DO - Ohio University College of Osteopathic Medicine
DO - Ohio University College of Osteopathic Medicine
DO - Ohio University College of Osteopathic Medicine
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>DO</strong><br />
perspectives from<br />
the college <strong>of</strong> osteopathic medicine<br />
TODAY’S<br />
summer 2006 volume 24.2 ohio university<br />
Pediatrics<br />
a Growing Specialty
TODAY’S<strong>DO</strong><br />
<strong>DO</strong><br />
Dean’s Message<br />
Today’s D.O. is published two<br />
times a year by the Office <strong>of</strong><br />
Communication <strong>of</strong> the <strong>Ohio</strong> <strong>University</strong><br />
<strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong>.<br />
Editorial <strong>of</strong>fices:<br />
Room 330, Grosvenor Hall,<br />
<strong>Ohio</strong> <strong>University</strong>, Athens, <strong>Ohio</strong>, 45701.<br />
Editorial Board<br />
Susan Lash Blanchard<br />
Assistant Dean for Development<br />
George F. Dunigan II<br />
Director <strong>of</strong> Governmental Affairs<br />
Mathew J. Rose<br />
Student Government President<br />
Edwin C. Rowland, Ph.D.<br />
Chair, Department<br />
<strong>of</strong> Biomedical Sciences<br />
John D. Schriner, Ph.D.<br />
Director <strong>of</strong> Admissions<br />
Sharon B. Zimmerman<br />
Director <strong>of</strong> Alumni Affairs<br />
Content Editor<br />
Sally Linder<br />
Copy Editor<br />
Shelby S. Mullins<br />
Design<br />
Kari Gunter-Seymour<br />
Photography<br />
John P. Sattler<br />
Writers and Contributors<br />
Kirsten Brown<br />
Melissa Cabral<br />
Melissa Rake Calhoun<br />
Maureen Harmon<br />
Richard Heck<br />
Linda Knopp<br />
Jennifer Kowalewski<br />
Sally Linder<br />
Joy Rodgers<br />
Administration<br />
Roderick J. McDavis, Ph.D<br />
President, <strong>Ohio</strong> <strong>University</strong><br />
John A. Brose, D.O.<br />
Dean, <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong><br />
Karoline Lane<br />
Director, Office <strong>of</strong> Communication<br />
Opinions expressed in Today’s D.O. are<br />
those <strong>of</strong> the authors and<br />
do not necessarily reflect<br />
viewpoints <strong>of</strong> the editors or <strong>of</strong>ficial<br />
policy <strong>of</strong> the <strong>Ohio</strong> <strong>University</strong><br />
<strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong>.<br />
© ’06 <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong>.<br />
Address updates for Today’s D.O.<br />
should be referred to Sheila Byc<strong>of</strong>ski,<br />
OU-COM, 332 Grosvenor Hall,<br />
Athens, OH 45701.<br />
phone: (740) 593-2346<br />
e-mail: byc<strong>of</strong>ski@ohio.edu.<br />
Few would argue that the osteopathic medical pr<strong>of</strong>ession is one <strong>of</strong> the<br />
major success stories in health care. The quality <strong>of</strong> our students and<br />
educational programs is higher than ever.<br />
Research was once the weak companion to teaching and service.<br />
This is no longer the case. Our students won’t allow it.<br />
Historically, many <strong>of</strong> the principles <strong>of</strong> our pr<strong>of</strong>ession were based on anecdote and shared<br />
experiences, rather than solid medical evidence. Today’s osteopathic medical student is<br />
too scientifically sophisticated to accept that. Dr. Norman Gevitz, pr<strong>of</strong>essor <strong>of</strong> social<br />
medicine at OU-COM, discussed this issue in a recent JAOA article when he noted,<br />
“<strong>Osteopathic</strong> students wish to see evidence. They want pro<strong>of</strong>. Instead <strong>of</strong> scientific<br />
demonstrations, however, they get only case reports, anecdotes, testimonials, theories,<br />
speculations, reasoning by analogy, and pilot studies. These studies typically have few<br />
subjects and usually prove little or nothing.”<br />
I believe that we are moving to another level in interpreting our own literature. Early in<br />
our pr<strong>of</strong>ession’s history, osteopathic research <strong>of</strong>ten suffered from inadequate numbers <strong>of</strong><br />
subjects, methodological error and misinterpretation <strong>of</strong> data. When studies came to the<br />
conclusions we desired, we were willing to ignore methodological flaws and quote them.<br />
One example <strong>of</strong> this is the frequently cited 1918 AOA survey regarding osteopathic care<br />
during the Spanish flu epidemic. Although this survey had significant methodological<br />
problems that prevented any significant conclusions being drawn, even 88 years later it is<br />
frequently cited. Similarly, even if our own studies spoke against commonly held beliefs,<br />
we sometimes ignored all or part <strong>of</strong> the findings.<br />
Fortunately, things are changing. <strong>Osteopathic</strong> medical schools located at state universities<br />
are building major research programs in many different areas. The AOA’s <strong>Osteopathic</strong><br />
Research Center has created well-designed research protocols to answer basic questions<br />
regarding traditional osteopathic therapy. These studies will create a scientific basis for<br />
OMM instruction.<br />
At the <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong>, we are joining forces with the Russ<br />
<strong>College</strong> <strong>of</strong> Engineering and Technology to build a multidisciplinary research center, the<br />
Integrated Learning and Research Facility, that is slated to open in 2009. This new facility,<br />
funded in part by the <strong>Osteopathic</strong> Heritage Foundations, will bring together the research<br />
talents <strong>of</strong> faculty from multiple <strong>Ohio</strong> <strong>University</strong> colleges. And whether or not studies show<br />
what we want them to, they will be published and integrated into our curriculum.<br />
This emphasis on quality research and the merging <strong>of</strong> research and education is a fundamental<br />
change in the approach to osteopathic medical education. The <strong>Ohio</strong> <strong>University</strong> <strong>College</strong><br />
<strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong> will continue its efforts to lead in that transition. Our students<br />
won’t have it any other way.<br />
Jack Brose, D.O.<br />
Dean, <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong><br />
<strong>Osteopathic</strong> <strong>Medicine</strong><br />
www.oucom.ohio.edu
<strong>DO</strong><br />
the college <strong>of</strong> osteopathic medicine<br />
TODAY’S<br />
TODAY’S<strong>DO</strong><br />
perspectives from<br />
Features<br />
The Hospitalist<br />
More D.O.s are becoming hospitalists, and the<br />
practice is moving quickly toward specialty status.<br />
These hospital-based physicians are changing the<br />
very nature <strong>of</strong> inpatient care.<br />
Number <strong>of</strong> General Pediatricians<br />
By Year (x1000) 14<br />
80<br />
8<br />
The Obstetrics Dilemma<br />
Obstetrics practices are especially hard hit by<br />
soaring malpractice premiums and litigation. No<br />
one is happy about the compromises physicians<br />
and patients have to make.<br />
60<br />
40<br />
20<br />
18<br />
28<br />
From Diapers to Driver’s Licenses<br />
Pediatrics is capturing a bigger share <strong>of</strong> graduates<br />
who find the primary-care specialty has special<br />
rewards–even if compensation isn’t necessarily<br />
one <strong>of</strong> them.<br />
Pr<strong>of</strong>iles<br />
Each <strong>of</strong> these OU-COM graduates is practicing<br />
medicine under challenging circumstances, but not<br />
one <strong>of</strong> them would trade in the experience for<br />
lighter duty.<br />
0<br />
1975<br />
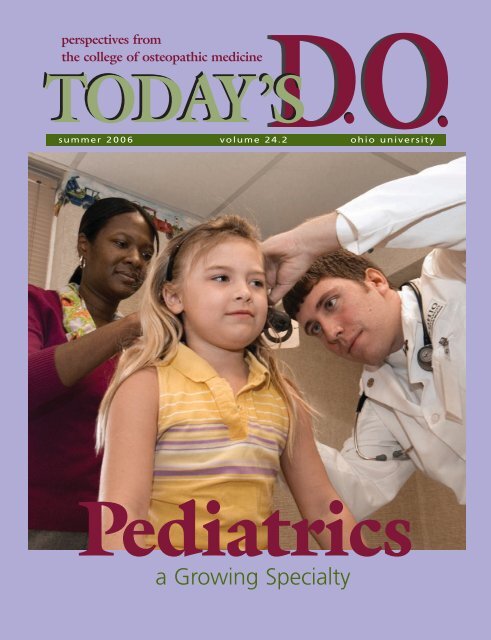
On the cover…<br />
Pediatrician Celeste Wallace,<br />
D.O. (‘02), and Dave Valent,<br />
OMS II, examine Tia, 8, a patient<br />
in Dr. Wallace's practice at<br />
<strong>University</strong> Medical Associates.<br />
2003<br />
2 News<br />
24 Celebrate<br />
26 Research News<br />
32 CORE News<br />
34 Alumni Update<br />
36 Congratulations
News<br />
A Virtually Perfect Back<br />
W<br />
ithin just one session <strong>of</strong> using the<br />
Virtual Haptic Back, first-year medical<br />
student Aaron Miller already could tell a<br />
difference in his palpation skills. Now Miller<br />
believes the revolutionary computer<br />
program should become a requirement<br />
for all students at <strong>Ohio</strong> <strong>University</strong> <strong>College</strong><br />
<strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong>.<br />
“Haptic Back is one <strong>of</strong> the most<br />
interesting and intelligently<br />
designed machines I have ever<br />
come across,” Miller says. “It<br />
was fascinating to use. It allows<br />
one to better understand<br />
what they should be feeling<br />
for (before working on the<br />
patients themselves).”<br />
The s<strong>of</strong>tware is an <strong>Ohio</strong><br />
<strong>University</strong> creation, developed<br />
four years ago by members <strong>of</strong><br />
the Interdisciplinary Institute<br />
for Neuromusculoskeletal<br />
Research (IINR), a multicollege<br />
project focusing on human<br />
neuromusculoskeletal research<br />
and clinical treatments.<br />
The Virtual Haptic Back<br />
Laboratory in OU-COM’s<br />
Irvine Hall houses the<br />
computer equipment that<br />
simulates the sensation <strong>of</strong> a<br />
back in various states, according to John<br />
Howell, Ph.D., IINR director and associate<br />
pr<strong>of</strong>essor <strong>of</strong> physiology in Biomedical<br />
Sciences at OU-COM. It eliminates the<br />
need to find human models on demand<br />
with the right conditions.<br />
Users place their fingertips into two robotic<br />
arms and “feel” in virtual space the<br />
sensation <strong>of</strong> a back in its normal state<br />
and with various somatic dysfunctions.<br />
The computer generates a tight muscle<br />
or strain, for instance, and the student<br />
can palpate a reliable reproduction <strong>of</strong><br />
the anomaly.<br />
“Anyone truly interested in osteopathic<br />
manipulative medicine should try it,”<br />
Miller says.<br />
Students took a pretest, performed eight<br />
sessions on the simulator and followed<br />
with a post-test. According to Howell, data<br />
showed distinct improvement.<br />
Tony Le, a first-year medical student, had<br />
palpated live subjects in the osteopathic<br />
manipulative medicine (OMM) lab for six<br />
months before trying the Virtual Haptic<br />
Back. ”I believe that it has enhanced my<br />
abilities to detect more sensitive areas,”<br />
he says. Le agrees with Miller that the<br />
Virtual Haptic Back should become part<br />
<strong>of</strong> OU-COM’s curriculum.<br />
After more studies, Howell says the<br />
university would like to see the s<strong>of</strong>tware<br />
nationwide, helping other future physicians<br />
better their manual medicine skills.<br />
Other OU-COM team members involved<br />
in the Virtual Haptic Back include David<br />
C. Eland, D.O., associate pr<strong>of</strong>essor <strong>of</strong> OMM<br />
in Family <strong>Medicine</strong>; Janet M. Burns, D.O.<br />
('95), assistant pr<strong>of</strong>essor <strong>of</strong> OMM in<br />
Family <strong>Medicine</strong>; Robert R. Conatser,<br />
research associate, IINR; and medical<br />
student Allen McGrew.<br />
Heptic Back and the IINR are supported in<br />
part by grants from the <strong>Osteopathic</strong> Heritage<br />
Foundations.<br />
–Jennifer Kowalewski<br />
John Howell, Ph.D. (left), and David Noyes, Ph.D. (right), watch as Robert Conatser settles<br />
Janet Burns, D.O., into the Virtual Haptic Back.<br />
2 www.oucom.ohio.edu
Noteworthy<br />
Ronald Moomaw, D.O (‘80), will join other renowned experts on the National Commission on Correctional<br />
Health Care to draft recommendations for improving the quality <strong>of</strong> health care in jails, prisons and juvenile<br />
confinement facilities. Moomaw’s three-year term on the 38-member commission begins in<br />
October 2006. At that time, he will join one <strong>of</strong> seven task-oriented committees charged with<br />
establishing best practices for correctional health care, monitoring correctional health-care services<br />
and ensuring a high standard <strong>of</strong> care at correctional facilities. Moomaw, who has been involved<br />
in correctional health-care issues throughout his career, is currently chief psychiatrist for the<br />
<strong>Ohio</strong> Department <strong>of</strong> Rehabilitation and Corrections. He also served on the governing boards<br />
<strong>of</strong> several correctional facilities in <strong>Ohio</strong>, including Oakwood Correctional Facility in Lima.<br />
Moomaw joined the OU-COM Society <strong>of</strong> Alumni and Friends as a board member this year.<br />
Keith Watson, D.O., associate dean for graduate medical education, chaired the steering committee <strong>of</strong> the first<br />
osteopathic medical education summit held in Chicago Jan. 26-29. The summit, which was funded by the<br />
<strong>Osteopathic</strong> Heritage Foundations, American <strong>Osteopathic</strong> Association and American Association<br />
<strong>of</strong> <strong>College</strong>s <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong>, brought together a gathering <strong>of</strong> 70 policymakers, administrators,<br />
educators and physicians to participate in frank discussions about the future <strong>of</strong> osteopathic<br />
medical education and a potential critical shortage <strong>of</strong> physicians by the year 2020, as projected<br />
by the federal Council on Graduate Medical Education. As chairman, Watson was responsible for<br />
overseeing organization and direction <strong>of</strong> the summit. The summit examined four key areas<br />
affecting medical education: 1) workforce; 2) recruitment, particularly for medical schools and<br />
graduate medical education; 3) funding issues for medical education and postgraduate training<br />
programs; and 4) defining standards for evaluating the quality <strong>of</strong> medical education.<br />
As a member <strong>of</strong> <strong>Ohio</strong> Gov. Bob Taft’s Medicaid Administrative Study Council, Brian Phillips,<br />
chief information <strong>of</strong>ficer for OU-COM, will have a hand in enhancing health-care services in the<br />
state. Tasked with examining the administration <strong>of</strong> <strong>Ohio</strong>’s Medicaid program and coming up<br />
with a plan for creating a new Medicaid department, the council has until Dec. 31 to issue a<br />
final report. The General Assembly is expected to enact recommendations into law by July 1,<br />
2007. Phillips’ was appointed, in part, because <strong>of</strong> his background in health information technology<br />
and his current work in computerizing medical records.<br />
George F. Dunigan, OOA and OU-COM director <strong>of</strong> government relations, received the 2006 <strong>Ohio</strong> <strong>Osteopathic</strong><br />
Association Meritorious Service Award in June. The award, the highest honor that the association confers, recognizes<br />
outstanding accomplishments in scientific, philanthropic or other fields <strong>of</strong> public service. Dunigan<br />
has been an advocate for osteopathic medicine for the past 31 years. As a lobbyist for the <strong>Ohio</strong><br />
<strong>Osteopathic</strong> Association he was instrumental in securing passage <strong>of</strong> the 1975 legislation calling<br />
for the creation <strong>of</strong> an osteopathic medical school at <strong>Ohio</strong> <strong>University</strong>. He helped the pr<strong>of</strong>ession<br />
build support for OU-COM among state lawmakers. He continues as an advocate today, working<br />
daily with key governmental <strong>of</strong>ficials at the state and national level on policy issues related to<br />
medical education, Medicaid, workers compensation and pr<strong>of</strong>essional liability insurance.<br />
Larry Robinson, D.O. (‘02); Benjamin Forrester, D.O. (‘03); Darnell Ladson (‘03); Suzanne Morgan, D.O.<br />
(‘04) and Jean Rettos, D.O. (‘04), were named 2005 Humanism and Excellence in Teaching Award recipients.<br />
This honor, which the Arnold P. Gold Foundation sponsors, recognizes residents who have excelled at teaching<br />
and exhibited a high level <strong>of</strong> compassion toward patients, families, students and colleagues.<br />
–Joy L. Rodgers and Kevin Sanders<br />
summer 2006 3
News<br />
A Pathway to <strong>Medicine</strong><br />
T<br />
hanks to an innovative partnership with Columbus area schools, the <strong>Ohio</strong> <strong>University</strong><br />
<strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong> hopes to funnel a broader range <strong>of</strong> students into its<br />
pipeline <strong>of</strong> future physicians.<br />
In the new Pathways Institute Partnership, OU-COM has teamed with Columbus Public Schools,<br />
Columbus State Community <strong>College</strong> and other organizations to help students from lower<br />
income families or whose parents never attended college realize that being a doctor is<br />
not out <strong>of</strong> their reach.<br />
There’s an overall shortage <strong>of</strong> people seeking health-care careers, according to Elizabeth<br />
Minor, Health Careers Opportunities Program (HCOP) program director at OU-COM.<br />
“Our program educates and encourages young people that likely don’t know there are<br />
very good career opportunities in the health-care industry. We want them to know that<br />
they have options and help them reach their goals,” she says. Students learn what to focus<br />
