Saving Newborn lives Initiative-aka Hala Project - Nipccd
Saving Newborn lives Initiative-aka Hala Project - Nipccd
Saving Newborn lives Initiative-aka Hala Project - Nipccd
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
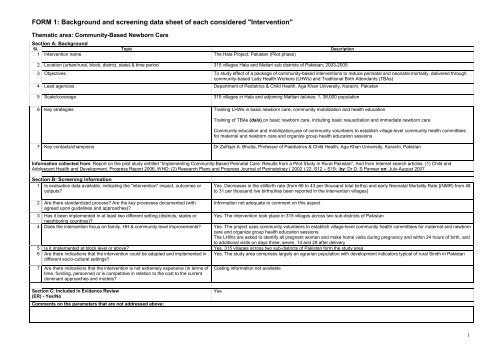
FORM 1: Background and screening data sheet of each considered "Intervention"<br />
Thematic area: Community-Based <strong>Newborn</strong> Care<br />
Section A: Background<br />
Sl. Topic Description<br />
1 Intervention name The <strong>Hala</strong> <strong>Project</strong>, Pakistan (Pilot phase)<br />
2 Location (urban/rural, block, district, state) & time period 315 villages <strong>Hala</strong> and Matiari sub districts of Pakistan; 2003-2005<br />
3 Objectives To study effect of a package of community-based interventions to reduce perinatal and neonatal mortality, delivered through<br />
community-based Lady Health Workers (LHWs) and Traditional Birth Attendants (TBAs)<br />
4 Lead agencies Department of Pediatrics & Child Health, Aga Khan University, Karachi, Pakistan<br />
5 Scale/coverage 315 villages in <strong>Hala</strong> and adjoining Mattiari talukas; 1, 38,000 population<br />
6 Key strategies Training LHWs in basic newborn care, community mobilization and health education<br />
Training of TBAs (dais) on basic newborn care, including basic resuscitation and immediate newborn care<br />
Community education and mobilization-use of community volunteers to establish village-level community health committees<br />
for maternal and newborn care and organize group health education sessions<br />
7 Key contacts/champions Dr Zulfiqar A. Bhutta, Professor of Paediatrics & Child Health, Aga Khan University, Karachi, Pakistan<br />
Information collected from: Report on the pilot study entitled “Implementing Community-Based Perinatal Care: Results from a Pilot Study in Rural Pakistan”; And from Internet search articles; (1) Child and<br />
Adolescent Health and Development. Progress Report 2006, WHO; (2) Research Plans and Progress Journal of Perinatology ( 2002 ) 22, S12 – S19; by: Dr D. S Panwar on: July-August 2007<br />
Section B: Screening information<br />
1 Is evaluation data available, indicating the "intervention" impact, outcomes or<br />
outputs?<br />
2 Are there standardized process? Are the key processes documented (with<br />
agreed upon guidelines and approaches)?<br />
Yes. Decreases in the stillbirth rate (from 66 to 43 per thousand total births) and early Neonatal Mortality Rate [(NMR) from 48<br />
to 31 per thousand live births)has been reported in the intervention villages]<br />
Information not adequate to comment on this aspect<br />
3 Has it been implemented in at least two different setting (districts, states or Yes. The intervention took place in 315 villages across two sub-districts of Pakistan<br />
neighboring countries)?<br />
4 Does the intervention focus on family, HH & community level improvements? Yes. The project uses community volunteers to establish village-level community health committees for maternal and newborn<br />
care and organize group health education sessions.<br />
The LHWs are asked to identify all pregnant women and make home visits during pregnancy and within 24 hours of birth, and<br />
to additional visits on days three, seven, 14 and 28 after delivery<br />
5 Is it implemented at block level or above? Yes. 315 villages across two sub-districts of Pakistan form the study area<br />
6 Are there indications that the intervention could be adapted and implemented in Yes. The study area comprises largely an agrarian population with development indicators typical of rural Sindh in Pakistan<br />
different socio-cultural settings?<br />
7 Are there indications that the intervention is not extremely expensive (in terms of<br />
time, funding, personnel) or is competitive in relation to the cost to the current<br />
dominant approaches and models?<br />
Section C: Included in Evidence Review<br />
(ER) - Yes/No<br />
Comments on the parameters that are not addressed above:<br />
Costing information not available<br />
Yes<br />
1
Form 2: Evidence Review for Community-Based <strong>Newborn</strong> Care<br />
Name of Intervention: <strong>Hala</strong> <strong>Project</strong> (Pilot phase), Pakistan<br />
Date of Review: August 2007<br />
1. Location and scale<br />
Number of villages by block, district and<br />
state names<br />
315 villages <strong>Hala</strong> and Matiari sub districts of<br />
