Intermediate-acting Insulin Preparations: NPH and ... - Diabetes Care
Intermediate-acting Insulin Preparations: NPH and ... - Diabetes Care
Intermediate-acting Insulin Preparations: NPH and ... - Diabetes Care
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Intermediate</strong>-<strong>acting</strong> <strong>Insulin</strong> <strong>Preparations</strong>:<br />
<strong>NPH</strong> <strong>and</strong> Lente<br />
TORSTEN DECKERT<br />
Physicochemically, <strong>NPH</strong> <strong>and</strong> lente insulins differ in size of crystals, content of protamine <strong>and</strong> zinc, <strong>and</strong><br />
often in species composition, since lente always contains beef insulin. The duration of the hypoglycemic<br />
effect of lente insulin seems to be longer than 24 h, whereas that of <strong>NPH</strong> insulin does not exceed 24 h<br />
when given in amounts of 0.2-0.3 U/kg body wt. Moreover, <strong>NPH</strong> <strong>and</strong> lente insulins differ in their<br />
ability to form stable mixtures with neutral insulin solutions, since only <strong>NPH</strong> insulin can be mixed with<br />
regular insulin without changing the specific course of effect of regular insulin. Highly purified porcine<br />
<strong>NPH</strong> <strong>and</strong> the lente-like porcine insulin preparation, Monotard, do not seem to differ regarding side<br />
effects (lipoatrophy, immunogenicity). However, highly purified lente insulin (containing beef insulin)<br />
seems to be more immunogenic than highly purified porcine <strong>NPH</strong> insulin, DIABETES CARE 3- 623-626,<br />
SEPTEMBER-OCTOBER 1980.<br />
The most widely used intermediate-<strong>acting</strong> insulin<br />
preparations are <strong>NPH</strong> <strong>and</strong> lente insulins. It is<br />
often asked whether there is any difference between<br />
them in their course of action, reproducibility<br />
of resorption, mixability with regular insulin, <strong>and</strong> side effects,<br />
particularly immunogenicity. To answer these questions,<br />
the known characteristics of these two insulin preparations<br />
are briefly reviewed.<br />
HISTORICAL BACKGROUND<br />
<strong>NPH</strong> (neutral protamine Hagedom) insulin is a further development<br />
of Hagedorn's protamine insulin 1 made by<br />
Krayenbiihl <strong>and</strong> Rosenberg at Nordisk <strong>Insulin</strong>laboratorium,<br />
Denmark, in 1946. 2 They found that insulin <strong>and</strong> protamine<br />
brought together in isophane proportions (the condition in<br />
which neither insulin nor protamine is found in excess) at<br />
neutral pH, in the presence of small amounts of zinc <strong>and</strong><br />
phenol <strong>and</strong>/or cresol, will precipitate in oblong tetragonal<br />
crystals without leaving any regular insulin in the supernatant.<br />
Lente insulin (zinc insulin preparation) was invented by<br />
Hallas-Mtfller et al. in 1952 at the Novo company, also in<br />
Denmark. 3 The prolongation of effect is based on the fact<br />
that the solubility of insulin at neutral pH in acetate buffer<br />
can be reduced by a surplus of zinc. Furthermore, it can be<br />
modified by the physical state of zinc insulin <strong>and</strong> by proper<br />
usage of the solubility characteristics of beef insulin.<br />
PHYSICOCHEMICAL CHARACTERISTICS<br />
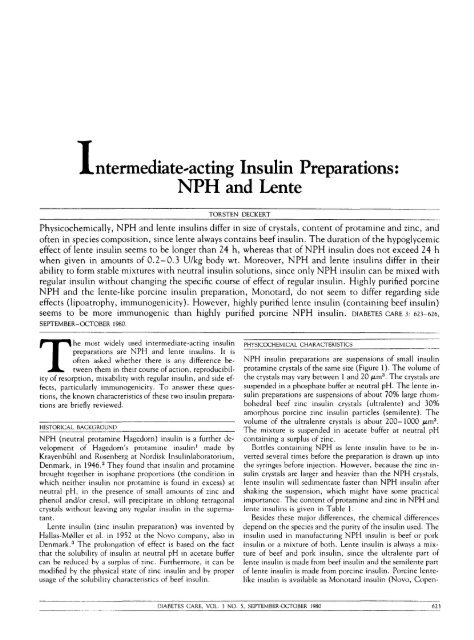
<strong>NPH</strong> insulin preparations are suspensions of small insulin<br />
protamine crystals of the same size (Figure 1). The volume of<br />
the crystals may vary between 1 <strong>and</strong> 20 fim 3 . The crystals are<br />
suspended in a phosphate buffer at neutral pH. The lente insulin<br />
preparations are suspensions of about 70% large rhombohedral<br />
beef zinc insulin crystals (ultralente) <strong>and</strong> 30%<br />
amorphous porcine zinc insulin particles (semilente). The<br />