on to make their career a reality.<br />
Arla Lyles has signed on as director <strong>of</strong> the Pathways Institute Partnership, housed in Columbus.<br />
She will oversee several initiatives that prepare students, as young as sixth graders, to navigate<br />
the steps toward health-care careers, including osteopathic medicine. By 2008, the partnership<br />
hopes to attract 275 students to OU-COM and other <strong>Ohio</strong> <strong>University</strong> health-care programs.<br />
The Partnership comprises seven middle schools; Columbus State; OU-COM; <strong>Ohio</strong> <strong>University</strong><br />
<strong>College</strong> <strong>of</strong> Arts and Sciences; three Columbus high-schools with health academies (East<br />
High, West High and Linden-McKinley High); and community health-care resources such as<br />
the city <strong>of</strong> Columbus Public Health Department and Doctors Hospital in Columbus.<br />
Pathways came about in part because <strong>of</strong> Minor’s chance meeting with John Francis, Ph.D.,<br />
a Columbus State biochemistry pr<strong>of</strong>essor. Minor says she and Francis began a conversation<br />
aboard a plane in 2001 about what they did at their institutions. Four years later, they<br />
finalized the Pathways Institute Partnership.<br />
Students first gain admission to Columbus State, where some will enter two-year programs<br />
related to health care. Students who want to continue their education, however, can easily<br />
transfer key credits to <strong>Ohio</strong> <strong>University</strong>.<br />
Students involved in Pathways also can participate in the OU-COM Summer Scholars Program,<br />
a rigorous premedical program designed to enhance preparation for admission to medical<br />
school and increase chances <strong>of</strong> acceptance.<br />
–Jennifer Kowalewski<br />
4 www.oucom.ohio.edu
photo provided by Julianna Batizy-Morely, D.O.<br />
OU-COM Grad Goes World Class<br />
I<br />
n an event that attracts more than 3,000 amateur<br />
triathletes from around the world, Julianna Batizy-<br />
Morley, D.O. (‘96), won the 2005 International<br />
Triathlon Union’s World Championship in Honolulu<br />
last October.<br />
Victory was even sweeter because just a year earlier<br />
on Thanksgiving, Batizy-Morley passed out while<br />
swimming and was diagnosed with multiple<br />
bilateral pulmonary emboli. According to her father,<br />
Levente Batizy, D.O., director <strong>of</strong> medical education<br />
at South Pointe Hospital, Cleveland, <strong>Ohio</strong>, and CORE<br />
clinical pr<strong>of</strong>essor <strong>of</strong> emergency medicine, “she<br />
could barely walk across the room without getting<br />
short <strong>of</strong> breath.”<br />
“It was a huge setback physically and took me six<br />
months or more to recover,” Batizy-Morley says.<br />
Doctors were not even sure she would regain pulmonary<br />
function. The emboli left her with joint pain, mouth<br />
sores, hoarseness and possible connective tissue disease.<br />
Against all those odds, however, she trained to<br />
become No.1 in the world for her class.<br />
Batizy-Morley completed the grueling 1,500 meter<br />
open-water swim, 40-kilometer bike course and 10-<br />
kilometer run in two hours, 12 minutes and 57<br />
seconds to win the female 35-39 age division. She<br />
was one <strong>of</strong> only 18 women in her age group to earn<br />
a place at the Worlds.<br />
“To see her on top <strong>of</strong> the podium in Honolulu …<br />
was an absolute thrill,” her father says.<br />
Batizy-Morley, who had been a competitive swimmer<br />
in high school, didn’t even start thinking about<br />
triathlons until almost two decades later.<br />
“I had done one or two (triathlons) in <strong>Ohio</strong> when I<br />
lived there just to see what they were like,” she says,<br />
“but didn’t take them too seriously.”<br />
Her children’s swim team coach, Gregory Zgliczynski,<br />
saw one <strong>of</strong> her swims and suggested she make the<br />
switch to triathlons. In 2003 Zgliczynski began coaching<br />
Batizy-Morley, and in May <strong>of</strong> 2004, at the age <strong>of</strong> 33,<br />
she won her first triathlon.<br />
Batizy-Morley trains hard and works as an emergency<br />
room physician, “every other week, every other<br />
day,” to reconcile the demands <strong>of</strong> motherhood with<br />
her 20-hour-a-week training schedule. On work<br />
weeks, for instance, she might be up 36 hours<br />
straight. Does she ever sleep? “That’s the million dollar<br />
question,” she laughs. “I don’t sleep as much as I<br />
should. I guess residency was a good way to get<br />
used to it.”<br />
Batizy-Morley is now setting her sights on a bigger<br />
goal: to become a pr<strong>of</strong>essional triathlete. That will<br />
require her to compete in at least three races with<br />
more than 500 participants and place in the top<br />
eight. With two such wins already under her belt as<br />
<strong>of</strong> this writing, she was confident she could cinch the<br />
third in the spring.<br />
Zgliczynski has no doubt she’ll join the pros.<br />
“At the age <strong>of</strong> 30, many people look for the easy way<br />
out,” he says. “She’s almost like a teenager with dreams,<br />
day in, day out, willing to take a lot <strong>of</strong> punishment.”<br />
–Sally Linder and Melissa Cabral<br />
Despite bilateral pulmonary emboli, Julianna Batizy-Morely, D.O. (‘96), rose to world-class status as a triathlete.<br />
summer 2006 5
News<br />
OU-COM’s Newest Scholarship<br />
–One More Molea Legacy<br />
A<br />
sk any nurse. Any colleague. Any student. Any patient.<br />
Ask anyone who knew John S. Molea, D.O., and in<br />
one way or another, they’ll say he was extraordinary.<br />
“He was one <strong>of</strong> the warmest people I ever met. He<br />
treated every individual as someone important,”<br />
<strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong><br />
Dean Jack Brose, D.O., says. “He was impossible not<br />
to like.”<br />
Molea, former associate dean for academic and clinical<br />
education at OU-COM, also was a pioneer, bringing<br />
about sea changes in the college’s third- and fourthyear<br />
rotation system. Working with assistant deans<br />
at the hospitals, he<br />
helped develop goals<br />
and objectives to standardize<br />
and improve<br />
clinical education at all<br />
sites. That created a<br />
foundation for the work<br />
he, Brose, former Dean<br />
Barbara Ross-Lee, D.O.,<br />
Chistopher T. Meyer, D.O.<br />
and Cheryl Riley, R.N.,<br />
M.S. did to establish in<br />
1995 a statewide medical<br />
education consortium,<br />
now known as the Centers<br />
for <strong>Osteopathic</strong> Research<br />
and Education (CORE).<br />
(See Winter 2006 Today’s<br />
D.O. for more on the<br />
CORE’s history.)<br />
CORE restructured the<br />
regional system and is<br />
nationally recognized as<br />
a standard for clinical<br />
teaching systems. “Now all hospitals work together<br />
as partners, not individual entities,” says Riley, assistant<br />
dean for CORE and Academic Affairs operations,<br />
stressing the importance <strong>of</strong> Molea’s contribution.<br />
”He had built strong relationships with and understood<br />
the teaching climate <strong>of</strong> the hospitals at the time.<br />
His knowledge and understanding <strong>of</strong> the continuum<br />
curriculum concept that was being fostered also lent<br />
credibility to the plan,” Riley says, with the same respect<br />
you hear in everyone’s voice who speaks <strong>of</strong> Molea.<br />
An associate pr<strong>of</strong>essor <strong>of</strong> surgery, Molea had the<br />
same deep relationship with students as he did with<br />
colleagues. “When students saw him, they greeted<br />
him like he was their father. They just loved him,”<br />
Brose says. It wasn’t just his good nature they<br />
appreciated, but also the encouragement to excel.<br />
Molea established the John S. Molea, D.O., Endowed<br />
Fund for Outstanding Case-Based Report Award for<br />
third- and fourth-year students. To motivate scholarship<br />
in case reports and literature reviews, he dangled a<br />
carrot: “The student authors <strong>of</strong> the top three papers<br />
each year receive a check and a plaque, with the best<br />
paper getting published in the OU-COM’s <strong>Ohio</strong> Research<br />
and Clinical Review journal,” Riley says<br />
In 1992, the National <strong>Osteopathic</strong> Foundation<br />
recognized Molea’s gift for teaching, selecting him<br />
as Educator <strong>of</strong> the Year. It was the first time the<br />
prestigious award had been conferred upon an OU-COM<br />
faculty member. The award is given annually to the<br />
educator who exemplifies and encourages osteopathic<br />
principles in his or her students.<br />
To continue and expand his support <strong>of</strong> students as he<br />
wished, his wife, Nellie, endowed the new Molea<br />
Scholarship Fund after his death last October. It will<br />
help third-year student recipients who have participated<br />
in community service to <strong>of</strong>fset education costs. The<br />
Case-Based Report Award will continue receiving funding<br />
through 2007.<br />
Molea came to OU-COM in 1976 and retired in 1994<br />
but continued to teach until 1997. He is remembered<br />
as an extraordinary surgeon, mentor, leader and man.<br />
He also will be remembered for leaving OU-COM a<br />
better place, according to Brose, who says Molea is<br />
one <strong>of</strong> an elite few to make such a lasting impression<br />
on the college.<br />
“The college could not have attained the academic<br />
reputation it has today without him,” he says.<br />
–Sally Linder<br />
If you wish to contribute, send your donation marked<br />
Molea Scholarship Fund to Susan Lash Blanchard,<br />
assistant dean for development, <strong>Ohio</strong> <strong>University</strong><br />
<strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong>, 205 Grosvenor Hall,<br />
Athens, OH 45701. For information, contact Blanchard<br />
at blanchas@ohio.edu or (740) 593-2151.<br />
John Molea, D.O., stood out at OU-COM for being an exceptional surgeon, mentor and leader .<br />
6 www.oucom.ohio.edu
Opportunities<br />
With 32 active donor-generated scholarships,<br />
<strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong><br />
alumni, friends and colleagues have established<br />
an impressive giving legacy. On average, OU-COM<br />
presents approximately $100,000 annually in<br />
awards that range from $500 to $10,000 per<br />
recipient. The amount depends on the supporting<br />
fund’s value. Fortunately for future generations<br />
<strong>of</strong> medical students, most <strong>of</strong> the funds are endowed<br />
and, therefore, perpetual.<br />
Want to be a donor? Consider creating a<br />
scholarship or contributing to any <strong>of</strong> the existing<br />
scholarship funds supporting OU-COM students.<br />
Scholarship descriptions vary according to donors’<br />
wishes and, when designated, the needs <strong>of</strong> the<br />
college. Here are a few examples:<br />
• Charles “Chip” Rogers Tribute Scholarship<br />
is relatively new. It was created by friends, family<br />
and colleagues <strong>of</strong> Rogers upon his retirement and<br />
in honor <strong>of</strong> his 28-year career with OU-COM. The<br />
college chooses the criteria annually depending<br />
on what will most benefit the class pool. This<br />
flexibility makes the Rogers Fund particularly<br />
beneficial in attracting students to OU-COM who<br />
otherwise would go to schools that are less<br />
expensive or have more scholarships to <strong>of</strong>fer.<br />
• Jerry A. Zinni, D.O., Memorial Scholarship<br />
annually supports four students from northeastern<br />
<strong>Ohio</strong> and honors Zinni, who was founder and<br />
principal leader <strong>of</strong> Richmond Heights (<strong>Ohio</strong>)<br />
General Hospital. The fund was established<br />
through the generosity <strong>of</strong> the Northeastern <strong>Ohio</strong><br />
HealthCare Foundation.<br />
• Walter J. Costello, Ph.D., Scholarship<br />
pays tribute to Costello, an OU-COM pr<strong>of</strong>essor<br />
<strong>of</strong> microanatomy, who died in 1998 at age 52.<br />
During 2002, thanks to his many friends and<br />
colleagues, the Costello Memorial Fund reached<br />
endowment level for students with academic<br />
merit in the Patient-Centered Curriculum program.<br />
• Bernard Master, D.O., Scholarship was<br />
established by Master <strong>of</strong> Worthington, <strong>Ohio</strong>, in the<br />
early 1990s. Today, 30-plus students have benefited<br />
from this award and continue to fulfill his interest<br />
<strong>of</strong> encouraging our medical students to pursue<br />
careers in urban medically underserved areas.<br />
–Susan Lash Blanchard<br />
Library Makes House Calls<br />
S<br />
tudents and faculty won’t always have to trudge up the Richland<br />
Avenue hill to do their research. The library has come to them.<br />
In October, the <strong>Ohio</strong> <strong>University</strong> Health Sciences Library at Alden Library<br />
opened a satellite in Irvine Hall to help students and faculty at <strong>Ohio</strong><br />
<strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong> with research, including mining<br />
online databases.<br />
“We thought it would add some value to OU-COM to have a small <strong>of</strong>fice<br />
here,” said Cheryl Ewing, director <strong>of</strong> the Health Sciences Library at Alden.<br />
Librarians staffing the satellite include Medical Reference and Instruction<br />
Librarian Susan Foster-Harper, Health Science Reference and Community<br />
Outreach Librarian Debi Orr and Biology Librarian Whitney Winberg.<br />
Ewing also spends time at the facility. The librarians generally rotate in<br />
for half-day stints, ensuring the <strong>of</strong>fice is staffed throughout the day.<br />
The librarians will travel to OU-COM <strong>of</strong>fices; they arrive equipped with<br />
wireless laptops to give one-on-one help exploring the Internet for<br />
research resources.<br />
At other times, the librarians serve drop-ins. “There’s a lot <strong>of</strong> traffic and a<br />
variety <strong>of</strong> people coming to see us,” Foster-Harper says. That includes the<br />
whole gamut at OU-COM: students, clinical instructors, faculty members<br />
and staff.<br />
“I don’t think (most people) know the wonders <strong>of</strong> the medical database,”<br />
Ewing says. “Our role as librarians is not only to find the good information<br />
but to help people find it on their own.”<br />
–Jennifer Kowalewski<br />
Wayne Carlsen, D.O., takes advantage <strong>of</strong> a library “house call”<br />
from librarian Susan Foster-Harper in between donating blood<br />
and heading for the hospital.<br />
summer 2006 7
photo by Lee Ann Yahle<br />
The<br />
Hospitalist<br />
8 www.oucom.ohio.edu
For nearly 10 years, Robin Thomas, D.O. (‘91), was in private practice<br />
in internal medicine. Now, she works 24-hour shifts caring for hospitalized<br />
patients–sometimes as many as 20 to 25 a day–at Blanchard Valley<br />
Regional Health Center in Findlay, <strong>Ohio</strong>. She misses the close<br />
relationships with her private-practice patients, but for her, she’s found<br />
a niche in this new role.<br />
“I always liked the hospital so much more than the <strong>of</strong>fice, so it was a<br />
good fit,” she says.<br />
Thomas is among a growing number <strong>of</strong> physicians who have become<br />
inpatient care providers in recent years. Hospitalists, as these medical<br />
providers <strong>of</strong>ten are called, oversee acute care for hospitalized patients,<br />
a role that previously had been the province <strong>of</strong> the primary care<br />
physician or specialists. “Hospitalists provide a service to...doctors<br />
who <strong>of</strong>ten are too busy with their practices to come to the hospital<br />
regularly,” says Jose Torres, D.O. (‘98), who works as a hospitalist at<br />
Grandview Hospital/Kettering Medical Center in Dayton, <strong>Ohio</strong>.<br />
“Without hospitalists, rounds could go on forever.”<br />
The number <strong>of</strong> physicians<br />
who oversee acute care in<br />
hospitals is growing.<br />
by Linda C. Knopp<br />
A Movement Takes Root<br />
Having physicians on staff to manage inpatient care isn’t a new<br />
phenomenon, but it is creating a growing field <strong>of</strong> medicine. In a 1996<br />
New England Journal <strong>of</strong> <strong>Medicine</strong> article, authors Robert Wachter, M.D.,<br />
and Lee Goldman, M.D., first coined the term “hospitalist” to describe<br />
a physician who spends a significant amount <strong>of</strong> work time in hospitals.<br />
Today, the Society <strong>of</strong> Hospital <strong>Medicine</strong> (SHM), a Philadelphia-based<br />
membership organization for inpatient care providers, defines hospitalists<br />
as “physicians whose primary pr<strong>of</strong>essional focus is the general medical<br />
care <strong>of</strong> hospitalized patients. Their activities include patient care, teaching,<br />
research and leadership related to hospital medicine.”<br />
SHM estimates that there are approximately 15,000 practicing<br />
hospitalists in the United States today–up from just a few hundred in<br />
the late 1990s and no more than a handful in the early ’70s. Even when<br />
Thomas completed her internal medicine residency at Akron City<br />
Hospital in 1995, most primary care physicians didn’t consider inpatient<br />
care a career choice. “At that time, there weren’t many hospitalists,” she<br />
