Gait disorder in older adults: Is it NPH? - ResearchGate
Gait disorder in older adults: Is it NPH? - ResearchGate
Gait disorder in older adults: Is it NPH? - ResearchGate
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
2.5<br />
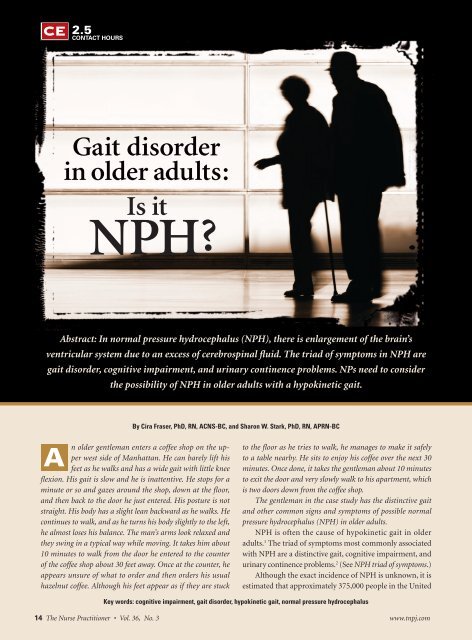
<strong>Ga<strong>it</strong></strong> <strong>disorder</strong> <strong>in</strong> <strong>older</strong> <strong>adults</strong>: <strong>Is</strong> <strong>it</strong> <strong>NPH</strong>?<br />
CONTACT HOURS<br />
<strong>Ga<strong>it</strong></strong> <strong>disorder</strong><br />
<strong>in</strong> <strong>older</strong> <strong>adults</strong>:<br />
<strong>Is</strong> <strong>it</strong><br />
<strong>NPH</strong>?<br />
Abstract: In normal pressure hydrocephalus (<strong>NPH</strong>), there is enlargement of the bra<strong>in</strong>’s<br />
ventricular system due to an excess of cerebrosp<strong>in</strong>al fluid. The triad of symptoms <strong>in</strong> <strong>NPH</strong> are<br />
ga<strong>it</strong> <strong>disorder</strong>, cogn<strong>it</strong>ive impairment, and ur<strong>in</strong>ary cont<strong>in</strong>ence problems. NPs need to consider<br />
the possibil<strong>it</strong>y of <strong>NPH</strong> <strong>in</strong> <strong>older</strong> <strong>adults</strong> w<strong>it</strong>h a hypok<strong>in</strong>etic ga<strong>it</strong>.<br />
A<br />
By Cira Fraser, PhD, RN, ACNS-BC, and Sharon W. Stark, PhD, RN, APRN-BC<br />
n <strong>older</strong> gentleman enters a coffee shop on the upper<br />
west side of Manhattan. He can barely lift his<br />
feet as he walks and has a wide ga<strong>it</strong> w<strong>it</strong>h l<strong>it</strong>tle knee<br />
flexion. His ga<strong>it</strong> is slow and he is <strong>in</strong>attentive. He stops for a<br />
m<strong>in</strong>ute or so and gazes around the shop, down at the floor,<br />
and then back to the door he just entered. His posture is not<br />
straight. His body has a slight lean backward as he walks. He<br />
cont<strong>in</strong>ues to walk, and as he turns his body slightly to the left,<br />
he almost loses his balance. The man’s arms look relaxed and<br />
they sw<strong>in</strong>g <strong>in</strong> a typical way while mov<strong>in</strong>g. It takes him about<br />
10 m<strong>in</strong>utes to walk from the door he entered to the counter<br />
of the coffee shop about 30 feet away. Once at the counter, he<br />
appears unsure of what to order and then orders his usual<br />
hazelnut coffee. Although his feet appear as if they are stuck<br />
to the floor as he tries to walk, he manages to make <strong>it</strong> safely<br />
to a table nearby. He s<strong>it</strong>s to enjoy his coffee over the next 30<br />
m<strong>in</strong>utes. Once done, <strong>it</strong> takes the gentleman about 10 m<strong>in</strong>utes<br />
to ex<strong>it</strong> the door and very slowly walk to his apartment, which<br />
is two doors down from the coffee shop.<br />
The gentleman <strong>in</strong> the case study has the dist<strong>in</strong>ctive ga<strong>it</strong><br />
and other common signs and symptoms of possible normal<br />
pressure hydrocephalus (<strong>NPH</strong>) <strong>in</strong> <strong>older</strong> <strong>adults</strong>.<br />
<strong>NPH</strong> is often the cause of hypok<strong>in</strong>etic ga<strong>it</strong> <strong>in</strong> <strong>older</strong><br />
<strong>adults</strong>. 1 The triad of symptoms most commonly associated<br />
w<strong>it</strong>h <strong>NPH</strong> are a dist<strong>in</strong>ctive ga<strong>it</strong>, cogn<strong>it</strong>ive impairment, and<br />
ur<strong>in</strong>ary cont<strong>in</strong>ence problems. 2 (See <strong>NPH</strong> triad of symptoms.)<br />
Although the exact <strong>in</strong>cidence of <strong>NPH</strong> is unknown, <strong>it</strong> is<br />
estimated that approximately 375,000 people <strong>in</strong> the Un<strong>it</strong>ed<br />
Key words: cogn<strong>it</strong>ive impairment, ga<strong>it</strong> <strong>disorder</strong>, hypok<strong>in</strong>etic ga<strong>it</strong>, normal pressure hydrocephalus<br />
14 The Nurse Pract<strong>it</strong>ioner • Vol. 36, No. 3 www.tnpj.com<br />
Copyright © 2011 Lipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s. Unauthorized reproduction of this article is prohib<strong>it</strong>ed.