volume of the ultralente crystals is about 200- 1000 fxm 3 .<br />
The mixture is suspended in acetate buffer at neutral pH<br />
containing a surplus of zinc.<br />
Bottles containing <strong>NPH</strong> as lente insulin have to be inverted<br />
several times before the preparation is drawn up into<br />
the syringes before injection. However, because the zinc insulin<br />
crystals are larger <strong>and</strong> heavier than the <strong>NPH</strong> crystals,<br />
lente insulin will sedimentate faster than <strong>NPH</strong> insulin after<br />
shaking the suspension, which might have some practical<br />
importance. The content of protamine <strong>and</strong> zinc in <strong>NPH</strong> <strong>and</strong><br />
lente insulins is given in Table 1.<br />
Besides these major differences, the chemical differences<br />
depend on the species <strong>and</strong> the purity of the insulin used. The<br />
insulin used in manufacturing <strong>NPH</strong> insulin is beef or pork<br />
insulin or a mixture of both. Lente insulin is always a mixture<br />
of beef <strong>and</strong> pork insulin, since the ultralente part of<br />
lente insulin is made from beef insulin <strong>and</strong> the semilente part<br />
of lente insulin is made from porcine insulin. Porcine lentelike<br />
insulin is available as Monotard insulin (Novo, Copen-<br />
DIABETES CARE, VOL. 3 NO. 5, SEPTEMBER-OCTOBER 1980 623
INTERMEDIATE-ACTING INSULIN: <strong>NPH</strong> AND LENTE/TORSTEN DECKERT<br />
(a)<br />
(b)<br />
FIG. I. Photomicrograph of (a) <strong>NPH</strong> suspension <strong>and</strong> (b) lente insulin suspension at room temperature. 1.0 cm =20<br />
/u,m.<br />
hagen, Denmark). The species specificity seems to play a role<br />
in the immunogenicity of insulin, since insulin preparations<br />
containing beef insulin have been shown to induce insulin<br />
antibodies more easily than insulin preparations containing<br />
only porcine insulin. 11<br />
The purity of the insulin component varies over a wide<br />
range. During the last years there has been a development<br />
toward insulin preparations of higher purity, since it has<br />
been shown that several side effects (for example, lipoatrophy,<br />
insulin resistance, insulin allergy, <strong>and</strong> the development<br />
of several humoral antibodies) depend largely on the<br />
purity of the insulin preparation. 4 * 5 The purity of <strong>NPH</strong> as<br />
well as lente insulin preparations is expressed in suffix as single<br />
peak, single component, monocomponent (MC), or rare<br />
immunogenic (RI). Single peak means that insulin has been<br />
isolated by gel filtration, which separates molecules according<br />
to their size (i.e., insulin, arginine insulin, desamidoinsulin,<br />
ethylester insulin, <strong>and</strong> small amounts of other polypeptides).<br />
Single component, monocomponent, <strong>and</strong> rare<br />
immunogenum (RI) means that insulin has been further<br />
purified by chromatography, which also separates molecules<br />
of the same molecular size <strong>and</strong> therefore contains less impurities.<br />
As well, <strong>NPH</strong> made from porcine insulin as lente insulin<br />
of highly purified quality is available. However, for docu-<br />
624 DIABETES CARE, VOL. 3 NO. 5, SEPTEMBER-OCTOBER 1980
INTERMEDIATE-ACTING INSULIN: <strong>NPH</strong> AND LENTE/TORSTEN DECKERT<br />
TABLE 1<br />
Content of protamine <strong>and</strong> zinc in <strong>NPH</strong> <strong>and</strong> lente insulins<br />
<strong>NPH</strong><br />
Lente<br />
Protamine<br />
Physical state pH Zn (mg/100 U) (mg/100 U)<br />
Crystalline<br />
70% crystalline<br />
30% amorphous<br />
7.3<br />
7.3<br />
0.02<br />
0.20<br />
0.3-0.4<br />
0<br />
menting purity, techniques such as gel filtration <strong>and</strong><br />
chromatography are insufficient. The purity of insulin should<br />
