Management of Dislocated PC IOL - KSOS
Management of Dislocated PC IOL - KSOS
Management of Dislocated PC IOL - KSOS
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
392 Kerala Journal <strong>of</strong> Ophthalmology Vol. XX, No. 4<br />
OPHTHALMIC<br />
S U R G E R Y<br />
<strong>Management</strong> <strong>of</strong> <strong>Dislocated</strong> <strong>PC</strong> <strong>IOL</strong><br />
Dr. Meena Chakrabarti MS, Dr. Valsa T. Stephen MS, Dr. Sonia Rani John DNB, Dr. Arup Chakrabarti MS<br />
Inadequate posterior capsular support or zonular<br />
rupture may allow <strong>IOL</strong> decentration or dislocation.<br />
Decentered <strong>IOL</strong>s may occur in 0.2 % to 1.2 % <strong>of</strong> cases<br />
postoperatively 1 . The specific cause <strong>of</strong> the displacement<br />
may not be always evident 1,2 .<br />
Various mechanisms include the following<br />
1. Inadequate posterior capsular support due to<br />
posterior capsular rent.<br />
2. Zonular rupture.<br />
3. Accidental placement <strong>of</strong> <strong>IOL</strong> through posterior<br />
capsular rent into the anterior vitreous face.<br />
4. Late haptic rotation out <strong>of</strong> a zone <strong>of</strong> thin capsular<br />
remnant.<br />
The cause <strong>of</strong> late spontaneous <strong>IOL</strong> rotation is<br />
unclear 3,4 . It may follow accidental changes in position,<br />
gravitational effect, accidental finger rubbing or other<br />
contact with the eye. Late dislocation <strong>of</strong> the <strong>IOL</strong> can<br />
occur spontaneously or following trauma.<br />
Generally posterior chamber <strong>IOL</strong> placement is safe if<br />
at least 180 degree <strong>of</strong> the capsular remnant is intact 5 .<br />
More extensive support is necessary if the capsular<br />
remnant is missing inferiorly or if the capsular margin<br />
on which the haptics are to be positioned is inadequate.<br />
Indications for subsequent surgery 3,4,5 : The<br />
indications for surgical removal include decreased<br />
visual acuity, chronic intraocular inflammation, retinal<br />
detachment and vitreous in the cataract wound<br />
associated with cystoid macular oedema. Although a<br />
Chakrabarti Eye Care Centre, Kochulloor, Trivandrum - 695 011,<br />
E-mail: tvm_meenarup@sancharnet.in<br />
dislocated <strong>IOL</strong> may be well tolerated for a considerable<br />
period <strong>of</strong> time by some patients, visual rehabilitation<br />
is usually difficult and surgical intervention may become<br />
necessary.<br />
Surgical Technique: For a subluxated <strong>IOL</strong> 6,7,8<br />
associated with symptoms, surgery may be performed<br />
by a limbal or parsplana approach. In patients with<br />
less extensive subluxation and posterior capsule that is<br />
intact for most <strong>of</strong> its part, repositioning can be done<br />
via the limbal route, after minimal or no anterior<br />
vitrectomy. However, in the presence <strong>of</strong> a sizeable<br />
posterior capsular rent, or posterior dislocation <strong>of</strong> the<br />
<strong>IOL</strong> into the vitreous cavity, a parsplana approach is<br />
prefered to acheive the goals <strong>of</strong> surgery 1 . A thorough<br />
preoperative assessment <strong>of</strong> the posterior capsular<br />
integrity is necessary to plan the surgical procedure.<br />
The first step <strong>of</strong> the procedure is to bring the dislocated<br />
<strong>IOL</strong> into the anterior vitreous in the plane <strong>of</strong> the pupil.<br />
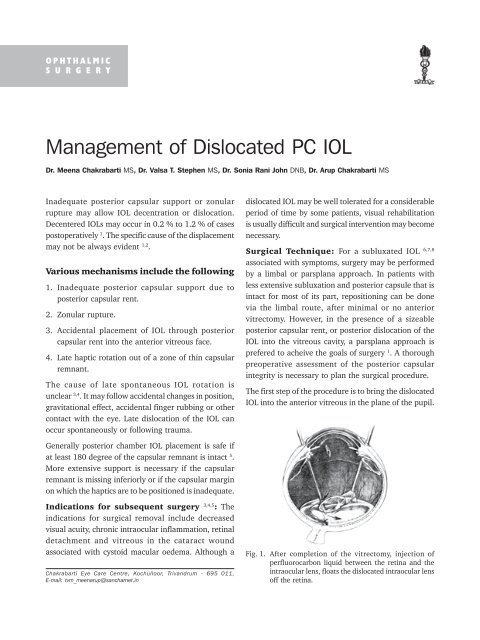
Fig. 1. After completion <strong>of</strong> the vitrectomy, injection <strong>of</strong><br />
perfluorocarbon liquid between the retina and the<br />
intraocular lens, floats the dislocated intraocular lens<br />
<strong>of</strong>f the retina.
