Lymphadenectomy and Extended Resections - Pancreatic Cancer ...
Lymphadenectomy and Extended Resections - Pancreatic Cancer ...
Lymphadenectomy and Extended Resections - Pancreatic Cancer ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
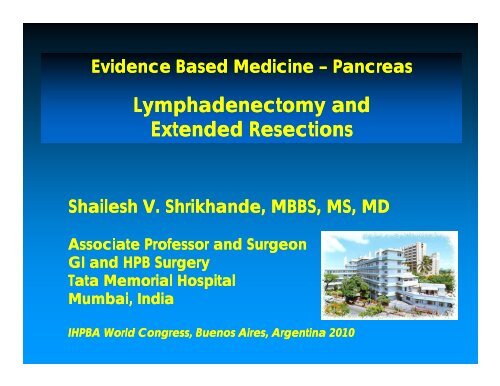
Evidence Based Medicine – Pancreas<br />
<strong>Lymphadenectomy</strong> <strong>and</strong><br />
<strong>Extended</strong> <strong>Resections</strong><br />
Shailesh V. Shrikh<strong>and</strong>e, MBBS, MS, MD<br />
Associate Professor <strong>and</strong> Surgeon<br />
GI <strong>and</strong> HPB Surgery<br />
Tata Memorial Hospital<br />
Mumbai, India<br />
IHPBA World Congress, Buenos Aires, Argentina 2010
Lymph node stations<br />
Anterior <strong>Pancreatic</strong>oduodenal<br />
Posterior <strong>Pancreatic</strong>oduodenal<br />
Common hepatic artery<br />
Hepatoduodenal d ligament<br />
Superior mesenteric artery
Japan Pancreas Society<br />
Alexakis et al., Br J Surg 2004
Lymph Node Involvement<br />
Fern<strong>and</strong>ez-Cruz et al. Dig Surg 1999<br />
Esposito I et al., Ann Surg Oncol 2008
St<strong>and</strong>ard <strong>Lymphadenectomy</strong>:<br />
What happens in the real world?<br />
4005 patients (SEER database, 1988 – 2003)<br />
Inadequate number of lymph nodes<br />
evaluated<br />
N0 patients with < 12 LN‘s are understaged<br />
N1 patients: Ratio of metastatic to<br />
examined LN‘s will better stratify prognoses<br />
Slidell MB et al., Ann Surg Oncol 2008
Open Question<br />
Quality of Histopathology<br />
LN range 0-30<br />
pTNM -status t<br />
was<br />
commonly without<br />
LN count<br />
Prognostic<br />
significance?<br />
Slidell MB et al., Ann Surg Oncol 2008
<strong>Extended</strong> <strong>Lymphadenectomy</strong><br />
RCT‘s<br />
Pedrazzoli et al., Ann Surg 1998 (81 patients)<br />
Henne-Bruns et al., Hepatogastroenterol 1998<br />
Yeo et al., Ann Surg 2002 (294 patients)<br />
Nimura et al., Pancreatology 2004 (101 patients)<br />
Farnell et al. Surgery 2005 (79 patients)
What constitutes <strong>Extended</strong><br />
<strong>Lymphadenectomy</strong>?<br />
1998<br />
No. of lymph nodes in the extended<br />
d<br />
groups<br />
20 (Pedrazolli)<br />
29 (Yeo)<br />
36 (Farnell)<br />
2005<br />
40 (Nimura)
<strong>Extended</strong> radical resection<br />
RCT (40 vs. 41)<br />
Lymph node positive patients<br />
St<strong>and</strong>ard<br />
<strong>Extended</strong><br />
Survival<br />
~ 11 months ~ 18 months<br />
p < 0.05<br />
(subgroup analysis)<br />
Pedrazzoli et al., Ann Surg 1998
St<strong>and</strong>ard vs <strong>Extended</strong> resection<br />
Three continents<br />
(Europe, America, Asia)<br />
No benefit of extended<br />
lymphadenectomy!