says. “Everyone had private practices and did inpatient work. The only<br />
physicians with hospital practices were critical care, ER and anesthesia.”<br />
Thanks, in part, to increased demands on the time <strong>of</strong> physicians with<br />
<strong>of</strong>fice practices, increased pressure from society to provide cost-effective<br />
and quality care to hospital inpatients, and limits on the number <strong>of</strong><br />
hours medical residents could work, the field <strong>of</strong> hospital medicine had<br />
taken <strong>of</strong>f by 2005 when Eric Schumacher, D.O. (’00), completed his<br />
residency in internal medicine and pediatrics at Wright State <strong>University</strong><br />
in Dayton. Because the work schedule and job duties appealed to him,<br />
Schumacher accepted a position as a hospitalist at <strong>Ohio</strong> State<br />
<strong>University</strong> Medical Center in Columbus, where he cares for patients<br />
through the hospital’s general inpatient service, its James Cancer<br />
hospitalist service and its Ross Heart hospitalist service. He also cares<br />
for hospitalized pediatric patients at Children’s Hospital and serves as<br />
an assistant pr<strong>of</strong>essor <strong>of</strong> internal medicine and pediatrics at <strong>Ohio</strong> State.<br />
Jose Torres, D.O. (‘98), is among a growing contingent <strong>of</strong> physicians who<br />
opt for a hospital-based career.<br />
summer 2006 9
“I really enjoy taking care <strong>of</strong> acutely ill patients with complex<br />
issues, and a career as a hospitalist fits this perfectly,” he says.<br />
“While I occasionally fill in for my outpatient colleagues to<br />
keep up my outpatient skills, I prefer the acuity <strong>of</strong> the<br />
inpatient setting. The complexity <strong>of</strong> the patients I see keeps<br />
me up to date on the medical literature,” he says, adding<br />
that, “The variety <strong>of</strong> disease processes I manage certainly<br />
makes each day different and filled with new challenges.”<br />
Growth in Field Benefits All<br />
According to those who work in the field, the job <strong>of</strong> hospitalist<br />
also <strong>of</strong>fers numerous other benefits to physicians, hospitals<br />
and patients. For physicians, there are predictable schedules,<br />
average- to above-average pay, and the opportunity to avoid<br />
the hassles and expenses <strong>of</strong> starting and growing a private<br />
practice. Hospitals gain experienced inpatient care providers<br />
who can consult with other physicians and surgeons and<br />
treat patients admitted to the institution without a primary<br />
care provider. And for patients, the benefits <strong>of</strong> having physicians<br />
who are monitoring their care on site 24 hours a day are<br />
immeasurable, some say.<br />
“Patients are usually very grateful to see an attending physician<br />
who is familiar with their care, checking in on them at any<br />
hour <strong>of</strong> the day or night,” Schumacher says. “Certainly,<br />
providing 24-hour care with in-house physicians provides<br />
patients and their families extra comfort in knowing someone<br />
can be there at a moment’s notice if needed.”<br />
Industry proponents say bringing on hospitalists–who are<br />
available throughout their shifts to monitor patient progress<br />
and to adjust treatment as needed–has improved the overall<br />
quality <strong>of</strong> care hospital patients receive. And by the nature <strong>of</strong><br />
their work, hospitalists have more experience treating patients<br />
in a hospital setting than most primary care providers. The<br />
result, they contend, is better outcomes at lower costs. And<br />
their arguments have some basis; studies reveal that employing<br />
hospitalists yields a 10 percent to 25 percent decrease in the<br />
length <strong>of</strong> hospital stay, with a resulting decrease in costs, which<br />
benefits the patients, the hospitals and the insurance companies.<br />
And some physicians, such as Thomas, like how the specialty<br />
meshes with real life. There’s less paperwork and more time<br />
with her family than when she was a primary care physician.<br />
“I guess the best thing is that when I am home, I am home.<br />
I have no beeper outside the hospital and do not get phone<br />
calls,” Thomas says.<br />
Who Are Hospitalists?<br />
According to SHM, two-thirds <strong>of</strong> major teaching hospitals,<br />
one-half <strong>of</strong> other teaching hospitals and one-quarter <strong>of</strong><br />
nonteaching hospitals <strong>of</strong>fer hospitalist programs. In the<br />
industry’s earliest days, hospitalist programs were more<br />
prevalent on the East and West Coasts, but now, hospitals in<br />
almost all major metro areas and a growing number <strong>of</strong> rural<br />
communities have hospitalists on staff.<br />
Wherever they’re located, hospitalists have similar goals:<br />
helping patients recover as quickly as possible or providing<br />
quality end-<strong>of</strong>-life care to those whose conditions do not<br />
allow for recovery. Still, the exact job description varies by<br />
institution. Most hospitalists are employed directly by hospitals<br />
or medical groups that work under contract with hospitals.<br />
Some hospitalists work exclusively with adults, while others<br />
treat both adult and pediatric patients. Some work 10- to<br />
12-hour shifts several days a month, while others work fewer,<br />
24-hour shifts a month.<br />
Wayne Carlsen, D.O., F.A.C.O.I., combines inpatient care<br />
at O’Bleness Memorial Hospital in Athens with his academic<br />
responsibilities at OU-COM. Carlsen, chair <strong>of</strong> the Department<br />
<strong>of</strong> Geriatric <strong>Medicine</strong>/Gerontology and associate pr<strong>of</strong>essor<br />
<strong>of</strong> geriatrics, handles most <strong>of</strong> the hospital-based care for the<br />
five-member Geriatric <strong>Medicine</strong> Department <strong>of</strong> <strong>University</strong><br />
Medical Associates. He spends about one-half <strong>of</strong> each day<br />
caring for hospitalized patients, which works well around<br />
his academic duties at OU-COM, he says. But even this<br />
schedule has its disadvantages. “In a hospital setting, the<br />
caseload varies greatly,” Carlsen says. “I might have to see<br />
two patients in that time one day and 22 another.”<br />
” Multiple docs and multiple<br />
nurses and multiple<br />
administrations can equal<br />
disaster with change.”<br />
–Robin Thomas, D.O.<br />
Still, he says, the work arrangement has advantages, too,<br />
for physicians and patients. Because he focuses primarily on<br />
hospital care, fellow physicians in his group can concentrate<br />
on other responsibilities. And because he works at the hospital<br />
regularly, Carlsen has been able to develop good working<br />
relationships with other health-care workers at O’Bleness.<br />
“They recognize my routines and I recognize theirs,” he<br />
says. The arrangement also provides patients with a continuity<br />
<strong>of</strong> care, since he typically sees a patient throughout his or<br />
her hospital stay.<br />
Most general hospitalists, including Thomas, Torres and<br />
Schumacher, are trained as internists. But other inpatient<br />
care providers, like Don Maxwell, D.O., F.C.C.P. (‘96), who<br />
is certified in critical care medicine, have undertaken further<br />
training to provide more specialized care to hospitalized<br />
patients. Maxwell, who is considered an intensivist rather<br />
than a hospitalist, cares for the most critically ill patients at<br />
Banner Desert Medical Center in Mesa, Ariz., as medical<br />
10 www.oucom.ohio.edu
director <strong>of</strong> the hospital’s medical and surgical transition<br />
intensive care units.<br />
Maxwell says the challenge <strong>of</strong> helping the most seriously<br />
ill patients recover drew him into critical care medicine.<br />
“[Caring for the sickest <strong>of</strong> the sick] requires continual inpatient<br />
monitoring and both clinical- and procedural-related skills<br />
to positively impact this population,” he says. “But on a<br />
patient-family aspect, it is so wonderful to educate, talk<br />
with and support families through these processes in the<br />
ICU. This is why I came into medicine in the first place.”<br />
Communication Plays Key Role<br />
Despite the many benefits that hospitalists can provide, some<br />
industry critics argue that switching providers can be stressful<br />
to hospitalized patients at a time when they need stress the<br />
least. And others point out that passing patient information<br />
back and forth between providers creates potential for<br />
inadequate communication, which could ultimately have a<br />
negative impact on patient care.<br />
Torres has heard both arguments and more, but he believes<br />
the field is here to stay. “A lot <strong>of</strong> patients are surprised at first<br />
when I come in to see them,” he says. “But once I explain<br />
to them...they begin to realize that their doctor can’t always<br />
drop everything at his or her <strong>of</strong>fice to come to the hospital<br />
every time a patient is admitted. He or she has patients in<br />
the <strong>of</strong>fice, too.”<br />
Handling communication with the patient’s primary care<br />
physician does take planning, however. In some integrated<br />
health-care organizations where the primary care physician<br />
and the hospital are part <strong>of</strong> the same group, sophisticated<br />
computer systems might be available to link information<br />
from the inpatient to <strong>of</strong>fice setting. More <strong>of</strong>ten, though,<br />
hospitalists rely on more rudimentary tools for passing<br />
along patient updates.<br />
Grandview Hospital in Dayton automatically sends copies<br />
<strong>of</strong> all lab work conducted on inpatients to their primary<br />
care physicians. Hospitalists also dictate a discharge summary<br />
for each patient that describes the diagnosis, treatment and<br />
any further follow-up needed, which is faxed to the patient’s<br />
primary care provider upon discharge, Torres says. If he<br />
believes a patient needs more follow-up attention, he then<br />
calls the primary care physician personally.<br />
As a former primary care physician herself, Thomas considers<br />
this relationship especially important. “Before I came, I don’t<br />
think they contacted physicians much at all,” she says. “I<br />
was told, ‘They get the discharge summary; that should be<br />
enough.’” This person had never been in private practice.<br />
Having experienced what it’s like to be blindsided by a patient<br />
or family, I designed some fax notifications.”<br />
Because hospitalists at Blanchard Valley Regional Health<br />
Center work 10 24-hour shifts a month, patients there <strong>of</strong>ten<br />
Eric Schumacher, D.O. (‘00), stresses the importance <strong>of</strong><br />
communication between the hospitalist and a patient’s<br />
primary-care physician.<br />
see different doctors each day. That, too, sometimes<br />
proves to be a challenge to seamless care. “In our<br />
case, patients have a different physician every 24<br />
hours,” says Thomas. “I try to inform them <strong>of</strong> that<br />
issue. There are times when I may be working every<br />
other day, so that helps some, but that is where I hear<br />
the most concern.”<br />
That’s also where primary care physicians can work<br />
together with hospitalists to provide the best care for<br />
patients. “Sometimes, physicians stop for social calls,<br />
which helps both the patient and us,” Thomas says.<br />
“Sometimes, they are in a better position to discuss<br />
sensitive issues than we are.”<br />
Still, ensuring smooth transitions between inpatient<br />
care providers and primary care physicians, or even<br />
between two inpatient care physicians, has bumps.<br />
“Multiple docs and multiple nurses and multiple<br />
administrations can equal disaster with change.”<br />
As the number <strong>of</strong> hospitalist programs across the<br />
United States grows, the challenges <strong>of</strong> ensuring<br />
adequate communication will only increase. “There<br />
are fewer primary care physicians seeing their patients<br />
as inpatients than there used to be,” Schumacher says.<br />
“We try to assure our patients that we will update<br />
their PCP about their condition and management.”<br />
photo provided by Eric Shumacher, D.O.<br />
summer 2006 11
photos by Lee Ann Yahle<br />
Jose Torres, D.O. (‘00), believes the development <strong>of</strong> hospital medicine core competencies will help forge its course as a specialty.<br />
Moving Forward as a Medical Specialty<br />
Because SHM predicts that the number <strong>of</strong> hospitalist positions<br />
could reach 30,000 by 2010, the field likely will become the<br />
job <strong>of</strong> choice for many medical school graduates in coming<br />
years. But despite growing numbers nationwide, hospital<br />
medicine still is not considered a formal medical specialty by<br />
some physicians because it lacks a credentialing body and a<br />
core set <strong>of</strong> skills and knowledge. SHM is working to change<br />
that, however.<br />
In February, the association, in conjunction with more than<br />
100 hospitalists and other physicians from across the country,<br />
developed The Core Competencies in Hospital <strong>Medicine</strong>: A<br />
Framework for Curriculum Development, the nation’s first<br />
comprehensive set <strong>of</strong> guidelines to help medical schools,<br />
postgraduate training programs and continuing medical<br />
education programs develop standardized curricula for<br />
teaching hospital medicine. The goal <strong>of</strong> the document is to<br />
help assess gaps in current training programs and to set the<br />
stage for any future hospitalist certification programs, says<br />
Steve Pantilat, M.D., SHM president.<br />
Most physicians interested in hospital medicine had to forge<br />
their own educational route, in many cases selecting residency<br />
programs that have a strong basis in hospital care to help<br />
prepare them for their career choice. None <strong>of</strong> the inpatient<br />
care providers interviewed for this story has formal training<br />
as a hospitalist. In fact, few formal hospitalist training programs<br />
exist even today.<br />
But some hospitalists believe that hospitalist training programs<br />
could take <strong>of</strong>f in coming years as more primary care physicians,<br />
patients and hospitals recognize the benefits. “In the near<br />
future, I would not be surprised to see a larger number <strong>of</strong><br />
fellowships and subspecialty board certification in the field,”<br />
Schumacher says.<br />
Torres also believes the development <strong>of</strong> SHM’s core<br />
competencies will help hospital medicine forge its course<br />
as a medical specialty. “Down the road, I think you’ll be<br />
able to choose a track in internal medicine,” he says. “You’ll<br />
either be able to study to be an inpatient care provider–a<br />
hospitalist–or an outpatient care provider.”<br />
TODAY’S<br />
<strong>DO</strong><br />
Contacts<br />
Society <strong>of</strong> Hospital <strong>Medicine</strong><br />
190 Independence Mall West<br />
Philadelphia, PA 19106-1572<br />
(800) 843-3360<br />
www.hospitalmedicine.org<br />
Society <strong>of</strong> Critical Care <strong>Medicine</strong><br />
701 Lee Street, Suite 200<br />
Des Plaines, IL 60016<br />
(847) 827-6869<br />
www.sccm.org<br />
Growth <strong>of</strong> Hospitalists in<br />
North America<br />
Year<br />
Number <strong>of</strong> Hospitalists<br />
Mid 1990s 800<br />
1998 2,000<br />
2002 6,000<br />
2003 8,000<br />
2005 15,000<br />
2010 (projected) 30,000<br />
Source: Society <strong>of</strong> Hospital <strong>Medicine</strong>, 2005<br />
12 www.oucom.ohio.edu
CME<br />
S A V E T H E D A T E<br />
James D. Joye, <strong>DO</strong>, FACC, FSCAI ‘88<br />
KEYNOTE ADDRESS<br />
Primary Care <strong>of</strong> the Patient with<br />
Peripheral Vascular Disease:<br />
Current State <strong>of</strong> the Art<br />
OCTOBER 27 - 29, 2006<br />
& ALL<br />
HILTON AT EASTON<br />
CLASS<br />
COLUMBUS,<br />
REUNION<br />
OHIO<br />
WORKSHOPS INCLUDE Intensive Diabetes Treatment and Pump Training ■<br />
Advanced Cardiac Life Support Renewal Course ■ OMT<br />
OHIO UNIVERSITY<br />
COLLEGE OF OSTEOPATHIC MEDICINE<br />
& Society <strong>of</strong> Alumni and Friends<br />
Dermatology Case Studies ■<br />
PROGRAM TOPICS INCLUDE What’s New in Nuclear Cardiology ■ Radiology Case Studies ■<br />
EKG Case Studies ■ Bird Flu ■ Endovascular Cryotherapy Advances ■ Treatment <strong>of</strong> Non-alcoholic Fatty Liver<br />
Disease ■ Complex Headaches Cases ■ Restless Leg Syndrome ■ Advances in the Treatment<br />
and Understanding <strong>of</strong> Obesity ■ Community Acquired Pneumonia ■ Pulmonary Sarcoidosis Evaluation<br />
■ Osteoporosis – an Update on Diagnosis and Treatment ■ “Why would I see a Urogynecologist?” ■ Rescue<br />
<strong>Medicine</strong> ■ AND MORE<br />
EARN UP TO 21.5 CME CREDITS ■ MEET COLLEAGUES, FORMER CLASSMATES AND OU-COM FACULTY<br />
Detailed program is coming soon – watch your mail.<br />
For additional information, please contact – Sharon Zimmerman, director <strong>of</strong> alumni affairs ■ (740) 593-2176 ■ zimmerms@ohio.edu<br />
To register online – https://commerce.cashnet.com/ohioalumnicme<br />
Reserve your room at the Hilton at Easton at our special rate <strong>of</strong> $142/night. Call (614) 414-5000 or go online at Hiltoncolumbus.com and enter code OHU.