Pakistan<br />
2. Agencies<br />
Lead agency(ies) Other key agencies<br />
(partners)<br />
Department of Pediatrics & London School of Tropical<br />
Child Health Aga Khan Medicine and Hygiene<br />
University, Karachi, Pakistan Govt. of Sindh<br />
2. Intervention Description<br />
Population covered Comments Time period<br />
138,600 2003-2005<br />
Implementing agencies Sponsor/donor Comments<br />
List Type (Govt./NGO/private) 1.World Health Organization<br />
1. Department of Health<br />
1. Government of Sind, Pakistan (WHO<br />
2.Aga Khan University<br />
2. Save the Children (funded<br />
by Bill and Melinda gates<br />
Foundation)<br />
Goal and Objectives Key strategies Key components/activities Primary target<br />
group<br />
Secondary target group<br />
Goal: To study effect of a package of 1.Training LHWs in home-based newborn care, 1. Household visits and health education by LHWs to mothers Pregnant Women of reproductive age,<br />
community-based interventions to community mobilization and health education<br />
during pregnancy and post-delivery (within 24 hours of birth mothers adolescent girls, community<br />
reduce perinatal and neonatal<br />
and days three,seven,14 and 28)<br />
elders and local political leaders<br />
mortality, delivered through<br />
2.Training of TBAs (dais)-on basic newborn care, 2. Delivery care by TBAs<br />
community-based Lady Health including basic resuscitation and immediate newborn 3. The community-based interventions included identification<br />
Workers (LHWs) and Traditional Birth care<br />
of community volunteers, formation of Community Health<br />
Attendants (TBAs)<br />
Committees (CHC), organizing emergency transport fund,<br />
3. Community education and mobilization-use of<br />
group education sessions by LHWs, and advocacy work<br />
community volunteers to establish village-level<br />
with community elders and local political leaders to promote<br />
community health committees for maternal and<br />
maternal and newborn care<br />
newborn care and organize group health education 4. Development of local Behavior Change Communication<br />
Information sources<br />
sessions<br />
(BCC) material including a two part video docudrama in<br />
local language (Sindhi)<br />
5. Training of LHWs and TBAs in intervention area<br />
6. Training in basic and intermediate newborn care to all public<br />
sector Rural Health Centre and hospital-based medical and<br />
nursing staff in intervention and control clusters<br />
Publication names Websites)/on-line Unpublished project documents Comments<br />
1. Child and Adolescent Health and Development; Progress Report 2006, WHO<br />
“Implementing Community-Based Perinatal<br />
Care: Results from a Pilot study in Rural<br />
2. Research Plans and Progress Journal of Perinatology ( 2002 ) 22, S12 – S19 SNL-<br />
Bangladesh Program Evaluation, Jan 2005, Save the Children<br />
Pakistan”<br />
2
5. Monitoring and Evaluation<br />
Methodology/design<br />
(adopted for program Monitoring and Evaluation data<br />
collection – summarize it from monitoring, baseline, special<br />
studies, midterm or final evaluation reports that you are<br />
referring)<br />
Eight clusters were randomly selected for the pilot study<br />
(which would guide the final effectiveness trial)<br />
A complete household and facility survey was conducted in<br />
these eight clusters from May - June 2003 to assess<br />
socio-economic characteristics and baseline perinatal and<br />
neonatal mortality rates<br />
All births and deaths in the preceding 12 month period were<br />
identified by recall<br />
Four of the eight clusters were chosen to receive the<br />
intervention. Choice was based on trying to ensure that the<br />
intervention and control clusters had similar distributions with<br />
respect to population size, number of births and neonatal<br />
deaths in the preceding 12 months, but did not use a formal<br />
randomization procedure<br />
In addition to the baseline survey in mid 2003, two<br />
cross-sectional surveys of all households were conducted by a<br />
separate census team at the midpoint (June-July 2004) and at<br />
the end of the pilot phase (August –September 2005) to collect<br />
data on births, deaths and care seeking patterns in the<br />
preceding 12 months<br />
Key measures/indicators Key lessons learnt<br />
1. % mothers who received tetanus toxoid during<br />