December 2008 M. Chakrabarti et al. - <strong>Management</strong> <strong>of</strong> <strong>Dislocated</strong> <strong>PC</strong> <strong>IOL</strong> 393<br />
This is achieved after a complete vitrectomy and release<br />
<strong>of</strong> vitreous adhesions to the <strong>IOL</strong>. The <strong>IOL</strong> is then lifted<br />
<strong>of</strong>f the retinal surface using foreign body forceps or<br />
with the help <strong>of</strong> perflurocarbon liquids (fig 1).<br />
Late spontaneous in - the - bag intra ocular lens and<br />
capsular tension ring dislocation 9,10 has been reported<br />
in pseudoexfoliation syndrome. Capsular tension ring<br />
implantation in “pseudoexfoliation associated zonular<br />
weakness” does not guarantee long term zonular<br />
stability and capsular bag / <strong>IOL</strong> positions. In these<br />
patients, parsplana vitrectomy, perflurocarbon liquid<br />
injection to lift up the CTR-<strong>IOL</strong>-CB complex, grasping<br />
this complex with forceps and bringing it to the<br />
pupillary space transfer across pupil, and with a Mc<br />
Phersons forceps the complex can be explanted through<br />
the cornea scleral incision as a single unit.<br />
Alternatively after PFCL injection 11,12 , the vitrectomy<br />
cutter is used to cut the capsular bag after supporting<br />
it with an illuminated hook followed by removal <strong>of</strong> the<br />
CTR and <strong>IOL</strong> separately through a smaller scleral<br />
tunnel.<br />
Once the <strong>PC</strong> <strong>IOL</strong> is in the pupillary plane depending on<br />
the integrity <strong>of</strong> the capsulozonular remnant there are<br />
three options available to the surgeon. These<br />
include 1,2 ,<br />
1. <strong>IOL</strong> repositioning.<br />
2. <strong>IOL</strong> explanation<br />
3. <strong>IOL</strong> exchange.<br />
<strong>IOL</strong> Repositioning: is performed when adequate<br />
capsulo zonular support is present. The lens may be<br />
repositioned without sutures on to the residual posterior<br />
capsule or fixated by sutures to the iris or the sclera.<br />
Surgical success depends on accurate placement <strong>of</strong> the<br />
haptics into the ciliary sulcus and this requires<br />
visualization <strong>of</strong> the residual posterior capsule.<br />
In patients with insufficient pupillary dilatation iris<br />
hooks or retractors may be used to allow a more<br />
accurate assessment <strong>of</strong> the posterior capsule. Since<br />
the use <strong>of</strong> capsulorhexis has become wide spread,<br />
the peripheral anterior capsule is left intact and<br />
frequently serves as adequate support for the<br />
sulcus fixation <strong>of</strong> the dislocated <strong>PC</strong> <strong>IOL</strong>. Repositioning<br />
<strong>of</strong> a posterior chamber <strong>IOL</strong> into the anterior chamber<br />
has also been reported, but this approach is not<br />
recommended due to chronic chafing <strong>of</strong> the iris by<br />
the <strong>IOL</strong>.<br />
<strong>IOL</strong> removal and or exchange options 13 are<br />
usually exercised during surgery when the <strong>IOL</strong> has been<br />
damaged (e.g. broken haptic), when appropriate<br />
instrumentation to reposit the <strong>IOL</strong> is unavailable, or<br />
when highly flexible haptics make the <strong>IOL</strong> unsuitable<br />
