not to use supplementary oxygen if the infant has been in air as the child's<br />
lungs are usually normal and a high PaO2 may result in ROP.<br />
Intubate and IPPV if child cyanosed or apnoea recurrent/persistent
2. Review possible causes (as above) and institute specific therapy<br />
e.g. Septic workup if sepsis suspected and commence antibiotics<br />
Remember to check blood glucose via glucometer.<br />
3. Management to prevent recurrence.<br />
Ref<br />
a. Keep at thermoneutral range. Nursing prone may reduce episodes of<br />
apnoea.<br />
b. Titrate the FiO2 to keep the PaO2 between 50 - 80 mmHg<br />
c. Monitoring:<br />
Apnoea monitor<br />
Problem with movement sensitive devices:-<br />
- Very small infants have imperceptible shallow breathing that<br />
causes frequent false alarms.<br />
- Some apnoeic infant will struggle for some time becoming<br />
progressively hypoxic before lying still and triggering the<br />
monitor alarm.<br />
Pulse Oximeter<br />
d. Drug therapy:<br />
IV Aminophylline<br />
Oral Theophylline<br />
e. If repeated attacks.<br />
Regular prophylactic tactile/surface stimulation<br />
Nasal CPAP (3 - 4 cm of H2O)<br />
IPPV (usually low settings)<br />
1. N.R.C. Roberton. Textbook of <strong>Neonatology</strong>. Churchill Livingstone<br />
2. Gomella, Cunningham, Eyal and Zenk. <strong>Neonatology</strong>. 4 th edition Lange<br />
3. Halliday, McClure and Reid. Neonatal Intensive Care. 4 th edition. Saunders<br />
4. Rennie and Roberton. Manual of Neonatal Intensive Care 4 th edition Arnold
History<br />
NEONATAL SEPSIS<br />
Septic Neonates deteriorate very rapidly within hours, therefore:<br />
1) Early diagnosis essential<br />
- even very trivial clinical findings suggesting infection demands full laboratory<br />
evaluation.<br />
2) Initial therapy must be started on clinical suspicion.<br />
Common Bacterial Infection in New-borns and the Antibiotic of Choice<br />
Bacteria Antibiotic of Choice Comments<br />
Group B Streptococcus Penicillin / Cefotaxime 70 - 80%<br />
E. Coli Cefotaxime ± Gentamycin of early<br />
onsetneonatal<br />
infection<br />
Pseudomonas Ceftazidime ± Gentamycin<br />
Other Gram negative bacilli Cefotaxime ± Gentamycin<br />
Staphylococcus Cloxacillin<br />
Listeria Monocytogenes Ampicillin + Gentamycin<br />
Anaerobes Metronidazole<br />
Candida Fluconazole / Amphotericin<br />
1. Is the infant compromised? (e.g. prematurity, indwelling catheter, endotracheal tube)<br />
2. Perinatal history (prolong rupture of membrane, maternal fever, positive HVS)<br />
3. Risk of nosocomial infection from staff, relatives or other sick infants.<br />
Early signs & symptoms<br />
1. Temperature instability: Hypo & Hyperthermia<br />
• 37.5 o C for >1hr or 2hrs in an appropriate environmental<br />
temperature is due to infection until proven otherwise.<br />
2. Refusal to feed in a previously healthy baby.<br />
3. Poor weight gain.<br />
4. Listlessness, lethargy, hypotonia, pallor, mottled skin<br />
• Baby just doesn't seem right<br />
• When a nurse tells you this, please take serious note<br />
5. Irritable; will not stop crying or whimpering even after feeding.<br />
6. Rapidly increasing neonatal jaundice in the absence of haemolytic disease.<br />
7. Vomiting and Diarrhoea (NB ‘Acute Gastroenteritis’ in a neonate is septicaemia<br />
until proven otherwise)<br />
8. Ileus/intestinal obstruction - vomiting, abdominal distension and constipation<br />
9. Pseudoparalysis - arthritis/osteomyelitis<br />
10. Apnoea - common early sign in Prems.<br />
11. Tachypnoea<br />
Investigations
Always:<br />
1. FBC: Hb, TWBC with differential count, Platelet.<br />
There is normally a leucocytosis up to 30 x10 9 /L at birth.<br />
