Tools for Transforming Trauma - The Eleventh International Erickson ...
Tools for Transforming Trauma - The Eleventh International Erickson ...
Tools for Transforming Trauma - The Eleventh International Erickson ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
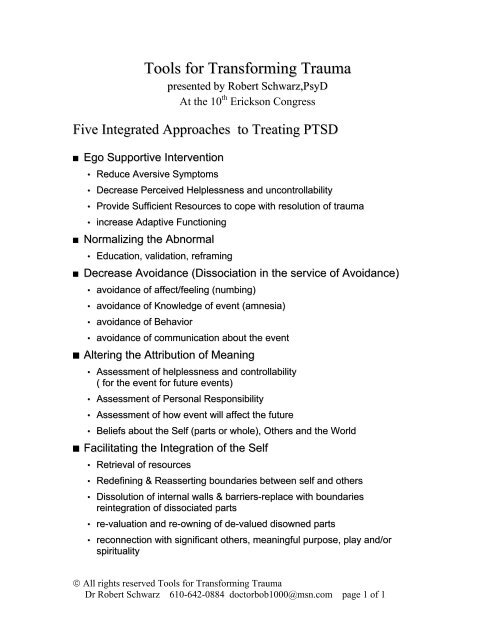
<strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
presented by Robert Schwarz,PsyD<br />
At the 10 th <strong>Erickson</strong> Congress<br />
Five Integrated Approaches to Treating PTSD<br />
Ego Supportive Intervention<br />
• Reduce Aversive Symptoms<br />
• Decrease Perceived Helplessness and uncontrollability<br />
• Provide Sufficient Resources to cope with resolution of trauma<br />
• increase Adaptive Functioning<br />
Normalizing the Abnormal<br />
• Education, validation, reframing<br />
Decrease Avoidance (Dissociation in the service of Avoidance)<br />
• avoidance of affect/feeling (numbing)<br />
• avoidance of Knowledge of event (amnesia)<br />
• avoidance of Behavior<br />
• avoidance of communication about the event<br />
Altering the Attribution of Meaning<br />
• Assessment of helplessness and controllability<br />
( <strong>for</strong> the event <strong>for</strong> future events)<br />
• Assessment of Personal Responsibility<br />
• Assessment of how event will affect the future<br />
• Beliefs about the Self (parts or whole), Others and the World<br />
Facilitating the Integration of the Self<br />
• Retrieval of resources<br />
• Redefining & Reasserting boundaries between self and others<br />
• Dissolution of internal walls & barriers-replace with boundaries<br />
reintegration of dissociated parts<br />
• re-valuation and re-owning of de-valued disowned parts<br />
• reconnection with significant others, meaningful purpose, play and/or<br />
spirituality<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 1 of 1
EXPERIENCE<br />
Degree of<br />
• Life Threat<br />
• Duration<br />
• Intensity<br />
• Natural<br />
vs. Man Made<br />
• etc.<br />
•<br />
Figure 1.1. Eco-systemic model of PTSD<br />
POST- TRAUMATIC<br />
COGNITIVE<br />
PROCESSING<br />
C Y B E R N E T I C D E V I A T I O N<br />
ENERGY-MERIDIAN<br />
NEURO-BIOLOGY<br />
CLASSICAL<br />
CONDITIONING<br />
RESPONDENT<br />
CONDITIONING<br />
APPRAISAL & MEANING<br />
View of Self & Others<br />
Actions & Intentions<br />
INDIVIDUAL<br />
CHARACTERISTICS<br />
• Pre-<strong>Trauma</strong> Personality<br />
• Coping Behaviors<br />
• Defensive Style, etc.<br />
RECOVERY<br />
ENVIRONMENT<br />
• Family Functioning<br />
• Social Supports<br />
• Societal Attitudes re: Events<br />
• Intactness of Community<br />
• Additional Stressors<br />
A M P L I F I C A T I O N C I R C U I T<br />
Affective<br />
Regulation<br />
vs.<br />
Dysregulation<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 2 of 2<br />
POSITIVE<br />
RESOLUTION<br />
Short Lived Symptoms<br />
Restabilization with<br />
• No residual effects<br />
• Coping with low<br />
residual effects<br />
ADAPTATION<br />
PATHOLOGICAL<br />
RESOLUTION<br />
PTSD based on<br />
1) Fear<br />
2) Dissociation<br />
3) Anger<br />
4) Withdrawal<br />
5) Embracing the <strong>Trauma</strong>
Basic Principles of Neo-<strong>Erickson</strong>ian Approach<br />
Principle 1: Social reality is constructed.<br />
Principle 2: Psychological experience is constructed and<br />
maintained in an ongoing moment-to-moment manner.<br />
Principle 3: Psychotherapy is based on changing at least one of the<br />
variables of constructed experience so that "felt experience"<br />
changes<br />
Principle 4: At the very least, patients should be treated with<br />
respect and dignity.<br />
Principle 5: It is the therapist's job to be:<br />
• as flexible as possible in identifying the variables that keep a<br />
patient locked into a problematic experience,<br />
• skilled in using tools that impact on those variables,<br />
• skilled at tracking the effects of their interventions, while<br />
• remembering to treat patients in a respectful dignifying manner<br />
e) hopeful that solutions and positive outcomes can be<br />
constructed <strong>for</strong> people who are suffering and<br />
• remaining humble about the "truths" of their own hypotheses and<br />
ideas about the people with whom they work<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 3 of 3
Well-Formed Outcomes<br />
<strong>The</strong> outcome must be stated in positive terms.<br />
A) <strong>The</strong> goal should be small.<br />
B) <strong>The</strong> goal should be seen as the beginning of<br />
something rather than the end of something.<br />
<strong>The</strong> outcome must be testable in sensory experience<br />
<strong>The</strong> outcome must be contextualized.<br />
<strong>The</strong> desired outcome must be initiated and maintained by the<br />
patient.<br />
<strong>The</strong> desired outcome must be ecologically sound.<br />
(In terms of trauma can not get rid of parts. Can not change when there are<br />
blocking beliefs around issues of safety and identity)<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 4 of 4
Herman<br />
(1992)<br />
Schwarz &<br />
Prout<br />
(1991)<br />
Van der<br />
Kolk,<br />
Mcfarlane<br />
and van<br />
der Hart<br />
(1997)<br />
Bloom<br />
(1997)<br />
Phillips &<br />
Frederick<br />
(1995)<br />
Phase oriented approaches to treating PTSD.<br />
Phase 1 Phase 2 Phase 3<br />
Developing Safety<br />
Ego support (including<br />
reducing aversive<br />
symptoms<br />
Normalizing the<br />
abnormal (usually with<br />
education),<br />
Education to help<br />
patients understand<br />
what is happening to<br />
them,<br />
Identification of feelings<br />
through talking,<br />
Developing the<br />
boundaries of a<br />
therapeutic milieu <strong>for</strong><br />
biological,<br />
psychological, social<br />
and moral safety<br />
Develop Safety &<br />
Stabilization<br />
Reconstruction of<br />
memories<br />
Decreasing avoidance (of<br />
affect, knowledge behavior)<br />
Decreasing perceived<br />
helplessness and providing<br />
resources to cope with<br />
traumatic memories),<br />
Altering negative or limiting<br />
attributions of meaning, and<br />
Identification of feelings<br />
through talking,<br />
Decreasing of avoidance<br />
through dissociation of<br />
