using nutrition to ease the pain of osteoarthritis - HillsVet
using nutrition to ease the pain of osteoarthritis - HillsVet
using nutrition to ease the pain of osteoarthritis - HillsVet
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>nutrition</strong> myths and truths, facts and fallacies<br />
Using Nutrition <strong>to</strong> Ease <strong>the</strong> Pain <strong>of</strong> Osteoarthritis<br />
Ron McLaughlin, DVM, DVSc, DACVS, Department <strong>of</strong> Clinical Sciences, Mississippi State University, College <strong>of</strong> Veterinary Medicine<br />
Introduction<br />
Osteoarthritis (OA) is a progressive, degenerative dis<strong>ease</strong> <strong>of</strong> synovial joints characterized by <strong>pain</strong>, disability,<br />
destruction <strong>of</strong> articular cartilage, and bony remodeling. It is <strong>the</strong> most common cause <strong>of</strong> lameness in dogs and is<br />
estimated <strong>to</strong> affect 20% <strong>of</strong> <strong>the</strong> canine population over 1 year <strong>of</strong> age. The radiographic prevalence <strong>of</strong> CHD has<br />
been reported <strong>to</strong> be as high as 70% in golden retrievers and Rottweilers. Risk fac<strong>to</strong>rs for developing OA include<br />
age, breed, genetics, trauma, obesity and developmental orthopedic conditions.<br />
Primary OA is rare in dogs and is <strong>the</strong> result <strong>of</strong> defective articular cartilage structure and biosyn<strong>the</strong>sis. Secondary<br />
OA is very common and may be caused by joint trauma, inflamma<strong>to</strong>ry conditions, congenital and developmental<br />
abnormalities, and metabolic, endocrine, neuropathic, neoplastic, or iatrogenic causes. Once <strong>the</strong> dis<strong>ease</strong> process<br />
begins, a progressive cascade <strong>of</strong> mechanical and biochemical events occurs resulting in cartilage destruction,<br />
subchondral bony sclerosis, synovial membrane inflammation, en<strong>the</strong>siophy<strong>to</strong>sis, and <strong>the</strong> development <strong>of</strong><br />
periarticular osteophytes.<br />
Pathophysiology<br />
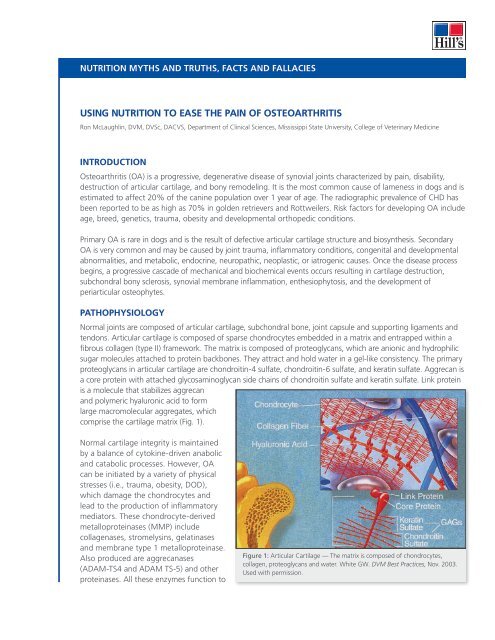
Normal joints are composed <strong>of</strong> articular cartilage, subchondral bone, joint capsule and supporting ligaments and<br />
tendons. Articular cartilage is composed <strong>of</strong> sparse chondrocytes embedded in a matrix and entrapped within a<br />
fibrous collagen (type II) framework. The matrix is composed <strong>of</strong> proteoglycans, which are anionic and hydrophilic<br />
sugar molecules attached <strong>to</strong> protein backbones. They attract and hold water in a gel-like consistency. The primary<br />
proteoglycans in articular cartilage are chondroitin-4 sulfate, chondroitin-6 sulfate, and keratin sulfate. Aggrecan is<br />
a core protein with attached glycosaminoglycan side chains <strong>of</strong> chondroitin sulfate and keratin sulfate. Link protein<br />
is a molecule that stabilizes aggrecan<br />
and polymeric hyaluronic acid <strong>to</strong> form<br />
large macromolecular aggregates, which<br />
comprise <strong>the</strong> cartilage matrix (Fig. 1).<br />
Normal cartilage integrity is maintained<br />
by a balance <strong>of</strong> cy<strong>to</strong>kine-driven anabolic<br />
and catabolic processes. However, OA<br />
can be initiated by a variety <strong>of</strong> physical<br />
stresses (i.e., trauma, obesity, DOD),<br />
which damage <strong>the</strong> chondrocytes and<br />
lead <strong>to</strong> <strong>the</strong> production <strong>of</strong> inflamma<strong>to</strong>ry<br />
media<strong>to</strong>rs. These chondrocyte-derived<br />
metalloproteinases (MMP) include<br />
collagenases, stromelysins, gelatinases<br />
and membrane type 1 metalloproteinase.<br />
Also produced are aggrecanases<br />
(ADAM-TS4 and ADAM TS-5) and o<strong>the</strong>r<br />
proteinases. All <strong>the</strong>se enzymes function <strong>to</strong><br />
Figure 1: Articular Cartilage — The matrix is composed <strong>of</strong> chondrocytes,<br />
collagen, proteoglycans and water. White GW. DVM Best Practices, Nov. 2003.<br />
Used with permission.