The Obstetrics Dilemma<br />
by Richard Heck<br />
Today malpractice<br />
insurance and<br />
litigation are<br />
changing the<br />
face <strong>of</strong> obstetrics.<br />
The one big<br />
casualty is<br />
choice —for<br />
patients and<br />
doctors<br />
alike.<br />
illustration by Danette Pratt
WWhen Mary Kruszewski, D.O. (‘88), began her practice in 1993, she paid $6,000 for insurance. This<br />
year, her total malpractice insurance premiums exceed $107,000. Money, however, has not been<br />
the only cost.<br />
Skyrocketing costs <strong>of</strong> medical malpractice insurance spell ominous warnings for the future <strong>of</strong><br />
health care and physicians’ practices. Kruszewski is feeling it firsthand like so many<br />
physicians, including other graduates <strong>of</strong> <strong>Ohio</strong> <strong>University</strong>’s <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong><br />
<strong>Medicine</strong>, who are speaking up.<br />
Recent studies, surveys, papers and reports reveal in ever-increasing frequency how<br />
the issue is impacting decisions physicians make, not only about how they treat patients<br />
but where and even if they practice. The field <strong>of</strong> obstetrics remains especially hard hit.<br />
An <strong>Ohio</strong> Department <strong>of</strong> Insurance report issued in February 2005 from a survey <strong>of</strong><br />
<strong>Ohio</strong> physicians concluded that the rising cost <strong>of</strong> malpractice insurance has significantly<br />
impacted physician behavior and their future plans in the state. The survey included<br />
answers from 1,359 physicians from across <strong>Ohio</strong>, 10 percent <strong>of</strong> whom were osteopathic<br />
physicians.<br />
Nearly four out <strong>of</strong> 10 respondents surveyed say they have retired or plan to retire by<br />
2008 because <strong>of</strong> rising insurance expenses. “This finding is all the more sobering since<br />
just 9 percent <strong>of</strong> the respondents were over the age <strong>of</strong> 64,” the report says.<br />
Among osteopathic physicians, 11 percent say they planned to retire during 2005, and<br />
15 percent say they planned to seek employment outside patient care.<br />
Kruszewski, who practices in Du Bois, Pa.–a rural town in a state considered in crisis because <strong>of</strong><br />
high premiums–has been affiliated with several insurance companies and named a defendant in<br />
lawsuits. “I’ve gone to two trials, both <strong>of</strong> which turned out in my favor,” she says. But her hefty<br />
insurance premiums have affected how she practices, including ordering more tests, but as <strong>of</strong><br />
yet, she has not considered moving her practice or leaving patient care. “I’m not ready to<br />
give it up because I like what I do,” she says.<br />
A paper issued by the <strong>University</strong> <strong>of</strong> Michigan Health System warned that increasing<br />
premiums are forcing many physicians to rethink how they practice, from reducing<br />
staff to quitting patient care altogether.<br />
“The hard cost <strong>of</strong> malpractice premiums is beginning to lead providers to drop or reduce<br />
obstetrical services,” says Scott B. Ransom, D.O., senior author <strong>of</strong> a research paper published<br />
in the June 2005 issue <strong>of</strong> the journal Obstetrics & Gynecology. “Our study shows that there<br />
is legitimate reason for concern about patients’ access to obstetric care and prenatal care in<br />
the future,” he warned.<br />
“It is frustrating,” says Michelle Wright, D.O. (‘95), who moved her obstetrics practice<br />
from Athens in rural <strong>Ohio</strong> to Sharon, Pa., for a variety <strong>of</strong> reasons, not the<br />
least <strong>of</strong> which was yearly double-digit rate increases for her malpractice<br />
insurance. Before relocating from Athens, Wright saw her premiums<br />
jump from $18,000 to $65,000 in just two years.<br />
“I can’t work without it; it’s a necessary evil.”<br />
The primary breadwinner in her household, Wright took a job at a federally funded clinic in<br />
western Pennsylvania mainly for economic reasons. Although Pennsylvania ranks close to<br />
<strong>Ohio</strong> for some <strong>of</strong> the highest medical malpractice insurance rates in the country, her clinic is<br />
covered under the federal court and tort system, keeping Wright’s insurance rates–and<br />
any possible malpractice claims–somewhat moderated. With family ties and roots in western<br />
Pennsylvania, the pr<strong>of</strong>essional change made more sense.<br />
Did malpractice insurance rates drive her out? Certainly in part. “Leaving Athens<br />
was difficult, but I had to find a stable climate and not worry about a paycheck at the end<br />
<strong>of</strong> the day,” Wright says.<br />
summer 2006 15
Wright is not alone. In 2004, 96 percent <strong>of</strong> the <strong>Ohio</strong><br />
Department <strong>of</strong> Insurance survey respondents said his or her<br />
malpractice rates jumped by an average <strong>of</strong> 39 percent over<br />
2003. More than a quarter were paying more than $50,000<br />
a year, and one in five physicians was paying 20 percent <strong>of</strong><br />
gross annual income for insurance. Obstetrics and gynecology<br />
physicians responding to the survey reported paying more<br />
than 30 percent <strong>of</strong> their annual income to malpractice insurers.<br />
Wright says that, financially, the high premiums hit<br />
younger physicians harder, considering many are already in<br />
debt from their education, practice start-up and young families.<br />
“It can be a balancing act,” she says.<br />
The <strong>Ohio</strong> insurance survey warned that malpractice insurance<br />
premium increases are impacting <strong>Ohio</strong> doctors in a<br />
variety <strong>of</strong> other areas, including influencing where physicians<br />
see patients, what type <strong>of</strong> services they <strong>of</strong>fer, how they provide<br />
treatment and what business practices are forced upon<br />
them, such as reducing staff.<br />
Alumni <strong>of</strong> OU-COM can attest to that.<br />
“ I had to find a stable climate and<br />
not worry about a paycheck at<br />
the end <strong>of</strong> the day.”<br />
Michelle Wright, D.O.<br />
The malpractice insurance crisis was a factor in George<br />
Abate’s decision to locate his practice in Indianapolis. His<br />
attendings warned him <strong>of</strong> how expensive it would be to<br />
practice in Cuyahoga County, according to Abate, D.O.<br />
(‘02), who at the time was completing his residency at<br />
northeastern <strong>Ohio</strong>’s Metrohealth System. The issue also<br />
impacts how he treats patients and the costs associated with<br />
their care.<br />
“As a resident we’re already taught to be defensive and more<br />
aware,” Abate says. “You have to order more tests than may<br />
be warranted, but (if you don’t, you) worry about missing a<br />
breast cancer or something that may be indicated from an<br />
MRI, which then adds more costs and more tests. That is<br />
going to affect patient care.”<br />
Abate also feels that the high malpractice insurance rates<br />
reflect an even greater problem for medical care across the<br />
board. “The rising cost <strong>of</strong> health care overall has the potential<br />
to bankrupt the country,” he warned.<br />
A nontraditional student while at OU-COM, Abate says his<br />
perspective on the issue may be somewhat different than<br />
younger colleagues. Along with other physicians, lawmakers,<br />
educators and experts, Abate blames growing malpractice<br />
lawsuits and astronomical plaintiff monetary awards.<br />
“There need to be caps on claims,” he says. “If there is<br />
harm to a patient, then they should be appropriately<br />
reimbursed...Part <strong>of</strong> the problem comes down to the size<br />
<strong>of</strong> the awards.”<br />
That is one perspective, but <strong>Ohio</strong>’s cap for awards in<br />
malpractice lawsuits, enacted nearly two years ago, has yet<br />
to show any significant difference in premiums, several<br />
physicians and insurance <strong>of</strong>ficials says. Legal experts report<br />
that insurance companies tend to wait before stabilizing<br />
premiums to see if such legislation will be overturned by<br />
the courts.<br />
Patrick Muffley, D.O. (‘97), who returned to his native<br />
Southeastern <strong>Ohio</strong> to practice at Holzer Medical System <strong>of</strong><br />
Gallipolis and Jackson, agreed that <strong>Ohio</strong>’s cap has yet to<br />
stem the problem, and no one knows how the courts will<br />
respond. “Look at Wisconsin, which enacted a cap, then<br />
was challenged and repealed,” he says. Muffley says some<br />
changes in current law, such as requiring medical experts to<br />
testify harm has been done to a patient before a lawsuit is<br />
even filed, might bring more responsibility to the system.<br />
Muffley, who relocated from Maine, saw his insurance<br />
premiums eased by participating in a large group practice,<br />
which is partly self-insured and helped reduce costs, he<br />
says.<br />
“It is affecting the way we practice medicine,” he says <strong>of</strong><br />
the more serious consequences litigation spawns. “When<br />
you look across the country and see how the c-section rate<br />
has jumped 30 percent, I think that is a response to avoid<br />
possible future litigation. Muffley says physicians hasten to<br />
order c-sections earlier than they might like because there<br />
are too many malpractice cases in which plaintiffs claim a<br />
c-section was done too late.<br />
Janet Zurovchak, D.O. (‘88), agrees. She practices in Logan<br />
County in western <strong>Ohio</strong>, where she’s delivered many babies<br />
in a Bellefontaine, <strong>Ohio</strong>, hospital. “I don’t wait as long before<br />
doing a c-section if there is anything that might be wrong<br />
because this is a smaller, community hospital,” she says. Her<br />
hospital doesn’t have a full-time anesthesiologist, and it can<br />
take 30 minutes or longer to summon one or transfer a<br />
patient to a larger metropolitan hospital in Springfield or<br />
Sydney with better facilities, she says.<br />
Higher premiums also changed Zurovchak’s practice in<br />
another way. Her three-physician practice was forced last<br />
16 www.oucom.ohio.edu
Anita Showalter, D.O., (‘93) whose practice is largely among<br />
Amish clients, discovered that if she moved her practice just 10<br />
miles to the south in neighboring Holmes County–closer to<br />
the majority <strong>of</strong> her patients–she could save $75,000 a year on<br />
her liability insurance.<br />
year to cut back, replacing a physician with a midwife.<br />
“The workload is naturally more, but we just couldn’t<br />
afford to pay more,” she says. If insurance premiums<br />
continue to increase, which she says has been occurring<br />
regularly for the past five years, she may even consider<br />
quitting obstetrics and just providing gynecology services.<br />
Physicians also face a complex task <strong>of</strong> sorting through<br />
insurance premiums based on specialty and location,<br />
regulations, managed care, hospital privileges and a variety<br />
<strong>of</strong> other issues. <strong>Ohio</strong> is considered a high-risk state for<br />
malpractice insurance, but insurance companies charge even<br />
higher rates in the southeastern and northeastern quadrants<br />
<strong>of</strong> the state. Often, managed care and insurance companies<br />
contribute to the problem.<br />
Anita Showalter, D.O. (‘93), whose practice is largely<br />
among Amish clients, noted her premiums only increased<br />
two percent last year. “Still, 2 percent is still a lot if you pay<br />
$150,000 a year,” she says.<br />
Options can be few, though. When Showalter considered<br />
moving her practice a county away after her insurance<br />
premiums jumped two and one-half times in one year, her<br />
insurance carrier was the obstacle. “For some reason, my<br />
insurance company decided to include my county (Wayne),<br />
which is in a rural area with an Amish cliental who tend not<br />
to sue, with northeastern <strong>Ohio</strong>,” she says, adding that she’s<br />
never been the subject <strong>of</strong> a lawsuit. But to her surprise,<br />
Showalter discovered that if she moved her practice<br />
just 10 miles to the south in neighboring Holmes<br />
County–closer to the majority <strong>of</strong> her patients,<br />
actually–she could save $75,000 a year on her liability<br />
insurance. When she questioned her insurance carrier<br />
about the logic <strong>of</strong> its reasoning, she received no<br />
substantial answer. In the end she stayed put and<br />
paid the price, so she wouldn’t have to switch her<br />
hospital affiliation.<br />
“I feel like physicians have sold the farm,” says<br />
Showalter, who is passionate about the issue. Defensive<br />
medicine gets in the way <strong>of</strong> good medicine. “If you<br />
have to look at every patient as a potential adversary<br />
in a lawsuit, you lose the trust that is needed between<br />
a physician and patient.”<br />
Showalter believes physicians and hospitals need to<br />
come up with solutions. She says she’d consider the<br />
option <strong>of</strong> forgoing liability insurance and creating a<br />
national fund to assist patients who encounter legitimate<br />
medical problems needing catastrophic care.<br />
Already, the idea <strong>of</strong> “going bare” is commonplace in<br />
Florida, so far with little downside, she says.<br />
“ The rising cost <strong>of</strong> health care<br />
overall has the potential to<br />
bankrupt the country.”<br />
George Abate, D.O.<br />
“We would be saying that we need physicians and<br />
hospitals and to give them the room to be human,”<br />
she says.<br />
“We need a national outrage,” Showalter says. “The<br />
people not being treated fairly are the physicians and<br />
the hospitals. Can we really afford to continue?”<br />
If you ask Zurovchak, she’ll say it’s not just physicians.<br />
“I don’t think the public realizes how much this affects<br />
them. They read about it and hear about it talked and<br />
tossed about in the news media, but until we say we<br />
have to make changes in our practice, the average person<br />
doesn’t realize that means their doctor,” she says.<br />
TODAY’S<br />
<strong>DO</strong><br />
summer 2006 17
18 www.oucom.ohio.edu<br />
.<br />
..