memory,<br />
Restructuring-trauma related<br />
cognitive schemes.<br />
Reconstruction of memories.<br />
<strong>The</strong> use of inpatient setting<br />
to provide structure,<br />
diagnose and counteract<br />
trauma reenactment within<br />
the milieu.<br />
Stage II: access trauma<br />
material by alternating<br />
uncovering sessions with<br />
ego strengthening sessions.<br />
Stage III: resolving traumatic<br />
material<br />
Continued working through,<br />
processing and connecting<br />
dissociated BASK of<br />
memories to ongoing<br />
awareness<br />
Reprinted From: Schwarz, 2002 <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Reintegration of social<br />
connections<br />
Decreasing avoidance<br />
(interactions with others)<br />
Facilitating integration of<br />
the self.<br />
Facilitating connections<br />
with others<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 5 of 5<br />
Re-establishment of social<br />
connections and<br />
Accumulation of positive<br />
emotional experiences (i.e.<br />
stop avoiding the world and<br />
live a decent life)<br />
Reconnection through<br />
community spirit.<br />
<strong>The</strong> importance of play and<br />
lightheartedness<br />
Stage IV Integration and<br />
new Identity<br />
Integration of personality<br />
Integration of identity and<br />
future visions of the self.
<strong>The</strong>re is no dissociation.<br />
<strong>The</strong>re is only, to where are you associated?<br />
State A State B<br />
State A State B<br />
State A<br />
Normal Association/<br />
Dis-association<br />
<strong>Trauma</strong>tic Dissociation<br />
State B<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 6 of 6
Phase 1 Interventions<br />
Symbols of and Suggestions <strong>for</strong> Containment<br />
<strong>The</strong> concept of containment is part of boundary making. <strong>The</strong> general idea is <strong>for</strong><br />
the therapist and or the patient to pick a symbol of a container and then to put the<br />
dysphoric feeling in the container and seal it up <strong>for</strong> some prescribed amount of<br />
time or until certain conditions are in place.<br />
Symbols <strong>for</strong> Containers include: Chests, Bottles, Boxes, Caves, Safes, bomb<br />
shelters.<br />
<strong>The</strong> goals of containment<br />
1) When goal is to help re-ground the patient because the patient is experiencing<br />
intense overwhelming affect or memories and appears to have no way to contain it.<br />
2) When goal is to decrease acting out because, the patient is self-harming or<br />
acting out as a response to intense affect or memories.<br />
3) When the goal is prepare the patient <strong>for</strong> more intense work ahead of time by<br />
teaching them this tool.<br />
4) When goal is to temporarily remove one affect or SoC to uncover an<br />
underlying affect or SoC. For instance the patient uses one affect (usually in the<br />
anger/rage dimension) to deny and defend against pain and hurt.<br />
“Do you see that chest there in your mind? <strong>The</strong> one with the big<br />
heavy lid. (Usually the patient will answer yes.) Good. I want you to open<br />
up the lid. Let me know when you have done that....Now I want you to put<br />
those memories/feelings, etc. in the chest, so they will not overwhelm you<br />
right now. We will come back to them at a later time. Right now it is more<br />
important <strong>for</strong> you to feel grounded. Once all of those memories are in the<br />
chest close the lid.”<br />
In using this tool the therapist needs to convey the confidence that it will<br />
work. <strong>The</strong> best attitude <strong>for</strong> the therapist to have is presupposition that this will<br />
help. It is not so much that you say this out loud to the patient. It is more of an<br />
internal expectation. Just like you expect the sun to come up in the morning, the<br />
patient will get relief by putting the difficult experience in the container.<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 7 of 7
Variations<br />
1) Magic pool of water that absorbs the “negative energy” “Negative<br />
feelings” of memories or experiences. Think of the pool in the movie<br />
“Cocoon”. Can also restore positive feelings<br />
2) Windows ( as in computer) file transfer imagery where the files of the<br />
negative experiences are transferred into a container but the negative<br />
energy is removed as part of the transfer process<br />
3) Create rooms in the house. Each part can have own room with<br />
whatever makes the part happy such as stuffed animals.<br />
4) Safe deposit boxes in a vault. Each part gets his or her own safe<br />
deposit box<br />
5) Slow leak version: Any container that has a slow leak that allows small<br />
bits of the affect to come up that is within the person’s ability to<br />
tolerate.<br />
Creating a Safe Space<br />
Images of lack of danger<br />
Low Sympathetic Arousal<br />
Deep Diaphragmatic Breathing<br />
Associations of com<strong>for</strong>t, relaxation, safety<br />
<strong>The</strong> problem solving list<br />
Identify where acting out/self harm is on the sequential list of strategies to reduce<br />
negative affect (Almost always in the top 5 if not top 3)<br />
Expand list to10 to 20 steps an place acting out at bottom of list (do not get rid of it)<br />
Fill inn other steps with small strategies<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 8 of 8
Sub-Modalities to Reduce Affect Intensity<br />
Size: Bigger is usually stronger, more powerful more important. Smaller is associated with less<br />
powerful and less important. To reduce power and importance of an image, shrink size of an<br />
entire image; change the relative size of the client vs. some other person so that the client is<br />
equal or bigger than the other person<br />
Distance: Closer is usually more immediate & intense. Further away is less immediate and<br />
intense. Move pictures or sounds further away to reduce affect.<br />
Location: In front and to the right tends to be happening now or in future-in back & to the left<br />
tends to be the past. To put things in the past move them behind or to the left of the person as if<br />
fading away.<br />
Color: Color is more affect. Black and white is less affect. Muted tones tend to mute intensity.<br />