<strong>nutrition</strong> myths and truths, facts and fallacies<br />
break down cartilage matrix faster than new matrix can be produced. The products <strong>of</strong> cartilage breakdown are<br />
antigenic and provoke synovitis.<br />
Synovial macrophages and leukocytes are abundant sources <strong>of</strong> cy<strong>to</strong>kines, procoagulant fac<strong>to</strong>rs, proteinases<br />
and oxygen-derived free radicals including nitric oxide (NO-). Interleukin-1-beta (IL-1) and tumor necrosis<br />
fac<strong>to</strong>r-alpha (TNF-) are <strong>the</strong> predominant proinflamma<strong>to</strong>ry cy<strong>to</strong>kines syn<strong>the</strong>sized during <strong>the</strong> OA process. IL-1<br />
stimulates <strong>the</strong> breakdown <strong>of</strong> matrix proteins and <strong>the</strong> accumulation <strong>of</strong> degradation products. TNF- appears <strong>to</strong><br />
drive <strong>the</strong> inflamma<strong>to</strong>ry process. Both substances induce articular cells <strong>to</strong> produce o<strong>the</strong>r cy<strong>to</strong>kines and incr<strong>ease</strong><br />
<strong>the</strong>ir own production, as well as stimulate production <strong>of</strong> prot<strong>ease</strong>s and prostaglandin E 2<br />
(PGE 2<br />
). Numerous<br />
o<strong>the</strong>r cy<strong>to</strong>kines and growth fac<strong>to</strong>rs are also involved in OA pathophysiology. These inflamma<strong>to</strong>ry cy<strong>to</strong>kines<br />
contribute <strong>to</strong> <strong>the</strong> perpetuation and progression <strong>of</strong> arthritis by sustaining catabolic processes. Once initiated,<br />
<strong>the</strong>se molecular and cellular pathways form a self-perpetuating cycle.<br />
Clinical Presentation<br />
Signalment: A patient’s breed, age, gender and body weight provide valuable information when assessing <strong>the</strong><br />
patient’s relative risk for <strong>osteoarthritis</strong>. Rapidly growing large breed dogs, for example, are <strong>of</strong>ten affected with<br />
developmental orthopedic conditions that can lead <strong>to</strong> OA. Older dogs <strong>of</strong>ten demonstrate signs <strong>of</strong> OA. Obese<br />
animals appear more susceptible <strong>to</strong> OA and, because <strong>of</strong> <strong>the</strong>ir added weight, may be more debilitated by <strong>the</strong><br />
dis<strong>ease</strong>. One long term study has documented that <strong>the</strong> prevalence and severity <strong>of</strong> <strong>osteoarthritis</strong> is greater in dogs<br />
with body condition scores above normal. Over <strong>the</strong> life span <strong>of</strong> <strong>the</strong>se same dogs, <strong>the</strong> mean age at which 50% <strong>of</strong><br />
<strong>the</strong> dogs required long-term treatment for clinical signs attributable <strong>to</strong> <strong>osteoarthritis</strong> was significantly earlier (10.3<br />
years, p
<strong>nutrition</strong> myths and truths, facts and fallacies<br />
hip joint<br />
KNEE joint<br />
healthy hip joint<br />
arthritic hip joint healthy knee joint arthritic knee joint<br />
Figure 2: Radiographic images <strong>of</strong> healthy and arthritic hip and knee joints demonstrating typical changes<br />
thickening <strong>of</strong> <strong>the</strong> joint capsule, sclerosis or erosion <strong>of</strong> <strong>the</strong> subchondral bone, periarticular osteophyte formation,<br />
en<strong>the</strong>siophytes, and joint mice (Fig. 2).<br />
Arthrocentesis and synovial fluid analysis: Synovial fluid collected from affected joints is examined for<br />
volume, color, clarity, viscosity, cy<strong>to</strong>logy, and biochemical analysis. Fluid from patients with OA may be clear or<br />
pale yellow and slightly turbid due <strong>to</strong> an incr<strong>ease</strong> in inflamma<strong>to</strong>ry cells. It typically contains synovial cells and<br />
less than 5 x 10 3 /L mononuclear cells (and a few red blood cells may also be present). Polymorphonuclear cells<br />
typically constitute 0-12% <strong>of</strong> cells. Synovial fluid analysis alone may not differentiate OA joints from normal<br />
joints (particularly in <strong>the</strong> early stages <strong>of</strong> OA), but is valuable in ruling out septic and immune-mediated arthritis.<br />
Physical<br />
Rehabilitation<br />
NSAID<br />
Adjunct<br />
Multimodal<br />
Osteoarthritis<br />
Management<br />
Weight Control<br />
and Exercise<br />
EPA-rich<br />
Diet<br />
Figure 3: Multimodal management <strong>of</strong><br />
<strong>osteoarthritis</strong><br />
Chondroprotectant<br />
Treatment Of OA<br />
Multimodal medical treatment is recommended for OA, including<br />
weight reduction, proper <strong>nutrition</strong>, exercise control, physical<br />
<strong>the</strong>rapy, and <strong>the</strong> administration <strong>of</strong> anti-inflamma<strong>to</strong>ry medications,<br />
analgesics, and <strong>osteoarthritis</strong> dis<strong>ease</strong> modifying agents (Fig. 3).<br />
Exercise and Physical Rehabilitation: Exercise and physical <strong>the</strong>rapy<br />
are <strong>of</strong>ten used as part <strong>of</strong> <strong>the</strong> treatment for OA in humans and dogs.<br />
Exercise reduces obesity (a primary contribu<strong>to</strong>r <strong>to</strong> <strong>the</strong> progression <strong>of</strong><br />
OA) and controlled exercise may help improve strength and range<br />
<strong>of</strong> motion in joints. Exercise may also reduce <strong>the</strong> need for analgesic<br />
medications. Low-impact exercises such as walking and swimming<br />
are preferred. The activity should be initiated gradually and incr<strong>ease</strong>d<br />
as joint function improves. Warm compresses, coldpacks, massage<br />
<strong>the</strong>rapy, electro<strong>the</strong>rapy, and ultrasound are techniques used in<br />
treatment <strong>of</strong> both human and canine OA patients.<br />
Nutrition: Fish oil as a source <strong>of</strong> omega-3 fatty acids has been shown <strong>to</strong> reduce inflammation and <strong>pain</strong> in<br />