for sulcus fixation. <strong>IOL</strong> exchange may sometimes be<br />
appropriate for plate haptic <strong>IOL</strong> which are slippery and<br />
difficult to grasp than PMMA lenses. Serrated or<br />
diamond dusted forceps are recommended when<br />
handling these <strong>IOL</strong>s. Repositioning may be particularly<br />
challenging with silicon plate haptic lenses because they<br />
are extremely floppy and difficult to manipulate. Also,<br />
since they are non expansible and sized for capsular<br />
fixation, centration with sulcus placement may be sub<br />
optimal because it requires a longer dimension.<br />
Implantation <strong>of</strong> a second <strong>IOL</strong> without removing the<br />
first <strong>IOL</strong> has been reported, but this approach is not<br />
generally recommended.<br />
In patients for whom repositioning <strong>of</strong> posterior chamber<br />
<strong>IOL</strong>s proves problematic, an intraoperative decision<br />
may be made to remove or replace the lens with an<br />
anterior chamber <strong>IOL</strong> or a scleral suture-fixated<br />
posterior chamber <strong>IOL</strong>. Exchanging for a scleral<br />
sutured- <strong>IOL</strong> has been simplified by new <strong>IOL</strong> designs<br />
that incorporate positioning holes at the point <strong>of</strong><br />
maximum haptic curvature. Alternatively, exchange for<br />
an anterior chamber <strong>IOL</strong> may be a faster, easier and<br />
less traumatic to the corneal endothelium 14,15,15,17 .<br />
Newer AC <strong>IOL</strong> designs avoid mechanical side effects<br />
that accompanied earlier designs.<br />
Scleral fixated <strong>PC</strong> <strong>IOL</strong>s are technically more complex<br />
than AC <strong>IOL</strong> implants. They carry a high risk <strong>of</strong> intra<br />
ocular hemorrhage because <strong>of</strong> penetration <strong>of</strong> the ciliary<br />
body. The major disadvantage <strong>of</strong> this technique is that<br />
it leaves a potentially permanent partial thickness fistula<br />
through the sclera, around the 10 0 prolene suture. This<br />
surgical technique requires a thorough anterior<br />
vitrectomy. <strong>IOL</strong> power calculation is difficult due to<br />
posteriorly placed optic <strong>of</strong> the <strong>IOL</strong>.<br />
It is important to verify the position <strong>of</strong> the scleral fixated<br />
<strong>IOL</strong> because 2 prolene sutures are its sole support and<br />
the position <strong>of</strong> the lens is the most important factor<br />
contributing to post-operative refraction. A one piece,
394 Kerala Journal <strong>of</strong> Ophthalmology Vol. XX, No. 4<br />
all PMMA, 10 0 vaulted, 13.5 mm haptic spread <strong>IOL</strong><br />
provides excellent optic centration and haptic<br />
stabilization, when the haptic positioning holes are<br />
placed at the point <strong>of</strong> greatest haptic spread and one<br />
trans-scleral suture pass per haptic is made. A scleral<br />
entry point 18,19,20 0.50 mm to 0.75 mm from the surgical<br />
limbus avoids the major arterial circle and the entire<br />
ciliary body and provides true ciliary sulcus placement<br />
<strong>of</strong> the <strong>IOL</strong>.<br />
Scleral fixation sutures 21,22,23 were first introduced for<br />
implantation <strong>of</strong> secondary <strong>IOL</strong>s from the limbal or<br />