be further specified by radioimmunologic determination of<br />
the relevant contaminants [i.e., a-components, proinsulin,<br />
glucagon-like materials, pancreatic polypeptide (PP), vasoactive<br />
intestinal peptide (VIP), somatostatin] by well-documented<br />
techniques. Also, the purity of protamine, zinc, <strong>and</strong><br />
other additives should be stated. Otherwise, the purity of<br />
<strong>NPH</strong> <strong>and</strong> lente insulins cannot be compared.<br />
ABSORPTION FROM SUBCUTANEOUS TISSUE<br />
bsorption studies with <strong>NPH</strong> <strong>and</strong> lente insulins have<br />
been done either by following the disappearance<br />
of radioactivity from subcutaneous tissue after<br />
the injection of labeled <strong>NPH</strong> or lente insulin or<br />
by following the plasma insulin concentration after subcutaneous<br />
injection of these preparations in patients with only<br />
minor or no endogenous insulin secretion. However, the<br />
same techniques have not been used <strong>and</strong> the results therefore<br />
are not strictly comparable.<br />
The most extensive studies with radioactive-labeled <strong>NPH</strong><br />
insulin have been done by Ktflendorf et al. 6 <strong>and</strong> with labeled<br />
lente insulin by Binder et al. 7 ' 8 The differences between<br />
<strong>NPH</strong> <strong>and</strong> lente insulin, according to their results, are shown<br />
in Table 2. Twenty-four hours after injection in the femoral<br />
region, remarkably more radioactivity is found at the injection<br />
site after lente insulin compared with <strong>NPH</strong> insulin.<br />
The disappearance of radioactivity at the injection site<br />
after <strong>NPH</strong> insulin followed first-order kinetics, 6 whereas<br />
lente was absorbed in a biphasic curve, 7 probably because<br />
lente insulin is a mixture of amorphous <strong>and</strong> crystalline zinc<br />
insulin.<br />
The reproducibility of day-to-day absorption in the same<br />
patient, measured as the variation coefficient of the time<br />
until 40-50% of the maximal radioactivity disappeared, was<br />
26% for <strong>NPH</strong> insulin 6 <strong>and</strong> about 35% for lente insulin. 7<br />
Thus, the reproducibility of the resorption of both insulin<br />
TABLE 2<br />
Differences in absorption between <strong>NPH</strong> <strong>and</strong> lente insulins<br />
Percent of injected insulin at injection site after:<br />
10 h 24 h 36 h<br />
preparations seems to be in the same range. It must, however,<br />
be mentioned that the experiments with lente insulin<br />
were\done with non-highly purified insulins.<br />
After subcutaneous injection of <strong>NPH</strong> insulin in reasonable<br />
doses, plasma insulin concentration increases significantly<br />
after 2 h <strong>and</strong> is maximal after 5 h. 6 After lente insulin in<br />
comparable amounts, the time for significant initial increments<br />
to occur is not known. The maximal plasma insulin<br />
concentration seems to be reached 7 h after the injection of<br />
lente insulin. 9 Twenty-four hours after the injection of <strong>NPH</strong><br />
insulin, the plasma insulin concentration is not higher than<br />
before the injection. Twenty-four hours after lente insulin,<br />
plasma insulin still seems to be elevated. 10<br />
COURSE OF ACTION<br />
The time curve of the blood glucose lowering action of <strong>NPH</strong><br />
<strong>and</strong> lente insulins (as given by Nordisk <strong>Insulin</strong>laboratorium<br />
<strong>and</strong> the Novo Company in 1978) is shown in Table 3. However,<br />
r<strong>and</strong>omized crossover experiments against placebo in<br />
fasting diabetic subjects have only been done by K^lendorf et<br />
al. with <strong>NPH</strong> insulin. 6 They found that the starting action<br />
began 120 min after the injection, <strong>and</strong> that the maximal action<br />