<strong>Ga<strong>it</strong></strong> <strong>disorder</strong> <strong>in</strong> <strong>older</strong> <strong>adults</strong>: <strong>Is</strong> <strong>it</strong> <strong>NPH</strong>?<br />
States, or 5% of the population may have <strong>NPH</strong>. The numbers<br />
are expected to <strong>in</strong>crease due to extended longev<strong>it</strong>y. 3 In<br />
2005, an <strong>in</strong>ternational study group developed and reported<br />
comprehensive guidel<strong>in</strong>es for <strong>NPH</strong>. 3<br />
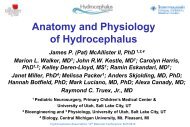
In <strong>NPH</strong>, there is an enlargement of the bra<strong>in</strong>’s ventricular<br />
system due to an excess of cerebrosp<strong>in</strong>al fluid (CSF) thought to<br />
be related to decreased reabsorption of CSF by the arachnoid<br />
villi surround<strong>in</strong>g the exterior of the bra<strong>in</strong> (see Normal flow of<br />
CSF). As the ventricles slowly enlarge from the accumulation<br />
of CSF, tissue compliance <strong>in</strong>creases and further ventricular<br />
enlargement results. 4 Subsequently, <strong>in</strong>creased <strong>in</strong>tracranial<br />
pressure is transient as the ventricles are able to accomodate<br />
more CSF. As the ventricles cont<strong>in</strong>ue to enlarge, edema, and<br />
permanent changes <strong>in</strong> the shape of the ventricles may cause<br />
periventricular and vascular damage. Add<strong>it</strong>ionally, compression<br />
of bra<strong>in</strong> parenchyma and vessels and the accumulation of<br />
tox<strong>in</strong>s due to slow refreshment of CSF and decreased clearance<br />
of metabol<strong>it</strong>es <strong>in</strong>creases CSF-flow obstruction and progressive<br />
ventriculomegaly. Signs and symptoms of <strong>NPH</strong> occur as<br />
various areas of the bra<strong>in</strong> are compressed. 4<br />
The etiology of <strong>NPH</strong> is unclear. Chrysikopoulos 4 states<br />
the perplex<strong>in</strong>g feature of <strong>NPH</strong> is the progressive enlargement<br />
of the ventricles <strong>in</strong> the absence of mechanical obstruction<br />
of CSF, along w<strong>it</strong>h a normal mean <strong>in</strong>traventricular and<br />
mean <strong>in</strong>tracranial pressure. <strong>NPH</strong> can be e<strong>it</strong>her idiopathic<br />
or secondary to head trauma, men<strong>in</strong>g<strong>it</strong>is, or subarachnoid<br />
bleed. The author hypothesized that <strong>in</strong> <strong>NPH</strong>, alterations<br />
<strong>in</strong> the normal systolic-diastolic cycle of blood flow <strong>in</strong> the<br />
bra<strong>in</strong> will disrupt the normal propulsion of CSF. Abnormal<br />
ventricular systole <strong>in</strong> the bra<strong>in</strong> is thought to be caused by<br />
stiff and narrowed arteries due to atherosclerosis and hypertension.<br />
4 Poor circulation of CSF is proposed to result <strong>in</strong><br />
toxic/osmotic effects that may <strong>in</strong>clude cellular and axonal<br />
dehydration. Chrysikopoulos 4 states there is evidence l<strong>in</strong>k<strong>in</strong>g<br />
<strong>NPH</strong> to diseases of the cerebral arteries.<br />
Krauss et al 5 <strong>in</strong>vestigated vascular risk factors and arteriosclerotic<br />
disease <strong>in</strong> <strong>NPH</strong> <strong>in</strong> <strong>older</strong> <strong>adults</strong>. The sample<br />
<strong>in</strong>cluded 65 participants who ranged <strong>in</strong> age from 50 to 87<br />
w<strong>it</strong>h a mean age of 70.8 years. Forty-six percent were men,<br />
and 54% were women. Variables exam<strong>in</strong>ed <strong>in</strong>cluded systemic<br />
arterial hypertension, diabetes mell<strong>it</strong>us, smok<strong>in</strong>g, hyperlipidemia,<br />
hypercholesterolemia, obes<strong>it</strong>y, and cardiac, cerebrovascular,<br />
and other arteriosclerotic disease. A highly significant<br />
association was found between <strong>NPH</strong> and systemic arterial<br />
hypertension. A pos<strong>it</strong>ive relationship was also found between<br />
the sever<strong>it</strong>y of cl<strong>in</strong>ical symptoms of <strong>NPH</strong> and the presence<br />
of systemic arterial hypertension, especially for severe ga<strong>it</strong><br />
disturbance. Diabetes mell<strong>it</strong>us was found to be associated<br />
w<strong>it</strong>h <strong>NPH</strong>; however, when the variables were exam<strong>in</strong>ed us<strong>in</strong>g<br />
logistic regression, only systemic arterial hypertension was<br />
found to have a significant association w<strong>it</strong>h <strong>NPH</strong>.<br />
S<strong>in</strong>ce <strong>NPH</strong> typically is most common <strong>in</strong> <strong>in</strong>dividuals <strong>in</strong><br />
their sixth and seventh decades, <strong>it</strong>s characteristic triad of<br />
symptoms can be easily mistaken for other cond<strong>it</strong>ions attributed<br />
to ag<strong>in</strong>g, thereby delay<strong>in</strong>g <strong>it</strong>s diagnosis. 6 The diagnosis<br />
of <strong>NPH</strong> does not require the presence of all three symptoms.<br />
The first symptom to be exhib<strong>it</strong>ed is usually a change <strong>in</strong> ga<strong>it</strong>,<br />
while cogn<strong>it</strong>ive and ur<strong>in</strong>ary changes occur later. In fact, if<br />
cogn<strong>it</strong>ive impairment occurs before disturbances <strong>in</strong> ga<strong>it</strong> then<br />
<strong>NPH</strong> is probably not present. 7,8<br />
■ Dist<strong>in</strong>ctive ga<strong>it</strong> of <strong>NPH</strong><br />
<strong>NPH</strong> is a diagnostic challenge w<strong>it</strong>h ga<strong>it</strong> impairment as the<br />
card<strong>in</strong>al sign. 9 <strong>Ga<strong>it</strong></strong> disturbance is an early sign of <strong>NPH</strong>.<br />
The dist<strong>in</strong>ctive ga<strong>it</strong> is described as hav<strong>in</strong>g reduced veloc<strong>it</strong>y,<br />
dim<strong>in</strong>ished stride length, broad-based, and reduced<br />
foot-to-floor clearance. There is an <strong>in</strong>creased foot angle,<br />
w<strong>it</strong>h the feet rotated outward. 10 Step height is greatly<br />
dim<strong>in</strong>ished, giv<strong>in</strong>g the appearance that the person’s feet<br />
are stuck to the floor. 1<br />
Older <strong>adults</strong> w<strong>it</strong>h <strong>NPH</strong> tend to hes<strong>it</strong>ate when <strong>in</strong><strong>it</strong>iat<strong>in</strong>g<br />
ambulation or turn<strong>in</strong>g. They are unsteady and lose their<br />
balance easily. <strong>NPH</strong> is dist<strong>in</strong>guished from a similar ga<strong>it</strong> <strong>in</strong><br />
Park<strong>in</strong>son disease by the preservation of reciprocal arm<br />
sw<strong>in</strong>g when walk<strong>in</strong>g. 11 Also, a levodopa challenge may be<br />
done to differentiate between <strong>NPH</strong> and Park<strong>in</strong>son disease.<br />
Patients w<strong>it</strong>h <strong>NPH</strong> will not respond to levadopa. 12<br />
Those w<strong>it</strong>h <strong>NPH</strong> struggle to rise from a seated pos<strong>it</strong>ion<br />
and have difficulty <strong>in</strong><strong>it</strong>iat<strong>in</strong>g the first steps <strong>in</strong> walk<strong>in</strong>g. Climb<strong>in</strong>g<br />
stairs may be problematic, as their step height is dim<strong>in</strong>ished<br />
and their stride length is shortened. Some patients may<br />
only present w<strong>it</strong>h a history of frequent falls. 7,13 Individuals<br />
w<strong>it</strong>h <strong>NPH</strong> may also appear to lean backwards slightly when<br />
stand<strong>in</strong>g and ambulat<strong>in</strong>g and have a larger sway area than<br />
healthy <strong>in</strong>dividuals. 14<br />
■ Cogn<strong>it</strong>ive impairment<br />
Cogn<strong>it</strong>ive impairments <strong>in</strong> <strong>NPH</strong> can range from m<strong>in</strong>imally<br />
detected to profoundly severe. Over time, cogn<strong>it</strong>ive impairments<br />
may become more generalized and more difficult to<br />
manage. 2 In <strong>NPH</strong>, cogn<strong>it</strong>ive impairment typically <strong>in</strong>cludes<br />
<strong>in</strong>attentiveness, lack of spontane<strong>it</strong>y, and latency <strong>in</strong> recall. The<br />
process<strong>in</strong>g of <strong>in</strong>formation tends to be slow. A fact recalled<br />
by a person w<strong>it</strong>h <strong>NPH</strong> is most often accurate. The answers<br />
provided to questions are frequently correct. The dementia<br />
from <strong>NPH</strong> is dist<strong>in</strong>ct from that noted <strong>in</strong> a person w<strong>it</strong>h Alzheimer<br />
disease (AD). The <strong>in</strong>dividual w<strong>it</strong>h <strong>NPH</strong> should not<br />
have difficulty w<strong>it</strong>h word formation or carry<strong>in</strong>g out simple<br />
tasks that do not require concentration. 13<br />
Differentiat<strong>in</strong>g between cortical and subcortical defic<strong>it</strong>s<br />
is key to dist<strong>in</strong>guish<strong>in</strong>g <strong>NPH</strong> from other cogn<strong>it</strong>ive<br />
impairments and dementias. If cogn<strong>it</strong>ive impairment is<br />
www.tnpj.com The Nurse Pract<strong>it</strong>ioner • March 2011 15<br />
Copyright © 2011 Lipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s. Unauthorized reproduction of this article is prohib<strong>it</strong>ed.