.<br />
........<br />
From Diapers to<br />
Driver’s Licenses<br />
by Melissa Rake Calhoun<br />
More and more graduates are choosing<br />
pediatrics. What’s accelerating the<br />
march to this specialty?<br />
Hint: It’s not the money.<br />
Mazen Abbas, D.O. (‘03), first felt the pull toward pediatric practice when he began treating a little<br />
girl with complicated pnemonia, and she surprised him. When she recovered beautifully, Abbas couldn’t<br />
get over the feeling he carried with him in the days after her release from Dewitt Army Community<br />
Hospital in Fort Belvoir, Va.<br />
“We took a three-year-old who looked absolutely miserable and scared, and made her happy and playful<br />
in one intervention,” Abbas says. “I remember specifically that’s the moment I went home and thought,<br />
‘I can’t wait to go to work tomorrow morning.’”<br />
That was more than two years ago. Now, Abbas is a pediatric resident and Army captain at Tripler<br />
Army Medical Center in Honolulu, Hawaii. He says he went into pediatrics because it provides an<br />
incredibly satisfying level <strong>of</strong> reward.<br />
Abbas’ story is not uncommon. Across the nation, an increasing number <strong>of</strong> medical graduates are choosing<br />
pediatrics as their practice focus. What’s more, in Abbas’ 2003 graduating class, 10 percent <strong>of</strong> graduates<br />
chose pediatrics–the highest percentage <strong>of</strong> a single class in OU-COM’s history.<br />
The number <strong>of</strong> general pediatricians nationally has grown from just over 22,000 in 1975 to nearly 70,000<br />
in 2003, according to the most recent statistics provided by the American Academy <strong>of</strong> Pediatrics. Much<br />
<strong>of</strong> the growth has taken place since 1990, representing a 67 percent increase, and is associated with the<br />
crest in primary care popularity beginning in the mid-1990s.<br />
A more marked shift has been taking place in the past decade among osteopathic graduates. Since<br />
1995, the number <strong>of</strong> osteopathic residents training in pediatrics has increased by 99 percent,<br />
summer 2006 19
Karen Montgomery-Reagan, D.O., and Celeste<br />
Wallace, D.O. (‘02), were drawn to pediatrics for<br />
similar but separate reasons.<br />
20 www.oucom.ohio.edu
compared to a 15 percent growth in the allopathic arena,<br />
according to a 2005 study published in The Journal <strong>of</strong> the<br />
American Medical Association.<br />
This trend is mirrored at OU-COM, although on a smaller<br />
scale. The number <strong>of</strong> graduates choosing pediatrics hasn’t<br />
exactly exploded but has been a slow climb from one or two<br />
graduates a year in the 1980s to anywhere from four to 10<br />
in the past decade. Current statistics show that 60, or 4<br />
percent, <strong>of</strong> OU-COM’s 1,653 practicing physicians<br />
are pediatricians. Double that for the percentage<br />
<strong>of</strong> OU-COM graduates currently in pediatrics<br />
residency programs.<br />
“We’ve seen a larger number <strong>of</strong> very bright<br />
students seeking pediatrics as a career choice,<br />
and I think America’s kids are going to be better<br />
<strong>of</strong>f for it,” says Michael Anderson, M.D., chair<br />
<strong>of</strong> the American Academy <strong>of</strong> Pediatrics’ Committee<br />
on Pediatric Workforce. “It’s a very exciting<br />
time to be in pediatrics because we’re making<br />
progress on disease processes that we didn’t<br />
have an impact on 10 years ago.”<br />
The reasons behind this trend are multifaceted.<br />
It’s not as simple as presuming more medical<br />
school graduates these days love working with<br />
children. Career satisfaction, job flexibility and<br />
changes in demographics are part <strong>of</strong> the equation.<br />
Reward, Reward, Reward<br />
When Carl Backes, D.O., talks about his 30<br />
years in pediatrics, his enthusiasm is clear.<br />
Backes can explain his draw to the field in a<br />
simple statement.<br />
“I don’t know <strong>of</strong> another primary care doctor<br />
who takes someone from birth through high<br />
school–through jaundice, immunizations, hospitalizations<br />
for illness, growing up and having school problems, the<br />
changes <strong>of</strong> puberty during adolescence and, finally, getting<br />
them ready for college,” he says. “It’s like being a mom<br />
and dad.”<br />
Many studies indicate high career satisfaction levels for<br />
pediatricians, and reward is a big reason why pediatricians love<br />
what they do. Backes, a former OU-COM regional dean<br />
and currently a CORE clinical pr<strong>of</strong>essor <strong>of</strong> pediatrics, is<br />
codirector <strong>of</strong> a dually accredited pediatric residency program<br />
at Doctors Hospital, along with a codirector at Children’s<br />
Hospital, both in Columbus, <strong>Ohio</strong>. In his role, Backes<br />
works with residents who have come into the field via different<br />
paths, some because it’s what they’ve always wanted to do<br />
and others who may have had an experience that inspired<br />
them to pursue a pediatric focus.<br />
According to Abbas, children typically bounce back. They<br />
want to get better, he explains, and parents usually listen to<br />
doctors’ recommendations because they want to take good care<br />
<strong>of</strong> their children. “It’s a ... positive experience, and you<br />
know there’s probably going to be a good outcome,”<br />
Abbas says.<br />
OU-COM Associate Pr<strong>of</strong>essor <strong>of</strong> Pediatrics Karen<br />
Montgomery-Reagan, D.O., says she was drawn to<br />
pediatrics for the same reasons and, like Abbas, has<br />
many positive anecdotes to share, such as the baby she<br />
treated in an emergency situation who’s now six years<br />
Number <strong>of</strong> General Pediatricians<br />
By Year (x1000)<br />
80<br />
60<br />
40<br />
20<br />
0<br />
.<br />
.<br />
.<br />
.<br />
.<br />
.<br />
.<br />
.<br />
.<br />
number <strong>of</strong> general pediatricians by year (x1000)<br />
1975<br />
2003<br />
old and still her patient. “I’ve got all kinds <strong>of</strong> stories<br />
that make me so warm inside because maybe God put<br />
me in the right place at the right time for these kids,”<br />
says Montgomery-Reagan, who’s been a practicing<br />
pediatrician since 1995.<br />
This aspect <strong>of</strong> pediatrics shouldn’t be downplayed as it<br />
brings more medical students into this primary care field<br />
every year. Katie Pestak, a second-year OU-COM<br />
student and president <strong>of</strong> the Pediatrics Club, seems<br />
as knowledgeable about the rewards <strong>of</strong> the pr<strong>of</strong>ession<br />
as some <strong>of</strong> her mentors. Through the Pediatrics<br />
Club, Pestak exhibits her passion by working with<br />
Montgomery-Reagan, club adviser, to open up<br />
physcian-shadowing and pediatric service opportunities<br />
for students.<br />
“Kids heal quickly, and they have such a sense about<br />
them when they are healing,” Pestak says. “If I heal a<br />
child, they have possibly 80 more years to live. You<br />
feel like you’re really making a difference.”<br />
informational graphic by Jeff Brown<br />
summer 2006 21
A Family-Friendly Specialty<br />
Lori Gordley, D.O (‘03), loves children, but that’s not the<br />
only reason she chose pediatrics. The flexibility it provides<br />
cemented her decision.<br />
“Lifestyle went into my choice, and pediatrics is good for<br />
physicians who have families. I don’t have children yet, but<br />
the ability to manage my schedule is important to me,” said<br />
Gordley, a pediatrics resident at Cincinnati Children’s Hospital.<br />
More graduates like Gordley are looking to balance family and<br />
career, and they’re realizing that pediatrics <strong>of</strong>fers flexibility.<br />
The average full-time pediatrician works about 50 hours a<br />
week, which is considerably less than some medical specialties.<br />
In addition, more pediatricians work part time than physicians<br />
in any other specialty. The percentage <strong>of</strong> pediatricians reporting<br />
they work part time has increased from nearly 11 percent in<br />
1993 to 20 percent in 2004, reports the American Academy<br />
<strong>of</strong> Pediatrics, and 26 percent <strong>of</strong> pediatricians versus 14<br />
percent <strong>of</strong> all physicians have worked part time at some<br />
point in their careers.<br />
“You’re going to work hard, but you’re not going to be<br />
beaten into the ground,” says Anderson <strong>of</strong> the American<br />
Academy <strong>of</strong> Pediatrics. “You make an impact on families’<br />
lives, but you have time for your own family.”<br />
This flexibility is appealing to women, who are entering<br />
the field in unprecedented numbers. Women made up<br />
about 20 percent <strong>of</strong> the pediatric workforce in 1970 and<br />
about 40 percent in 1990, according to the American<br />
Medical Association. Today, they represent more than 50<br />
percent <strong>of</strong> the workforce, a historic first for any specialty<br />
in the United States.<br />
Pediatricians haven’t always had the ability to manage their<br />
schedules, however. The pediatrician’s role was very different<br />
when Backes was practicing in the years following his<br />
graduation from the Kirksville <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong><br />
<strong>Medicine</strong> in 1972. He recalls working long hours and running<br />
from hospital to hospital to treat children.“There weren’t<br />
many pediatricians then, so we were always on call,” he says.<br />
“It was a very challenging time.”<br />
Many pediatricians say the reward and flexibility their field<br />
provides makes up for the fact that pediatrics is one <strong>of</strong> the<br />
lowest-paying medical disciplines. The average pediatrician<br />
earns just more than $143,000 compared to $230,000 and<br />
up for obstetrics/gynecology and general surgery. Even family<br />
medicine practitioners, at nearly $150,000, make more.<br />
Considering the rising cost <strong>of</strong> malpractice insurance and<br />
heavy student loan debt many graduates are saddled with in<br />
their early years, it stands to reason that some graduates<br />
may be drawn to more lucrative specialties. Others, however,<br />
see the long-term promise <strong>of</strong> job satisfaction.<br />
“I really like what I’m doing, and I’m going to enjoy getting<br />
up and going to work every day,” Gordley says. “Knowing<br />
that, I don’t mind not making as much money. You have to<br />
decide what’s most important.”<br />
For Abbas, it’s not about the money, either. “I thought about<br />
my kids and that I wanted to choose a specialty where I could<br />
be there for them. It’s more important for me to see my<br />
family rather than having more money,” says Abbas, who<br />
has two children, Jad, 6, and Carabelle, 3.<br />
Preventive <strong>Medicine</strong><br />
In pediatrics, education extends beyond the patient; a<br />
pediatrics practice is a perfect platform for reaching both the<br />
child and parent–children in terms <strong>of</strong> educating them about<br />
staying healthy and safe, and parents in terms <strong>of</strong> teaching<br />
them how to reinforce this message to their children. The<br />
multigenerational reach has made pediatrics especially<br />
attractive to some graduates.<br />
“Children are at risk because they’re dependent entirely on<br />
the parent,” says Thomas Clark, D.O., chair <strong>of</strong> OU-COM’s<br />
Department <strong>of</strong> Pediatrics. “It’s important for us to be an<br />
advocate for the child while educating parents about ways to<br />
keep their children healthy.”<br />
For example, Clark continually reinforces to his students the<br />
importance <strong>of</strong> talking to parents about childhood immunizations.<br />
“Younger pediatricians aren’t as aggressive about immunizations<br />
because they didn’t see all these kids die from diseases,” he<br />
says. “We need to be more aggressive about advocating for<br />
children to get immunizations.”<br />
Abbas, who earned a master’s degree in public health, talks<br />
to parents about everything from preventing sickness and<br />
injury to issues involving discipline. To this end, Abbas plans<br />
to develop a parenting class that residents near Tripler Army<br />
Medical Center can attend. This type <strong>of</strong> class is especially<br />
relevant on a military base, where many parents are young<br />
and <strong>of</strong>ten far from family.<br />
“Good parenting skills can make a big difference in a child’s<br />
health and psychological development, and we need to make<br />
sure we’re helping parents on all levels,” Abbas says.<br />
Celeste Wallace, D.O. (‘02), who is an assistant pr<strong>of</strong>essor<br />
in OU-COM’s Pediatrics Department and practices with<br />
Montgomery-Reagan, also was drawn to primary pediatrics<br />
for its preventive nature. Whether it’s hygiene or diet and<br />
exercise, Wallace has found that many children will not head<br />
down a healthy path if they don’t learn the basics early.<br />
“Once they’re adults, it’s too hard to reprogram them. It’s<br />
easier to start with young minds,” she says.<br />
The drive to make an impact fits right in with Wallace’s<br />
other reason for choosing pediatrics: “I love children, and<br />
you have to do what you love.”<br />
More Doctors in the Making<br />
Although Pestak, a native <strong>of</strong> Cleveland, has two more years<br />
<strong>of</strong> medical school and three years in a residency, she already<br />
knows she’d like to practice pediatrics in <strong>Ohio</strong> and be a part<br />
<strong>of</strong> this burgeoning pr<strong>of</strong>ession.<br />
22 www.oucom.ohio.edu
“I think pediatrics is growing because people are more interested<br />
in continuation <strong>of</strong> care,” she says. “You develop long-term<br />
relationships, and I think people are wanting to connect with<br />
their doctors.”<br />
More medical students are realizing the benefits <strong>of</strong> a career in<br />
pediatrics because pr<strong>of</strong>essors are creating opportunities for<br />
students to experience pediatric practice, such as through<br />
OU-COM’s Pediatrics Club, and through medical apprenticeship<br />
and mentoring programs that the American Academy <strong>of</strong><br />
Pediatrics and other organizations <strong>of</strong>fer.<br />
The American <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> Pediatricians reaches out to<br />
medical students through chapters. Students additionally are<br />
invited to conferences and to serve on the organization’s<br />
Board <strong>of</strong> Trustees. Lee J. Herskowitz, D.O., president <strong>of</strong> the<br />
“ I really like what I’m doing, and I’m<br />
going to enjoy getting up and going<br />
to work every day. Knowing that, I don’t<br />
mind not making as much money. You<br />
have to decide what’s most important.”<br />
organization, believes its important to tap into students’ interests,<br />
perceptions and concerns about the field.<br />
“We, as a <strong>College</strong>, are doing as much as we can to try to encourage<br />
students to look at pediatrics,” Herskowitz says. “We involve<br />
them in organization activities such as helping us improve the<br />
academic curriculum in the area <strong>of</strong> pediatrics. Their viewpoints<br />
are important.”<br />
Although there’s been some debate about whether the general<br />
pediatrician workforce will expand more rapidly into the next<br />
decade than the child population, Anderson says, there will<br />
always be a need for pediatricians, especially in rural communities.<br />
“Getting pediatricians to practice in underserved areas will<br />
continue to be a concern, and that’s why it’s important for<br />
us to try to make an impact on students early on about the need<br />
and <strong>of</strong>fer them incentives to practice in rural areas,” he says.<br />
For the pediatric field to continue to flourish, however, it’s<br />
important that medical school students keep experiencing the<br />
“aha” moments that lead them to a satisfying career in the field.<br />
“Treating children is a very visceral sort <strong>of</strong> thing,” Anderson<br />
says. “We have to show what fun we have and the impact we<br />
have on families.”<br />
TODAY’S<br />
<strong>DO</strong><br />
–Lori Gordley, D.O.<br />
summer 2005 23
Celebrate<br />
1981<br />
Family Health ® airs on 18 radio stations in <strong>Ohio</strong> and West<br />
Virginia. Fred J. Jenson, D.O. is the first host. Jack Brose,<br />
D.O. serves as the interim on-air voice for Family Health ®<br />
radio in 1982.<br />
Fred J. Jenson, D.O.<br />
Sound Medical Advice<br />
Family Health ® , a drive time audio<br />
staple, turns 25 this year. These twoand-a-half<br />
minute radio spots enlighten<br />
12 million listeners daily, across the<br />
nation and around the world.<br />
The format is familiar to listeners: A theme song and<br />
announcer cue the audience that Harold C. Thompson,<br />
an osteopathic family physician, will provide health<br />
information in layman's terms about a medical issue<br />
that recently surfaced in the news or in answer to a<br />
question frequently asked by patients. The program<br />
ends neatly with suggestions that listeners can <strong>of</strong>ten<br />
readily act upon.<br />
Family Health ® was the product <strong>of</strong> a brainstorming<br />