mammals. Certain omega-3 fatty acids have been shown <strong>to</strong> reduce <strong>the</strong> expression and activity <strong>of</strong> proteoglycandegrading<br />
enzymes, <strong>the</strong>reby having <strong>the</strong> potential <strong>to</strong> s<strong>to</strong>p <strong>the</strong> progression <strong>of</strong> <strong>osteoarthritis</strong> (Fig.4). Damaged<br />
chondrocytes produce inflamma<strong>to</strong>ry cy<strong>to</strong>kines that contribute <strong>to</strong> <strong>the</strong> progression <strong>of</strong> OA through catabolic
<strong>nutrition</strong> myths and truths, facts and fallacies<br />
Physical Stress<br />
DOD<br />
Weight<br />
Trauma<br />
Structural &<br />
Functional<br />
Failure<br />
Cartilage<br />
Damage<br />
X<br />
Inflammation<br />
EPA<br />
X<br />
Matrix<br />
Damage<br />
Degradation caused<br />
by aggrecanases<br />
processes. Normally, arachidonic acid<br />
is <strong>the</strong> precursor for <strong>the</strong> syn<strong>the</strong>sis <strong>of</strong><br />
<strong>the</strong>se inflamma<strong>to</strong>ry cy<strong>to</strong>kines. EPA,<br />
an omega-3 fatty acid, competes<br />
with arachidonic acid for <strong>the</strong> same<br />
enzyme systems; and <strong>the</strong> eicosanoids<br />
derived from EPA promote minimal <strong>to</strong><br />
no inflamma<strong>to</strong>ry activity. Thus, a diet<br />
containing n-3 fatty acids results in<br />
a decr<strong>ease</strong> in membrane arachidonic<br />
acid levels and an associated decr<strong>ease</strong><br />
in <strong>the</strong> pro-inflamma<strong>to</strong>ry cy<strong>to</strong>kines<br />
that perpetuate OA. Studies have<br />
documented that inflamma<strong>to</strong>ry<br />
eicosanoids produced from arachidonic<br />
acid are depressed when dogs consume<br />
foods with high levels <strong>of</strong> n-3 fatty acids, and specifically foods containing EPA. Though <strong>the</strong> exact molecular<br />
mechanisms for reducing inflammation (likely via resolvins and protectins) have not been fully explained, it is<br />
conceivable that omega-3 fatty acids modulate this process at <strong>the</strong> level <strong>of</strong> <strong>the</strong> genome or proteome.<br />
Four randomized, double-masked, controlled studies have been conducted in which arthritic dogs were fed a<br />
control food or a test food containing various levels <strong>of</strong> EPA (omega-3 fatty acid). These studies reported that <strong>the</strong><br />
dogs fed <strong>the</strong> EPA-supplemented food improved in range <strong>of</strong> motion and ability <strong>to</strong> bear weight, had a decr<strong>ease</strong> in<br />
<strong>pain</strong> and lameness, had significantly improved ability <strong>to</strong> rise form a resting position, and improved ability <strong>to</strong> run<br />
and play at 6 weeks. In one <strong>of</strong> <strong>the</strong>se studies, biomechanical force plate analysis was also performed and found<br />
that dogs fed a diet containing EPA had an incr<strong>ease</strong> in weight bearing on <strong>the</strong> affected limb. Only 31% <strong>of</strong> <strong>the</strong><br />
“control” dogs had improved weight bearing after <strong>the</strong> 90-day feeding trial, whereas 82% <strong>of</strong> dogs in <strong>the</strong> “EPA”<br />
group showed incr<strong>ease</strong>d weight bearing. These clinical studies indicate that <strong>nutrition</strong>al management <strong>using</strong> a<br />
<strong>the</strong>rapeutic food supplemented with n-3 fatty acids helped improve <strong>the</strong> clinical signs <strong>of</strong> <strong>osteoarthritis</strong> in dogs as<br />
noted by pet owners, clinical orthopedic examination, and gait analysis <strong>of</strong> ground reaction forces.<br />
Dis<strong>ease</strong>-modifying <strong>osteoarthritis</strong> agents: These agents reportedly enhance cartilage health by providing<br />
<strong>the</strong> necessary precursors <strong>to</strong> maintain and repair cartilage. Many have been shown <strong>to</strong> positively affect cartilage<br />
matrix, enhance hyaluronate production, and inhibit catabolic enzymes. Oral dis<strong>ease</strong>-modifying OA agents<br />
typically contain glucosamine and chondroitin sulfate in various forms.<br />
Glucosamine is a precursor <strong>to</strong> <strong>the</strong> disaccharide unit <strong>of</strong> glycosaminoglycans, which comprise <strong>the</strong> proteoglycan<br />
matrix <strong>of</strong> articular cartilage. Studies <strong>using</strong> radiolabeled compounds have shown that 87% <strong>of</strong> orally administered<br />
glucosamine is absorbed and is eventually incorporated in<strong>to</strong> <strong>the</strong> cartilage matrix. Glucosamine reportedly acts<br />
by providing <strong>the</strong> regula<strong>to</strong>ry stimulus and raw materials for syn<strong>the</strong>sis <strong>of</strong> glycosaminoglycans. Since chondrocytes<br />
obtain preformed glucosamine from <strong>the</strong> circulation (or syn<strong>the</strong>sizes it from glucose and amino acids), adequate<br />
glucosamine levels in <strong>the</strong> body are essential for syn<strong>the</strong>sis <strong>of</strong> glycosaminoglycans in cartilage. Glucosamine is also<br />
used directly for <strong>the</strong> production <strong>of</strong> hyaluronic acid by synoviocytes. In vitro biochemical and pharmacological<br />
studies indicate that <strong>the</strong> administration <strong>of</strong> glucosamine may normalize cartilage metabolism and stimulates<br />
<strong>the</strong> syn<strong>the</strong>sis <strong>of</strong> proteoglycans. Clinical trials in man and animals indicate that glucosamine may have a positive<br />
effect on cartilage health and helps control symp<strong>to</strong>ms associated with OA.<br />
X<br />
Figure 4: Pathophysiology <strong>of</strong> OA — In <strong>the</strong> dog, high levels <strong>of</strong> EPA help control<br />
pathways <strong>of</strong> inflammation and degradation.