occurred 5.5 h after the injection, 30 min after the<br />
maximal plasma insulin concentration had been reached.<br />
From Rasmussen et al.'s experiments in nonfasting diabetic<br />
subjects, it seems that the maximal effect after lente was first<br />
achieved after 10 h. 9<br />
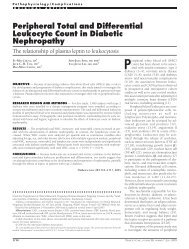
The porcine lente-like preparation Monotard appears to<br />
have a shorter effect than lente insulin. Our crossover experiments<br />
on maturity-onset diabetic subjects using highly<br />
purified porcine <strong>NPH</strong> insulin <strong>and</strong> the highly purified porcine<br />
lente-like preparation Monotard did not indicate differences<br />
in the blood glucose lowering effects between these two preparations<br />
(Figure 2). Reproducibility of the blood glucose<br />
lowering effect of <strong>NPH</strong> insulin in maturity-onset diabetes<br />
was shown to be excellent. 6<br />
It can be concluded from resorption studies, studies of<br />
plasma insulin concentration after subcutaneous injection,<br />
<strong>and</strong> studies of the blood glucose lowering effects of <strong>NPH</strong> <strong>and</strong><br />
lente that lente has a more protracted action than <strong>NPH</strong> insulin.<br />
MIXABILITY<br />
Regular insulin can be mixed with <strong>NPH</strong> or lente insulin in<br />
the same syringe in every ratio. However, the course of effect<br />
will change with lente/regular mixtures depending on the<br />
TABLE 3<br />
Time curve of action<br />
of <strong>NPH</strong> <strong>and</strong> lente insulins<br />
Onset<br />
Course of effect (h)<br />
Maximum<br />
End<br />
<strong>NPH</strong><br />
Lente<br />
40<br />
70<br />
10<br />
40<br />
0<br />
25<br />
<strong>NPH</strong><br />
Lente<br />
1*4<br />
2Vi<br />
4-12<br />
24<br />
24 Vi<br />
Data from K0lendorf et al. 6 <strong>and</strong> Binder. 7 Data from Nordisk <strong>Insulin</strong>laboratorium <strong>and</strong> Novo Company, 1978.<br />
DIABETES CARE, VOL. 3 NO. 5, SEPTEMBER-OCTOBER 1980 625
INTERMEDIATE-ACTING INSULIN: <strong>NPH</strong> AND LENTE/TORSTEN DECKERT<br />
per cent of initial<br />
blood glucose (m* SEM )<br />
100-<br />
-<br />
80-<br />
x <strong>NPH</strong> (Retard RI®)<br />
o Lente like (Monotard®)<br />
n= 12<br />
60-<br />
40-<br />
20-<br />
T injection<br />
^N-f+Hnu-——-—Hi<br />
13 15 17 19 21<br />
TIME<br />
FIG. 2. Blood glucose lowering effect in percent<br />
of initial capillary blood glucose (initial = mean<br />
of blood glucose at 0700, 0800, <strong>and</strong> 0900 h)<br />
after highly purified porcine <strong>NPH</strong> insulin (Retard<br />
RI) <strong>and</strong> the highly purified porcine Ientelike<br />
preparation (Monotard) given subcutaneous^<br />
(at the arrow) in the femoral region.<br />
R<strong>and</strong>omized crossover experiment.<br />
ratio between lente <strong>and</strong> regular insulin in the syringe, 10 presumably<br />
because the surplus of zinc in the supernatant of<br />
lente insulin will react with regular insulin <strong>and</strong> change it to a<br />
semilente-like preparation. This is not the case when mixing<br />
regular insulin with <strong>NPH</strong>. Stable mixtures of regular <strong>and</strong> intermediate-<strong>acting</strong><br />
insulin can only be prepared with <strong>NPH</strong> insulin.<br />
6<br />
IMMUNOGENICITY<br />
The immunogenicity of <strong>NPH</strong> <strong>and</strong> lente insulin depends<br />
largely on the purity <strong>and</strong> species of the insulin<br />
used. <strong>Preparations</strong> containing beef insulin are<br />
more immunogenic than insulin preparations<br />
made of porcine insulin of comparable purity. 11 However, by<br />
using lente insulin of monocomponent purity (lente prepared<br />
from highly purified beef <strong>and</strong> highly purified porcine insulin),<br />