People can have fun playing with different color palettes.<br />
Associated/Dis-associated: Associated means the person is in the experience, which will<br />
increase affect and intensity. This is the position of looking out of one’s own eyes. Dis-<br />
associated means meta to the experience, which decreases affect & intensity. This position is<br />
watching oneself as if in a movie.<br />
Tunnel Vision (TV)/ Peripheral Vision (PV): TV is associated with loss of boundaries &<br />
increased intensity. PV is associated with good boundaries and having perspective and less<br />
intensity.<br />
Loudness: Louder is stronger and more intense. Softer is the opposite<br />
Pitch/Tone: Much in<strong>for</strong>mation is carried in voice tone. Low & deep tone usually means more<br />
intensity and power. High tone with squeaky pitch is less powerful. Change internal voices to<br />
sound as if they have inhaled helium to reduce their power and fearfulness.<br />
______________________________________________________________<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 9 of 9
Phase 2 Interventions<br />
<strong>Trauma</strong>tized<br />
From “Either Or” to “Both And” to<br />
“More and Less”<br />
key<br />
= trauma<br />
= Resources<br />
Both<br />
And<br />
Either<br />
Or<br />
© 1992 Robert A Schwarz, PsyD / I.A.C.T. / PO Box326 / Villanova/ Pa / 19085 / 800-637-1434<br />
www.solutionmind.com E:Mail IACTinc@Aol.com<br />
Increasing resources<br />
Decreasing <strong>Trauma</strong><br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 10 of 10<br />
More<br />
and<br />
Less<br />
Dissociative<br />
Amnesia<br />
Moving On
“Yes And” Imagery<br />
<strong>The</strong> goal is to provide the experience of being aware of traumatic material AND<br />
at the same time stay connected with positive resources.<br />
1. Have the person get in touch with (make an associated image) of a<br />
resource.<br />
2. Build up the positive feelings and associations.<br />
3. Put that image in a ball in mental space.<br />
4. Repeat with 4-6 additional resources<br />
5. Put the traumatic memory in another ball in space<br />
6. Have he client Stay aware of everything.<br />
Teacher<br />
Friend<br />
Mastery<br />
Event<br />
Music<br />
Pet<br />
Nature<br />
trauma<br />
Safety<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 11 of 11
Trigger<br />
Trigger<br />
Sample <strong>Trauma</strong> Molecule<br />
visual memory<br />
of trauma<br />
(associated) hightened<br />
arousal<br />
Feelings<br />
of Shame<br />
& Fear<br />
appraisal<br />
of danger<br />
neg. self<br />
talk<br />
© 1994 Robert A Schwarz, PsyD / I.A.C.T. / PO Box326 / Villanova/ Pa / 19085 / 610-525-4626 Fax 610-525-4864<br />
E-Mail IACTinc@AOL.com Copying is permissable<br />
Reconditioned <strong>Trauma</strong> Molecule<br />
hightened<br />
arousal<br />
feelings of<br />
belonging &<br />
empathy<br />
Appraisal<br />
of relative<br />
safety<br />
visual image of<br />
self sitting with<br />
therapist in<br />
com<strong>for</strong>t<br />
neutral<br />
self-talk<br />
visual memory<br />
of trauma<br />
(dis-associated)<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 12 of 12<br />
INCREASED<br />
TRAUMA<br />
MASTERY<br />
© 1994 Robert A Schwarz, PsyD / I.A.C.T. / I.A.C.T. / PO Box326 / Villanova/ Pa / 19085 / 610-525-4626 Fax<br />
610-525-4864 E-Mail IACTinc@AOL.com Copying is permissable
<strong>Trauma</strong> Reassociative Conditioning<br />
Step-By-Step Instructions <strong>for</strong> TRC and Commentary<br />
(A complete example of using TRC with a Vietnam vet is included on the DVD that comes with<br />
this book)<br />
1) Educate the patient about the rationale <strong>for</strong> the procedure. It is particularly important to<br />
make sure the patient understands that he is not suppose to feel the traumatic feelings as though<br />
he were back in the trauma, with the exception of the next step. He is to feel the resourceful<br />
feelings that you will be helping them to feel.<br />
2) Calibrate the <strong>Trauma</strong> SoC. Have the patient think of the traumatic experience. <strong>The</strong> patient<br />
needs to pick a discrete trauma that has a beginning and an end.<br />
Explain to him that it will only be long enough so that you can see what they look like, if he starts<br />
to relive the trauma. <strong>The</strong>n look <strong>for</strong> minimal cues of the trauma SoC. <strong>The</strong> therapist can watch <strong>for</strong><br />
changes in breathing. Usually the face gives away many clues. Changes in muscle tone,<br />
grimaces, changes in skin color. <strong>The</strong> important point is that the therapist discovers some nonverbal,<br />
early warning sign that the patient is entering the traumatic SoC, so that later on, the<br />
therapist can stop that from happening.<br />
As soon as you notice the smallest sign of trauma, have the patient stop thinking about it and get<br />
out of the trauma SoC. If necessary, have him get up move around, change the subject. Talk<br />
about the weather.<br />
3a) Elicit a description of a resourceful state that the patient needs now so that dealing with<br />
the memory of the trauma would not be traumatic<br />
Resources used in this context tend to be described in one of two ways: feelings or<br />
complex evaluations. <strong>The</strong>y include: safety, strength, joy, feeling loved, knowing it is not my fault,<br />
knowing I will live/survive. It is important to recognize that whatever verbal description given to<br />
the resource, it is a complex SoC with both affective and cognitive components<br />
This step is in itself a process of negotiation. It involves clinical acumen. A patient’s first<br />
choice at a resource is often insufficient. It is up to the therapist to help make sure the patient has<br />
picked an adequate resource. <strong>The</strong> patient should become increasingly involved with the ideas<br />
we are discussing. <strong>The</strong> discussion will become compelling to the patient.<br />
If these things are not happening that is feedback to me that we are not heading in the correct<br />
direction. At the end of this process, which can take up to fifteen or twenty minutes (although five<br />