<strong>nutrition</strong> myths and truths, facts and fallacies<br />
Chondroitin Sulfate (CS) is <strong>the</strong> predominant glycosaminoglycan found in articular cartilage. Bioavailability<br />
studies have shown 70% absorption <strong>of</strong> CS following oral administration. The effect <strong>of</strong> CS on cartilage has been<br />
investigated in several in vivo and in vitro studies. The findings suggest that CS reduces collagenolytic activity,<br />
inhibits degradative enzymes, incr<strong>ease</strong>s hyaluronate concentrations, and reduces symp<strong>to</strong>ms <strong>of</strong> OA. Most<br />
research indicates that glucosamine and chondroitin sulfate work synergistically. Numerous studies performed<br />
on one such combination (Cosequin ® Nutrimax Labora<strong>to</strong>ries, Inc.) have demonstrated improved syn<strong>the</strong>sis <strong>of</strong><br />
glycosaminoglycans and reduced proteolytic activity. Clinical trials have repeatedly shown a positive clinical<br />
effect in OA patients.<br />
Injectable dis<strong>ease</strong>-modifying OA agents are also available, <strong>the</strong> most common one used in dogs being Adequan ® *<br />
(used under license, Novartis Animal Health). Adequan is a polysulfated glycosaminoglycan (PSGAG), and studies<br />
have shown it has a positive anabolic effect on cartilage and decr<strong>ease</strong>s cartilage catabolism.<br />
Anti-inflamma<strong>to</strong>ry and analgesic medications (NSAIDs): NSAIDs are used because <strong>of</strong> <strong>the</strong>ir ability <strong>to</strong><br />
reduce joint <strong>pain</strong> and decr<strong>ease</strong> synovitis. A variety <strong>of</strong> NSAIDs are available for use in animals and are effective,<br />
in part, by decreasing prostaglandin syn<strong>the</strong>sis through <strong>the</strong> inhibition <strong>of</strong> cyclooxygenase (COX). Newer NSAIDs<br />
have been shown <strong>to</strong> have no detrimental affect on <strong>the</strong> syn<strong>the</strong>sis <strong>of</strong> cartilage proteoglycans in vitro at <strong>the</strong><br />
recommended dosing. Drugs commonly used <strong>to</strong> control <strong>pain</strong> in dogs with OA include acetaminophen (15 mg/<br />
kg q 8h), carpr<strong>of</strong>en (4.4 mg/kg q 24h), e<strong>to</strong>dolac (10-15 mg/kg q 24h), meloxicam (0.1 mg/kc q 8h), deracoxib<br />
(1-2 mg/kg q 24h), and tepoxalin (10mg/kg q 24h) among o<strong>the</strong>rs. It is important <strong>to</strong> recognize that individual<br />
patients respond <strong>to</strong> specific NSAIDs quite differently.<br />
Corticosteroid treatment for OA remains controversial. Corticosteroids decr<strong>ease</strong> <strong>the</strong> production <strong>of</strong> arachidonic<br />
acid, are potent anti-inflamma<strong>to</strong>ry agents, and decr<strong>ease</strong> catabolic activity within <strong>the</strong> joint. However,<br />
corticosteroids may also damage cartilage (with long-term usage) by decreasing syn<strong>the</strong>sis <strong>of</strong> collagen and<br />
matrix proteoglycans.<br />
Summary<br />
Although prevention <strong>of</strong> <strong>osteoarthritis</strong> is ideal, it is not always possible. Because <strong>osteoarthritis</strong> is a heterogeneous<br />
dis<strong>ease</strong> with diverse origins, it can present with a range <strong>of</strong> clinical manifestations. As a result, <strong>the</strong>rapeutic<br />
recommendations should be cus<strong>to</strong>mized for each patient. When appropriate, surgical correction <strong>of</strong> underlying<br />
conditions should be considered. After <strong>osteoarthritis</strong> is diagnosed, clients should be educated <strong>to</strong> foster<br />
realistic expectations. Osteoarthritis is usually irreversible but good management can minimize <strong>pain</strong> and slow<br />
progression <strong>of</strong> <strong>the</strong> dis<strong>ease</strong>. The goals <strong>of</strong> management include:<br />
✔ mitigation <strong>of</strong> risk fac<strong>to</strong>rs<br />
✔ controlling clinical signs<br />
✔ slowing progression <strong>of</strong> <strong>the</strong> dis<strong>ease</strong>.<br />
Thus, effective treatment requires a multimodal approach, <strong>of</strong> which <strong>the</strong>rapeutic <strong>nutrition</strong> is an important<br />
component. The goals <strong>of</strong> <strong>nutrition</strong>al management include reducing inflammation and <strong>pain</strong>, enhancing cartilage<br />
repair, slowing cartilage degradation and providing tangible improvement in clinical signs <strong>of</strong> <strong>osteoarthritis</strong>.<br />
Foods designed for patients with <strong>osteoarthritis</strong> should supply age-appropriate <strong>nutrition</strong> and specific nutrients<br />
that may help reduce inflammation and <strong>pain</strong>, slow <strong>the</strong> degradative process, complement prescribed medications<br />
and provide tangible improvement in clinical signs.<br />
* As with all drugs in this class, side effects involving <strong>the</strong> digestive system, kidneys or liver may occur. These are normally mild, but may be serious. Pet owners should<br />
discontinue <strong>the</strong>rapy and contact <strong>the</strong>ir veterinarian immediately if side effects occur. Evaluation for pre-existing conditions and regular moni<strong>to</strong>ring are recommended<br />
for pets on any medication, including Adequan. ® Use with o<strong>the</strong>r NSAIDs or corticosteroids should be avoided.