<strong>Ga<strong>it</strong></strong> <strong>disorder</strong> <strong>in</strong> <strong>older</strong> <strong>adults</strong>: <strong>Is</strong> <strong>it</strong> <strong>NPH</strong>?<br />
<strong>NPH</strong> triad of symptoms 1,2,10,11,13<br />
<strong>Ga<strong>it</strong></strong> disturbance<br />
• Appears before cogn<strong>it</strong>ive or ur<strong>in</strong>ary symptoms<br />
• Reduced veloc<strong>it</strong>y<br />
• Dim<strong>in</strong>ished stride length<br />
• Broad based<br />
• Reduced floor-to-foot clearance<br />
• Dim<strong>in</strong>ished step height<br />
• Increased foot angle<br />
• Feet rotated outward<br />
• Feet appear to be stuck to the floor<br />
• Hes<strong>it</strong>ates when <strong>in</strong><strong>it</strong>iat<strong>in</strong>g ambulation<br />
• Hes<strong>it</strong>ates when turn<strong>in</strong>g<br />
• Unsteady<br />
• Loses balance easily<br />
• Normal reciprocal arm sw<strong>in</strong>g when walk<strong>in</strong>g<br />
Cogn<strong>it</strong>ive impairment<br />
• Inattentiveness<br />
• Lack of spontane<strong>it</strong>y<br />
• Latency <strong>in</strong> recall<br />
• Slowed process<strong>in</strong>g of <strong>in</strong>formation<br />
• Fact recall most often accurate<br />
• Answers provided to questions frequently correct<br />
• No difficulty w<strong>it</strong>h word formation<br />
• Can carry out simple tasks<br />
Ur<strong>in</strong>ary cont<strong>in</strong>ence problems<br />
• Perception of press<strong>in</strong>g need to void<br />
• Ur<strong>in</strong>ary frequency more than six void<strong>in</strong>g episodes <strong>in</strong><br />
12 hours<br />
• Nocturia more than twice <strong>in</strong> an average night<br />
• Episodic <strong>in</strong>cont<strong>in</strong>ence<br />
• Persistent <strong>in</strong>cont<strong>in</strong>ence (later sign)<br />
the predom<strong>in</strong>ant symptom, <strong>it</strong> is not likely that <strong>NPH</strong> is<br />
present. 7,8 Symptoms such as memory loss and aphasia are<br />
the result of a dysfunction <strong>in</strong> the cortex and are not likely<br />
to be associated w<strong>it</strong>h <strong>NPH</strong>. 7,13 AD <strong>in</strong> conjunction w<strong>it</strong>h<br />
<strong>NPH</strong> is common among the elderly w<strong>it</strong>h hypertension. 15<br />
■ Ur<strong>in</strong>ary cont<strong>in</strong>ence problems<br />
Ur<strong>in</strong>ary cont<strong>in</strong>ence issues <strong>in</strong> <strong>NPH</strong> primarily <strong>in</strong>volve ur<strong>in</strong>ary<br />
urgency and frequency. These early symptoms can<br />
later progress to ur<strong>in</strong>ary <strong>in</strong>cont<strong>in</strong>ence. Ur<strong>in</strong>ary cont<strong>in</strong>ence<br />
problems may <strong>in</strong>clude episodic or persistent ur<strong>in</strong>ary <strong>in</strong>cont<strong>in</strong>ence<br />
and frequent perception of a press<strong>in</strong>g need to<br />
void. Ur<strong>in</strong>ary frequency <strong>in</strong> <strong>NPH</strong> is typically more than six<br />
void<strong>in</strong>g episodes <strong>in</strong> 12 hours desp<strong>it</strong>e lim<strong>it</strong>ed fluid <strong>in</strong>take.<br />
Also nocturia more than twice <strong>in</strong> an average night is common<br />
<strong>in</strong> <strong>NPH</strong>. 2 Underly<strong>in</strong>g medical problems, such as benign<br />
prostatic hyperplasia, bladder cancer, neurogenic bladder,<br />
and cyst<strong>it</strong>is should be considered before attribut<strong>in</strong>g ur<strong>in</strong>ary<br />
symptoms to <strong>NPH</strong>. Also the use of diuretics, anticholenergics,<br />
and other medications may be the cause of ur<strong>in</strong>ary<br />
urgency and frequency. 7,13<br />
■ Add<strong>it</strong>ional problems associated w<strong>it</strong>h <strong>NPH</strong><br />
In add<strong>it</strong>ion to the triad of symptoms most often associated<br />
w<strong>it</strong>h <strong>NPH</strong>, there are a number of add<strong>it</strong>ional problems<br />
that may occur <strong>in</strong> <strong>NPH</strong>. Affected neuropsychologic<br />
and cogn<strong>it</strong>ive functions may <strong>in</strong>clude, but are not lim<strong>it</strong>ed<br />
to, short-term memory, numeracy (math skills needed to<br />
cope w<strong>it</strong>h everyday life), abstract thought, concentration,<br />
dexter<strong>it</strong>y, and wr<strong>it</strong><strong>in</strong>g skills. In add<strong>it</strong>ion, behavioral and<br />
psychiatric changes observed <strong>in</strong> <strong>NPH</strong> may <strong>in</strong>clude awaken<strong>in</strong>g<br />
fluctuations, fantastic confabulation, reduced alertness,<br />
easily fatigued, apathy, bipolar <strong>disorder</strong>, depression, and<br />
obsessive-compulsive <strong>disorder</strong>. 10<br />
■ Health history and assessment<br />
A thorough health history and physical exam are essential to<br />
efficiently and accurately diagnose <strong>NPH</strong> so that treatment<br />
can beg<strong>in</strong> quickly. Delayed diagnosis and treatment have<br />
negative effects on the patient’s prognosis. 6,16<br />
A thorough patient history of symptom onset and<br />
progression, medical history of both the patient and the<br />
family, and past and present medications are important<br />
components of the evaluation. 8,16,17 A detailed ga<strong>it</strong> history<br />
should be obta<strong>in</strong>ed from the patient and family about the<br />
onset of walk<strong>in</strong>g problems and whether the ga<strong>it</strong> problems<br />
had a sudden onset or a gradual decl<strong>in</strong>e. A gradual decl<strong>in</strong>e<br />
is consistent w<strong>it</strong>h <strong>NPH</strong>. 7 Many other diseases present w<strong>it</strong>h<br />
similar symptoms as <strong>NPH</strong> and must be considered <strong>in</strong> the<br />
differential diagnoses. Headache, visual disturbances, and<br />
nausea may be present as a result of the <strong>in</strong>creased <strong>in</strong>tracranial<br />
pressure. 8,16,17<br />
<strong>Ga<strong>it</strong></strong> should be assessed for reduced veloc<strong>it</strong>y, dim<strong>in</strong>ished<br />
stride length, broad-based stance, and reduced foot-to-floor<br />
clearance. Also assess for an <strong>in</strong>creased foot angle, w<strong>it</strong>h the<br />
feet rotated outward. 10 A greatly dim<strong>in</strong>ished step height gives<br />
the appearance that the person’s feet are stuck to the floor. 1<br />
Hes<strong>it</strong>ation when the <strong>in</strong>dividual <strong>in</strong><strong>it</strong>iates ambulation and when<br />
turn<strong>in</strong>g, unstead<strong>in</strong>ess, and loss of balance are consistent w<strong>it</strong>h<br />
<strong>NPH</strong>. 11 The ga<strong>it</strong> of <strong>NPH</strong> is dist<strong>in</strong>guished from that of Park<strong>in</strong>son<br />
through observation of postur<strong>in</strong>g and arm sw<strong>in</strong>g. 11,14<br />
A cogn<strong>it</strong>ive evaluation will typically reveal mild cogn<strong>it</strong>ive<br />
impairments present<strong>in</strong>g as <strong>in</strong>attentiveness, lack of<br />
spontane<strong>it</strong>y, and latency <strong>in</strong> recall. 13 Although the process<strong>in</strong>g<br />
of <strong>in</strong>formation tends to be slow, memory recall is accurate<br />
and answers to questions are mostly correct. Unlike those<br />
w<strong>it</strong>h Alzheimer disease, <strong>in</strong>dividuals w<strong>it</strong>h <strong>NPH</strong> can carry<br />
out simple tasks and do not experience difficulty w<strong>it</strong>h word<br />
formation and understand<strong>in</strong>g. 7,13 Cogn<strong>it</strong>ive evaluation<br />
us<strong>in</strong>g standardized neuropsychologic evaluation tools are<br />
useful <strong>in</strong> identify<strong>in</strong>g cogn<strong>it</strong>ive impairments and dementias. 6<br />
Ur<strong>in</strong>ary cont<strong>in</strong>ence issues are identified dur<strong>in</strong>g history<br />
tak<strong>in</strong>g and can be further evaluated through urodynamic<br />
16 The Nurse Pract<strong>it</strong>ioner • Vol. 36, No. 3 www.tnpj.com<br />
Copyright © 2011 Lipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s. Unauthorized reproduction of this article is prohib<strong>it</strong>ed.