to ten is often enough), the patient will have identified a resource by some label or name.<br />
3b Elicit the Resource SoC. Have the patient think of a time he had this resource and imagine<br />
himself fully associated to that time so it is as if he is living it. Invite the patient to make it as vivid<br />
as possible. Ideally, it would be like a vivid positive flashback. Have the patient focus on what he<br />
sees and hears and feels. <strong>The</strong>rapists that know hypnosis can use their training to help make the<br />
experience as vivid as possible.<br />
Ask the patient to let you know when he is as fully involved in the experience as he can<br />
get. <strong>The</strong>n ask the patient to tell you what he calls this experience.<br />
3c) Create Anchors to Stabilize the Resource State. Repeat the patient’s label back to them in<br />
the same tone of voice that he used while the patient is in the positive experience. This creates<br />
an associative “anchor or “cue”. <strong>The</strong>n tell the patient that you want him to create his own “<br />
positive button” to help bring back the state. Tell the patient to make a button using his hands. It<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 13 of 13
could be a squeeze of the wrist, a fist, or an OK sign. Whatever he would like to create. Make<br />
sure the patient is still strongly in the positive state. Have the patient make the “positive button”.<br />
You can also repeat the auditory label that they created.<br />
4) Have the patient establish a doubly dissociated point of view.<br />
Specifically, have patient imagine himself sitting in a movie theater. It should not be a very good<br />
movie theater, other than very com<strong>for</strong>table seats. It is small screen and poor sound. <strong>The</strong> person<br />
should imagine that he and you are sitting about two thirds of the way back. Ask the patient to<br />
tell you once he has this in mind. <strong>The</strong>n have the patient imagine himself floating up to the<br />
projection booth or off to the side even further back so that he can see you and him sitting<br />
together watching the blank screen. This double dissociation allows <strong>for</strong> a great deal of safety. It<br />
is also symbolic of creating an observing self that can see the patient in a therapeutic relationship<br />
with the therapist. You can also establish an anchor <strong>for</strong> this state by tapping on a table or<br />
snapping your fingers.<br />
5) Re-Condition the SoC’s linked to the trauma. At this point the patient is now up in the<br />
projection booth watching himself sitting with you com<strong>for</strong>tably. He should also be feeling the<br />
resourceful state of mind both in the booth and in the chair. <strong>The</strong> goal is to hold these states<br />
constant while the patient reviews the trauma. <strong>The</strong> patient is instructed to keep the resource SoC<br />
constant while he watches the trauma from beginning until he gets to the point after the traumatic<br />
event is over. <strong>The</strong> patient is told to use his “positive button” to strengthen the resource whenever<br />
he needs to. <strong>The</strong> patient can be told that he can watch the movie at a very fast speed if he<br />
wants. He can watch the movie more than once if he needs to. <strong>The</strong> suggestion is given that<br />
somehow the patient will know when he is finished. While the movie is running the therapist<br />
must rein<strong>for</strong>ce the positive SoC with verbal suggestion. <strong>The</strong> therapist wants to keep the patient<br />
associated to the resource SoC, in the current year, to the current aged self. To do this the<br />
following language is used:<br />
"as you continue up in the projection booth feeling "resource label" watching you and me sitting<br />
here feeling "resource label" in 2005 ( current year) watching what the younger you went through<br />
back then..."<br />
While the patient watches the movie the therapist can suggest that he may notice<br />
something different that he had not realized be<strong>for</strong>e, or he may have a new perspective on what<br />
happened since He is reviewing this event in this new way. It can be helpful to underscore that<br />
this may be the first time that he has been able to acknowledge the trauma without being in it.<br />
It is imperative that the therapist keeps watching the patient <strong>for</strong> signs of trouble<br />
and not allow him to fall back into the traumatic feelings/experiences. If at any time the<br />
patient starts to develop the traumatic experience, rein<strong>for</strong>ce the dissociation or resource anchor.<br />
If that does not work, use sub-modalities to reduce the affect by making the movie farther away or<br />
smaller or black and white. Sometimes it is enough to just remind the patient not to associate<br />
into the movie. If this does not work stop the treatment. You will need to go back to the drawing<br />
boards. See the following section on trouble shooting TRC.<br />
6) Re-valuing the self: When patient finishes watching the old experience (he may need to<br />
watch more than one time- This is a matter of clinical acumen and the patient's own desires) -<br />
Release the dissociation cue and instruct patient to float back to his or her body. Have patient<br />
from the here and now resourceful position look at younger self at the end of the trauma. Have<br />
the patient walk down to the movie screen. Ask the patient to do one of the following things:<br />
either a) step into the picture or b) bring the younger self off the screen, or c) just talk to the<br />
younger self on the screen.<br />
Instruct the patient to tell the younger self whatever, "he needs <strong>for</strong> healing". In some<br />
cases the patient can be left completely on their own to say what they need to say to himself. It is<br />
often helpful to offer some possible things to say. <strong>The</strong>se can include: a) the patient is from the<br />
future and is living proof that the younger person survived, b) that he made the best choice<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 14 of 14
available to him at the time c) <strong>The</strong> patient loves the younger self. <strong>The</strong>se ideas should be offered<br />