session between Ed McDonald, a radio producer at<br />
the <strong>Ohio</strong> <strong>University</strong> Telecommunications Center (now<br />
called the Center for Public Media); Fred J. Jensen,<br />
D.O., <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong><br />
(OU-COM) pr<strong>of</strong>essor <strong>of</strong> pathology; and Carl J. Denbow,<br />
Ph.D., OU-COM director <strong>of</strong> communication.<br />
In 1988, Adam Hochberg (right),<br />
today a National Public Radio<br />
correspondent, got his start as<br />
a scriptwriter working with<br />
Frank Myers, D.O., Producer<br />
Don Bilski (seated) and Project<br />
Director Carl Denbow, Ph.D.<br />
Today, 6,500 shows later,<br />
Family Health ® is regarded<br />
by the pr<strong>of</strong>ession as one<br />
<strong>of</strong> its major vehicles to “make<br />
D.O. a household word,”<br />
according to Guy Beaumont,<br />
executive director <strong>of</strong> the<br />
American <strong>College</strong> <strong>of</strong><br />
<strong>Osteopathic</strong> Surgeons. Over<br />
the years, primary support<br />
for Family Health ® has come<br />
from the American <strong>Osteopathic</strong><br />
Association, with additional<br />
critical annual gifts from the<br />
American <strong>College</strong> <strong>of</strong><br />
<strong>Osteopathic</strong> Surgeons and the<br />
American <strong>College</strong> <strong>of</strong><br />
<strong>Osteopathic</strong> Family Physicians.<br />
Frank W. Myers, D.O.<br />
Harold C. Thompson, D.O.<br />
1982<br />
Jack Brose, D.O., hosts Family Health ® .<br />
1983<br />
Frank W. Myers, D.O., then OU-COM dean, is selected as the<br />
new permanent host. Family Health ® airs on 142 radio stations.<br />
1990<br />
The Family Health theme song was written and performed<br />
by Mark Phillips, pr<strong>of</strong>essor <strong>of</strong> music at <strong>Ohio</strong> <strong>University</strong>.<br />
Affiliate stations number their highest, at 330.<br />
1994<br />
Audio files <strong>of</strong> Family Health ® are available via download <strong>of</strong><br />
from its Web site, www.fhradio.org.<br />
1998<br />
Harold C. Thompson III, D.O., assistant pr<strong>of</strong>essor <strong>of</strong><br />
emergency medicine in the Department <strong>of</strong> Family <strong>Medicine</strong>,<br />
succeeds Dr. Myers upon his retirement.<br />
2006<br />
Family Health ® reaches about 12 million listeners each day<br />
on an international network that includes nearly 300<br />
domestic stations, a few foreign stations, and the U.S.<br />
Armed Forces Radio Network.<br />
Family Health ® Top 10 Listener<br />
Choice Shows <strong>of</strong> 2006<br />
• The Family Health ® First Aid Fact Finder<br />
• Sleeping pills<br />
• Adding protein to your diet<br />
• Preventing osteoporosis<br />
• Chronic fatigue syndrome<br />
• Restless leg syndrome<br />
• Sense <strong>of</strong> smell’s influence on health<br />
• Lifesaving showering routine<br />
• Vitamin A and bone health<br />
• Getting more sleep can help lose weight<br />
24 www.oucom.ohio.edu
Your <strong>Ohio</strong> <strong>University</strong> Alumni Association connects you . . .<br />
The <strong>Ohio</strong> <strong>University</strong> Alumni Association<br />
<br />
partnerships with nationally prominent<br />
vendors — simply making life better!<br />
Need insurance ...<br />
Travel Auto<br />
Home Renter<br />
Health (short term/long term)<br />
Show your <strong>Ohio</strong> pride ...<br />
<br />
Apparel<br />
License plate<br />
Consolidate your school loans ...<br />
Student loan<br />
consolidation program<br />
Travel the world ...<br />
Alumni tours<br />
Get connected ...<br />
Chapter networks<br />
Society networks<br />
The [Gateway]<br />
Online directory<br />
Dr. Shubrook proudly wears the Official Ring <strong>of</strong> <strong>Ohio</strong> <strong>University</strong>.<br />
Contact the alumni association at<br />
740-593-4300<br />
alumni@ohio.edu or visit<br />
www.ohio.edu/alumni/<br />
for more information.<br />
Jay Shubrook D.O. (’96)<br />
Involved. Ambassador.<br />
Role model. Bobcat.<br />
The Official Ring <strong>of</strong> <strong>Ohio</strong><br />
<strong>University</strong> is exclusively<br />
designed by Balfour
Research News<br />
Survey Shows Diabetes Rates Higher<br />
in <strong>Ohio</strong> Appalachian Counties<br />
An epidemic <strong>of</strong> diabetes mellitus, or type 2 diabetes, is occurring in the United States and in other parts <strong>of</strong><br />
the industrialized world. According to a recent survey conducted by the Appalachian Rural Health Institute<br />
(ARHI), people who live in Southeast <strong>Ohio</strong> also appear to have a higher prevalence <strong>of</strong> diabetes than other<br />
regions <strong>of</strong> the state and the nation as a whole–rates nearly equivalent to ethnic populations that have a<br />
known higher incidence <strong>of</strong> the disease–according to ARHI researchers.<br />
In a telephone survey conducted in January 2006, more than 2,220 adult residents <strong>of</strong> seven Southeast <strong>Ohio</strong><br />
counties were asked, “Have you ever been told by a doctor or other health-care pr<strong>of</strong>essional that you have<br />
diabetes?” and 11.3 percent answered “yes.”<br />
To compare, the Center for Disease Control's Behavioral Risk Factor Surveillance<br />
System survey, the world's largest telephone survey, reported rates <strong>of</strong> diabetes<br />
at 7.3 percent for all <strong>of</strong> <strong>Ohio</strong> and 7.7 percent for the nation when respondents<br />
were asked the same question.<br />
Please don't hang up!<br />
Help us gather information that will be used<br />
to develop diabetes services in your county.<br />
Do you have diabetes or heart disease or do you<br />
know someone who does? What kinds <strong>of</strong> clinic and<br />
education services would help you and others in your<br />
county? The Appalachian Rural Health Institute at<br />
<strong>Ohio</strong> <strong>University</strong> is running an anonymous telephone<br />
survey this week. The goal <strong>of</strong> the survey is to learn<br />
about chronic conditions such as diabetes and heart<br />
disease affecting people in Southeast <strong>Ohio</strong>. The<br />
interviewers will be gathering information that will<br />
be used to develop diabetes services in your county.<br />
You can help by taking a few moments to answer<br />
the questions.<br />
The Appalachian Rural Health Institute is a health<br />
services and research institute at <strong>Ohio</strong> <strong>University</strong>.<br />
The Institute was founded with a goal <strong>of</strong> improving<br />
the health and quality <strong>of</strong> life <strong>of</strong> underserved rural<br />
populations in Southeastern <strong>Ohio</strong>.<br />
arhi<br />
The Appalachian Rural Health Institute<br />
appalachian rural health institute<br />
“The results <strong>of</strong> this survey indicate that persons in Appalachian <strong>Ohio</strong> have<br />
prevalence rates for diabetes equivalent to those reported for high risk<br />
ethnic groups in the country,” says Frank Schwartz, M.D., director <strong>of</strong> ARHI’s<br />
Diabetes/Endocrine Center, OU-COM associate pr<strong>of</strong>essor <strong>of</strong> endocrinology<br />
and principal investigator for the study.<br />
“Within Appalachia there are clusters <strong>of</strong> counties that are at higher<br />
risk, and they tend to be more devastated economically and have lower<br />
group socioeconomic status,” says Schwartz. Vinton County has a 12.8<br />
percent prevalence rate, for example, which approaches rates reported<br />
in African Americans (13.3 percent) and American Indians (12.8 percent).<br />
Schwarz explains that many <strong>of</strong> <strong>Ohio</strong>’s 29 Appalachian counties have a<br />
disproportionately high number <strong>of</strong> people who live at or near poverty<br />
level, have lower education levels, suffer from obesity, and lead unhealthy<br />
life-styles. “Our study <strong>of</strong> seven counties suggests that they may also<br />
have higher prevalence rates <strong>of</strong> diabetes.”<br />
According to the <strong>Ohio</strong> Department <strong>of</strong> Health, approximately 110,000 residents<br />
in <strong>Ohio</strong>’s Appalachian counties have been diagnosed with diabetes, and an additional 30,000<br />
remain undiagnosed, which Schwarz believes could be “a gross underestimate.”<br />
The study is part <strong>of</strong> <strong>Ohio</strong> Governor Taft’s Appalachian Diabetes Initiative, which focuses on heightening awareness<br />
and improving care and self-management, with the aim <strong>of</strong> preventing or delaying the onset <strong>of</strong> diabetes and its<br />
related complications. The study was funded by the Centers for Disease Control and Prevention, the Appalachian<br />
Regional Commission and the <strong>Ohio</strong> Diabetes Prevention and Control Program.<br />
The ARHI Diabetes/Endocrine Center was established in 2003 to spearhead <strong>Ohio</strong> <strong>University</strong>'s effort to increase<br />
and improve diabetes care, clinical and basic diabetes research, diabetes education, clinical outreach and<br />
training <strong>of</strong> health care pr<strong>of</strong>essionals in Southeastern <strong>Ohio</strong>. ARHI is a collaborative <strong>of</strong> several academic units<br />
including OU-COM, the <strong>College</strong> <strong>of</strong> Health and Human Services, the <strong>College</strong> <strong>of</strong> Arts and Sciences, the <strong>College</strong> <strong>of</strong><br />
Communication, the Edison Biotechnology Institute and the Voinovich Center for Leadership and Public Affairs.<br />
Schwarz suggests that the seven county findings, if confirmed in all <strong>of</strong> Appalachia, could indicate that the risk<br />
for diabetes is more closely related to poverty and obesity rather than genetics.<br />
“With all <strong>of</strong> the long-term complications associated with diabetes, I see a critical need in changes to health-care<br />
policy for adequate diabetes education,” adds Schwarz. “I’m hoping that the results <strong>of</strong> this survey will lead to<br />
funding to conduct the survey in other parts <strong>of</strong> Appalachia.”<br />
–The Editors<br />
26 www.oucom.ohio.edu
OU-COM Participates in First-<strong>of</strong>-a-kind<br />
Prehypertension Drug Study<br />
A pioneering six-year study on postponing or preventing<br />
hypertension has shown that a new drug, if introduced<br />
while a patient is prehypertensive, can reduce that patient’s<br />
risk <strong>of</strong> developing hypertension. OU-COM was one <strong>of</strong> 71<br />
sites participating in the nationwide clinical trial.<br />
The Trial <strong>of</strong> Preventing Hypertension, or TROPHY, study<br />
is groundbreaking. “It’s the first study to examine the<br />
potential to change the natural history <strong>of</strong> hypertension<br />
through early pharmacological intervention in patients<br />
diagnosed with prehypertension,” principal investigator<br />
Stevo Julius, M.D., pr<strong>of</strong>essor <strong>of</strong> internal medicine and<br />
physiology at the <strong>University</strong> <strong>of</strong> Michigan, Ann Arbor, says.<br />
Prehypertension, according to the Centers for Disease<br />
Control and Prevention, is defined as a systolic blood<br />
pressure <strong>of</strong> 120-139 mmHg or a diastolic blood pressure<br />
<strong>of</strong> 80-89 mmHg.<br />
Persons with prehypertension are at greater risk to advance<br />
to hypertension. Hypertension or high blood pressure<br />
raises the risk for heart disease and stroke, both leading<br />
causes <strong>of</strong> death in this country. About one in three adults<br />
in this country has hypertension.<br />
Patients in the TROPHY study had blood pressures <strong>of</strong><br />
130-139 (systolic) and 89 or lower (diastolic); or 139<br />
(systolic) and 85-89 (diastolic). Untreated patients, age<br />
30 to 65, were enrolled in a four-year, multicenter,<br />
randomized study.<br />
The study demonstrated that beneficial anatomic or<br />
physiologic changes were occurring in patients taking<br />
candesartan that lasted even after the medication was<br />
discontinued, says OU-COM Dean Jack Brose, D.O.<br />
“Because <strong>of</strong> this study, I think we have shown we can<br />
compete with larger sites in terms <strong>of</strong> the number <strong>of</strong><br />
patients we recruit and how well we follow the research<br />
protocols,” Brose says. Then assistant dean for clinical<br />
research, Brose served as principal investigator at OU-COM.<br />
Other participating physicians were Jay Shubrook, D.O.<br />
(‘94); Robert Gotfried, D.O.; and Chris Simpson, D.O.<br />
OU-COM managed its trial and made day-to-day decisions<br />
about patient health and participation, as did each <strong>of</strong><br />
the other 70 sites. However, OU-COM so successfully<br />
recruited patients that Julius flew Brose and research<br />
nurse Lori Arnott to Michigan to meet with researchers<br />
from a select few other top recruitment sites. They discussed<br />
the ways they had recruited patients, which was shared<br />
with the other participating sites.<br />
The college enrolled 25 patients in the study and retained<br />
23 throughout the four-year process. Patients reported<br />
“excellent” satisfaction with their participation in the<br />
clinical trial. The reason for this, says Brose, was<br />
the first-rate care that the college’s research nurse<br />
staff–Arnott; Cammie Starner; Lynn Petrik, R.N.; and<br />
Rosemary Vance–provided.<br />
The research nurses also administered routine blood<br />
pressure checks and educated patients on healthy living.<br />
Patients were evaluated every three months.<br />
“Most loved being involved with the study,” says Starner.<br />
“We did a great job <strong>of</strong> following up on them. Any suspected<br />
adverse events were dealt with quickly.”<br />
Prehypertension patients were identified with the help<br />
<strong>of</strong> local physicians. During the study, about half the<br />
patients received a placebo while the others received<br />
candesartan. After two years, those on candesartan were<br />
switched to a placebo.<br />
In March, Brose and Starner flew to Atlanta to share<br />
in the unveiling <strong>of</strong> the results at the American <strong>College</strong><br />
<strong>of</strong> Cardiology’s 55th annual Scientific Session.<br />
The study showed that after two years, patients who had<br />
received candesartan were almost 67 percent less likely<br />
to develop hypertension. After four years, when all<br />
patients had been on placebo for two years, patients<br />
who had been on candesartan were almost 16 percent<br />
less likely to develop hypertension. Brose says the study<br />
not only showed candesartan helped prevent hypertension,<br />
it showed that patients who went <strong>of</strong>f the experimental<br />
drug after two years were still less likely to develop the<br />
potentially fatal condition.<br />
“I’m very pleased that we helped contribute to this<br />
landmark study,” says Brose. “We rank right up there<br />
with the best clinical research sites in America.”<br />
Currently, OU-COM is involved in other clinical trials,<br />
including several diabetes trials, a dyslipidemia trial and a<br />
prevention trial.<br />
–Jennifer Kowalewski<br />
summer 2006 27
<strong>Medicine</strong> on the<br />
photo provided by Timothy G. Law, D.O.<br />
Whether they’re bringing medicine to the deep rain forest, making house calls to uninsured<br />
patients or tending to wounded in Iraq, <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong> grads<br />
are working on the “frontlines,” doing more than a small share <strong>of</strong> service. Their journeys are not<br />
always ones they envisioned.<br />
Not-So-Small-Town Doc<br />
After a woman in a wheelchair showed up in<br />
Timothy G. Law Sr.’s <strong>of</strong>fice with three family<br />
members-–all <strong>of</strong> whom had to take the day <strong>of</strong>f work to<br />
get her there–he said that he would come to her next<br />
time. And he did. The local hospital where he worked<br />
thought he should be in<br />
his <strong>of</strong>fice, not <strong>of</strong>f visiting<br />
patients, so Law, D.O. (‘94),<br />
started to make house calls<br />
on his time to housebound<br />
locals and those without<br />
health insurance. Twelve<br />
years later, he still does–<br />
every day.<br />
Law eventually set up practice<br />
so that, among other<br />
things, house calls could be<br />
a part <strong>of</strong> his services. In May<br />
2001, he opened the Vine<br />
Grove Family Clinic in Vine<br />
Grove, Ky., a small town<br />
with a population under<br />
3,000–the kind <strong>of</strong> town that<br />
has a main street called<br />
Main Street and a real barber<br />
shop. He drives a pickup so<br />
he can haul his supplies and<br />
carries an old-fashioned<br />
leather bag; but the Mayberry image stops there.<br />
“[This isn’t] a country bumpkin operation,” says Law,<br />
who recently moved to a larger building on–where<br />
else?–Main Street, treating everything from run-<strong>of</strong>the-mill<br />
colds and hypertension one day, performing<br />
minor surgery the next. He <strong>of</strong>fers Botox treatments,<br />
collagen injections and laser hair removal. He even has<br />
