Amputation of Finger by Horse Bite With Complete Avulsion ... - Healio
Amputation of Finger by Horse Bite With Complete Avulsion ... - Healio
Amputation of Finger by Horse Bite With Complete Avulsion ... - Healio
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
■ Case Report<br />
<strong>Amputation</strong> <strong>of</strong> <strong>Finger</strong> <strong>by</strong> <strong>Horse</strong> <strong>Bite</strong> <strong>With</strong><br />
<strong>Complete</strong> <strong>Avulsion</strong> <strong>of</strong> Both Flexor Tendons<br />
LIOR KOREN, MD; SHALOM STAHL, MD; ALEXEY ROVITSKY, MD; ELI PELED, MD<br />
abstract<br />
Full article available online at ORTHOSuperSite.com. Search: 20110627-26<br />
<strong>Amputation</strong> <strong>of</strong> fingers with tendon avulsion occurs through a traction injury, and most<br />
occur through a ring avulsion mechanism. Usually the flexor digitorum pr<strong>of</strong>undus is<br />
torn out with the amputated finger. Replantation usually is recommended only when<br />
the amputation is distal to the flexor digitorum superficialis insertion. Animal bites are<br />
relatively common, with a decreasing order <strong>of</strong> frequency <strong>of</strong> dogs, cats, and humans.<br />
<strong>Horse</strong> bites are relatively infrequent but are associated with crush injuries and tissue<br />
loss when they occur.<br />
1<br />
This article describes a 23-year-old man with amputation <strong>of</strong> his middle finger at the<br />
level <strong>of</strong> the proximal phalanx after being bitten <strong>by</strong> a horse. The amputated stump<br />
was avulsed with the middle finger flexor digitorum pr<strong>of</strong>undus and flexor digitorum<br />
superficialis torn from the muscle-tendon junction from approximately the middle <strong>of</strong><br />
the forearm. The patient had no other injuries, and he was able to move his other 4<br />
fingers with only mild pain. As the amputated digit was not suitable for replantation,<br />
the wound was irrigated and debrided. The edges <strong>of</strong> the phalanx were trimmed, and<br />
the edges <strong>of</strong> the wound were sutured. Tetanus toxoid and rabies vaccine were administered,<br />
along with intravenous amoxicillin and clavulanic acid. The patient was<br />
discharged from the hospital 2 days later, with no sign <strong>of</strong> infection <strong>of</strong> the wound or<br />
compartment syndrome <strong>of</strong> the forearm. This case demonstrates the weakest point in<br />
the myotendinous junction and emphasizes the importance <strong>of</strong> a careful physical examination<br />
in patients with a traumatic amputation.<br />
2<br />
Figure 1: Photograph showing the stump <strong>of</strong> the<br />
third fi nger. Figure 2: Photograph showing the amputated<br />
middle fi nger with the tendon attached up<br />
to the myotendinous junction. The avulsed fl exor<br />
digitorum pr<strong>of</strong>undus and fl exor digitorum superfi<br />
cialis are attached to the amputated finger, and<br />
a few muscle fi bers are attached to the tendons in<br />
the proximal part.<br />
Drs Koren, Rovitsky, and Peled are from the Department <strong>of</strong> Orthopedic Surgery B, and Dr Stahl is<br />
from the Hand Surgery Unit, Rambam Health Care Campus and the Bruce Rappaport Faculty <strong>of</strong> Medicine,<br />
Technion-Israel Institute <strong>of</strong> Technology, Haifa, Israel.<br />
Drs Koren, Stahl, Rovitsky, and Peled have no relevant fi nancial relationships to disclose.<br />
Correspondence should be addressed to: Eli Peled, MD, Department <strong>of</strong> Orthopedic Surgery B, Rambam<br />
Health Care Campus, POB 9602, Haifa 31096, Israel (e_peled@rambam.health.gov.il).<br />
doi: 10.3928/01477447-20110627-26<br />
AUGUST 2011 | Volume 34 • Number 8<br />
e421
■ Case Report<br />
<strong>Amputation</strong> <strong>of</strong> fingers with tendon<br />
avulsion from their musculotendinous<br />
junction are caused <strong>by</strong> a traction<br />
injury, most <strong>of</strong> which occur through a<br />
ring avulsion mechanism. Ring avulsion<br />
has been classified <strong>by</strong> Urbaniak et al 1 and<br />
revised <strong>by</strong> Kay et al. 2 Several case reports<br />