in a tentative way. <strong>The</strong> patient should be given enough time and silence to do their own work.<br />
During this part of the treatment the patient often has gentle tears of acceptance and love.<br />
7) Re-integration. Once the patient is finished, have patient bring the younger self off the<br />
screen and sit back down in the chair with the here and now self. Instruct the patient to imagine<br />
bringing the younger part inside the patient. <strong>The</strong> patient is then instructed to open his eyes and<br />
be fully present in the therapy room.<br />
Once the patient is finished there are several options that the therapist can take. <strong>The</strong> first<br />
is to test the work by having the patient think of the original old trauma and discover how much<br />
the affect and experience has changed. <strong>The</strong> goal is that the patient should look visibly more<br />
com<strong>for</strong>table and should report feeling and thinking differently about the traumatic event. When<br />
asking the patient to do this it is important to make sure that the problem is appropriately put into<br />
the past. <strong>The</strong> therapist can say, “I would like you to think of the scene that use to be so<br />
problematic <strong>for</strong> you.” Or, the therapist can say, I’d like you to think of the old problem. It would<br />
be a mistake to say, “ I’d like you to think of the problem that gives you so much trouble.” This<br />
last sentence uses the present tense and is verbally re-associating the problem SoC to the<br />
present.<br />
If the patient often had symptoms in certain contexts (e.g. every time they had to talk with<br />
their boss) an additional strategy would be to have the patient imagine a time in future where the<br />
old symptoms would have come up to see if the patient feels more com<strong>for</strong>table. <strong>The</strong> patient<br />
should report that he feels a significant improvement over what he usually feels when he<br />
anticipates the context.<br />
Troubleshooting the trauma Re-associative Conditioning process.<br />
Problem 1) During the watching of the movie the patient starts to lose his resourcefulness<br />
and collapses in to the traumatic event<br />
a) Make sure that the therapist is using dissociative language that keeps the patient in<br />
the present and the trauma in the past. For instance if the therapist says, “watch the movie of the<br />
traumatic event happening”. <strong>The</strong> use of the present tense “happening” could collapse the<br />
separation of the patient from what “happened”. Make sure to emphasize the difference between<br />
the resourceful patient in the current year from the younger self in the past.<br />
b) Make sure that the patient’s image of himself in the chair next to the therapist is an<br />
adult version of the self. In some cases patients have put a child version of themselves next to<br />
the therapist, which collapses the distinction between time and place.<br />
c) Re-instruct the patient that you do not want them to feel what happened back then.<br />
Sometimes, patients just do not understand the instructions. This can happen if they have had<br />
previous therapy experience that emphasized catharsis.<br />
d) Use sub-modalities to reduce intensity. Make the picture black & white, move it away<br />
and/or make it smaller. Add peripheral vision.<br />
e) Have patient use their “positive button” to strengthen positive state. Increase the<br />
verbalization of the auditory label of the positive feeling as well as the dissociative language.<br />
f) If all else fails, stop the process. Go back to the resource negotiation phase and either<br />
pick a different resource and/or strengthen the resource by finding additional examples of it and<br />
pairing those examples to the same anchors. (In NLP this is referred to as “stacking anchors”)<br />
Problem 2) <strong>The</strong> patient starts to cry while watching the movie. Usually, this is not really a<br />
problem. If the patient is empathically crying ABOUT what happened to that younger person in<br />
the past, then the process is working well. Simply tell the patient that these empathic feelings are<br />
OK as long as they are the feellings of the adult self about what happened to the younger self<br />
(Notice the continued use of the language that separates time and place) and make sure that he<br />
is still in contact with the resourceful SoC as well.<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 15 of 15
Figure 7.1 <strong>The</strong> Process of the Holistic Self<br />
Create Create stories stories of of<br />
understanding<br />
understanding<br />
& & <strong>for</strong>giveness <strong>for</strong>giveness<br />
Identify Identify & & modulate modulate<br />
social social pressures pressures<br />
Accept<br />
painful<br />
feelings<br />
Phase 3 Interventions<br />
Acknowledge<br />
Acknowledge<br />
dysfunctional<br />
dysfunctional<br />
behaviors behaviors &&<br />
beliefs beliefs<br />
Choose healthy<br />
actions even if<br />
difficult<br />
Accept<br />
“That what is”<br />
& “That<br />
what was”<br />
Create Create stories stories<br />
of of mastery mastery<br />
Access Access &&<br />
Strengthen Strengthen<br />
resources resources<br />
Engage Engage<br />
support support<br />
from from others others<br />
“Get A Life” <strong>The</strong>rapy<br />
1) Do at least one thing on a regular basis that connects you with your best self<br />
or fills you with joy.<br />
2) Do something that makes your body feel good on a regular basis.<br />
3) Pay attention to, privilege and be grateful <strong>for</strong> positive events (especially small<br />
things) every day<br />
4) Eat well (not lots)<br />
5) Spend time in nature<br />
6) Regularly do small acts of self care<br />
7) Regularly connect in positive ways ( especially giving love) with family,<br />
children, friends or others.<br />
8) Connect with mentors (can be family, friends, characters)<br />
9) Take regular stock of / Give credit <strong>for</strong> what is going better; what you are<br />
doing well<br />
10) Develop a spiritual practice<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 16 of 16
1<br />