Indicators of infection:<br />
1st day - Neutropenia; immature cells & toxic granulation<br />
Beyond 3 days- Polymorph > 7.5-8.0x10 9 /L or < 2x10 9 /L<br />
Monocytes > 0.8 x 10 9 /L<br />
Both thrombocytopenia and thrombocytosis may implicate infection<br />
2.. Blood C&S<br />
When available:<br />
1. C reactive protein (CRP) : A raised CRP is presumptive of infection and will help in<br />
deciding on the start of antibiotics if clinical picture is uncertain till the result of culture and<br />
sensitivity is available. It may also help in deciding on the duration of antibiotic therapy.<br />
When indicated :<br />
1. Lumbar Puncture (CSF biochemistry, microscopy, latex agglutination for bacterial<br />
antigen and culture and sensitivity)<br />
2. CXR<br />
3. AXR<br />
4. Maternal HVS C&S (Ring up postnatal ward to see if it has been done)<br />
5. Culture of ETT aspirate<br />
6. Culture of tip of IV cannula / umbilical catheters.<br />
7. Urine FEME and C&S / SPA urine C&S<br />
8. ABG<br />
Treatment<br />
1. Antibiotics<br />
- Start immediately when diagnosis is suspected and after all appropriate specimens<br />
taken. Do not wait for C&S result!<br />
Recommended Empiric Therapy:<br />
For early-onset infection:<br />
IV Penicillin and IV Gentamycin to cover for GBS and Pneumococci. / Gram negative<br />
organisms (Use high dose Penicillin 100,000U/kg)<br />
For late-onset community acquired infection:<br />
IV Cloxacillin and Gentamycin to cover for Staphylococci / Gram negative organisms in<br />
non-CNS sepsis, cefotaxime and penicillin for CNS infection<br />
For nosocomial (hospital acquired) infections:
Antibiotic choice will depend on prevailing infecting organisms and their sensitivities. A<br />
carbapenem and vancomycin are often used in units where ESBL and MRSA/MRSE are<br />
common<br />
- Add metronidazole if intra-abdominal sepsis or NEC present.<br />
- Consider fungal septicaemia if child does not respond especially preterm with or without<br />
long lines and usage of TPN.<br />
Adjust final antibiotics according to C&S results.<br />
Duration of therapy:<br />
- If cultures are negative and infection is clinically unlikely after further review, off<br />
antibiotics by 48-72 hours.<br />
- If proven infection: 10 days for septicaemia, 7-14 days for pneumonia and 14 to 21<br />
days for meningitis and septicaemia<br />
2. Supportive Measures<br />
i) Monitoring: Temp, fluid balance, weight, hydration state, ABG<br />
ii) Temperature control<br />
- servo - controlled incubator is contraindicated as it will affect temperature<br />
recording.<br />
- maintain environment temp at top end or above the normal thermoneutral range.<br />
iii) Treatment of Shock - hypotension esp. in Gram-neg. septicaemia.<br />
- Keep MAP to around Gestation + 5 mmHg<br />
- May need to transfuse albumin or FFP (Albumin 25% give 4 ml/kg made up with<br />
NaCl to 20 ml/kg)<br />
- Start inotropes ( dopamine / dobutamine/adrenaline or noradrenalin) as indicated<br />
iv) Removal of central lines - Remove UAC or UVC in NEC or other abdominal sepsis.<br />
Also consider removal of UAC, UVC and peripherally –inserted central venous catheter if<br />
sepsis is not readily cleared<br />
v) If DIVC occurs<br />
- Check APTT, PT, Platelet count<br />
- treat with FFP/cryoprecipitate/platelet or blood transfusion as indicated<br />
Prevention<br />
The prevention of cross infections in the NNU is of utmost importance. The most<br />
effective preventive measure is hand washing. Other infection control measures e.g.<br />
aseptic techniques in patient procedures must also be strictly adhered to.<br />
References:<br />
N.R.C. Roberton. Textbook of <strong>Neonatology</strong>. Churchill Livingstone