a massage therapist on staff. And he delivers babies,<br />
sometimes at home. Last May, for example, he traveled<br />
to a local Amish community to deliver triplets.<br />
His practice keeps him busy, yet once a week he also<br />
helps out at Acutecare, an emergency medical service,<br />
and for five years he has served on the board <strong>of</strong> the<br />
Kentucky <strong>Osteopathic</strong> Medical Association (KOMA).<br />
Come June, Law will become its president. Outgoing<br />
President Michael Murphy, D.O., associate dean <strong>of</strong><br />
postgraduate education at Pikeville (Ky.) <strong>College</strong> <strong>of</strong><br />
<strong>Osteopathic</strong> <strong>Medicine</strong>, is pleased. “He’s an outstanding<br />
individual, highly intelligent.” And, it seems, highly<br />
motivated: “He was a captain in the Army, a body<br />
builder–you just have to look at him to see that,” says<br />
Murphy “He has successfully run a private practice in a<br />
rural Kentucky town [and] been the program director for<br />
two KOMA scientific programs that drew rave reviews.”<br />
He drives a pickup and carries<br />
an old-fashioned bag, but the<br />
Mayberry image stops there.<br />
Law’s journey into medicine started with an Ann<br />
Landers column on osteopathic medicine. His mom<br />
thought he might be interested, so she sent it to<br />
him. After reading the column, Law decided to check<br />
out OU-COM. At age 27, with a wife and two kids,<br />
he went back to school once again. At the time, he<br />
was teaching biology at the <strong>University</strong> <strong>of</strong> Pittsburgh,<br />
where he earned a master’s in education. He also<br />
had a bachelor’s in veterinary science (he thought<br />
he’d be a farmer and a vet) from the <strong>University</strong> <strong>of</strong><br />
Pennsylvania, Philadelphia. Before settling into Vine<br />
Grove, he completed his Army stint as a general medical<br />
<strong>of</strong>ficer and traveled worldwide with the National<br />
Karate Team–his children were competing–as team doc.<br />
For now, Law is the only physician in town, and luckily<br />
he has the approval <strong>of</strong> Edward Hand, M.D., the<br />
doctor who served Vine Grove until his retirement in<br />
1998. When Law opened his practice, Hand (“He<br />
delivered most <strong>of</strong> my patients and their parents,” says<br />
Law) gave him a call. Hand’s former patients had<br />
been asking him if Law was a good doctor, so Hand<br />
had to check him out for himself. In small towns like<br />
Vine Grove, good news travels fast.<br />
Timothy Law, D.O. ('94), structured his rural practice to allow for daily house calls.<br />
28 www.oucom.ohio.edu
Frontlinesby Maureen Harmon<br />
Missionary <strong>Medicine</strong><br />
photo provided by Tim Kubacki, D.O.<br />
Tim Kubacki, D.O. (‘90), had planned to be a baseball<br />
player. He retired that dream, though, when he was cut<br />
from the Yankees minor leagues in his 20s. That dream<br />
was supplanted by an<br />
epiphany that not only<br />
rearranged his career<br />
but his life and took<br />
him all the way to the<br />
Brazilian rainforest.<br />
“I had gotten pretty<br />
wrapped up in me and<br />
my own happiness. I<br />
recognized the futility<br />
<strong>of</strong> such a pursuit,”<br />
Kubacki says. Worried<br />
about the suffering <strong>of</strong><br />
people in developing<br />
countries, Kubacki acted<br />
when a retired missionary<br />
suggested he take his biology degree and pursue<br />
a career in medicine to help those in poor areas. Kubacki<br />
found his calling. “In the next three months,” Kubacki<br />
writes in his blog, “I went from having no desire for<br />
medicine to applying to medical school” so his life would<br />
“count for something,” he says.<br />
By 1993, Kubacki had wrapped up a residency in family<br />
medicine and was working part-time at Morrow County<br />
Hospital in <strong>Ohio</strong>. Dave Keseg, who works for a company<br />
that staffs hospitals, asked Kubacki to direct Morrow<br />
County’s Emergency Department. “I knew he was a man<br />
<strong>of</strong> high integrity,” says Keseg, “… and I knew I wanted<br />
him working for our company.”<br />
“ I never cease to be amazed at<br />
the difficulty <strong>of</strong> these people’s<br />
lives.” –Tim Kubacki, D.O. (’90)<br />
Kubacki and Keseg also had similar vision and values.<br />
They opened the Vineyard Free Medical Clinic in<br />
Columbus, <strong>Ohio</strong>, which a nearby church sponsored. Every<br />
Wednesday night in the lobby <strong>of</strong> the church’s food<br />
pantry, the doctors and churchgoers <strong>of</strong>fered two hours<br />
<strong>of</strong> medical and spiritual help to the uninsured people <strong>of</strong><br />
Columbus. Kubacki, Keseg and eventually a few other<br />
volunteer physicians <strong>of</strong>fered simple medical care to<br />
“anybody that had episodic health needs,” says Keseg.<br />
It started with just a few patients a night, but now the<br />
team can expect to see between 30 and 60 patients<br />
streaming through the clinic.<br />
Kubacki was so pleased with the way spirituality and<br />
medicine complemented each other at the clinic, he<br />
wanted to replicate the model. In December 2005, he<br />
and his wife, Betsy, packed up their belongings and four<br />
children and headed to Brazil near the Xingu River, a<br />
tributary to the Amazon.<br />
“[It was a] a bittersweet parting,” says Keseg. On the<br />
one hand they were losing a friend and a fine doctor,<br />
but “we know this is something the Lord has laid on<br />
[Kubacki’s] heart for a long time,” he said.<br />
In Brazil, Kubacki joined a group called the Xingu Mission<br />
in the small town <strong>of</strong> Altamira, where Kubacki and his<br />
family are now living. The interdenominational group <strong>of</strong><br />
nine families had been doing missionary work in the area<br />
for a decade. Kubacki, who is working to get a Brazilian<br />
medical license, is the first physician to join the group and<br />
address medical needs.<br />
“The area is the Amazon Rain Forest that you’ve read<br />
about.” It is rife with problems typical <strong>of</strong> tropical regions,<br />
which <strong>of</strong>ten have no running water or electricity: dysentery,<br />
malaria and parasitic illness. He’s seen leprosy and<br />
tuberculosis. But, “It’s absolutely beautiful,” he’s quick to<br />
point out. Still, he writes, “I never cease to be amazed at<br />
the difficulty <strong>of</strong> these people’s lives.” He travels quite a<br />
http://spaces.msn.com/members/kubacki6<br />
For Tim Kubacki, D.O. ('90), a call to missionary medicine in Brazil was a family affair.<br />
summer 2006 29
it, treating people as he goes and delivering his<br />
spiritual message. His group also dispenses practical<br />
items, such as water filters.<br />
Some <strong>of</strong> the work he’s done in the Amazon has already<br />
earned him honor among the people. One family was<br />
thrilled just to receive some Children’s Motrin to lessen<br />
a daughter’s pain from mouth sores. The little girl, on<br />
the other hand, was not so pleased to learn that<br />
Kubacki was a doctor. “The child immediately began<br />
crying, afraid she was to receive a shot,” Kubacki wrote.<br />
“Made me feel right at home!”<br />
For an in-depth account <strong>of</strong> Kubacki’s work in Brazil,<br />
see his blog at http://spaces.msn.com/members/kubacki6/<br />
Service to His Country<br />
As an embedded journalist for TIME magazine, it was<br />
Michael Weisskopf’s job to ride along with soldiers<br />
from a U.S. artillery survey unit when it patrolled the<br />
streets <strong>of</strong> Baghdad. That’s where a grenade landed<br />
in his vehicle. Weisskopf picked it up to toss it out,<br />
according to TIME’s Dec. 29, 2003, issue, but it exploded.<br />
Weisskopf’s hand was gone. His arm was bleeding<br />
badly. When he was transported to the 28th Combat<br />
Support Hospital, surgeon Gregory Hill, D.O. (‘86),<br />
was on the job.<br />
Located in Baghdad’s Green Zone, Hill’s hospital was<br />
the referral center for support units patrolling and<br />
fighting in places like Mosul, Falluja, Tikrit and<br />
Baghdad. Though journalists weren’t Hill’s typical<br />
patients (soldiers, Iraqi civilians, even insurgents<br />
were), he had seen that kind <strong>of</strong> trauma plenty <strong>of</strong><br />
times during his two deployments in the Middle<br />
“ A lot <strong>of</strong> times, docs can be alo<strong>of</strong>.<br />
They’re on call 24 hours, and<br />
they never get any rest. But Dr.<br />
Hill was always right there.”<br />
–Capt. Terry Partin<br />
East–open fractures, gunshot wounds from arms<br />
fire, and injuries from explosives. He also saw the<br />
kinds <strong>of</strong> injuries you wouldn’t associate with wartime,<br />
such as sprained ankles from basketball games, injuries<br />
from car accidents, and plenty <strong>of</strong> somatic dysfunction.<br />
“[Soldiers] were wearing body armor in the field and<br />
on convoys and missions, sometimes for days at a time,”<br />
Hill says. So he added trigger-point injections and<br />
s<strong>of</strong>t-tissue techniques to his regimen.<br />
Hill always knew he was going to be a doctor, and<br />
joining the military–a family tradition–<br />
was a good way to pay for school. “All<br />
<strong>of</strong> my [male] siblings have been in the<br />
military,” he says.<br />
Still, the Middle East was a long way from<br />
where Hill began his medical career. He<br />
did his internship and orthopedic surgery<br />
residency at Cuyahoga Falls General<br />
Hospital followed by a one-year handand<br />
upper-extremity microsurgery fellowship<br />
at the <strong>University</strong> <strong>of</strong> Buffalo.<br />
Hill then headed for Akron, <strong>Ohio</strong>, to a<br />
private practice, but after September 11, he<br />
would be the first <strong>Ohio</strong> doctor mobilized<br />
to Iraq. After six months, he was back in<br />
Akron, but by August 2005, Hill again<br />
found himself on a military plane headed<br />
for the war.<br />
The second tour would find him squarely<br />
in the line <strong>of</strong> fire, the only physician<br />
working in a battalion aid station not far<br />
Gregory Hill, D.O. ('86), was the first <strong>Ohio</strong> physician mobilized to Iraq.<br />
30 www.oucom.ohio.edu
from the Syrian border (where Al-Qaeda<br />
fighters were believed to enter Iraq).<br />
According to the battalion chaplain, Capt.<br />
Terry Partin, they all were targets for rockets,<br />
mortars and up to two attacks a day from<br />
explosive devices or small-arms fire.<br />
In those harrowing conditions, Hill took care<br />
<strong>of</strong> his patients–and fellow medics. “A lot <strong>of</strong><br />
times, docs can be alo<strong>of</strong>,” Partin says. “They’re<br />
on call 24 hours, and they never get any rest. But<br />
Dr. Hill was always right there…you’d <strong>of</strong>ten<br />
find him hanging out at the medic stations.”<br />
Hill, “old enough to be some <strong>of</strong> these kids’<br />
fathers,” required his crew to be all business<br />
with the wounded, but made himself available<br />
during down time. “They came to ask me<br />
questions about relationships, marriage, my<br />
opinions about women,” he says. “I had<br />
already been through these things.”<br />
His own life has settled down a bit now that<br />
he’s stateside. Early this year, Hill–husband,<br />
father <strong>of</strong> four, and soon-to-be grandfather–<br />
became a staff physician at Orthopedic<br />
Surgery and Sports <strong>Medicine</strong> in Temecula, Calif.,<br />
and is on staff at Southwest Healthcare System<br />
and Riverside County Regional Medical Center,<br />
a level-one Trauma Center in Moreno Valley.<br />
And last year, Weisskopf tells Today’s D.O. he<br />
looked up Hill. The journalist interviewed him<br />
for Blood Brothers: Among the Soldiers <strong>of</strong><br />
Ward 57, Weisskopf’s book, due out this fall.<br />
Though Hill is readjusting to civilian life,<br />
memories <strong>of</strong> the war stick with him. “It’s one<br />
<strong>of</strong> those things I think about on a daily basis,”<br />
he says. He still will jump at loud noises like<br />
cars backfiring or the sound <strong>of</strong> metal on<br />
metal in the operating theater. It takes him<br />
back to the hair-trigger questions you would<br />
always have on your mind over there: “How<br />
close was that explosion? Was it incoming or<br />
outgoing?” For now it’s neither. But as long<br />
as he’s a military man, there’s always a chance<br />
Hill will see the front a third time.<br />
TODAY’S<br />
<strong>DO</strong><br />
In the Aftermath<br />
Just two weeks after Hurricane Katrina hit the Gulf Coast last August,<br />
Eric Beck trawled the flooded streets <strong>of</strong> New Orleans on a boat with<br />
volunteers and military personnel, looking for survivors. The crew<br />
stopped at every door, calling out for survivors, sometimes cutting the<br />
engine for fear <strong>of</strong> missing shouts for help. Beck and coworkers rescued<br />
five people still living in the attics <strong>of</strong> their homes, severely dehydrated.<br />
Two were diabetic and in desperate need <strong>of</strong> insulin. All were too weak<br />
to protest leaving any more.<br />
Beck should have been preparing for his second year at <strong>Ohio</strong> <strong>University</strong><br />
<strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong> when Katrina struck, but he couldn’t<br />
overcome his nature. A volunteer firefighter and paramedic, Beck’s list <strong>of</strong><br />
volunteer and work activities goes on and on. In addition to being a<br />
student, Beck works part-time at Coolville, <strong>Ohio</strong>, Emergency Medical<br />
Services. His boss there, Joe Egan, only sees him about twice a month<br />
when their schedules collide, but even in that short time, Egan thinks he<br />
made a pretty good hire. “His skills are on par with anybody out there,”<br />
Egan says.<br />
Beck has helped out in emergency rooms and clinics for schools, donates<br />
his time to give local Boy Scouts physical examinations as part <strong>of</strong> the group’s<br />
Annual Physical Examination Program, and is an instructor for OU-COM’s<br />
Annual Continuing Medical Education Program, where he teaches Advanced<br />
Cardiac Life Support. “He’s a pretty busy guy,” Egan says.<br />
No surprise, then, that Beck put school on hold, hopped a flight to Baton<br />
Rouge, La., and volunteered at a makeshift command center for 24-hour<br />
rescue operations.<br />
Though Beck had done rescue missions before, never had he seen anything<br />
quite like this. “There were literally bodies all over the place,” he says,<br />
adding that some were “covered head to toe in, essentially, sewage. ..."<br />
One man’s plight will stay with Beck for a long time. He only knows him<br />
as Travis, a retired New Orleans<br />
police <strong>of</strong>ficer, who was waiting<br />
it out with his wife at a shelter<br />
at Nicholls State <strong>University</strong> in<br />
Thibodaux, La. Travis hadn’t<br />
been religious about taking his<br />
medication before the storm,<br />
but with none available, he had<br />
begun to suffer seizures and<br />
fainting spells. But when Beck’s<br />
team tried to take Travis to a<br />
nearby hospital, he refused to go<br />
without his scores <strong>of</strong> cardboard<br />
boxes filled with personal<br />
treasures. Beck and the other<br />
paramedics couldn’t make him<br />
choose–they loaded all <strong>of</strong> the boxes and Travis onto the ambulance.<br />
It’s not only the victims <strong>of</strong> Katrina that stand out to Beck, it’s also the<br />
people who came to help. He joined hundreds <strong>of</strong> volunteers and military<br />
personnel in that command center in Baton Rouge. “For all <strong>of</strong> the problems<br />
our country and our world have,” says Beck, “people still do rally around<br />
those who are in need."<br />
–Maureen Harmon with Melissa Cabral<br />
Eric Beck, OMS II and 2006 OU-COM Student D.O. <strong>of</strong> the Year (with parents Scott and<br />
Preston Beck), says that after Katrina, “There were literally bodies all over the place.”<br />
summer 2006 31
CORE News<br />
CORE Receives Commendations<br />
The Centers for <strong>Osteopathic</strong> Research and Education (CORE), a medical education consortium that<br />
includes the <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong> (OU-COM), 14 teaching hospitals and<br />
three affiliated colleges <strong>of</strong> osteopathic medicine, received two commendations during the American<br />
<strong>Osteopathic</strong> Association (AOA) on-site inspection in February.<br />
AOA inspectors commended the CORE for its three-year osteopathic manipulative medicine (OMM)<br />
clinical curriculum and for the research initiatives it has undertaken in the past three years.<br />
“The CORE has been described by many in our pr<strong>of</strong>ession as ‘the gold standard’ in graduate medical<br />
education,” Jack Brose, D.O., OU-COM dean, says. “That reputation has been reinforced by this visit.”<br />
“It was a spotless inspection,” Keith Watson, D.O., chief academic <strong>of</strong>ficer for CORE and OU-COM<br />
associate dean for graduate medical education, said. “We hope to be one <strong>of</strong> the first <strong>Osteopathic</strong> Postdoctoral<br />
Training Institutes (OPTI) to achieve a five-year accreditation award.”<br />