describe this specific injury. 2-6 When a<br />
tendon is torn out with the amputated segment,<br />
it is usually with the flexor digitorum<br />
pr<strong>of</strong>undus. Replantation is recommended<br />
only when the amputation is distal to the<br />
flexor digitorum superficialis insertion.<br />
This article presents a case <strong>of</strong> a 23-<br />
year-old man with amputation <strong>of</strong> his<br />
middle finger at the level <strong>of</strong> the proximal<br />
phalanx after being bitten <strong>by</strong> a horse.<br />
CASE REPORT<br />
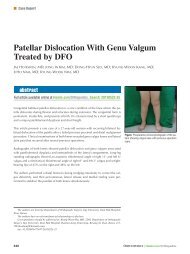
A 23-year-old right-handed man presented<br />
after being bitten <strong>by</strong> a horse, with amputation<br />
<strong>of</strong> his middle finger at the level <strong>of</strong> the proximal<br />
phalanx (Figure 1). The amputated stump was<br />
avulsed with the middle finger flexor digitorum<br />
pr<strong>of</strong>undus and the flexor digitorum superficialis<br />
from the muscle-tendon junction to the<br />
middle <strong>of</strong> the forearm (Figure 2). The patient<br />
reported pain in the proximal forearm. He had<br />
no other injuries, and he was able to move his<br />
other 4 fingers with only mild pain. The digit<br />
was not suitable for replantation.<br />
The wound was irrigated <strong>by</strong> saline and debrided.<br />
The edges <strong>of</strong> the phalanx were trimmed,<br />
and the edges <strong>of</strong> the wound were proximated <strong>by</strong><br />
single sutures nylon 4/0. Tetanus toxoid and rabies<br />
vaccine were administered, and the patient<br />
was given intravenous amoxicillin and clavulanic<br />
acid. The patient was discharged from the hospital<br />
2 days later with no sign <strong>of</strong> infection <strong>of</strong> the wound<br />
or compartment syndrome <strong>of</strong> the forearm.<br />
DISCUSSION<br />
In their classification system for ring<br />
avulsion injuries, Kay et al 2 described 4<br />
categories:<br />
● I—circulation adequate,<br />
● II—circulation inadequate,<br />
● III—circulation inadequate with fracture<br />
or a joint injury, and<br />
● IV—complete amputation.<br />
1 2<br />
Figure 1: Photograph showing the stump <strong>of</strong> the third fi nger. Figure 2: Photograph showing the amputated<br />
middle fi nger with the tendon attached up to the myotendinous junction. The avulsed fl exor digitorum<br />
pr<strong>of</strong>undus and fl exor digitorum superficialis are attached to the amputated fi nger, and a few muscle fibers<br />
are attached to the tendons in the proximal part.<br />
In their review <strong>of</strong> 55 cases <strong>of</strong> ring<br />
avulsion injuries, Kay et al 2 found 3 had<br />
adequate circulation and 8 had primary<br />
amputation. Salvage was attempted in 44<br />
cases; <strong>of</strong> these, 9 were amputated secondarily,<br />
19 were successfully revascularized,<br />
and 16 were successfully replanted.<br />
In 1974, Ponnampalam 5 described a<br />
case <strong>of</strong> a man working close to a conveyor<br />
belt who caught his right thumb on a side<br />
rail. The thumb was amputated at the base<br />
<strong>of</strong> the distal phalanx along with 25 cm<br />
<strong>of</strong> an avulsed flexor pollicis longus. The<br />
wound <strong>of</strong> the stump was covered with skin<br />
from the avulsed segment.<br />
In their study describing their revised<br />
classification, Kay et al 2 reported a case<br />
<strong>of</strong> a 45-year-old man whose finger was<br />
caught <strong>by</strong> a ring when he fell. The finger<br />
was completely amputated at the level <strong>of</strong><br />
the distal middle phalanx. Although the<br />
flexor digitorum pr<strong>of</strong>undus was avulsed<br />
from the musculotendinous junction, the<br />
flexor digitorum superficialis was intact.<br />
The finger was replanted with shortening<br />
and fusion <strong>of</strong> the distal interphalangeal<br />
joint. At his final follow-up examination,<br />
the patient was satisfied with the outcome.<br />
In another case report, Huemer and<br />
Dunst 6 described a 17-year-old adolescent<br />
who suffered a ring avulsion injury<br />
with amputation <strong>of</strong> the finger at the distal<br />