<strong>Ga<strong>it</strong></strong> <strong>disorder</strong> <strong>in</strong> <strong>older</strong> <strong>adults</strong>: <strong>Is</strong> <strong>it</strong> <strong>NPH</strong>?<br />
evaluation. It is a late sign <strong>in</strong> <strong>NPH</strong><br />
patients and patients will <strong>in</strong><strong>it</strong>ially<br />
relate that they experience ur<strong>in</strong>ary<br />
urgency, frequency, and nocturia.<br />
Other underly<strong>in</strong>g medical<br />
issues and/medications need to<br />
be ruled out before attribut<strong>in</strong>g<br />
<strong>in</strong>cont<strong>in</strong>ence to <strong>NPH</strong>. 2,7,13<br />
■ Diagnostic tests<br />
Standardized neuropsychologic<br />
tests are useful for identify<strong>in</strong>g<br />
cogn<strong>it</strong>ive impairment and to dist<strong>in</strong>quish<br />
subcortical from cortical<br />
dementias. 6 There are several<br />
screen<strong>in</strong>g <strong>in</strong>struments useful to<br />
determ<strong>in</strong>e cogn<strong>it</strong>ive defic<strong>it</strong>s <strong>in</strong><br />
those w<strong>it</strong>h <strong>NPH</strong>. The M<strong>in</strong>i-Cog<br />
and Short Portable Mental Status<br />
Questionnaire are useful to<br />
identify cogn<strong>it</strong>ive impairment,<br />
and the Folste<strong>in</strong> M<strong>in</strong>i-Mental<br />
State Exam<strong>in</strong>ation can identify<br />
the sever<strong>it</strong>y of cogn<strong>it</strong>ive impairment.<br />
Visuospatial skills and executive<br />
function are assessed w<strong>it</strong>h<br />
Normal flow of CSF<br />
the Clock Draw<strong>in</strong>g Test. 7 F<strong>in</strong>ally, the Geriatric Depression<br />
Scale identifies depression that may present as cogn<strong>it</strong>ive<br />
deficiencies. These tests are helpful <strong>in</strong> determ<strong>in</strong><strong>in</strong>g not only<br />
whether a person is a candidate for shunt<strong>in</strong>g, but also how<br />
successful the shunt<strong>in</strong>g is when completed. 6,7<br />
Cystoscopic and urodynamic test<strong>in</strong>g are useful <strong>in</strong> determ<strong>in</strong><strong>in</strong>g<br />
stress and/or overflow <strong>in</strong>cont<strong>in</strong>ence, as well as other<br />
causes of ur<strong>in</strong>ary symptoms such as benign prostatic hyperplasia,<br />
bladder cancer, neurogenic bladder, and cyst<strong>it</strong>is. 18,19 A<br />
urodynamic evaluation will show hyperactiv<strong>it</strong>y of the bladder. 8<br />
Radiographic imag<strong>in</strong>g is used to support the diagnosis<br />
of <strong>NPH</strong>, as well as rul<strong>in</strong>g out other causes of symptom<br />
presentation. In <strong>NPH</strong>, computed tomography (CT) scans<br />
reveal ventricular enlargement. Magnetic resonance imag<strong>in</strong>g<br />
(MRI) results reveal significantly <strong>in</strong>creased CSF <strong>in</strong> the<br />
ventricles of the bra<strong>in</strong>. There is also decreased CSF <strong>in</strong> the<br />
medial subarachnoid spaces when those w<strong>it</strong>h <strong>NPH</strong> are compared<br />
w<strong>it</strong>h those w<strong>it</strong>h vascular dementia or w<strong>it</strong>h Alzheimer<br />
disease. 20 The follow<strong>in</strong>g imag<strong>in</strong>g cr<strong>it</strong>eria may be helpful to<br />
ascerta<strong>in</strong> ideal candidates for shunt placement: ventriculomegaly,<br />
improvement of symptoms after CSF dra<strong>in</strong>age,<br />
normal-sized or occluded sylvian fissures and cortical sulci,<br />
absent or moderate wh<strong>it</strong>e matter lesions. 12<br />
In <strong>NPH</strong>, s<strong>in</strong>gle-photon emission computed tomography<br />
(SPECT) will reveal dim<strong>in</strong>ished cerebral blood flow that is<br />
The illustration below represents the normal flow of CSF from <strong>it</strong>s formation from<br />
blood <strong>in</strong> the choroid plexuses until <strong>it</strong>s return to the blood <strong>in</strong> the superior sag<strong>it</strong>tal s<strong>in</strong>us.<br />
Subarachnoid<br />
space<br />
Superior<br />
sag<strong>it</strong>tal<br />
s<strong>in</strong>us<br />
Lateral ventricle<br />
Interventricular<br />
foramen<br />
Pons<br />
Arachnoid villi<br />
Choroidal plexus<br />
fourth ventricle<br />
Foramen of Magendie<br />
Source: Porth CM, Matf<strong>in</strong>, G. Pathophysiology Concepts of Altered Health States. 8th ed. Philadelphia, PA:<br />
Wolters Kluwer Health/Lipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s, 2009.<br />
Choroidal<br />
plexus third<br />
ventricle<br />
common <strong>in</strong> <strong>NPH</strong>. Radionuclide cisternogram differentiates<br />
communicat<strong>in</strong>g from obstructive hydrocephalus and determ<strong>in</strong>es<br />
CSF flow after radioactive material is <strong>in</strong>fused <strong>in</strong>to the<br />
CSF and tracer activ<strong>it</strong>y identifies CSF outflow obstructions. 6,17,19<br />
Tests that <strong>in</strong>volve lumbar puncture show the most potential<br />
<strong>in</strong> diagnos<strong>in</strong>g <strong>NPH</strong> and also identify appropriate<br />
candidates for shunt placement. A lumbar puncture reveals<br />
normal CSF pressure and normal levels of prote<strong>in</strong>, glucose,<br />
and cell counts. 15 McGirt et al 21 conducted a 10-year retrospective<br />
study and found that <strong>NPH</strong> can be diagnosed accurately<br />
us<strong>in</strong>g a 3-day CSF dra<strong>in</strong>age trial via sp<strong>in</strong>al catheter or<br />
CSF pressure mon<strong>it</strong>or<strong>in</strong>g. The w<strong>it</strong>hdrawal of 50 mL of CSF<br />
is also used for the prognostic evaluation. There is vary<strong>in</strong>g<br />
specific<strong>it</strong>y and sens<strong>it</strong>iv<strong>it</strong>y evident <strong>in</strong> the medical l<strong>it</strong>erature.<br />
The removal of CSF reveals transient improvement <strong>in</strong> ga<strong>it</strong><br />
and cogn<strong>it</strong>ion. 22 A CSF <strong>in</strong>fusion test <strong>in</strong>volves <strong>in</strong>fusion of<br />
fluid <strong>in</strong>to the lumbar subarachnoid space to determ<strong>in</strong>e a<br />
patient’s capac<strong>it</strong>y to absorb CSF (CSF absorptive capac<strong>it</strong>y)<br />
and shows improvement <strong>in</strong> symptoms. Symptom improvement<br />
<strong>in</strong> any of these tests <strong>in</strong>dicates that ventricular shunt<strong>in</strong>g<br />
is an appropriate <strong>in</strong>tervention (See <strong>NPH</strong> diagnostic tests). 15<br />
■ Treatments<br />
<strong>NPH</strong> is often treated w<strong>it</strong>h a ventriculoper<strong>it</strong>oneal shunt (VP<br />
Shunt) to divert excess CSF away from the bra<strong>in</strong>. A ventricu-<br />
www.tnpj.com The Nurse Pract<strong>it</strong>ioner • March 2011 17<br />
Copyright © 2011 Lipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s. Unauthorized reproduction of this article is prohib<strong>it</strong>ed.