parsplana approach or even for placement <strong>of</strong> a primary<br />
<strong>PC</strong> <strong>IOL</strong> in the absence <strong>of</strong> adequate capsulozonular<br />
support. Although a wide variety <strong>of</strong> techniques have<br />
been described, all have the following common<br />
objectives:-<br />
1. Proper suture attachments to the <strong>IOL</strong> haptic.<br />
2. Proper scleral sutures positioned to avoid<br />
torsion,decentration or damage to intraocular<br />
structures.<br />
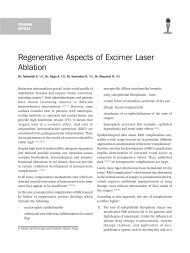
a b<br />
c d<br />
Fig. 2 a-d Technique for scleral suture fixation. (2a) Suture is<br />
threaded through a 27-guage straight needle with a<br />
hole in the bevel. Needle and suture are introduced<br />
into the vitreous cavity 1mm posterior to the limbus<br />
through the bed <strong>of</strong> a partial thickness scleral flap.<br />
Slack is created in the suture along the shaft <strong>of</strong> the<br />
needle by withdrawing it slightly. Under direct<br />
visualization the haptic is threaded through the loop<br />
along the shaft <strong>of</strong> the needle, using an intraocular<br />
forceps to grasp the optic. (2b) The needle is<br />
withdrawn, and the suture is tied under the scleral<br />
flap. (2c) Similar procedure is performed for the other<br />
haptic (2d). Side view <strong>of</strong> 2c.<br />
3. Proper scleral flap sutures to avoid externalization<br />
<strong>of</strong> the fixation sutures and reduce the risk <strong>of</strong><br />
endophthalmitis.<br />
In any scleral suture fixation procedures, the <strong>IOL</strong> is<br />
first retrieved, then a suture loop is introduced through<br />
the pars plana region into the vitreous cavity and<br />
around the <strong>IOL</strong> and the suture is firmly secured to the<br />
sclera. The technique that is commonly used for<br />
repositioning the dislocated <strong>PC</strong> <strong>IOL</strong> with scleral sutures<br />
in given below 24,25 (Fig. 2)<br />
<strong>IOL</strong> torsion and decentration can be avoided by accurate<br />
ciliary sulcus placement and adequate excision <strong>of</strong> bulky<br />
capsular remnant and cortical matter. Histopathological<br />
studies have shown little or no fibrosis around the<br />
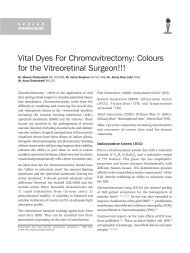
a b c<br />
d<br />
f g<br />
Fig. 3. 10-0 prolene suture on an STC6 plus (ethicon) needle.<br />
Is passed at 10’o clock, docked on a 30 guage needle<br />
at 4’o clock (a) and pulled out with the later diagonally<br />
(b). A Sinskey hook pulls out the suture from superior<br />
corneo-scleral section. The prolene suture is then tied<br />
to the <strong>PC</strong> <strong>IOL</strong> haptic(d). The <strong>PC</strong> <strong>IOL</strong> is then delivered<br />
into the posterior chamber with Mc Pherson<br />
forseps(e). The sutures are pulled at 4’o clock and<br />
10’o clock meridians (f). A single posterior scleral bite<br />
is taken and sutures are tied to themselves (g)<br />
e
December 2008 M. Chakrabarti et al. - <strong>Management</strong> <strong>of</strong> <strong>Dislocated</strong> <strong>PC</strong> <strong>IOL</strong> 395<br />
sutured <strong>PC</strong> <strong>IOL</strong> haptics. Therefore, a non dissolving<br />
suture material must be used since it provides the sole<br />
means <strong>of</strong> support at the ciliary sulcus 24 .<br />