<strong>nutrition</strong> myths and truths, facts and fallacies<br />
Clinical Case:<br />
Nutritional management <strong>of</strong> <strong>osteoarthritis</strong><br />
Phoebe<br />
His<strong>to</strong>ry and clinical findings<br />
Phoebe, a 6-year-old neutered female Labrador retriever mix, was<br />
examined for rear limb lameness <strong>of</strong> two years duration. Clinical signs<br />
were mild <strong>to</strong> moderate in severity and included difficulty in rising<br />
from rest, limping, stiffness and reluctance <strong>to</strong> run, jump or play. No<br />
medications or supplements were being given by <strong>the</strong> owner. Phoebe<br />
weighed 75 pounds but was considered overweight with a body<br />
condition score <strong>of</strong> 4 on a 5-point scale. Phoebe was fed a low-calorie<br />
dry dog food but had access <strong>to</strong> o<strong>the</strong>r food sources for cats and dogs in<br />
<strong>the</strong> same household.<br />
Physical examination was normal except for <strong>the</strong> overweight body condition and orthopedic problems. A thorough<br />
orthopedic examination revealed <strong>the</strong> following abnormalities:<br />
✔ slight lameness at a walk<br />
✔ normal weight-bearing at rest but favors <strong>the</strong> left rear limb when walking<br />
✔ mild limitation in range <strong>of</strong> motion <strong>of</strong> <strong>the</strong> left hip joint<br />
✔ <strong>of</strong>fers mild resistance when <strong>the</strong> right rear limb is elevated but bears full weight on <strong>the</strong> left hind limb<br />
✔ mild <strong>pain</strong> is elicited upon palpation <strong>of</strong> <strong>the</strong> left hip joint.<br />
A complete blood count, serum biochemistry pr<strong>of</strong>ile and<br />
urinalysis were normal. Radiographs showed changes consistent<br />
with bilateral hip dysplasia and degenerative joint dis<strong>ease</strong> with<br />
<strong>the</strong> left cox<strong>of</strong>emoral joint more severely affected (Fig. 1).<br />
Questions<br />
Q. What are <strong>the</strong> <strong>the</strong>rapeutic goals for managing patients with<br />
<strong>osteoarthritis</strong> or degenerative joint dis<strong>ease</strong> <strong>of</strong> hip joints?<br />
A. Therapeutic goals for managing chronic <strong>osteoarthritis</strong> or<br />
degenerative joint dis<strong>ease</strong> in <strong>the</strong> cox<strong>of</strong>emoral joints include:<br />
✔ Eliminating underlying causes (e.g., femoral head and<br />
neck excision for aseptic necrosis <strong>of</strong> <strong>the</strong> femoral head)<br />
Figure 1: Radiographs consistent with<br />
bilateral hip dysplasia and degenerative<br />
joint dis<strong>ease</strong> with <strong>the</strong> left cox<strong>of</strong>emoral joint<br />
more severely affected.<br />
✔ Setting realistic treatment expectations with Phoebe’s<br />
owner<br />
✔ Enhancing Phoebe’s quality <strong>of</strong> life by reducing <strong>pain</strong>,<br />
maintaining or improving activity level and improving<br />
joint function<br />
✔ Slowing dis<strong>ease</strong> progression by modifying cartilage<br />
structure and function.
<strong>nutrition</strong> myths and truths, facts and fallacies<br />
Physical<br />
Rehabilitation<br />
NSAID<br />
Adjunct<br />
Multimodal<br />
Osteoarthritis<br />
Management<br />
Weight Control<br />
and Exercise<br />
EPA-rich<br />
Diet<br />
Figure 2: Multimodal management <strong>of</strong><br />
<strong>osteoarthritis</strong><br />
Chondroprotectant<br />
Most animals with chronic <strong>osteoarthritis</strong> or degenerative joint dis<strong>ease</strong><br />
have irreversible changes with no opportunity <strong>to</strong> eliminate or cure<br />
<strong>the</strong> condition. This makes client education very important. Realistic<br />
expectations for both Phoebe’s owner and <strong>the</strong> veterinarian should<br />
acknowledge <strong>the</strong> facts that degenerative joint dis<strong>ease</strong> is controllable<br />
but not curable. A comprehensive multimodal management plan<br />
should focus on long-term <strong>pain</strong> management, altering dis<strong>ease</strong><br />
progression and improving Phoebe’s quality <strong>of</strong> life (Fig. 2).<br />
Q. How might <strong>the</strong> overweight body condition contribute <strong>to</strong> <strong>the</strong><br />
clinical problems in this dog?<br />
A. Osteoarthritis is <strong>of</strong>ten associated with abnormal forces acting on<br />
normal joints or normal forces acting on abnormal joints. Obesity<br />
may contribute <strong>to</strong> progression <strong>of</strong> degenerative joint dis<strong>ease</strong> and<br />
clinical signs by ca<strong>using</strong> excess physical stress on ei<strong>the</strong>r normal or<br />
abnormal joints. Additionally, recent studies have documented<br />
metabolic activity in adipose tissue that may be <strong>of</strong> equal or greater importance. Adipocytes secrete several<br />
hormones including leptin and adiponectin and produce a diverse range <strong>of</strong> proteins termed adipokines. Among<br />
<strong>the</strong> currently recognized adipokines are a growing list <strong>of</strong> media<strong>to</strong>rs <strong>of</strong> inflammation (Fig. 3). These adipokines<br />
are found in human and canine adipocytes. Production <strong>of</strong> <strong>the</strong>se proteins is incr<strong>ease</strong>d in obesity, suggesting<br />
that obesity is a state <strong>of</strong> chronic low-grade inflammation. Low-grade inflammation may contribute <strong>to</strong> <strong>the</strong><br />
pathophysiology <strong>of</strong> a number <strong>of</strong> dis<strong>ease</strong>s commonly associated with obesity including <strong>osteoarthritis</strong>. This might<br />
explain why relatively small reductions in body weight can result in significant improvement in clinical signs.<br />
IL-6<br />
IL-beta<br />
IGF-1<br />
PAI-1<br />
Leptin<br />
C 3<br />
Adipose Tissue<br />
Angiotensinogen<br />
TGF-b<br />
SAA<br />
TNF<br />
Adiponectin<br />
Resistin<br />
Figure 3. Adipocy<strong>to</strong>kines and inflamma<strong>to</strong>ry media<strong>to</strong>rs produced<br />
by adipocytes and adipocyte associated macrophages. C3,<br />
complement protein 3; IGF-1, insulin-like growth fac<strong>to</strong>r-1; IL,<br />
interleukin; PAI-1, plasminogen activa<strong>to</strong>r inhibi<strong>to</strong>r-1; SAA, serum<br />
amyloid A; TNF-a, tumor necrosis fac<strong>to</strong>r-a; TGF-b, transforming<br />
growth fac<strong>to</strong>r-b.<br />
Q. Could this condition have been prevented with<br />
proper <strong>nutrition</strong>al management?<br />
A. Large- and giant-breed dogs are at risk for<br />
developmental orthopedic dis<strong>ease</strong> including<br />
hip and elbow dysplasia, osteochondrosis and<br />
o<strong>the</strong>r conditions associated with joint instability<br />
or incongruity. Nutritional risk fac<strong>to</strong>rs for<br />
developmental orthopedic dis<strong>ease</strong> include excess<br />
energy, fat and calcium intake during growth. Use<br />
<strong>of</strong> foods specifically formulated for large breed<br />
puppies helps manage <strong>the</strong>se <strong>nutrition</strong>al risk fac<strong>to</strong>rs<br />
and ensure a normal, healthy growth rate. Obesity<br />
is recognized as a risk fac<strong>to</strong>r for development<br />
<strong>of</strong> degenerative joint dis<strong>ease</strong> in dogs; avoiding<br />
obesity can help reduce <strong>the</strong> incidence and severity<br />
<strong>of</strong> <strong>osteoarthritis</strong>. Recent studies have shown that<br />
when at-risk puppies were fed free choice during<br />
growth, <strong>the</strong>y exhibited an incr<strong>ease</strong>d incidence<br />
and severity <strong>of</strong> hip joint laxity and hip dysplasia<br />
compared <strong>to</strong> puppies fed in a restricted fashion. Over time, those dogs fed <strong>to</strong> maintain lean body condition<br />
throughout life exhibited reduced severity <strong>of</strong> <strong>osteoarthritis</strong> and a delayed need for medication compared <strong>to</strong><br />
<strong>the</strong>ir heavier siblings.