<strong>Ga<strong>it</strong></strong> <strong>disorder</strong> <strong>in</strong> <strong>older</strong> <strong>adults</strong>: <strong>Is</strong> <strong>it</strong> <strong>NPH</strong>?<br />
<strong>NPH</strong> diagnostic tests<br />
Neurologic<br />
• CT scan reveals ventricular enlargement 20<br />
• MRI reveals <strong>in</strong>creased CSF <strong>in</strong> the ventricles 12<br />
6, 17, 19<br />
• SPECT reveals dim<strong>in</strong>ished cerebral blood flow<br />
• Radionuclide cisternogram w<strong>it</strong>h radioactive tracer<br />
differentiates communicat<strong>in</strong>g from obstructive hydrocephalus,<br />
CSF flow, and outflow obstructions<br />
6, 17, 19<br />
• Lumbar puncture reveals CSF pressure, prote<strong>in</strong>,<br />
glucose, and cell counts 17<br />
• 3-day CSF dra<strong>in</strong>age trial via sp<strong>in</strong>al catheter or CSF<br />
pressure mon<strong>it</strong>or<strong>in</strong>g reveals transient improvement <strong>in</strong><br />
21, 22<br />
ga<strong>it</strong> and cogn<strong>it</strong>ion<br />
• CSF <strong>in</strong>fusion test determ<strong>in</strong>es CSF absorptive capac<strong>it</strong>y<br />
and improvement <strong>in</strong> symptoms 15<br />
Cogn<strong>it</strong>ive<br />
• The M<strong>in</strong>i-Cog evaluates level of cogn<strong>it</strong>ive abil<strong>it</strong>y 6, 7<br />
• Short Portable Mental Status Questionnaire evaluates<br />
level of cogn<strong>it</strong>ive abil<strong>it</strong>y 6, 7<br />
• Folste<strong>in</strong> M<strong>in</strong>i-Mental State Exam<strong>in</strong>ation evaluates level<br />
of cogn<strong>it</strong>ive abil<strong>it</strong>y 7<br />
• Clock Draw<strong>in</strong>g Test identifies visuospatial skills and<br />
executive function 7<br />
• Geriatric Depression Scale identifies depression 6, 7<br />
Urologic<br />
• Cystoscopic and urodynamic test<strong>in</strong>g determ<strong>in</strong>es<br />
causes of ur<strong>in</strong>ary symptoms 18,19<br />
• A urodynamic evaluation identifies bladder hyperactiv<strong>it</strong>y 8<br />
lar catheter is <strong>in</strong>serted <strong>in</strong>to the bra<strong>in</strong>, and CSF ex<strong>it</strong>s through<br />
a valve and is connected to a catheter that is tunneled under<br />
the sk<strong>in</strong> down to the per<strong>it</strong>oneal cav<strong>it</strong>y. 6,8,19<br />
Follow<strong>in</strong>g the <strong>in</strong>sertion of a VP shunt, care should <strong>in</strong>clude<br />
pos<strong>it</strong>ion<strong>in</strong>g the <strong>in</strong>dividual sup<strong>in</strong>e 12 to 24 hours<br />
and elevat<strong>in</strong>g the head of the bed gradually, follow<strong>in</strong>g the<br />
neurosurgeon’s protocol. This gradual elevation helps to<br />
prevent overshunt<strong>in</strong>g of CSF. 23 Overshunt<strong>in</strong>g can result <strong>in</strong><br />
collapse of the ventricles of the bra<strong>in</strong> and cause bleed<strong>in</strong>g.<br />
Acute <strong>in</strong>tracranial hemorrhage is the primary risk follow<strong>in</strong>g<br />
the <strong>in</strong>sertion of a VP shunt and tends to be underreported. 23<br />
A new laparoscopic technique is be<strong>in</strong>g used by some neurosurgeons<br />
to <strong>in</strong>sert the per<strong>it</strong>oneal portion of the VP shunt<br />
catheter. This new approach has a number of benef<strong>it</strong>s when<br />
compared w<strong>it</strong>h the trad<strong>it</strong>ional approach. The length of time<br />
for surgery is shorter, less trauma for the patient, and fewer<br />
complications, especially shunt obstruction. 24<br />
Individuals w<strong>it</strong>h a shorter duration of <strong>NPH</strong> symptoms<br />
and the presence of ga<strong>it</strong> impairment are likely to improve follow<strong>in</strong>g<br />
the <strong>in</strong>sertion of a VP shunt. 21 In a review of the l<strong>it</strong>erature<br />
back to 1966, Kl<strong>in</strong>ge, Marmarou, Bergsneider, Relk<strong>in</strong>, and<br />
Black 25 found that ga<strong>it</strong> improvement follow<strong>in</strong>g the <strong>in</strong>sertion<br />
of a VP shunt ranged from 30% to 95%. Improvement is not<br />
sudden, but occurs slowly over the weeks and months that<br />
follow the <strong>in</strong>sertion of the shunt. Improvement will persist<br />
as long as the shunt is work<strong>in</strong>g properly. 7<br />
Unlike other dementias, cogn<strong>it</strong>ive impairment <strong>in</strong> <strong>NPH</strong><br />
can, <strong>in</strong> some cases, be reversed. Patients w<strong>it</strong>h multiple medical<br />
problems should be thoroughly evaluated so that successful<br />
reversal of <strong>NPH</strong> is not delayed. Surgical shunt<strong>in</strong>g provides<br />
the most benef<strong>it</strong> when performed early <strong>in</strong> the disease process.<br />
Shprecher, Schwalb, and Kurlan 15 reported that AD, <strong>in</strong><br />
comb<strong>in</strong>ation w<strong>it</strong>h <strong>NPH</strong>, is common among the elderly w<strong>it</strong>h<br />
hypertension. Although shunt<strong>in</strong>g may improve ga<strong>it</strong> dysfunction,<br />
severe dementia does not improve. Therefore, shunt<strong>in</strong>g<br />
<strong>in</strong> patients w<strong>it</strong>h severe dementia is discouraged.<br />
■ Complications<br />
Shunt complication are estimated to be as follows: <strong>in</strong>tracerebral<br />
hematoma 3%, <strong>in</strong>fection 6%, seizure activ<strong>it</strong>y 3% to<br />
11%, subdural hematoma 2% to 17%, and shunt malfunction<br />
20%. 23 Malfunction <strong>in</strong>cludes obstruction and overand<br />
underdra<strong>in</strong>age of CSF. Shunt obstruction is the most<br />
common complication and should be suspected when there<br />
is no improvement <strong>in</strong> symptoms or if symptoms recur. 8,12<br />
■ Implications for practice<br />
NPs and other healthcare professionals are likely to recognize<br />
the symptoms of <strong>NPH</strong> <strong>in</strong> <strong>older</strong> <strong>adults</strong> and make a difference<br />
<strong>in</strong> the qual<strong>it</strong>y of life of <strong>older</strong> <strong>adults</strong> and their family members.<br />
Fraser and Fraser 26 state that all healthcare professionals need<br />
to become familiar w<strong>it</strong>h the ga<strong>it</strong> <strong>in</strong> <strong>NPH</strong>. The ga<strong>it</strong> is the card<strong>in</strong>al<br />
sign of <strong>NPH</strong>. The abil<strong>it</strong>y to recognize the <strong>NPH</strong> ga<strong>it</strong> can<br />
