download magazine pdf - Ohio University College of Osteopathic ...
download magazine pdf - Ohio University College of Osteopathic ...
download magazine pdf - Ohio University College of Osteopathic ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Faculty monitor from a control room as students<br />
interview community members with Parkinson’s Disease<br />
in the Clinical Skills Assessment Lab.<br />
By 2030, one in five Americans will be 65 or<br />
older. The senior population will double to 71<br />
million in that year. But there will be only<br />
about 8,000 geriatricians.<br />
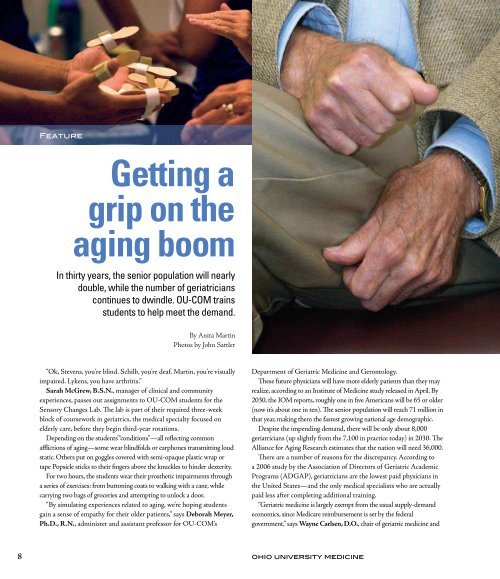
Feature<br />
Getting a<br />
grip on the<br />
aging boom<br />
In thirty years, the senior population will nearly<br />
double, while the number <strong>of</strong> geriatricians<br />
continues to dwindle. OU-COM trains<br />
students to help meet the demand.<br />
By Anita Martin<br />
Photos by John Sattler<br />
“Ok, Stevens, you’re blind. Schilb, you’re deaf. Martin, you’re visually<br />
impaired. Lykens, you have arthritis.”<br />
Sarah McGrew, B.S.N., manager <strong>of</strong> clinical and community<br />
experiences, passes out assignments to OU-COM students for the<br />
Sensory Changes Lab. The lab is part <strong>of</strong> their required three-week<br />
block <strong>of</strong> coursework in geriatrics, the medical specialty focused on<br />
elderly care, before they begin third-year rotations.<br />
Depending on the students’ “conditions”—all reflecting common<br />
afflictions <strong>of</strong> aging—some wear blindfolds or earphones transmitting loud<br />
static. Others put on goggles covered with semi-opaque plastic wrap or<br />
tape Popsicle sticks to their fingers above the knuckles to hinder dexterity.<br />
For two hours, the students wear their prosthetic impairments through<br />
a series <strong>of</strong> exercises: from buttoning coats to walking with a cane, while<br />
carrying two bags <strong>of</strong> groceries and attempting to unlock a door.<br />
“By simulating experiences related to aging, we’re hoping students<br />
gain a sense <strong>of</strong> empathy for their older patients,” says Deborah Meyer,<br />
Ph.D., R.N., administer and assistant pr<strong>of</strong>essor for OU-COM’s<br />
Department <strong>of</strong> Geriatric Medicine and Gerontology.<br />
These future physicians will have more elderly patients than they may<br />
realize, according to an Institute <strong>of</strong> Medicine study released in April. By<br />
2030, the IOM reports, roughly one in five Americans will be 65 or older<br />
(now it’s about one in ten). The senior population will reach 71 million in<br />
that year, making them the fastest growing national age demographic.<br />
Despite the impending demand, there will be only about 8,000<br />
geriatricians (up slightly from the 7,100 in practice today) in 2030. The<br />
Alliance for Aging Research estimates that the nation will need 36,000.<br />
There are a number <strong>of</strong> reasons for the discrepancy. According to<br />
a 2006 study by the Association <strong>of</strong> Directors <strong>of</strong> Geriatric Academic<br />
Programs (ADGAP), geriatricians are the lowest paid physicians in<br />
the United States—and the only medical specialists who are actually<br />
paid less after completing additional training.<br />
“Geriatric medicine is largely exempt from the usual supply-demand<br />
economics, since Medicare reimbursement is set by the federal<br />
government,” says Wayne Carlsen, D.O., chair <strong>of</strong> geriatric medicine and<br />
gerontology. “When all other expenses in the practice go up and Medicare<br />
reimbursements either stay the same or get cut, physician salaries go down.”<br />
Meanwhile, medical students typically incur between $120,000<br />
and $160,000 in educational debt, as reported by the Association <strong>of</strong><br />
American <strong>College</strong>s <strong>of</strong> Medicine reported in 2007.<br />
“With the rising costs <strong>of</strong> medical school, students are worried about<br />
repaying loans, which can deter even very interested students from<br />
becoming geriatricians,” says Katie Wehri, OMS III, who served as<br />
president <strong>of</strong> the OU-COM Geriatric Medicine Club last year.<br />
Wehri adds that because elderly patients <strong>of</strong>ten have multiple chronic<br />
conditions and can present symptoms differently, medical students<br />
may find it overwhelming to care for this population.<br />