Figure 8.3. Solution-oriented checklist <strong>for</strong><br />
therapist development.<br />
Below are 34 behavior patterns that, as a therapist, you may or may not do when treating clients who are recovering from trauma.<br />
Please rate the occurrence of each item according to the following 0 to 10 scale where 10 = 100% of the time when it is appropriate,<br />
5 = 50% of the time when appropriate, 0= not at all. If you are not sure, just put what feels accurate at this point in time.<br />
Date__________________<br />
0-10 0 -10<br />
Able to notice small positive changes even though no large ones 19<br />
Can talk with client about the consequences of dysfunctional<br />
coping skills without labeling<br />
2 Looks <strong>for</strong> strengths and resources of client 20 Can give direction and structure to client<br />
3 Can help client focus on angry feelings 21 Able to feel com<strong>for</strong>table while feeling angry at abusers<br />
4 Can help client focus on sad feelings 22 Able to feel com<strong>for</strong>table while being asked to solve ambiguity<br />
5 Can help client focus on fearful feelings 23 Able to reflect ambiguity back toward client<br />
6 Can help client focus on spiritual feelings 24<br />
Able to feel com<strong>for</strong>table dealing with angry/hurtful aspects of<br />
client<br />
7 Can help client focus on joyful feelings 25 Able to feel com<strong>for</strong>table dealing with childlike aspects of client<br />
8 Can recognize a negative interactional pattern 26 Tolerates constructive criticism from client well.<br />
9 Can do something different to change a negative interactional pattern 27 Accepts praise from client well.<br />
10 Shows sense of humor when appropriate. 28 Believes that the client can live a “good enough” life<br />
11 Can feel “OK” even when client is doing poorly 29 Able to construct positive motivations <strong>for</strong> symptoms<br />
12 Gives client Praise <strong>for</strong> taking small steps 30 Acknowledges pain and weaknesses of client<br />
13 Can acknowledge that “I” made a mistake 31 Can suspend judgment<br />
14 Can apologize to the client <strong>for</strong> that mistake 32 Can be <strong>for</strong>giving of client’s actions and/or problems<br />
15 Able to listen to details of abuse & remain centered & present 33 Can be <strong>for</strong>giving of abuser<br />
16 Able to be com<strong>for</strong>table while feeling sad or crying with client<br />
17 Able to feel com<strong>for</strong>table while feeling angry with client Other<br />
18 Can set limits well Other<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 17 of 17<br />
34<br />
Can be <strong>for</strong>giving of yourself when you make mistakes (as a<br />
therapist or in your life)
No <br />
Yes <br />
No <br />
Yes <br />
Figure 8.2 A solution-oriented decision tree model<br />
<strong>for</strong> correcting problems in treatment.<br />
Can you identify when things have gone well (a solution pattern)?<br />
(Spend some time on this. You should be able to come up with<br />
something. If not you have waited far too long to use this approach.)<br />
Can you identify the problem pattern?<br />
Can you imagine the relationship from patient’s point of view?<br />
(Do aligning perceptual positions yourself. (See chapter 7. <strong>The</strong> other<br />
is the patient.)<br />
Does this point of view give you new in<strong>for</strong>mation about the patient and<br />
how your actions are problematic to the patient?<br />
Have you consulted with the patient about either when things have<br />
gone well/ better or about the problem and asked <strong>for</strong> his/her input or<br />
advice?<br />
Yes <br />
No <br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 18 of 18<br />
Do more of that. Go to last<br />
step<br />
Consultation with patient or<br />
others<br />
Yes Go to <br />
No Do it. <strong>The</strong>n go down 1 step<br />
Yes Have you followed the patient’s input or advice No Try their advice<br />
Yes Go to<br />
END<br />
Was it helpful? No Go to next step<br />
Yes Has the patient’s advice given you new in<strong>for</strong>mation? No Consultation<br />
Yes <br />
Yes <br />
With this In<strong>for</strong>mation, can you imagine what a solution would look<br />
and sound like and feel like?<br />
What steps can you take to make that happen?<br />
What would support you taking those steps?<br />
No <br />
Yes Put steps into action. Do they make a difference? No <br />
END<br />
Do more of those things. Reflect with self and/or patient about the<br />
impact and meaning of those changes. What needs to happen to<br />
make you more consistent or more flexible?<br />
Consultation<br />
New skill development<br />
None Consultation<br />
Do something different, go<br />
back to previous steps or<br />
get consultation
. Chart of tools, their goals, approximate timing by phase of treatment, and location by chapter.<br />
Stage of<br />
therapy<br />
Chap.<br />
Reduce<br />
affect<br />
Improve<br />
cognitive<br />
processing<br />
Improve<br />
grounding<br />
Identify<br />
traumatic<br />
memories<br />
Process<br />
traumatic<br />
memories<br />
Boundaries<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 19 of 19<br />
Increase<br />
selfefficacy<br />
Safe Place First 4 () <br />
Breathing First 4 <br />
Increase<br />
resources<br />
Problems Solving<br />
Check List<br />
First 4 <br />
Rainy Day Letter 4 () ()<br />
Sub-Modalities First, second 4 () <br />
Increase<br />
positive<br />
self-<br />
Image<br />
Containment<br />
symbols<br />
First 4 () <br />
54321 First 4 <br />
Peripheral vision<br />
Energy Bubble<br />
End state retraining<br />
Somatic/ affect<br />
bridge<br />
Ideomotor<br />
questioning<br />
T RC<br />
Safe<br />
remembering<br />
Hypnotic<br />
abreaction<br />
Creating<br />
alternative<br />
memories<br />
First<br />
(second)<br />
First<br />
(second)<br />
4 () <br />
4 () <br />
First -second 4 <br />
Second(first<br />
or third)<br />
5 () <br />
Decrease<br />
self<br />
destructive<br />
behaviors<br />
Second 5 ()<br />
Second<br />
(first or third)<br />
5 ()<br />
Second 5 <br />
Second 5 ()<br />
Second<br />
(third)<br />
5 ()<br />
Yes and Second third 5 () <br />
Thought field<br />
therapy<br />
Current problem<br />
as chance to<br />