pregnancy<br />
2. % mothers who received antenatal check-up during<br />
last pregnancy<br />
3. % mothers who received maternal newborn health<br />
information during pregnancy<br />
4. % mothers who received domiciliary visit by LHW<br />
during the last pregnancy<br />
5. % mothers who procured clean delivery kit before<br />
delivery<br />
6. % mothers who delivered in a government health<br />
facility<br />
7. % deliveries with presence of LHW<br />
8. % of newborns received post-natal visit by LHW after<br />
birth<br />
9. % of newborns examined by LHWs within the first 48<br />
hours after birth<br />
10. % newborns with bathing delayed beyond six hours<br />
11. % mothers who fed colostrums to their babies<br />
12. % mothers who breastfed their infant within an hour<br />
of birth<br />
13. % mothers who breastfed their infant exclusively for<br />
first four months<br />
14. % mothers reported receiving support from the<br />
community health committee during pregnancy<br />
Community health workers can play a major role in delivering effective interventions for<br />
maternal and newborn care, and can do so in collaboration with both TBAs and skilled<br />
care providers<br />
Packages of evidence-based interventions can be delivered through community care and<br />
outreach strategies within the existing health system, and make a difference to newborn<br />
outcomes<br />
Dais and LHWs from the same community collaborated readily and community members<br />
(both males and females) were generally receptive to their messages and group sessions<br />
Community group counseling sessions may be a powerful, low-cost and effective means<br />
of reaching large numbers of women in rural settings and may also influence other<br />
community members<br />
Although the overall number of skilled attendants in the area did not change during the<br />
period 2003-5, the proportion of births attended by skilled attendants within the public<br />
sector facilities increased substantially in the intervention clusters indicating that<br />
community support strategies and demand creation affect care seeking<br />
behaviors and neonatal mortality<br />
The observed increase in skilled attendant utilization in these public health facilities<br />
underscores the importance of health system strengthening as a complement to<br />
community-based approaches<br />
Health staff retention was an issue. For example, of the 28 medical officers in the eight<br />
clusters trained in neonatal care and resuscitation, 19 (68%) were transferred out during<br />
the course of the pilot study, including the pediatrician in the district referral hospital.<br />
There were three different director generals of health in the area during the period<br />
2002-2005, placing a large burden on project staff with respect to communication and<br />
consensus building with health system managers and staff<br />
6. Program cost<br />
Total per year Estimated cost per component Estimated cost per beneficiary/unit Comments<br />
Information on cost not<br />
A full analysis of costs and cost-effectiveness<br />
available<br />
analysis is planned for the main trail currently<br />
being implemented in 16 clusters. Results<br />
should be available in late 2008<br />
3
FORM 3 - Data sheet for Effectiveness-Community-Based <strong>Newborn</strong> Care<br />
Name of Intervention: <strong>Hala</strong> <strong>Project</strong> (Pilot phase), Pakistan<br />
List of "impact" indicators with<br />
achievements<br />
Intervention clusters: Stillbirth rate<br />
reduced from 66 per 1000 births at<br />
baseline to 43 at endline (Mantel-<br />
Haenszel risk ratio = 0.66 (95% C.I. 0.53,<br />
0.83; P
Form 5 - Expandability Data<br />
Thematic Area: Community-Based <strong>Newborn</strong> Care<br />
Name of the Intervention: <strong>Hala</strong> <strong>Project</strong> (Pilot phase)<br />
Sl. Broad issues<br />
No<br />
1 Simplicity and clarity (is the<br />
intervention clear and simple, are<br />
the components clear and simple?<br />
could it possibly be simplified and<br />
still have results? does it take long<br />
to get results?)<br />
2 Key processes documented (are the<br />
key processes well documented?)<br />
Available information<br />
a) <strong>Project</strong> notes<br />
Yes. The intervention is clear focusing on delivery of a package of communitybased<br />
interventions to reduce neonatal mortality through community-based<br />