Iris fixation sutures 25 requires passing a suture through<br />
the cornea, iris, around the <strong>IOL</strong> haptic and back through<br />
cornea and iris. Placement <strong>of</strong> the needle is not accurate<br />
making <strong>IOL</strong> centration a challenging task. Other<br />
disadvantage includes the increased risk <strong>of</strong> inviting a<br />
chronic iris mediated intra ocular inflammation 12 .<br />
Fig 3 a-g describes the technique <strong>of</strong> two point scleral<br />
fixator that we have been using for several years and it<br />
has given us predictable results 12,13 .<br />
Alternatively a 4 –point scleral fixation can be<br />
performed where the suture passage is made twice,<br />
ensuring adequate anchorage, centration and<br />
eliminating torsion.<br />
Boris Malyugin 26 et al described a technique for<br />
repositioning and trans scleral fixation <strong>of</strong> a dislocated<br />
plate – haptic foldable collamer posterior chamber<br />
intraocular lens. The displaced <strong>IOL</strong> was positioned in<br />
the anterior chamber, and a double armed suture or a<br />
curved needle was fixed to the sclera at 10.30 O’ clock<br />
position. The needle then entered the globe and passed<br />
through the superior haptic eyelet <strong>of</strong> the <strong>IOL</strong> and was<br />
withdrawn through the scleral wound on the opposite<br />
side. The inferior haptic was fixed at 4.30 and 7.30 o’<br />
clock and provided the mirror reflection <strong>of</strong> the suture<br />
path <strong>of</strong> the upper fixed haptic. This technique may be<br />
an useful alternative to lens removal and exchange.<br />
Richard H<strong>of</strong>fman 27 et al decribed a technique <strong>of</strong> scleral<br />
fixation without conjuctival dissection. The scleral<br />
tunnel technique for scleral fixation utilizes a scleral<br />
pocket initiated through a peripheral clear corneal<br />
incision. Full thickness passage <strong>of</strong> a doubled arm suture<br />
through scleral pocket and conjunctiva with subsequent<br />
retrieval <strong>of</strong> the suture ends through the external corneal<br />
incision for tying avoids the need for conjunctival<br />
dissection, and a sutured wound closure.<br />
A new technique that relies on glue 28 to implant <strong>IOL</strong>s<br />
in eyes that lack posterior capsular support was<br />
described by Agarwal et al. They used biological glue<br />
(a quick acting surgical fibrin sealant derived from<br />
human plasma with both hemostatic and adhesive<br />
properties) to perform scleral fixation in a case <strong>of</strong><br />
dislocated <strong>IOL</strong>. Using microrhexis forceps the haptic <strong>of</strong><br />
the PMMA non-foldable <strong>IOL</strong> is grasped and externalized<br />
under the previously prepared scleral flap. Fibrin glue<br />
is applied on the bed <strong>of</strong> the flap and the flap is closed<br />
in position. In the 12 eyes in their series there were no<br />
notable postoperative complications such as<br />
postoperative inflammation, hyphema, decentration,<br />
glaucoma or corneal oedema on regular follow up.<br />
However a long term follow up is necessary to validate<br />
the efficacy <strong>of</strong> the procedure.<br />
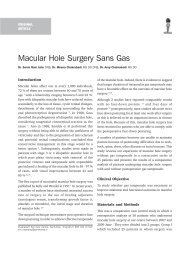
Surgical Results: The incidence <strong>of</strong> retinal<br />