AOA inspections are required to reaccredit the CORE as an OPTI. Although AOA can reaccredit an OPTI<br />
for up to five years, OPTIs have been receiving reaccreditation for three and a half years on average<br />
according to a 2002 survey by Scott Dalhouse, the OPTI manager <strong>of</strong> the AOA department <strong>of</strong> education.<br />
Cheryl Riley, R.N., M.S., assistant dean for academic affairs and CORE operations, explained that CORE<br />
met all but one minor standard regarding sign-<strong>of</strong>fs on conflict <strong>of</strong> interest statements. “And that’s easily<br />
corrected, virtually with a stroke <strong>of</strong> the pen.”<br />
Riley, whose association with the CORE extends to its very beginning, credited the hospitals and their<br />
collaborative relationship for innovations in the curriculum.<br />
“I’ve watched enormous change in both predoctoral and postdoctoral osteopathic medical education as<br />
program directors from all over <strong>Ohio</strong> have met regularly over the years to share best practices and<br />
troubleshoot issues,” Riley said.<br />
The osteopathic pr<strong>of</strong>ession is currently tackling challenges in graduate medical education (GME). At an<br />
inaugural medical education summit held last January sponsored by the <strong>Osteopathic</strong> Heritage Foundations,<br />
the AOA and the American Association <strong>of</strong> <strong>College</strong>s <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong>, over 70 leaders met to<br />
identify and examine osteopathic GME. They also began to develop strategies to respond to those issues.<br />
Watson chaired the summit’s steering committee (see “Noteworthy,” page 4).<br />
“We do face tough issues ahead in educating the doctors <strong>of</strong> tomorrow,” Watson explains. “The trend<br />
among students to move away from osteopathic GME programs, the question <strong>of</strong> a physician shortage,<br />
the shortage <strong>of</strong> GME funding, perceptions <strong>of</strong> quality in osteopathic GME programs, the lower priority <strong>of</strong><br />
research in osteopathic medical education–these are just a few <strong>of</strong> the issues being discussed nationally. We<br />
need to be ready to respond in the CORE.”<br />
Riley says the CORE system will continue making improvements–plans are already underway to expand<br />
the OMM clinical curriculum to the residency years–using what it has learned from the on-site survey<br />
and the self-study, which OU-COM completed before the site visit.<br />
–Jennifer Kowalewski<br />
Grandview Receives Three Top Honors<br />
Grandview Medical Center in Dayton, <strong>Ohio</strong>, has just won the equivalent <strong>of</strong> a hospital triple crown-three<br />
times over.<br />
In February, Grandview landed on the coveted Solucient 100 Top Hospitals list for teaching hospitals for<br />
its third time. It is one <strong>of</strong> only 25 hospitals in the nation to receive the designation.<br />
This came after winning, for the third year in a row, the Health Grades Distinguished Hospital for Clinical<br />
Excellence. Only 5 percent <strong>of</strong> the more than 5,000 hospitals in the nation receive this honor.<br />
For a third year also, Grandview was ranked in the top 50 <strong>of</strong> U.S. News and World Report's Best Hospitals.<br />
It placed 44th in the Respiratory Disorders category and in the Neurology and Neurosurgery category.<br />
32 www.oucom.ohio.edu
Grandview Hospital, with 450 beds, is the flagship <strong>of</strong> Grandview Medical Center's facilities and a Centers for <strong>Osteopathic</strong><br />
Research and Education (CORE) site.<br />
“It's pretty exciting for a hospital in Dayton to be ranked with the Mayo Clinics and the Johns Hopkins <strong>of</strong> the world,”<br />
Craig Self, director business development, Grandview and Southview Hospitals, says.<br />
To arrive at their rankings, the ratings organizations look at various clinical outcomes–such as Medicare-reported<br />
morbidity, mortality and length <strong>of</strong> stay–and financial indicators, operational data and growth. In large part, a “very<br />
aggressive quality improvement process” is responsible for the national recognition the medical center receives,<br />
according to Self.<br />
Peter A. Bell, D.O., assistant dean for the CORE sites in Dayton and Columbus, believes the honors played a role in<br />
the record number <strong>of</strong> internship applications that Grandview received this year. “We've had so many medical students<br />
wanting to come here for their internships. We doubled our numbers,” he says.<br />
“Residents, interns and medical students who come here are a critical part <strong>of</strong> this success, Self says. “They learn how we<br />
attain high quality standards at Grandview and are able to understand and adopt them. It makes for better education and<br />
stronger osteopathic medicine in the nation in general,” he says<br />
–Sally Linder<br />
CORE Celebrated its 10th Anniversary During its April Board Meeting<br />
More than 50 hospital executives, CORE representatives, and <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong><br />
<strong>Medicine</strong> faculty and staff members gathered in Pickerington, <strong>Ohio</strong>, where they commemorated three<br />
individuals and ten hospitals for their founding roles in the CORE.<br />
CORE Assistant<br />
DeanNamed<br />
Cheryl Riley, R.N., M.S., assistant dean for academic affairs and<br />
CORE operations, was one <strong>of</strong> three individuals who were awarded<br />
a Crystal Apple, the highest honor bestowed upon those who have<br />
given above and beyond in the call <strong>of</strong> CORE duty. (Left to right)<br />
Jack Brose, D.O., dean, OU-COM; Keith Watson, D.O., chief<br />
academic <strong>of</strong>ficer for CORE and OU-COM associate dean for graduate<br />
medical education; Riley; and Roy G. Chew, Ph.D., president <strong>of</strong><br />
Grandview Medical Center and chairman <strong>of</strong> the CORE board.<br />
Andrew Culver, D.O.<br />
(‘99), has been named<br />
CORE assistant dean at<br />
Doctors Hospital <strong>of</strong><br />
Stark County. Culver<br />
has been the acting<br />
assistant dean since<br />
November 2005.<br />
Christopher Meyer, D.O., and Richard Vincent, president, <strong>Osteopathic</strong> Heritage Foundations, also received<br />
Crystal Apples in honor <strong>of</strong> their roles as the founding chairmen <strong>of</strong> the CORE board.<br />
summer 2006 33
Alumni Update<br />
Mentoring Made Easy<br />
by Sharon Zimmerman<br />
Jeff Stanley, D.O. (‘82)<br />
For nearly every student who has walked through the doors <strong>of</strong> OU-COM, life changes<br />
dramatically <strong>of</strong>ten in part because <strong>of</strong> an interaction with someone in the osteopathic<br />
pr<strong>of</strong>ession. <strong>Osteopathic</strong> physicians have a long history <strong>of</strong> reaching out to those learning<br />
the art <strong>of</strong> osteopathic medicine. You, our OU-COM alumni, play an ever critical role,<br />
both as health-care providers and as advocates for our medical students. Why? Because it<br />
is the right thing to do.<br />
In April during our Career Medical Specialties week, students listened to alumni perspectives<br />
about what to really expect in a specific medical discipline, how to get the most out <strong>of</strong><br />
their medical education, and how to prepare for a graduate medical education program.<br />
I’ve spoken to one student recently who decided to enter emergency medicine after talking<br />
with one <strong>of</strong> our graduates. Another decided to enter family medicine after listening to<br />
the rewarding experiences that one <strong>of</strong> our visiting graduates shared. Whether it’s on campus, at one<br />
<strong>of</strong> our Centers for <strong>Osteopathic</strong> Research and Education, or at an annual state or national conference, our<br />
alumni have <strong>of</strong>ten supplied that critical experience, conversation, or even a moment that has made a difference<br />
in a student’s future.<br />
Maybe you remember someone who made a difference in your career, or perhaps there was a crucial conversation<br />
you wish you would have had with someone. It’s not difficult to be a mentor to a student, and it can<br />
take as much–or as little–time as you have to <strong>of</strong>fer. Here are nine ways you can mentor a student:<br />
1. Provide the industry lowdown during Career Medical Specialties Week at OU-COM.<br />
2. Congratulate the newest generation <strong>of</strong> Bobcat physicians each year during the OU-COM Alumni<br />
Graduation Reception.<br />
3. Introduce a student to at least one person who will help launch his or her career during the annual<br />
AOA, OOA or ACOFP Conventions.<br />
4. Join students for D.O. Day in Washington D.C. or at the <strong>Ohio</strong> Statehouse to discuss<br />
issues concerning osteopathic medical education and practice.<br />
5. Add your perspective as a practicing physician to our annual Policy Puzzle Program, which<br />
introduces students to local, state and national health-care policy issues.<br />
6. Join our discussion about pr<strong>of</strong>essionalism in osteopathic medicine by participating in our<br />
Pr<strong>of</strong>essionalism Series for year first- and second-year students.<br />
7. Share your passion for research during our Alumni Research Series.<br />
8. Become a CORE clinical faculty member and have a student at your side in your <strong>of</strong>fice or hospital.<br />
9. Provide financial assistance to support student travel to pr<strong>of</strong>essional osteopathic conventions and conferences.<br />
Give me a call. I’m happy to discuss these and other ways you can lend your support, share your gifts and<br />
show your <strong>Ohio</strong> alumni pride to a future osteopathic physician.<br />
Nicole Wadsworth, D.O. (‘97)<br />
To learn more about mentoring opportunities, contact Sharon Zimmerman at zimmerms@ohio.edu or<br />
(740) 593-0761.<br />
34 www.oucom.ohio.edu
Anderson Appointed to<br />
the <strong>University</strong>'s Alumni Board<br />
Thomas M. Anderson, D.O. (‘83), FACRO, was appointed to<br />
<strong>Ohio</strong> <strong>University</strong>'s Alumni Association Board <strong>of</strong> Directors. The<br />
board, which serves as an advisory body for the Alumni Association,<br />
helps to shape policy for the association and assists it in fulfilling<br />
its mission, which includes volunteerism, philanthropy and advocacy.<br />
Anderson, who currently serves as president <strong>of</strong> the OU-COM<br />
Society <strong>of</strong> Alumni and Friends, was named to a three-year term<br />
this spring.<br />
“It is a privilege for me to give back,” Anderson said. “I have said<br />
so many times, if it hadn't been for OU-COM, I would never<br />
have been a doctor. This appointment is an honor I didn’t expect.<br />
I am looking forward to representing OU-COM and its graduates,<br />
but this is a wonderful opportunity to represent graduates from<br />
all <strong>Ohio</strong> <strong>University</strong> colleges.”<br />
Anderson was chosen to sit on the 24-member board because <strong>of</strong><br />
his strong ties to both the university and the medical community,<br />
says Ralph Amos, executive director <strong>of</strong> the alumni association<br />
and assistant vice president for alumni relations.<br />
“We're excited to have him join the board. Tom is a proven,<br />
dynamic leader with a keen mind for strategic thinking and<br />
planning,” says Amos. The board, says Amos, also engages in<br />
outreach to university departments involved in alumni relations<br />
and oversees a host <strong>of</strong> programs available to alumni.<br />
“I’ve observed his outstanding leadership in the university over<br />
the years and look forward to all that he will undoubtedly bring<br />
to the board.”<br />
Anderson, a respected specialist in radiation oncology, is the<br />
medical director <strong>of</strong> Hobbs Oncology Center, Oncology Services<br />
<strong>of</strong> Doctors Hospital <strong>Ohio</strong> Health and the Heartland Hospice in<br />
Columbus. He is chairman <strong>of</strong> the Radiation Safety Committee at<br />
Doctors Hospital <strong>Ohio</strong> Health. As a CORE clinical pr<strong>of</strong>essor,<br />
Anderson trains future osteopathic physicians from OU-COM,<br />
and he has participated in many OU-COM events including the<br />
annual alumni CME gathering and Career Medical Specialties Week.<br />
Anderson has received numerous honors and awards over the<br />
years, including the <strong>Ohio</strong> <strong>University</strong> Master Volunteer Clinical<br />
Teaching Award, Doctors Hospital Patient Educator <strong>of</strong> the Year<br />
Award, Outstanding Oncology Caregiver Award,<br />
Columbus Cancer Clinic Outstanding Healthcare<br />
Pr<strong>of</strong>essional <strong>of</strong> the Year Award, and most<br />
recently, the 2005 Physician Customer<br />
Service Champion Award from <strong>Ohio</strong> Health.<br />
“Dr. Anderson is truly a model osteopathic<br />
physician and an alumnus who continues to<br />
make a positive impact on the college and the<br />
university,” said Dean Jack Brose, D.O.<br />
“He strives to serve as an advocate through<br />
his excellent leadership abilities.” Thomas Anderson, D.O. (‘83)<br />
Alumni Events Calendar<br />
June 20-24<br />
American Association <strong>of</strong> <strong>College</strong>s <strong>of</strong> <strong>Osteopathic</strong><br />
<strong>Medicine</strong><br />
Annual Meeting and Capitol Hill Day<br />
Theme: Challenges and Opportunities<br />
Renaissance Harborplace Hotel<br />
Baltimore, Md.<br />
For information, contact: Tom Levitan, e-mail tlevitan@aacom.org; or<br />
visit www.aacom.org/events/annualmtg<br />
June 22-25<br />
<strong>Ohio</strong> <strong>Osteopathic</strong> Association Convention<br />
The Lodge at Sawmill Creek Resort<br />
Huron/Sandusky, <strong>Ohio</strong><br />
For information, contact: Jean Eberst, (800) 234-4848, Ext. 204;<br />
e-mail jeberst@ooanet.org; or visit www.ooanet.org<br />
June 22: OU-COM Alumni Reception, 5:30-7:30<br />
For information about OU-COM events, contact: Carol Blue,<br />
(740) 593-2178; e-mail blue@ohio.edu<br />
Aug. 12<br />
OU-COM Convocation and White Coat Ceremony<br />
Templeton Blackburn Memorial Auditorium<br />
Athens<br />
11 am<br />
Sept. 29-Oct. 1<br />
Doctors Hospital Annual Family Practice CME Conference<br />
Dublin Marriott, Dublin, <strong>Ohio</strong><br />
For information, contact: Geri Urse, D.O. (‘93), (614) 544-0101<br />
Oct. 16-20<br />
American <strong>Osteopathic</strong> Association 111th Annual<br />
Convention and Scientific Seminar<br />
Theme: D.O.s: A Family <strong>of</strong> <strong>Medicine</strong> Built on the Basics<br />
Las Vegas Hilton Hotel, Las Vegas, Nev.<br />
For information, contact: (800) 621-1773, ext. 8256;<br />
e-mail convention@osteopathic.org; or visit<br />
www.do-online.osteotech.org (click on “Convention Home”)<br />
Conference reservations open in June.<br />
OU-COM special conference events:<br />
Oct. 17: OU-COM Alumni Luncheon, 1:15 pm, Hilton Convention Center<br />
Oct. 17: OU-COM Reception, 6 pm, Hilton Hotel<br />
For information about OU-COM events, contact: Sharon Zimmerman,<br />
(740) 593-2176; e-mail zimmerms@oucom.ohiou.edu<br />
Oct. 27-29<br />
Annual OU-COM Alumni CME/Reunion Program<br />
Columbus Hilton Hotel at Easton, Columbus, <strong>Ohio</strong><br />
For hotel reservations, call: (614) 414-5000<br />
For information, contact: Sharon Zimmerman,<br />
(740) 593-2176; e-mail zimmerms@oucom.ohiou.ed<br />
summer 2006 35
Congratulations<br />
Two <strong>of</strong> OU-COM’s longest tenured<br />
pr<strong>of</strong>essors retire this year. (Kind <strong>of</strong>.)<br />
Robert Hikida, Ph.D., and John Howell, Ph.D.,<br />
recently accepted <strong>Ohio</strong> <strong>University</strong>’s <strong>of</strong>fer<br />
<strong>of</strong> early retirement. We question the word<br />
“early,” though, given their combined 66<br />
years <strong>of</strong> service to the <strong>Ohio</strong> <strong>University</strong><br />
<strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong>.<br />
Fortunately for OU-COM students, Hikida<br />
and Howell will continue to conduct research<br />
and they will teach the subjects they love<br />
(microanatomy, and physiology and its<br />
relation to OMM, respectively) for one<br />
academic quarter a year.<br />
Robert Hikida, Ph.D.<br />
John Howell, Ph.D.<br />
OU-COM thanks you, pr<strong>of</strong>essors, for all you’ve given<br />
to the students, the college and the pr<strong>of</strong>ession.
Congratulations<br />
Class <strong>of</strong> 2006
inside this issue<br />
world class performances and special deliveries<br />
5<br />
OU-COM Grad Goes World Class<br />
Julianna Batizy-Morley, D.O. (‘96),<br />
wins a world triathlon championship,<br />
despite disabling pulmonary emboli<br />
just one year earlier.<br />
14<br />
The Obstetrics Dilemma<br />
Choices for doctors and patients–and<br />
the very fabric <strong>of</strong> a specialty–have<br />
been altered by litigation and soaring<br />
malpractice premiums.<br />
<strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong><br />
332 Grosvenor Hall<br />
Athens, OH 45701<br />
Non Pr<strong>of</strong>it Org.<br />
U.S. Postage<br />
PAID<br />
Permit No. 100<br />
Athens, OH<br />
ADDRESS SERVICE REQUESTED