workers-Lady Health Workers (LHWs) and Traditional Birth Attendants (TBAS).<br />
The components of LHW training, dai training and community mobilization are<br />
clear. The dai training in less intensive than those tried out in other interventions.<br />
Focus is on community behaviors, community support strategies and demand<br />
creation<br />
b) Originator’s comments:<br />
a) <strong>Project</strong> notes: Available information not adequate to comment<br />
b) Originator’s comments:<br />
“Yes, we have process documentation for all the key processes throughout the life<br />
of the project, in which there are / were some periodic and some of them were<br />
regular.<br />
Training of HCP (HCFS including doctors, paramedics, LHVs, LHWs, TBAs). From<br />
all theses trainings we have the number of person’s trained at each facility, pre<br />
and post test results for all the trainings.<br />
Health system strengthening / information:<br />
New borns assessment by LHWs / CHWs by conducting visit on days 0,3,7,14 &<br />
28th day on monthly basis, Home base delivery, HCFs base delivery, Private<br />
HCFs base delivery, Skilled Birth Attendants ( SBAs) delivery, “NVDs”, sick<br />
newborns seen by LHW, sick newborns referred by LHW, sick newborns seeking<br />
care at HCFS, self referral, referred by LHW.<br />
HCFs MIS: on monthly basis were collected from the respective HCF of both<br />
intervention and control areas.<br />
Pregnant women registered, # of ANC visits, # of deliveries, delivery by SBAs,<br />
# of total births, newborn weighed, Low Birth Weight (LBW), still birth, maternal<br />
deaths, sick < one year.<br />
LHWs HMIS: on monthly basis (monthly LHW reports were also collected from<br />
both sides, pregnant women registered, ANC visits, delivery by SBAs, referred to<br />
HCF, newborn weighed, LBW, women examined within 24 Hrs of delivery,<br />
miscarriages, live births, still births, ENDs, LNDs, maternal deaths, referred
3 Feasibility for Govt. system to<br />
implement<br />
(could the Govt. system assimilate<br />
this intervention relatively easily,<br />
does it match well with current Govt.<br />
systems and capacities, does it<br />
require a minimum of new learning,<br />
new inputs, and change)<br />
4 “Dependencies” (what does the<br />
intervention’s success depend on?<br />
For eg. strong PRI/local self<br />
government institution, strong<br />
supervision system, lots of<br />
dedicated NGOs in the area, a<br />
charismatic leader. Does the<br />
intervention have a minimum and<br />
practical no. of dependencies?)<br />
a) <strong>Project</strong> notes<br />
The intervention utilizes the existing resources available within the Govt. health<br />
system and in the community. The training of Lady Health Workers (LHWs) was<br />
built –upon the standard training being provided under the LHW program in<br />
Pakistan (the LHW program is one of the flagship programs of the Govt. of<br />
Pakistan). In the intervention clusters, a total of six extra days were added to the<br />
standard curriculum to enhance the basic newborn care and community<br />
mobilization components. This is a feasible approach for scale up under the LHW<br />
program. The intervention shows that LHWs can deliver effective interventions for<br />
maternal and newborn care in collaboration with traditional births attendants,<br />
another resource existent in communities. The community mobilization<br />
components like selection of community volunteers, formation of CHCs, group<br />
education sessions, organization of emergency transport funds are additional<br />
activities for LHWs<br />
b) Originator’s comments:<br />
a) <strong>Project</strong> notes<br />
The project does not create a parallel infrastructure and attempts to deliver the<br />
interventions within the existing health system. Support of the Govt. is critical for<br />
expandability as it utilizes the LHWs for delivery of interventions. Community<br />
mobilization activities such as selection of community volunteers, formation of<br />
CHCs, group education sessions, organization of emergency transport funds<br />
require support dedicated LHWs willing to take additional workload. Since training<br />
of LHWS and TBAs is an important component, capacity to train staff and<br />
availability of resources for the same is a practical requirement<br />
b) Originator’s comments:<br />
6