interphalangeal joint with avulsion <strong>of</strong> the<br />
flexor digitorum pr<strong>of</strong>undus from the myotendinous<br />
junction. The torn-out tendon<br />
was resected, and the amputated part <strong>of</strong><br />
the finger was replanted microsurgically.<br />
The final result was 50° <strong>of</strong> motion at the<br />
proximal interphalangeal joint and 30° <strong>of</strong><br />
motion at the distal interphalangeal joint.<br />
A search <strong>of</strong> the English literature did<br />
not reveal an injury that resulted in complete<br />
avulsion <strong>of</strong> both the flexor digitorum<br />
pr<strong>of</strong>undus and the flexor digitorum superficialis<br />
at the musculotendinous junction.<br />
A case <strong>of</strong> incomplete avulsion <strong>of</strong> both tendons<br />
was reported <strong>by</strong> Docker and Titley 7<br />
who described a 37-year-old woman who<br />
fell and whose ring finger was caught in a<br />
rack; the finger was amputated at the level<br />
<strong>of</strong> the midshaft <strong>of</strong> the middle phalanx. The<br />
distal finger was still attached to the hand<br />
via 10 to 15 cm <strong>of</strong> the flexor digitorum superficialis<br />
and flexor digitorum pr<strong>of</strong>undus<br />
tendons that were not completely avulsed.<br />
Interestingly, the patient developed compartment<br />
syndrome <strong>of</strong> the forearm, which<br />
was treated with a fasciotomy.<br />
Animal bites are relatively common,<br />
with a decreased order <strong>of</strong> frequency <strong>of</strong><br />
dogs, cats, and humans. <strong>Horse</strong> bites are<br />
relatively infrequent, but when they occur,<br />
they are associated with crush injuries and<br />
tissue loss. 8,9 Failure has been reported to<br />
occur with muscle strain injuries within<br />
the muscle belly, at the myotendinous<br />
junction, or within muscle near the myotendinous<br />
junction. 10<br />
Our case demonstrates the devastating<br />
power <strong>of</strong> a horse bite and its traction force<br />
in addition to its cutting force. This type<br />
e422<br />
ORTHOPEDICS | ORTHOSuperSite.com
AMPUTATION OF FINGER BY HORSE BITE | KOREN ET AL<br />
<strong>of</strong> bite demonstrates the weakest point in<br />
the myotendinous junction and emphasizes<br />
the importance <strong>of</strong> a careful physical<br />
examination <strong>of</strong> patients with a traumatic<br />
amputation. If the patient arrives with just<br />
the stump, the level <strong>of</strong> the tendon injury<br />
might not be recognized at first.<br />
REFERENCES<br />
1. Urbaniak JR, Evans JP, Bright DS. Microvascular<br />
management <strong>of</strong> ring avulsion injuries. J<br />
Hand Surg Am. 1981; 6(1):25-30.<br />
2. Kay S, Werntz J, Wolff TW. Ring avulsion<br />
injuries classification and prognosis. J Hand<br />
Surg Am. 1989; 14(2 pt 1):204-213.<br />
3. Boyes JH, Wilson JN, Smith JW. Flexor-tendon<br />
ruptures in the forearm and hand. J Bone<br />
Joint Surg Am. 1960; 42:637-646.<br />
4. Hussain SA. Traumatic amputation <strong>of</strong> the finger<br />
with complete avulsion <strong>of</strong> flexor pr<strong>of</strong>undus<br />
tendon. J Trauma. 1977; 17(3):241-242.<br />
5. Ponnampalam MS. Rupture <strong>of</strong> muscles <strong>by</strong><br />
traction. Injury. 1974; 5(3):237-238.<br />
6. Huemer GM, Dunst KM. Images in clinical<br />
medicine: finger avulsion with pulled-out flexor<br />
tendon. N Engl J Med. 2005; 352(6):e5.<br />
7. Docker C, Titley OG. A case <strong>of</strong> forearm compartment<br />
syndrome following a ring avulsion<br />
injury. Injury. 2002; 33(3):274-275.<br />
8. Kose R, Sogut O, Mordeniz C. Management<br />
<strong>of</strong> horse and donkey bite wounds: a series<br />
<strong>of</strong> 24 cases. Plast Reconstr Surg. 2010;<br />
125(6):251-252e.<br />
9. Vidal S, Barcala L,Tovar JA. <strong>Horse</strong> bite injury.<br />
Eur J Dermatol. 1998; 8(6):437-438.<br />
10. Tidball JG, Salem G, Zernicke R. Site and<br />
mechanical conditions for failure <strong>of</strong> skeletal<br />
muscle in experimental strain injuries. J Appl<br />
Physiol. 1993; 74(3):1280-1286.<br />
AUGUST 2011 | Volume 34 • Number 8<br />
e423