<strong>nutrition</strong> myths and truths, facts and fallacies<br />
Q. Outline a comprehensive nonsurgical management plan for Phoebe.<br />
A. Non-surgical management <strong>of</strong> <strong>osteoarthritis</strong> should focus on three main aspects:<br />
✔ Activity modification<br />
✔ Medications and supplements <strong>to</strong> modify joint <strong>pain</strong> and function<br />
✔ Nutritional management that emphasizes weight control and modifying joint inflammation<br />
and cartilage degradation.<br />
In <strong>the</strong> past, limiting activity levels in patients with <strong>osteoarthritis</strong> and degenerative joint dis<strong>ease</strong> was considered<br />
important. However, recent studies in human and veterinary patients with <strong>osteoarthritis</strong> have shown <strong>the</strong><br />
benefits <strong>of</strong> exercise including decr<strong>ease</strong>d <strong>pain</strong> scores, improved joint function scores and less use <strong>of</strong> analgesic<br />
medications. Today, veterinary specialists are recommending <strong>the</strong>rapeutic exercise as a way <strong>to</strong> improve quality <strong>of</strong><br />
life for dogs with chronic <strong>osteoarthritis</strong>. A variety <strong>of</strong> medications and supplements are available <strong>to</strong> manage <strong>pain</strong><br />
and joint function. Responses <strong>to</strong> medications and supplements vary considerably in patients with <strong>osteoarthritis</strong><br />
and specific products and doses need <strong>to</strong> be individually tailored for each dog.<br />
Figure 4. Uptake <strong>of</strong> omega-3 fatty acids by canine chondrocytes AlA, alphalinolenate;<br />
EPA, eicosapentaenoate; DHA, docosahexanoate; control, serum free<br />
Dulbecco’s modified Eagle’s medium (DMEM). Caterson, B, Flannery CR, Hughes<br />
CE, et al. Mechanisms involved in cartilage proteoglycan catabolism. Matrix Biology<br />
2000;19(4):333-344.<br />
New information has been generated<br />
about canine <strong>osteoarthritis</strong> from in<br />
vitro studies with cartilage models<br />
and clinical studies in dogs with<br />
various forms <strong>of</strong> arthritis. In vitro<br />
cartilage studies have shown that<br />
canine chondrocyte membranes<br />
selectively s<strong>to</strong>re <strong>the</strong> omega-3 fatty<br />
acid EPA (eicosapentaenoic acid), and<br />
not o<strong>the</strong>r omega-3 fatty acids (Fig. 4).<br />
EPA is <strong>the</strong> most important fatty acid<br />
for helping manage inflammation in<br />
cartilage <strong>of</strong> dogs. EPA is also <strong>the</strong> only<br />
omega-3 fatty acid shown <strong>to</strong> inhibit<br />
activity <strong>of</strong> enzymes that degrade<br />
cartilage and helps turn <strong>of</strong>f <strong>the</strong> signal<br />
<strong>to</strong> make degradative enzymes (Fig. 5).<br />
Based on <strong>the</strong>se in vitro studies, clinical<br />
trials were performed in dogs with<br />
arthritis <strong>using</strong> Hill’s ® Prescription Diet ®<br />
j/d Canine, a food enhanced with<br />
levels <strong>of</strong> EPA much higher than those found in typical pet food and <strong>the</strong> only canned <strong>the</strong>rapeutic pet food<br />
in <strong>the</strong> <strong>osteoarthritis</strong> category. Hill’s ® Prescription Diet ® j/d Canine also contains <strong>the</strong> highest levels <strong>of</strong> <strong>to</strong>tal<br />
omega-3 fatty acids,* an omega-6 <strong>to</strong> omega-3 ratio less than 1.0, high carnitine levels, added glucosamine and<br />
chondroitin sulfate, added antioxidant nutrients and added lysolecithin. Feeding Hill’s ® Prescription Diet ® j/d <br />
Canine <strong>to</strong> dogs with arthritis resulted in higher serum EPA concentrations, significant improvements in clinical<br />
signs observed by pet owners, improved clinical assessments <strong>of</strong> arthritis by veterinarians and improved weight<br />
bearing on affected limbs as measured by force plate gait analysis. Many <strong>of</strong> <strong>the</strong> dogs in <strong>the</strong> studies were not<br />
receiving medications or supplements in conjunction with <strong>the</strong> food.<br />
* Data on file. Hill’s Pet Nutrition, Inc.