correct the past<br />
Cultivating<br />
resources<br />
(external)<br />
All 6 ()<br />
Second<br />
(first or third)<br />
Second-third<br />
(but sooner<br />
the better)<br />
7 <br />
7 <br />
Change<br />
beliefs
Cultivating<br />
resources<br />
internal)<br />
Stage of<br />
therapy<br />
Chap<br />
Reduce<br />
affect<br />
Improve<br />
cognitive<br />
processing<br />
Improve<br />
grounding<br />
Identify<br />
traumatic<br />
memories<br />
Process<br />
traumatic<br />
memories<br />
Boundaries<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 20 of 20<br />
Increase<br />
selfefficacy<br />
Increase<br />
resources<br />
Increase<br />
positive<br />
self Image<br />
third 7 () <br />
Decrease<br />
self<br />
destructive<br />
behaviors<br />
Self-image thinking third 7 () ()<br />
Questions to link<br />
resources<br />
All 7 <br />
Aligning percep.<br />
posit.<br />
Third<br />
(second)<br />
7 () <br />
Compare and<br />
contrast<br />
Third<br />
(second)<br />
7 () <br />
<strong>The</strong>n & now All 7 () <br />
Externalizing<br />
problems<br />
All 7 () <br />
Letter to God Third 7 <br />
Counter practices<br />
to self sabotage<br />
<strong>Tools</strong> <strong>for</strong><br />
therapist<br />
development<br />
Translating DSM<br />
Dx into action<br />
plans<br />
Countertransference<br />
question list<br />
Solution oriented<br />
decision tree<br />
Solution oriented<br />
check list<br />
Cultivating<br />
resources<br />
(external)<br />
Cultivating<br />
resources<br />
internal)<br />
All 8 ()<br />
First (All) 3<br />
All 8<br />
All 8<br />
All 8<br />
All 7 <br />
All 7 <br />
First = the primary phase in which the tool would be used (first) = secondary or optional phases in which the tool will be used<br />
= This goal is a main target of the tool () = This goal is either a secondary effect of the tool or the tool may assist in furthering this goal.<br />
= This goal is strongly influenced by this tool.<br />
Change<br />
beliefs
REFERENCES & RESOURCES<br />
Resources from Dr Schwarz<br />
(Special Pricing at this Training)<br />
1) <strong>Tools</strong> <strong>for</strong> trans<strong>for</strong>ming <strong>Trauma</strong>. Brunner Routledge: New York (available at amazon.com)<br />
2) <strong>Tools</strong> <strong>for</strong> Mastering <strong>Trauma</strong> Self Help Audio CDS (available from www.doctor-bob.net/<br />
(also available from the couragetochange.com)<br />
3) <strong>Trauma</strong> Reassociative Conditioning Video tape <strong>for</strong> therapists: (available from www.doctorbob.net/<br />
(also available from the couragetochange.com)<br />
Websites of organizations relevant to this workshop<br />
American Society of Clinical Hypnosis www. ASCH.net<br />
MiltonH <strong>Erickson</strong> Foundation www. www.erickson-foundation.org<br />
<strong>International</strong> Society <strong>for</strong> the Study of Dissociation www.issd.org<br />
<strong>International</strong> Society <strong>for</strong> the Study of traumatic Stress www.istss.org<br />
Great Books and Articles on <strong>Trauma</strong> Treatment<br />
Braun, B., G. (1988). <strong>The</strong> BASK model of dissociation. Dissociation, 1 (1), 4-23.<br />
Briere, J., N. (1992) Child abuse trauma: <strong>The</strong>ory and treatment of the lasting effects. Thousand Oaks,Ca. :Sage<br />
Calof, D. (1995). Compassionate alternatives to direct validation of memories. Presented at the 3rd<br />
Annual Conference on Advances in Treating Survivors of Abuse. San Francisco March 5, 1995 .Audio<br />
Cassette # H129 Info-medix 1-800-367-9286.<br />
Calof, D.F. (1995b) “Chronic self-injury in adult survivors of abuse: Sources, motivations and functions of self<br />
injury” (Part 1). Treating Abuse Today 5, (3), 11-17.<br />
deMause, L., (1991) <strong>The</strong> universality of incest, Journal of Psychohistory. 19,(2), 1-21.<br />
Herman, J.L., (1992), <strong>Trauma</strong> and Recovery: <strong>The</strong> aftermanth of violence-from domestic abuse to<br />
political terror. New York: Basic.<br />
Herman, J.L., Perry, J.C. & van der Kolk, B.A. (1989). Childhood trauma in borderline personality disorder.<br />
American Journal of Psychiatry, 146, 490-495.<br />
Herman, J. L & Schatzow, E. (1987). Recovery & verification of memories of childhood sexual trauma,<br />
Psychoanalytic Psychology, 4,1,1-14.<br />
Herman, J.L.& van der Kolk, B.A (1987) <strong>Trauma</strong>tic origins of borderline personality disorder. In B.A.van der<br />
Kolk (ed). Psychological <strong>Trauma</strong>. Washington: APA Press.<br />
Horowitz, M.J. (1986). Stress response syndromes (2nd edition). New York: Jason Aronson.<br />
Janoff-Bulman. R. (1992). Shattered assumptions: Towards a new psychology of trauma. New York: <strong>The</strong> Free<br />
Press.<br />
Kilpatrick, D.G., Saunders, B.E. Amick-McMullan, A., Best, C.L., Veronen, L.J.. & Resnick, H.S. (1989). “Victims<br />
and crime factors associated with the development of crime related post-traumatic stress disorder.”<br />
Behavior <strong>The</strong>rapy, 20, 199-214.<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 21 of 21
Kluft, R. P. (1984) Treatment of multiple personality disorder: A study of 33 cases. Psychiatric clinics of north<br />
America 7,(1),9-29.<br />
Kluft, R. P. (1990b)<strong>The</strong> Fractionated Abreaction technique in D.C Hammond (Ed.) <strong>The</strong> Handbook of Hypnotic<br />
Suggestions and Metaphors. New York: WW Norton.<br />
Kluft, R. P. (1994),Treatment trajectories in multiple personality disorder. Dissociation, Vol 7, 1, pp63-76,<br />
Linehan, M. M., (1983a). Cognitive-Behavioral Treatment of Borderline Personality Disorder. San Francisco:<br />
Guil<strong>for</strong>d.<br />
Linehan, M. M., (1983b). Skills Training Manual <strong>for</strong> Treating Borderline Personality Disorder. San Francisco:<br />
Guil<strong>for</strong>d.<br />
Maltz, W. (1992). <strong>The</strong> Sexual Healing Journey : A Guide <strong>for</strong> Survivors of Sexual Abuse. Harper: New York.<br />
McCann, I. L. & Pearlman, L. A. (1990) Psychological trauma and the adult survivor: <strong>The</strong>ory therapy and<br />
trans<strong>for</strong>mation. New York: Brunner/Mazel.<br />