be sharpened by observ<strong>in</strong>g those recently diagnosed, those<br />
who just had a shunt <strong>in</strong>serted, or by review<strong>in</strong>g a video of the<br />
dist<strong>in</strong>ctive ga<strong>it</strong>. 27 When a patient presents w<strong>it</strong>h the dist<strong>in</strong>ctive<br />
ga<strong>it</strong> of <strong>NPH</strong> alone, or w<strong>it</strong>h cogn<strong>it</strong>ive impairment and/or<br />
ur<strong>in</strong>ary cont<strong>in</strong>ence problems, a comprehensive history and<br />
physical exam is <strong>in</strong>dicated to differentiate <strong>NPH</strong> from other<br />
diseases. Family-focused care is essential <strong>in</strong> obta<strong>in</strong><strong>in</strong>g an accurate<br />
history of the patient’s symptoms, behaviors, walk<strong>in</strong>g<br />
characteristics and pattern over time, history of falls, and<br />
activ<strong>it</strong>ies of daily liv<strong>in</strong>g. Family-focused care is also essential<br />
dur<strong>in</strong>g the ongo<strong>in</strong>g care of the <strong>older</strong> adult w<strong>it</strong>h <strong>NPH</strong>. 26<br />
Evaluation of ga<strong>it</strong>, changes <strong>in</strong> cogn<strong>it</strong>ion over time and<br />
present cogn<strong>it</strong>ive state, and present ur<strong>in</strong>ary symptoms and<br />
progression of symptoms provide important <strong>in</strong>dicators<br />
for diagnos<strong>in</strong>g <strong>NPH</strong>. If <strong>NPH</strong> is suspected, imag<strong>in</strong>g studies<br />
should be performed to identify ventriculomegaly. If ventriculomegaly<br />
is confirmed, prompt referral for neurologic<br />
or neurosurgical evaluation is essential.<br />
Follow<strong>in</strong>g shunt placement, improvement may develop<br />
over weeks and months. 7 Education provides the knowl-<br />
18 The Nurse Pract<strong>it</strong>ioner • Vol. 36, No. 3 www.tnpj.com<br />
Copyright © 2011 Lipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s. Unauthorized reproduction of this article is prohib<strong>it</strong>ed.
<strong>Ga<strong>it</strong></strong> <strong>disorder</strong> <strong>in</strong> <strong>older</strong> <strong>adults</strong>: <strong>Is</strong> <strong>it</strong> <strong>NPH</strong>?<br />
<strong>NPH</strong> webs<strong>it</strong>es<br />
Life <strong>NPH</strong>: Hope for People w<strong>it</strong>h Normal Pressure<br />
Hydrocephalus<br />
http://www.lifenph.com/<br />
Chicago Inst<strong>it</strong>ute of Neurosurgery and Neuroresearch<br />
CINN <strong>NPH</strong> Program<br />
http://www.c<strong>in</strong>n.org/other/nph-home.html<br />
Medtronic: Normal Pressure Hydrocephalus<br />
http://www.medtronic.com/hydrocephalus/nph/<strong>in</strong>dex.html<br />
National Inst<strong>it</strong>ute of Neurological Disorders and Stroke<br />
Normal Pressure Hydrocephalus Information Page<br />
http://www.n<strong>in</strong>ds.nih.gov/<strong>disorder</strong>s/normal_pressure_<br />
hydrocephalus/normal_pressure_hydrocephalus.htm<br />
Hydrocephalus Association<br />
http://www.hydroassoc.org/tag/normal-pressurehydrocephalus/<br />
edge necessary for patients and families to have realistic<br />
expectations and recognize shunt complications early. They<br />
should be taught to be attentive to the return of preoperative<br />
symptoms, headaches, visual disturbances, fatigue, sleep<br />
difficulties, personal<strong>it</strong>y changes, and paralysis and report<strong>in</strong>g<br />
them promptly to the neurosurgeon. 6,7,19 The patient and<br />
family need to be aware that headache that is relieved when<br />
the person recl<strong>in</strong>es may possibly be due to overshunt<strong>in</strong>g and<br />
should be reported promptly to the neurosurgeon. A CT<br />
scan may reveal the presence of collapsed ventricles. Infection<br />
near the implanted shunt <strong>it</strong>self may result <strong>in</strong> men<strong>in</strong>g<strong>it</strong>is<br />
or CSF <strong>in</strong>fection that may result <strong>in</strong> per<strong>it</strong>on<strong>it</strong>is. The patient<br />
and family should be taught the general signs and symptoms<br />
of <strong>in</strong>fection, as well as those for men<strong>in</strong>g<strong>it</strong>is and per<strong>it</strong>on<strong>it</strong>is.<br />
Any problems or concerns should be reported immediately<br />
to the neurosurgeon. Also, the patient should receive regular<br />
follow-up care w<strong>it</strong>h the neurosurgeon. 25<br />
As <strong>older</strong> <strong>adults</strong> live longer, stress and burden will <strong>in</strong>crease<br />
among families and <strong>in</strong>dividuals who take on the role<br />
of family caregiver for the <strong>older</strong> adult. As such burden and<br />
stress will be experienced <strong>in</strong> <strong>in</strong>creas<strong>in</strong>g levels, NPs can assist<br />
caregivers. Therefore, NPs must advocate for patients’<br />
families and caregivers by referr<strong>in</strong>g them for support services<br />
through local support groups, social services, and <strong>NPH</strong> organizations.<br />
Support and knowledge can improve the qual<strong>it</strong>y<br />
of life for both those affected by <strong>NPH</strong> and those responsible<br />
for their care. (See <strong>NPH</strong> webs<strong>it</strong>es and Case study of a delayed<br />
diagnosis and recovery from <strong>NPH</strong>).<br />
Lastly, <strong>it</strong> is important that patients and families be <strong>in</strong>formed<br />
about the treatment options and prognoses when<br />
decid<strong>in</strong>g on shunt<strong>in</strong>g <strong>in</strong>tervention. NPs have an opportun<strong>it</strong>y<br />
to provide unbiased <strong>in</strong>formation about <strong>NPH</strong> signs,<br />
symptoms, diagnosis, treatment, surgical risks, benef<strong>it</strong>s, and<br />
Case study of a delayed diagnosis and<br />
recovery from <strong>NPH</strong> 26<br />
SF was 74 when his daughter realized that he was hav<strong>in</strong>g<br />
some new problems. SF had a 10-year history of type 2<br />
diabetes and hypertension, but started to have a problem<br />
w<strong>it</strong>h his walk<strong>in</strong>g and frequent falls. His ga<strong>it</strong> was extremely<br />
slow and his feet looked as though they were glued to the<br />
floor. His stance was wide-based w<strong>it</strong>h l<strong>it</strong>tle knee flexion.<br />
SF tended to lean backward a b<strong>it</strong> as he stood <strong>in</strong> place or<br />
walked. Because he had <strong>in</strong>attentiveness and the slow ga<strong>it</strong>,<br />