<strong>nutrition</strong> myths and truths, facts and fallacies<br />
Degradation<br />
begins with<br />
physical<br />
stress<br />
Degradation<br />
begins with<br />
physical<br />
stress<br />
functional<br />
Chondrocyte<br />
damage<br />
Chondrocyte<br />
damage<br />
High levels <strong>of</strong> omega-3<br />
and a low ratio <strong>of</strong><br />
omega-6 <strong>to</strong> omega-3<br />
interrupt<br />
inflammation<br />
Structural &<br />
failure<br />
Matrix<br />
damage<br />
Inflammation<br />
EPA interrupts<br />
degradation<br />
Degradation<br />
a. Up regulation <strong>of</strong> aggrecanase enzymes and<br />
inflamma<strong>to</strong>ry media<strong>to</strong>rs perpetuate cycle <strong>of</strong><br />
proteoglycan breakdown and matrix damage.<br />
b. Appropriate levels <strong>of</strong> EPA inhibit <strong>the</strong> up<br />
regulation <strong>of</strong> aggrecanase enzymes at <strong>the</strong> level <strong>of</strong><br />
mRNA and modulate <strong>the</strong> inflamma<strong>to</strong>ry response<br />
breaking <strong>the</strong> cycle <strong>of</strong> matrix damage.<br />
Figure 5. Eicosapentaenoic acid (EPA) interrupts <strong>the</strong> cycle <strong>of</strong> cartilage degradation and inflammation.<br />
Case management<br />
Hill’s ® Prescription Diet ® j/d Canine Dry pet food was dispensed for <strong>the</strong> owners <strong>to</strong> feed <strong>to</strong> Phoebe. The amount<br />
<strong>of</strong> food was calculated for an obese-prone animal. The owners were encouraged <strong>to</strong> deny Phoebe access <strong>to</strong><br />
o<strong>the</strong>r sources <strong>of</strong> dog and cat food in <strong>the</strong> same household. Controlled exercise was also encouraged <strong>using</strong> walks<br />
on a leash. Six weeks later <strong>the</strong> owner reported improvements in all clinical problems associated with arthritis<br />
and improvements in Phoebe’s overall personality. The improvements observed by <strong>the</strong> owner continued at<br />
<strong>the</strong> three-month recheck and no <strong>pain</strong> was elicited on palpation <strong>of</strong> <strong>the</strong> left hip joint by <strong>the</strong> veterinarian. These<br />
improvements were noted without concurrent use <strong>of</strong> medications or supplements. Body weight and body<br />
condition score remained <strong>the</strong> same so client education focused on <strong>the</strong> importance <strong>of</strong> weight management with<br />
appropriate reductions in food, limiting access <strong>to</strong> o<strong>the</strong>r pet food and incr<strong>ease</strong>d levels <strong>of</strong> exercise.<br />
Hill’s ® Prescription Diet ® j/d Canine is clinically proven <strong>to</strong>:<br />
• Improve mobility in as few as 21 days 1,2,4<br />
• Reduce <strong>pain</strong> in dogs with arthritis 2,3<br />
• Help dogs with arthritis walk, run, and play better, and climb stairs more easily 1,2,4<br />
• Help improve <strong>the</strong> quality <strong>of</strong> life <strong>of</strong> dogs suffering from arthritis 2,4<br />
Hill’s ® Prescription Diet ® j/d Canine product attributes:<br />
• High levels <strong>of</strong> EPA intercept <strong>the</strong> genetic signal that causes cartilage damage<br />
• Omega-3 fatty acids help <strong>to</strong> maintain joint health<br />
• High L-carnitine levels help <strong>to</strong> burn fat while maintaining lean muscle mass<br />
• Added glucosamine and chondroitin sulfate help <strong>to</strong> provide building blocks for cartilage repair<br />
• Improved taste and highly palatable <strong>nutrition</strong> help <strong>to</strong> improve compliance<br />
1<br />
Dose titration effects <strong>of</strong> omega-3 fatty acids fed <strong>to</strong> dogs with <strong>osteoarthritis</strong> (3-month feeding study), 2003. Unpublished data.<br />
2<br />
Cross AR, Roush JK, Renberg WC, et al. Effects <strong>of</strong> feeding omega-3 fatty acids on clinical signs and force plate analysis in dogs with <strong>osteoarthritis</strong> (3-month feeding study), 2004. Unpublished data.<br />
3<br />
A multi-center, practice-based study <strong>of</strong> <strong>the</strong>rapeutic food and a nonsteroidal anti-inflamma<strong>to</strong>ry drug in dogs with <strong>osteoarthritis</strong> (3-month feeding study), 2004. Unpublished data.<br />
4<br />
Dodd CE, Fritsch DA, Allen TA, et al. Omega-3 fatty acids in canine <strong>osteoarthritis</strong>: a randomized, double-masked study (6-month feeding study), 2004. Unpublished data.
<strong>nutrition</strong> myths and truths, facts and fallacies<br />
Acknowledgements<br />
Thanks <strong>to</strong> Dr. James Roush <strong>of</strong> Kansas State University and Dr. Tara Enwiller <strong>of</strong> Gilbert, Arizona, for providing<br />
information about this patient.<br />
Bibliography<br />
Paster ER, LaFond E, Biery DN, et al. Estimates <strong>of</strong> prevalence <strong>of</strong> hip dysplasia in Golden Retrievers and<br />
Rottweilers and <strong>the</strong> influence <strong>of</strong> bias on published prevalence figures. Journal <strong>of</strong> <strong>the</strong> American Veterinary<br />
Medical Association 2005;226(3):387-392.<br />
Harari J. Clinical evaluation <strong>of</strong> <strong>the</strong> osteoarthritic patient. Vet Clin N Am. 1997;27(4):725-734.<br />
May SA. Degenerative joint dis<strong>ease</strong> (Osteoarthritis, Osteoarthrosis, Secondary Joint Dis<strong>ease</strong>). In Houl<strong>to</strong>n JEF,<br />
Collinson RW (eds): Manual <strong>of</strong> Small Animal Arthrology. British Small Animal Veterinary Association. Iowa State<br />
University Press, 1994, p 62.<br />
Wener LL. Arthrocentesis and joint fluid analysis: Diagnostic applications in joint dis<strong>ease</strong>s <strong>of</strong> small animals.<br />
Compendium on Continuing Education. 1979;1:855-862.<br />