Peterson, C., Prout, M., Schwarz, R. (1991). Post-traumatic stress disorder: A clinicians guidebook. New York:<br />
Plennum Press.<br />
Phillips, M. & Frederick, C. (1995). Healing the divided self: Clinical and <strong>Erickson</strong>ian hypnotherapy <strong>for</strong> posttraumatic<br />
and dissociative conditions New York: Norton.<br />
Putnam, F.W. (1989). Diagnosis and treatment of multiple personality disorder. New York: Guil<strong>for</strong>d.<br />
Ross, C. A. (1989), Multiple Personality Disorder: Diagnosis, clinical features and .treatment. New York: Wiley.<br />
Ross, C. A. 1995 Satanic Ritual Abuse: Principles of Treatment, University of Toronto Press, Toronto<br />
Salter, A. C. (1995). Trans<strong>for</strong>ming trauma. Thousand Oaks:Sage.<br />
Schwarz, R.A (1994) Hypnotic Approaches in Treating PTSD: An <strong>Erickson</strong>ian Framework in M.B. Williams &<br />
J.F. Sommer, (Eds.) <strong>The</strong> Handbook of post traumatic stress. Westport,Ct.: Greenwood Press<br />
Schwarz, R.A (1995) Clinical treatment strategies to reduce distortions of memory and action in trauma work,”<br />
Innovations in Clinical Practice Vol. 14, Professional Resource Press (1995).<br />
Schwarz, R.A (1998) From “Either-or” to “Both-And”: Collaborative Approaches to Treating Dissociative Disorders.<br />
In M. Hoyt (ed) Constructive <strong>The</strong>rapies 3 . San Francisco: Guil<strong>for</strong>d.<br />
Schwarz & Calof (1994). Indirect Suggestion, unwitting therapist influence & other iatrogenic issues in trauma<br />
work. Presented at Advances in Treating Survivors of Sexaul Abuse: Empowering the Healing Process<br />
II. San Diego, March 10,1994 Info-medix 1-800-367-9286.<br />
Schwarz, R.A. & Dolan, Y. (1995) Strategies of successful thrivors: Unpublished<br />
Schwarz, R. A. & Prout, M. F. (1991). Integrative approaches in the treatment of post-traumatic stress disorder.<br />
Psychotherapy, 28, 364-372.<br />
Terr, L. (1994). Unchained Memories: True Stories of <strong>Trauma</strong>tic Memories Lost and Found. NY: Basic Books.<br />
Trepper, T. S., & Barrett, M. J. (1989). Systemic treatment of incest. New York: Brunner/Mazel.<br />
van der Kolk, B. A. (1988). Psychological <strong>Trauma</strong>. Washington: APA Press.<br />
van der Kolk, B. A. (1989). <strong>The</strong> compulsion to repeat trauma: Revictimization, attachment and masochism.<br />
Psychiatric Clinics of North America,12, 389-411.<br />
van der Kolk, B. A (1996a) <strong>The</strong> complexity of adaptation to trauma: Self regulation, stimulus discrimination and<br />
characterological development. In B.A. van der Kolk (ed) Posttraumatic stress disorder: Psychological<br />
and biological sequelae. Washington, D.C.: American Psychiatric Press<br />
van der Kolk, B. A (1996b) <strong>Trauma</strong> and Memory. In B.A. van der Kolk (ed) Posttraumatic stress disorder:<br />
Psychological and biological sequelae. Washington, D.C.: American Psychiatric Press<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 22 of 22
Van der kolk, B.A.., Boyd.h., Krystal. J. et al. (1984) Post traumatic stress disorder as a biologically based<br />
disorder: Implications of the animal model of inescapable shock. In B.A. van der Kolk (ed) Posttraumatic<br />
stress disorder: Psychological and biological sequelae. Washington, D.C.: American Psychiatric Press<br />
van der Kolk, B.A., McFarlane, A. C. & Weisaeth, L. (Eds.) (1996) <strong>Trauma</strong>tic Stress: <strong>The</strong> effects of<br />
Overwhelming Experience on the Mind, Body and Society, Guil<strong>for</strong>d Press: New York.<br />
Great Books and Articles on Hypnosis ( often as it applies to trauma)<br />
Beahrs, J.O. (1982). Unity and Multiplicity. New York: Brunner/Mazel.<br />
Brown, D.P., Scheflin, A.W., & Hammnond, D. C.(1998). Memory, treatment and the law. New York: Norton.<br />
Cheek, D & Lecron, L. (1968). Clincal Hypnotherapy. New York: Grune & Stratton.<br />
<strong>Erickson</strong>, M., H. (1980a) Deep hypnosis and its induction in E. L. Rossi (Ed.) <strong>The</strong> collected papers of Milton H.<br />
<strong>Erickson</strong> on Hypnosis (vol1). New York: Irvington (Original work published 1952).<br />
<strong>Erickson</strong>, M.H. (1959/1980b) <strong>The</strong> utilization approach<br />
<strong>Erickson</strong>, M.H. (1980). <strong>The</strong> collected paper of Milton H. <strong>Erickson</strong> on Hypnosis (E. L. Rossi, Ed.) New York:<br />
Irvington.<br />
<strong>Erickson</strong>, M.H., Rossi, E.L., & Rossi, S.I. (1976) Hypnotic realities: <strong>The</strong> induction of clinical hypnosis and <strong>for</strong>ms<br />
of indirect suggestion. New York: Irvington.<br />
<strong>Erickson</strong>, M.H., & Rossi, E.L. (1979) Hypnotherapy: An exploratory casebook. New York: Irvington.<br />
Gilligan, S.(1987). <strong>The</strong>rapeutic trances: <strong>The</strong> cooperation principle in <strong>Erickson</strong>ian hypnotherapy. New York:<br />
Bruner/Mazel.<br />
Hammond, D., C. (Ed.) (1990). Handbook of hypnotic suggestions and metaphors. New York: Norton.<br />
Hammond, C. D. (1995) Clinical Hypnosis And Memory: Guidelines For Clinicians And For Forensic Hypnosis,<br />
ASCH Committee on Hypnosis & Memory, Des Plaines, IL. ASCH Press.<br />
Hammond, D.C. & Cheek, D.B. (1988). Ideomotor signaling: A method <strong>for</strong> rapid unconscious exploration in D.C.<br />
Hammond (Ed.) Hypnotic Induction and Suggestion: An introductory Manual. Des Plaines, Il. American<br />
Society of Clinical Hypnosis, pp 90-97.<br />
Lankton, S. R. (1985) A state of consciousness model of <strong>Erickson</strong>ian hypnosis in S. R.Lankton (ed.) <strong>Erickson</strong>ian<br />
monographs Vol 1 Elements and dimensions of an <strong>Erickson</strong>ian approach, 26-41.<br />
Lankton, S. R. & Lankton C. (1983). <strong>The</strong> answer within: A clinical framework of <strong>Erickson</strong>ian hypnotherapy. New<br />
York: Bruner/Mazel.<br />
Lankton, S. R. & Lankton C. (1987), Enchantment and intervention. New York: Bruner/Mazel.<br />
Watkins, John & Watkins, H. (1997) Ego states theory and Practice. New York; Norton<br />
© All rights reserved <strong>Tools</strong> <strong>for</strong> Trans<strong>for</strong>ming <strong>Trauma</strong><br />
Dr Robert Schwarz 610-642-0884 doctorbob1000@msn.com page 23 of 23