<strong>it</strong> took him about 10 m<strong>in</strong>utes to walk from one room to<br />
another <strong>in</strong> his apartment. He seemed forge tful and slower<br />
<strong>in</strong> thought, yet he was able to carry out simple tasks<br />
<strong>in</strong>dependently. SF had been very good w<strong>it</strong>h his math for<br />
most of his life and started to have difficulty manag<strong>in</strong>g his<br />
checkbook. He was gett<strong>in</strong>g forgetful and had difficulty tak<strong>in</strong>g<br />
his medication properly. He had urgency, frequency,<br />
nocturia, and bladder <strong>in</strong>cont<strong>in</strong>ence at least once a day. His<br />
daughter was concerned about his health and took him to<br />
his long-time primary care provider every 3 months and<br />
also to a geriatric specialist. Both stated there was noth<strong>in</strong>g<br />
that could be done about his recent health issues and that<br />
his dementia would gradually get worse. This went on for<br />
4 years, but he only had mild cogn<strong>it</strong>ive decl<strong>in</strong>e dur<strong>in</strong>g this<br />
time and cont<strong>in</strong>ued problems w<strong>it</strong>h walk<strong>in</strong>g, occasional<br />
falls, and the ur<strong>in</strong>ary symptoms.<br />
SF’s daughter felt that someth<strong>in</strong>g could be done for<br />
her father and arranged for him to be evaluated by a<br />
multidiscipl<strong>in</strong>ary team. The diagnosis of <strong>NPH</strong> was made<br />
when he was 78 years old. He had a neurologic assessment;<br />
a CT scan revealed dilated lateral ventricles <strong>in</strong> the<br />
bra<strong>in</strong>. The w<strong>it</strong>hdrawal of 50 mL CSF via lumbar puncture<br />
resulted <strong>in</strong> transient improvement <strong>in</strong> his ga<strong>it</strong> for about<br />
18 hours. The ventriculoper<strong>it</strong>oneal shunt <strong>in</strong>sertion <strong>in</strong>to<br />
the lateral ventricle on the nondom<strong>in</strong>ant side of his bra<strong>in</strong><br />
resulted <strong>in</strong> gradual improvement over a 1-year period.<br />
Dur<strong>in</strong>g the first month, his social <strong>in</strong>teractions improved<br />
and he was more attentive. He walked w<strong>it</strong>h a quad cane<br />
to avoid fall<strong>in</strong>g and received physical therapy three<br />
times a week at home for 1 month.<br />
At 3 months, his ga<strong>it</strong> was steady and he could walk<br />
slowly and safely <strong>in</strong> his apartment w<strong>it</strong>hout a cane. At 6<br />
months, his memory had improved. He was once aga<strong>in</strong><br />
able to calculate simple math problems and manage his<br />
own checkbook. He walked at a normal pace w<strong>it</strong>hout fall<strong>in</strong>g.<br />
One year after surgery he was able to wr<strong>it</strong>e better,<br />
was more attentive, and had improved memory.<br />
prognosis and to educate patients and families so they can<br />
make educated decisions and best care for themselves and<br />
their dependent elders.<br />
REFERENCES<br />
1. Stolze H, Kuhtz-Buschbeck JP, Drücke H, et al. <strong>Ga<strong>it</strong></strong> analysis <strong>in</strong> idiopathic<br />
normal pressure hydrocephalus- which parameters respond to the CSF tap<br />
test? Cl<strong>in</strong> Neurophysiol. 2000;111(9):1678-1686.<br />
2. Relk<strong>in</strong> N, Marmarou A, Kl<strong>in</strong>ge P, Bergsneider M, Black PM. Diagnos<strong>in</strong>g<br />
idiopathic normal-pressure hydrocephalus. Neurosurg. 2005;57(3 suppl):S4-S16.<br />
3. Marmarou A. Foreward to I<strong>NPH</strong> guidel<strong>in</strong>es. Neurosurg. 2005;57(3):S2:1.<br />
4. Chrysikopoulos H. Idiopathic normal pressure hydrocephalus: Thoughts on<br />
etiology and pathophysiology. Med Hypoth. 2009;73(5):718-724.<br />
www.tnpj.com The Nurse Pract<strong>it</strong>ioner • March 2011 19<br />
Copyright © 2011 Lipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s. Unauthorized reproduction of this article is prohib<strong>it</strong>ed.
<strong>Ga<strong>it</strong></strong> <strong>disorder</strong> <strong>in</strong> <strong>older</strong> <strong>adults</strong>: <strong>Is</strong> <strong>it</strong> <strong>NPH</strong>?<br />
5. Krauss JK, Regal JP, Vach W, Droste DW, Borremans JJ, Mergner T. Vascular<br />
risk factors and arteriosclerotic disease <strong>in</strong> idiopathic normal-pressure<br />
hydrocephalus of the elderly. Stroke. 1996;27(1):24-29.<br />
6. Thynne K. Normal pressure hydrocephalus. J Neurosci Nurs. 2007;39(1),27-32.<br />
7. Factora R, Luciano M. When to consider normal pressure hydrocephalus <strong>in</strong><br />
the patient w<strong>it</strong>h ga<strong>it</strong> disturbance. Geriatrics. 2008;63(2):32-37.<br />
8. Gallia GL, Rigamonti D, Williams MA. The diagnosis and treatment of<br />
idiopathic normal pressure hydrocephalus. Nat Cl<strong>in</strong> Pract Neurol. 2006;<br />
2(7):375-381.<br />
9. Vanneste JA. Diagnosis and management of normal-pressure hydrocephalus.<br />
J Neurol. 2000;247(1):5-14.<br />
10. Jones HC, Kl<strong>in</strong>ge PM. Hydrocephalus. 17-20th September, Hannover<br />
Germany: A conference report. Cerebrosp Fluid Resear. 2008;5:19.<br />
doi:10.1186/1743-8454-5-19.<br />
11. Kuba H, Inamura T, Ikezaki K, et al. <strong>Ga<strong>it</strong></strong> disturbance <strong>in</strong> patients w<strong>it</strong>h low<br />
pressure hydrocephalus. J Cl<strong>in</strong> Neurosci. 2002;9(1): 33-36.<br />
12. Dalvi AI, Premkumar AP. Normal pressure hydrocephalus. EMedic<strong>in</strong>e. 2010.<br />
http://emedic<strong>in</strong>e.medscape.com/article/1150924.<br />
13. Verrees M, Selman WR. Management of normal pressure hydrocephalus.<br />
American Family Physician. 2004;70(6):1071-1078.<br />
14. Blomsterwall E, Svantesson U, Carlsson U, Tullberg M, Wikkelsö C. Postural<br />
disturbance <strong>in</strong> patients w<strong>it</strong>h normal pressure hydrocephalus. Acta Neurol<br />
Scand. 2000;102(5):284-291.<br />
15. Shprecher D, Schwalb J, Kurlan R. Normal pressure hydrocephalus: Diagnosis<br />
and treatment. Curr Neurol Neurosci Rep. 2008;8(5):371-376.<br />
16. Siedlecki SL. Normal pressure hydrocephalus: Are you miss<strong>in</strong>g the signs? J<br />
Gerontol Nurs. 2008;34(2):27-33.<br />
17. Wilson JA, <strong>Is</strong>lam O. Normal pressure hydrocephalus. 2004. http://www.<br />
emedic<strong>in</strong>e.com/radio/topic479.htm.<br />
18. Bejjani GK, Hammer MD. Normal-pressure hydrocephalus. Another<br />
treatable dementia. Part I. Contemp Neurosurg. 2005;27(1):2-4.<br />