It doesn’t help that few American medical schools actually require<br />
geriatric coursework. In 2006, the New York Times reported that <strong>of</strong> the<br />
145 U.S. medical schools at the time, only nine percent had a distinct<br />
department <strong>of</strong> geriatric medicine.<br />
“We’re pretty far ahead <strong>of</strong> the game at OU-COM in terms <strong>of</strong> what<br />
we <strong>of</strong>fer,” says Meyer, pointing out that the college’s former Geriatric<br />
Medicine/Gerontology Section (then in the Department <strong>of</strong> Family<br />
Medicine) gained departmental status in 1998. The three-week<br />
intensive geriatrics block <strong>of</strong> coursework began one year later.<br />
OU-COM students received distinctive geriatric medical training<br />
long before that. The Sensory Changes Lab dates back almost as far<br />
as the college itself, as does the required two- to four-week geriatrics<br />
rotation, which can be completed through any site in the Centers for<br />
<strong>Osteopathic</strong> Research and Education (CORE) system. And for 23<br />
years, OU-COM medical students have chosen to study international<br />
policy issues related to geriatric medicine in Edinburgh, Scotland,<br />
through the Charles J. Cannon Edinburgh Geriatric Tutorial.<br />
Meyer adds that OU-COM students begin thinking about geriatric<br />
medicine from the start. In 2007, geriatric medicine faculty facilitated 350<br />
hours in small-group, case-based studies; 80 hours in classroom and lab<br />
time and another 432 hours supervising students’ early clinical contact, all<br />
<strong>of</strong> which takes place within the first two years <strong>of</strong> medical school.<br />
“This is so important, because (physicians) will encounter more and more<br />
elderly patients in every area <strong>of</strong> medicine,” Meyer says. Especially in primary<br />
care, she adds, the field <strong>of</strong> choice for 54 percent <strong>of</strong> OU-COM graduates.<br />
An unexpected calling<br />
Sarah Snyder, D.O. (’06), wasn’t exactly looking forward to her<br />
required geriatric medicine rotation three years ago. “(The rotation<br />
is) perceived as somewhat sad—not exciting like sports medicine or<br />
cardiology,” she says. “I thought I wasn’t going to like it.”<br />
Snyder originally planned to go into pediatrics. But that changed<br />
when she began her geriatrics rotation.<br />
“There was one patient I interviewed, a female in her 90s, very frail,”<br />
Snyder says, “She talked to me for about an hour about how her life is,<br />
how it used to be.”<br />
When Snyder stood to go, she says the patient began crying. “She<br />
just thanked me for listening to her. She said a lot <strong>of</strong> docs are in and<br />
out, and that I really made her feel listened to. Right there I thought,<br />
wow. This is it. This is my calling.”<br />
Snyder is currently a family medicine resident at Firelands Hospital<br />
in Sandusky, <strong>Ohio</strong>. She has completed three additional geriatric medicine<br />
out-rotations as a resident: at Akron City Hospital, the Mountain Area<br />
Health Education Center in Asheville, N.C., and Christ Hospital in<br />
Cincinnati, <strong>Ohio</strong>.<br />
Snyder also received eight weeks <strong>of</strong> hospice training this year.<br />
Next she plans to pursue a fellowship in geriatric medicine, followed<br />
by another in palliative care (non-curative medicine aimed at relieving<br />
pain and suffering) before becoming a full-time geriatrician.<br />
“That (initial required geriatrics) rotation is the whole reason I’m<br />
choosing geriatrics. It gave me a new respect for the field,” Snyder<br />
says. “I really thought the experience was much more in line with the<br />
osteopathic philosophy than a lot <strong>of</strong> my other rotations in terms <strong>of</strong><br />
treating the whole patient, physically, mentally and emotionally.”<br />
To illustrate the holistic approach to treating older adults, Snyder<br />
describes how, upon starting her residency in Akron, she was given<br />
a five-page questionnaire to go over with each new patient. It covers<br />
everything from medications, sleep patterns and diet to social habits,<br />
mood trends and living space.<br />
“I found that I really love home visits, seeing people in their own<br />
environment,” Snyder says. “Now I can’t imagine practicing medicine<br />
without understanding how patients function in their everyday lives.”<br />
8 ohio university medicine Winter 2009<br />
9