McLaughlin RM. Management <strong>of</strong> chronic osteoarthritic <strong>pain</strong>. Vet Clin North Am Sm Anim Pract. 2000;30:933-949.<br />
Goldring MB. The role <strong>of</strong> <strong>the</strong> chondrocyte in <strong>osteoarthritis</strong>. Arthritis Rheum. 2000;43:1916-1926.<br />
Denko CW, Malemud CJ. Metabolic disturbances and synovial joint responses in <strong>osteoarthritis</strong>. Frontiers<br />
Bioscience. 1999;4:686-693.<br />
Martel-Pelletier J, Alaaeddine N, Pelletier JP. Cy<strong>to</strong>kines and <strong>the</strong>ir role in <strong>the</strong> pathophysiology <strong>of</strong> <strong>osteoarthritis</strong>.<br />
Frontiers Bioscience. 1999;4:694-703.<br />
Holderbaum D, Haqqi TM, Moskowitz RW. Genetics and <strong>osteoarthritis</strong>; exposing <strong>the</strong> iceberg. Arthritis Rheum.<br />
1999;42:397-405.<br />
Prockop DJ. Heritable <strong>osteoarthritis</strong>, diagnosis and possible modes <strong>of</strong> cell and gene <strong>the</strong>rapy. Osteoarthritis and<br />
Cartilage. 1999;7:354-366.<br />
Martel-Pelletier J. Pathophysiology <strong>of</strong> <strong>osteoarthritis</strong>. Osteoarthritis and Cartilage. 1999;7:371-373.<br />
Goldring MB. The role <strong>of</strong> cy<strong>to</strong>kines as inflamma<strong>to</strong>ry media<strong>to</strong>rs in <strong>osteoarthritis</strong>: Lessons from animal models.<br />
Conn Tissue Res. 1999;40:1-11.<br />
Bassler C, Henrotin Y, Franchiment P. In vitro evaluation <strong>of</strong> drugs proposed as chondroprotective agents. Int J<br />
Tissue React. 1992;14:231-241.<br />
Ben<strong>to</strong>n HP, Vasseur PB, Broderick-Villa GA, Koolpe M. Effect <strong>of</strong> carpr<strong>of</strong>en on sulfated glycosaminoglycan<br />
metabolism, protein syn<strong>the</strong>sis, and prostaglandin rel<strong>ease</strong> by cultured osteoarthritic canine chondrocytes. Am J<br />
Vet Res. 1997;58:286-292.<br />
Bucci, LR. Chondroprotective agents: glucosamine salts and chondroitin sulphate. Townsend Letter for Doc<strong>to</strong>rs,<br />
1994;Jan:52-54.<br />
Eisele I, Wood IS, German AJ, et al. Adipokine gene expression in dog adipose tissues and dog white adipocytes<br />
differentiated in primary culture. Hormone and Metabolic Research 2005;37(8):474-481.<br />
Tryahurn P, and Wood IS. Adipokines: inflammation and <strong>the</strong> pleiotropic role <strong>of</strong> white adipose tissue. The British<br />
Journal <strong>of</strong> Nutrition 2004;92(3):347-355.<br />
Burkholder WJ, Taylor L, Hulse DA. Weight loss <strong>to</strong> optimal body condition incr<strong>ease</strong>s ground reactive forces in<br />
dogs with <strong>osteoarthritis</strong> (abstract) , in Proceedings. Purina Nutrition Forum 2000:74.<br />
10
<strong>nutrition</strong> myths and truths, facts and fallacies<br />
Impellizeri JA, Tetrick MA, Muir P. Effect <strong>of</strong> weight reduction on clinical signs <strong>of</strong> lameness in dogs with hip<br />
<strong>osteoarthritis</strong>. J Am Vet Med Assoc 2000;216:1089-1091.<br />
Budsberg S, Bartges J, Schoenherr B, et al. Effects <strong>of</strong> different n6:n3 fatty acid diets on canine stifle<br />
<strong>osteoarthritis</strong> (abstract), in Proceedings. Veterinary Orthopedic Society Annual Conference 2001;28:40.<br />
Caterson B, Flannery CR, Hughes CE, et al. Mechanisms involved in cartilage proteoglycan catabolism. Matrix<br />
Biology 2000;19:333-344.<br />
Curtis CL, Hughes CE, Flannery CR, et al. n-3 fatty acids specifically modulate catabolic fac<strong>to</strong>rs involved in<br />
articular cartilage degradation. J Biol Chem 2000;275:721-724.<br />
Curtis CL, Rees SG, Cramp J, et al. Effects <strong>of</strong> n-3 fatty acids on cartilage metabolism. Proc Nutr Soc<br />
2002;61:381-389.<br />
Dodd CE. Multicenter clinical study on <strong>the</strong> effect <strong>of</strong> an investigational food containing elevated omega-3 fatty<br />
acids on canine <strong>osteoarthritis</strong> clinical signs. Final report. Hill’s Pet Nutrition Center, 2004.<br />
Hansen RA, Allen KGD, Pluhar EG, et al. N-3 fatty acids decr<strong>ease</strong> inflamma<strong>to</strong>ry media<strong>to</strong>rs in arthritic dogs<br />
(abstract), in Proceedings. FASEB 2003.<br />
Kealy RD, Olsson SE, Monti JL, et al. Effects <strong>of</strong> limited food consumption on <strong>the</strong> incidence <strong>of</strong> hip dysplasia in<br />
growing dogs. J Am Vet Med Assoc 1992;201:857-863.<br />
Kealy RD, Lawler DF, Ballam JM, et al. Five-year longitudinal study on limited food consumption and<br />
development <strong>of</strong> <strong>osteoarthritis</strong> in cox<strong>of</strong>emoral joints <strong>of</strong> dogs. J Am Vet Med Assoc 1997;210:222-225.<br />
Kealy RD, Lawler DF, Ballam JM, et al. Evaluation <strong>of</strong> <strong>the</strong> effect <strong>of</strong> limited food consumption on <strong>the</strong> radiographic<br />
evidence <strong>of</strong> <strong>osteoarthritis</strong> in dogs. J Am Vet Med Assoc 2000;217:1678-1680.<br />
11
<strong>nutrition</strong> myths and truths, facts and fallacies<br />
Ron McLaughlin, DVM, DVSc, DACVS, is Pr<strong>of</strong>essor and Chief <strong>of</strong> Small<br />
Animal Surgery and Head <strong>of</strong> <strong>the</strong> Department <strong>of</strong> Clinical Sciences at Mississippi<br />
State University College <strong>of</strong> Veterinary Medicine. His primary areas <strong>of</strong> interest<br />
include <strong>the</strong> clinical areas <strong>of</strong> surgery, orthopedics and lameness. His research<br />
interests include orthopedics, gait analysis and biomechanics.<br />
®/ Hill’s, Prescription Diet and j/d trademarks are owned by Hill’s Pet Nutrition Inc. Adequan is a registered trademark owned by Luitpold Pharmaceuticals, Inc.<br />
Cosequin is a registered trademark <strong>of</strong> Nutrimax Labora<strong>to</strong>ries, Inc. ©2008 Hill’s Pet Nutrition, Inc.<br />
12