19. Johnson M, Graham K. Diagnosis and surgical treatment of normal-pressure<br />
hydrocephalus. J AAPA. 2010;23(5):51-56.<br />
20. K<strong>it</strong>agaki H, Mori E, <strong>Is</strong>hii K, Yamaji S, Hirono N, Imamura T. CSF spaces<br />
<strong>in</strong> idiopathic normal pressure hydrocephalus: Morphology and volumetry.<br />
AJNR Am J Neuroradiol. 1998;19(7):1277-1284.<br />
21. McGirt MJ, Woodworth G, Coon AL, Thomas G, Williams MA, Rigamonti<br />
D. Diagnosis, treatment, and analysis of long-term outcomes <strong>in</strong> idiopathic<br />
normal-pressure hydrocephalus. Neurosurgery. 2005;57(4):699-705.<br />
22. Marmarou A, Bergsneider M, Kl<strong>in</strong>ge P, Relk<strong>in</strong> N, Black PM. The value of<br />
supplemental prognostic tests for the preoperative assessment of idiopathic<br />
normal-pressure hydrocephalus. Neurosurgery. 2005;57(3 suppl):S17-S28.<br />
23. Bergsneider M, Black PM, Kl<strong>in</strong>ge P, Marmarou A, Relk<strong>in</strong> N. Surgical<br />
management of idiopathic normal-pressure hydrocephalus. Neurosurgery.<br />
2005; 57(3 suppl):S29-S39.<br />
24. Li B, Zhang Q, Liu J, Yu H, Hu S. Cl<strong>in</strong>ical application of a laparoscope<br />
<strong>in</strong> ventri-per<strong>it</strong>oneal shunt<strong>in</strong>g. M<strong>in</strong>im Invasive Ther Allied Technol.<br />
2007;16(6):367-369.<br />
25. Kl<strong>in</strong>ge P, Marmarou A, Bergsneider M, Relk<strong>in</strong> N, Black P. Outcome of<br />
shunt<strong>in</strong>g <strong>in</strong> idiopathic normal-pressure hydrocephalus and the value<br />
of outcome assessment <strong>in</strong> shunted patients. Neurosurgery. 2005;57(3<br />
Suppl):S40-S52.<br />
26. Fraser JJ, Fraser C. <strong>Ga<strong>it</strong></strong> <strong>disorder</strong> is the card<strong>in</strong>al sign of normal pressure<br />
hydrocephalus: A case study. J Neurosci Nurs. 2007;39(3):132-134, 192.<br />
27. Life <strong>NPH</strong>: Hope for people w<strong>it</strong>h normal pressure hydrocephalus. 2010.<br />
http://www.lifenph.com.<br />
The authors have disclosed that they have no f<strong>in</strong>ancial relationships related to<br />
this article.<br />
Cira Fraser is an associate professor and graduate faculty and Sharon W. Stark is<br />
associate dean and graduate faculty at Marjorie K. Unterberg School of Nurs<strong>in</strong>g<br />
and Health Studies, Monmouth Univers<strong>it</strong>y, West Long Branch, New Jersey, N.J.<br />
DOI-10.1097/01.NPR.0000393969.13812.2e<br />
For more than 80 add<strong>it</strong>ional cont<strong>in</strong>u<strong>in</strong>g education articles related to<br />
Advanced Practice Nurs<strong>in</strong>g topics, go to Nurs<strong>in</strong>gCenter.com/CE.<br />
Earn CE cred<strong>it</strong> onl<strong>in</strong>e:<br />
Go to http://www.nurs<strong>in</strong>gcenter.com/CE/NP and<br />
receive a certificate w<strong>it</strong>h<strong>in</strong> m<strong>in</strong>utes.<br />
INSTRUCTIONS<br />
<strong>Ga<strong>it</strong></strong> <strong>disorder</strong> <strong>in</strong> <strong>older</strong> <strong>adults</strong>: <strong>Is</strong> <strong>it</strong> <strong>NPH</strong>?<br />
TEST INSTRUCTIONS<br />
• To take the test onl<strong>in</strong>e, go to our secure webs<strong>it</strong>e<br />
at http://www.nurs<strong>in</strong>gcenter.com/ce/NP.<br />
• On the pr<strong>in</strong>t form, record your answers <strong>in</strong><br />
the test answer section of the CE enrollment<br />
form on page 21. Each question has only one<br />
correct answer. You may make copies<br />
of these forms.<br />
• Complete the registration <strong>in</strong>formation and<br />
course evaluation. Mail the completed form<br />
and registration fee of $24.95 to: Lipp<strong>in</strong>cott<br />
Williams & Wilk<strong>in</strong>s, CE Group, 2710<br />
Yorktowne Blvd., Brick, NJ 08723. We will<br />
mail your certificate <strong>in</strong> 4 to 6 weeks. For<br />
faster service, <strong>in</strong>clude a fax number and<br />
we will fax your certificate w<strong>it</strong>h<strong>in</strong> 2 bus<strong>in</strong>ess<br />
days of receiv<strong>in</strong>g your enrollment form.<br />
• You will receive your CE certificate of<br />
earned contact hours and an answer key<br />
to review your results.There is no m<strong>in</strong>imum<br />
pass<strong>in</strong>g grade.<br />
• Registration deadl<strong>in</strong>e is March 31, 2013.<br />
DISCOUNTS and CUSTOMER SERVICE<br />
• Send two or more tests <strong>in</strong> any nurs<strong>in</strong>g journal published by Lipp<strong>in</strong>cott Williams<br />
& Wilk<strong>in</strong>s together and deduct $0.95 from the price of each test.<br />
• We also offer CE accounts for hosp<strong>it</strong>als and other healthcare facil<strong>it</strong>ies on<br />
nurs<strong>in</strong>gcenter.com. Call 1-800-787-8985 for details.<br />
PROVIDER ACCREDITATION<br />
Lipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s, publisher of The Nurse Pract<strong>it</strong>ioner<br />
journal, will award 2.5 contact hours for this cont<strong>in</strong>u<strong>in</strong>g nurs<strong>in</strong>g education<br />
activ<strong>it</strong>y.<br />
Lipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s is accred<strong>it</strong>ed as a provider of cont<strong>in</strong>u<strong>in</strong>g<br />
nurs<strong>in</strong>g education by the American Nurses Credential<strong>in</strong>g Center’s Commission<br />
on Accred<strong>it</strong>ation.<br />
This activ<strong>it</strong>y is also provider approved by the California Board of Registered<br />
Nurs<strong>in</strong>g, Provider Number CEP 11749 for 2.5 contact hours. Lipp<strong>in</strong>cott Williams &<br />
Wilk<strong>in</strong>s is also an approved provider of cont<strong>in</strong>u<strong>in</strong>g nurs<strong>in</strong>g education by the District<br />
of Columbia and Florida #FBN2454.<br />
Your certificate is valid <strong>in</strong> all states.<br />
The ANCC’s accred<strong>it</strong>ation status of Lipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s Department of<br />
Cont<strong>in</strong>u<strong>in</strong>g Education refers only to <strong>it</strong>s cont<strong>in</strong>u<strong>in</strong>g nurs<strong>in</strong>g educational activ<strong>it</strong>ies<br />
and does not imply Commission on Accred<strong>it</strong>ation approval or endorsement of<br />
any commercial product.<br />
20 The Nurse Pract<strong>it</strong>ioner • Vol. 36, No. 3 www.tnpj.com<br />
Copyright © 2011 Lipp<strong>in</strong>cott Williams & Wilk<strong>in</strong>s. Unauthorized reproduction of this article is prohib<strong>it</strong>ed.