detachment following vitrectomy for dislocated <strong>PC</strong> <strong>IOL</strong>s<br />
is given in Table 1. In recent series,approximately<br />
70 % <strong>of</strong> patients achieved a final visual acuity ³<br />
20/40. But surgical series are difficult to compare<br />
accurately due to nonhomogenicity <strong>of</strong> the variety <strong>of</strong><br />
management techniques used.<br />
Table 1. Results <strong>of</strong> PPV for <strong>Dislocated</strong> <strong>PC</strong> <strong>IOL</strong>s<br />
Study Total RD before RD after Cumulative<br />
(Year) patients PPV PPV<br />
1. Blodi et al 32 4 3 7<br />
(1992) (12.5 %) (9.3 %) (21.9 %)<br />
2. Scott 343 25 19 44<br />
(2003) (7.3 % ) (5.5 %) (12.8 %)<br />
3. Smiddy 100 4 4 8<br />
(2003) (4.0 %) (4.0 %) (8.0 %)<br />
References<br />
1. W. Smiddy; H. J. Flynn Managing lens fragments and<br />
dislocated posterior chamber lenses after Cataract<br />
Surgery. Focal Points: 1996<br />
2. William E Smiddy; Gonzalo V Ibanez; Eduardo Alfonso;<br />
Harry Flynn Surgical <strong>Management</strong> <strong>of</strong> dislocated<br />
<strong>IOL</strong>s.JCRS; Vol 21; Jan 1995, 64-69.<br />
3. Randy V Campo; Kelly D Chung; Ray T Oyakaura. Pars<br />
plana vitrectomy in the management <strong>of</strong> dislocated<br />
posterior chamber lenses. Am. J Ophthalmol; 108;<br />
529-534; Nov 1989<br />
4. Harry W Flynn Jr MD; Delyse Buus MD; William W<br />
Culbertson MD. <strong>Management</strong> <strong>of</strong> Subluxated and<br />
Posteriorly <strong>Dislocated</strong> <strong>IOL</strong>s using Pars plana Vitrectomy<br />
Instrumentation. JCRS; Vol 16, Jan 1990; 51-56<br />
5. Flynn H W Jr . Pars Plana Vitrectomy in the management<br />
<strong>of</strong> subluxated and posteriorly dislocated intra ocular<br />
lens. Graefes Arch Clin Exp Ophthalmol 225; 169; 1987<br />
6. Richard J Duffey; Edward J Holland et al. Anatomic<br />
Study <strong>of</strong> Transsclerally sutured intra ocular lens<br />
implantation.Am. J. Ophthalmol 108; 300-309, Sept<br />
1989.<br />
7. Michael Cahane MD; Varda Chen; Issac Avni.<br />
Dislocation <strong>of</strong> scleral fixated <strong>PC</strong> <strong>IOL</strong> after fixation suture<br />
removal . JCRS, Vol 20, March 1994.
396 Kerala Journal <strong>of</strong> Ophthalmology Vol. XX, No. 4<br />
8. Fransic W Price, Jr. MD, William E Withson MD. Visual<br />
results <strong>of</strong> suture fixated <strong>PC</strong><strong>IOL</strong>s during PKP. Oph 96,<br />
1989:1234-1240,<br />
9. F.Haken Oner, Nilufer Kocak, Osman Saatis. Dislocation<br />
<strong>of</strong> capsular bag with <strong>IOL</strong> and capsular tension ring. J.<br />
Cataract Refract Surg 2006; 32:1756-1758<br />
10. Schneidermann TE, Johnson MW et al. Surgical<br />
management <strong>of</strong> dislocated plate haptic <strong>IOL</strong>s. Am. J.<br />
Ophthalmol 1997;123:629-635<br />
11. William E Smiddy, Gonzalo V Ibanez, Edward Alfons,<br />
Haerry Hynn. Surgical management <strong>of</strong> <strong>Dislocated</strong> <strong>IOL</strong>s.<br />
JCRS.Vol 21, Jan 1995. 64-69.<br />
12. Hilel Lewis. MD; German Sanchez MD. The use <strong>of</strong> PFCL<br />
in the repositioning <strong>of</strong> posteriorly dislocated<br />
<strong>IOL</strong>s.Ophthalmol 1993; 100; 1055-1059.<br />
13. Randy .V. Campo, Kelly .D. Chung, Ray. T. Oyakawa. Pars<br />