formation of antibodies can be avoided in some instances,<br />
4 but not to the same extent as with highly purified<br />
porcine insulin. 11 Highly purified porcine <strong>NPH</strong> insulin Leo<br />
Retard RI (Nordisk) <strong>and</strong> the highly purified porcine lentelike<br />
insulin preparation Monotard (Novo) are of very low<br />
immunogenicity. Antibody formation against proinsulin, 12<br />
glucagon, VIP, PP, <strong>and</strong> probably somatostatin can be<br />
avoided. 13 Antibodies against protamine have not been described,<br />
but in a few patients with insulin allergy, positive<br />
cutaneous reactions were seen against highly purified insulin<br />
as well as protamine. 14 It is not known whether the insulin<br />
preparation plays a role in the development of late diabetic<br />
complications; probably this cannot be substantiated.<br />
From Steno Memorial Hospital, DK-2820, Gentofte, Copenhagen,<br />
Denmark.<br />
REFERENCES<br />
1 Hagedorn, H. C, Jensen, B. N., Krarup, N. B., <strong>and</strong> Wodstrup,<br />
I.: Protamine insulinate. JAMA 106: 177-80, 1936.<br />
2 Krayenbiihl, C., <strong>and</strong> Rosenberg, T.: Crystalline protamine insulin.<br />
Rep. Steno Hosp. (Kbh.) 1: 60-73, 1946.<br />
3 Hallas-Mtfller, K., Jersild, M., Petersen, K., <strong>and</strong> Schlichtkrull,<br />
J.: Zinc insulin preparations for single daily injection. JAMA 150:<br />
1667-71, 1952.<br />
4 Schlichtkrull, J., Pingel, M., Heding, L. G., Brange, J., <strong>and</strong><br />
J^rgensen, K. H.: <strong>Insulin</strong> preparations with prolonged effect. In <strong>Insulin</strong><br />
II. Hasselblatt, A., <strong>and</strong> Bruchhausen, F. v., Eds. Berlin,<br />
Springer-Verlag, 1975, pp. 729-77.<br />
5 Deckert, T., Andersen, O. O., <strong>and</strong> Poulsen, J. E.: The clinical<br />
significance of highly purified pig-insulin preparations. Diabetologia<br />
10: 703-08, 1974.<br />
6 K«ilendorf, K., Aaby, P., Westergaard, S., <strong>and</strong> Deckert, T.:<br />
Resorption, effect <strong>and</strong> side effects of highly purified porcine <strong>NPH</strong>insulin<br />
preparations (Leo®). Eur. J. Pharmacol. In press.<br />
7 Binder, Chr.: Absorption of Injected <strong>Insulin</strong>. Copenhagen,<br />
Munksgaard, 1969.<br />
8 Faber, O. K., Lauritzen, T., Binder, Chr., Mouridsen, H. T.,<br />
<strong>and</strong> V^lund, Aa.: Comparison of absorption <strong>and</strong> clinical effects of<br />
<strong>Insulin</strong> Monotard® <strong>and</strong> <strong>Insulin</strong> Novo Lente®. Ugeskr. Laeg. 137:<br />
2510-14, 1975.<br />
9 Rasmussen, S. M., Heding, L. G., Parbst, E., <strong>and</strong> V«ilund,<br />
Aa.: Serum IRI in insulin-treated diabetics during a 24/hour period.<br />
Diabetologia JJ: 151-58, 1975.<br />
10 Schlichtkrull, J.: The absorption of insulin. Acta Paediatr.<br />
Sc<strong>and</strong>. [Suppl.] 270: 97-102, 1977.<br />
11 Chance, R. E., Root, M. A., <strong>and</strong> Galloway, J. A.: The immunogenicity<br />
of insulin preparations. Acta Endocrinol. (Kbh.)<br />
Suppl. 205: 185-99, 1976.<br />
12 Falling, I., Jerwell, J., Aagenaes, 0., <strong>and</strong> Aarseth, S.: Antibodies<br />
to insulin <strong>and</strong> proinsulin, metabolic control, <strong>and</strong> insulin<br />
dose, in diabetics changing to highly purified insulins. Diabetologia<br />
12: 390, 1976.<br />
13 Bloom, S. R., West, A. M., Polak, J. M., Barnes, A. J., <strong>and</strong><br />
Adrian, T. E.: Hormonal Contaminants of <strong>Insulin</strong> from Gut Hormones.<br />
Bloom, S. R., Ed. Edinburgh, Churchill Livingstone, 1978,<br />
pp. 318-22.<br />
14 Rosenthal, A.: Genetic control of insulin antibody formation.<br />
Juvenile <strong>Diabetes</strong> Foundation International Workshop on <strong>Insulin</strong>.<br />
New York, 1978.<br />
626 DIABETES CARE, VOL. 3 NO. 5, SEPTEMBER-OCTOBER 1980