Plana Vitrectomy in the management <strong>of</strong> posterior chamber<br />
lenses. Am.J.Ophthalmol 108, Nov 1989; 529-534.<br />
14. Edward .S. Lim, MD, David .J. Apple MD, Jolie C. Tsai<br />
MD et al. An analysis <strong>of</strong> Flexible Anterior Chamber<br />
lenses with special reference to the normalised rate <strong>of</strong><br />
lens explanation. Ophthalmol 1991, 98: 243-246<br />
15. Tarek.S.Hassen, Kaz Soong, Alan Sugar et al.<br />
Implantation <strong>of</strong> Kelman-Style open loop AC <strong>IOL</strong>s during<br />
Keratoplasty for aphakic and pseudophakic bullous<br />
keratopathy – A comparison with iris sutured posterior<br />
chamber lenses. Ophthalmol 1991,98:875-880<br />
16. Lawerence .E. Weene MD. Flexible open-loop AC <strong>IOL</strong><br />
implants. Ophthalmol 1993, 100, 1636-1639<br />
17. Jonathan .H. Lass, Deana .M. Desentis, Wiliam J.<br />
Reinhart. Clinical and morphometric results <strong>of</strong> PKP<br />
with one piece AC or suture fixted <strong>PC</strong><strong>IOL</strong>s in the<br />
absence <strong>of</strong> lens capsule. Arch. Ophthalmol 1990,108:<br />
1427-1430.<br />
18. Richard .J. Duffey, Edward .J, Holland et al. Anatomic<br />
study <strong>of</strong> trans sclerally sutured intraocular lens<br />
implantation. Am. J. Ophthalmol 108, Sept 1989:<br />
300-309<br />
19. Surendra Basti, P.C. Tejaswi et al. Outside – in<br />
Transscleral fixation for ciliary sulcus <strong>IOL</strong> placement.<br />
JCRS Vol 20, Jan 1994, 89-92.<br />
20. Anthony .J. Lubniewski MD, Edward J Holland MD,<br />
Woodford .S. Van Meter MD et al. Histological study <strong>of</strong><br />
Eye with Trans sclerally sutured posterior chamber <strong>IOL</strong>s.<br />
Am. J. Ophthalmol.110, Sept 1990:237-243<br />
21. Emigdio A Navia- Aray MD. A technique for knotting a<br />
suture around the loops <strong>of</strong> a dislocated <strong>IOL</strong> within the<br />
eye for fixation in the ciliary sulcus. Oph Surgery Oct<br />
1993, Vol 24, No:10 :702-707<br />
22. Steven .M. Bloom, Richard .E. Wyszynske Alexander<br />
.J. Brucker. Scleral fixation suture for dislocated <strong>PC</strong><strong>IOL</strong>S.<br />
Ophthalmic surgery Dec 1990, Vol 21, No:12<br />
23. Martin .S. Arkin, Roger F Stenert. Sutured posterior<br />
chamber intraocular lenses. J Cataract Refract Surg.<br />
Dec. 1991, Vol. 21.<br />
24. Kerry Solomon, MD, Joseoh .R. Gussler, Carter Gussler,<br />
Woodford S. Van Meter. Incidence and management <strong>of</strong><br />
complications <strong>of</strong> transsclerally sutured <strong>PC</strong><strong>IOL</strong>s.<br />
J.Cat.Refract Surgery Vol 19, July 1993; 488 -493<br />
25. S.Gregory Smith MD, Wilmengton Deluerare Frank<br />
Showden et al. Topographical anatomy <strong>of</strong> the ciliary<br />
sulcus. J. Cataract Refract Surg. Vol 13, Sept 1984:<br />
543 -547<br />
26. Boris Malyugin et al. Technique for respositioning and<br />
trans –scleral fixation <strong>of</strong> a dislocated plate haptic<br />
foldable posterior chamber intraocular lens. J.Cataract<br />
Refract Surg 2008<br />
27. Richard S H<strong>of</strong>fmann, Howard Fine et a .Scleral fixation<br />
without conjunctival dissection .J.Cataract Refract Surg<br />
2006;32:1907-1912<br />
28. Amar Agarwal et al. <strong>PC</strong><strong>IOL</strong> fixed by Fibrin glue. Ocular<br />
Surg News Europe/ Asia-Pacific Edition March 2008