St<strong>and</strong>ard vs. <strong>Extended</strong> Lymphadnectomy<br />
Review:<br />
Comparison:<br />
Outcome:<br />
LA in PDAC<br />
01 <strong>Extended</strong> LA vs St<strong>and</strong>ard LA<br />
02 3 YSR<br />
3-year survival<br />
Study <strong>Extended</strong> LA St<strong>and</strong>ard LA OR (r<strong>and</strong>om) Weight OR (r<strong>and</strong>om)<br />
or sub-category n/N n/N 95% CI % 95% CI<br />
Pedrazzoli 1998 9/41 9/40 14.71 0.97 [0.34, 2.76]<br />
Yeo 2002 65/148 64/146 56.03 1.00 [0.63, 1.59]<br />
Farnell 2005 16/39 10/40 17.28 2.09 [0.80, 5.44]<br />
Nimura 2005 5/50 9/51 11.98 0.52 [0.16, 1.67]<br />
Total (95% CI) 278 277 100.00 1.05 [0.69, 1.59]<br />
Total events: 95 (<strong>Extended</strong> LA), 92 (St<strong>and</strong>ard LA)<br />
Test for heterogeneity: Chi² = 3.42, df = 3 (P = 0.33), I² = 12.4%<br />
Test for overall effect: Z = 0.21 (P = 0.83)<br />
Review:<br />
Comparison:<br />
Outcome:<br />
LA in PDAC<br />
01 <strong>Extended</strong> LA vs St<strong>and</strong>ard LA<br />
04 Overall Complications<br />
0.1 0.2 0.5 1 2 5 10<br />
Favours <strong>Extended</strong> LA Favours St<strong>and</strong>ard LA<br />
morbidity<br />
Study <strong>Extended</strong> LA St<strong>and</strong>ard LA OR (r<strong>and</strong>om) Weight OR (r<strong>and</strong>om)<br />
or sub-category n/N n/N 95% CI % 95% CI<br />
Pedrazzoli 1998 8/41 11/40 27.46 0.64 [0.23, 1.81]<br />
Yeo 2002 79/148 36/146 31.3434 3.50 [2.13, 5.74]<br />
Farnell 2005 39/39 25/40 13.37 48.02 [2.75, 838.36]<br />
Nimura 2005 34/50 7/51 27.83 13.36 [4.94, 36.11]<br />
Total (95% CI) 278 277 100.00 4.52 [1.16, 17.61]<br />
Total events: 160 (<strong>Extended</strong> LA), 79 (St<strong>and</strong>ard LA)<br />
Test for heterogeneity: Chi² = 20.64, df = 3 (P = 0.0001), I² = 85.5%<br />
Test for overall effect: Z = 2.17 (P = 0.03)<br />
0.1 0.2 0.5 1 2 5 10<br />
Favours <strong>Extended</strong> LA Favours St<strong>and</strong>ard LA<br />
Michalski CW et al., Br J Surg 2007
PPPD or Whipple Resection?<br />
Survival<br />
Favors pppd<br />
Favors c Whipple<br />
RCT’s 6<br />
Equally radical operations<br />
No difference in survival<br />
No difference in morbidity / mortality<br />
Similar QOL<br />
Wenger et al., Chirurg 1999<br />
Tran et al., Ann. Surg. 2004<br />
Lin et al., Hepatogastroenterology 2005<br />
Seiler et al., Br. J. Surg. 2005<br />
Paquet et al., Chir. Gastroenterol. 1998<br />
Bloechle et al., DGCh Forumb<strong>and</strong> 1999<br />
Diener M et al., Ann. Surg. 2007
MARGIN POSITIVE RESECTIONS<br />
Short survival <strong>and</strong> early recurrence!<br />
Author R1 /<br />
R2<br />
Millikan 1999<br />
% pts Survival<br />
Survival<br />
+ ve -ve<br />
R1 29% 8 mo 17 mo<br />
Sohn 2000<br />
R1/R2 30% 12 mo 19 mo<br />
Benassai 2000<br />
Neoptolemos<br />
2001<br />
Richter 2003<br />
Takai 2003<br />
Kuhlmann 2004<br />
R1/R2 20% 9 mo 26 mo<br />
R1 19% 11 mo 17 mo<br />
R1/R2 37% NS<br />
NS<br />
R1/R2 68% 8 mo 23 mo<br />
R1/R2 50% NS<br />
NS<br />
Varadhachary GR, Tamm EP et al. Ann Surg Oncol 2006;13:1035-46.<br />
Katz MH, Pisters PW et al. J Am Coll Surg. 2008;206:833-46; discussion 846-8. 8.
Borderline resectable tumors
SMV /<br />
PV Resection<br />
16 cohorts<br />
> 640 patients with venous resection<br />
Mortality <strong>and</strong> morbidity not increased<br />
No higher N+ <strong>and</strong> R1 resection rates<br />
rather a problem of tumor location than of<br />
aggressive biology<br />
Hartel et al., Eur J Surg 2002, Fuhrman et al., Ann Surg 1996,<br />
Harrison et al., Ann Surg 1996
BORDERLINE RESECTABLE TUMORS:<br />
The Contradictions…<br />
St<strong>and</strong>ard PD<br />
VR<br />
181 patients 26.5 months<br />
110 patients 23.4 months<br />
VR must be offered <strong>and</strong> results are superior<br />
to historical “Locally advanced disease”<br />
BUT<br />
If vein positive, artery also positive!<br />
Tseng JF, Raut CP et al. J Gastrointest Surg 2004:8;935-4949
Borderline Resectable<br />
<strong>Pancreatic</strong> <strong>Cancer</strong> with<br />
Vein Resection<br />
SMV – PV involved but SMA free!<br />
GDA involved but HA free!<br />
Large head mass but neck free!
Correlated with depth of invasion<br />
Poor outcomes<br />
Fukuda S, Ossoultzoglou E et al. Arch Surg 2007:142;172-79<br />
79
Venous Resection (SMV / PV)<br />
Fair evidence for resection<br />
However the caveat is -<br />
Judicious patient selection<br />
Experienced surgeon / surgical team<br />
R0 resection<br />
Weitz et al., J Am Coll Surg 2007<br />
Tseng et al., Best Pract Res Clin Gastroenterol t 2006<br />
Capussotti et al. Arch Surg 2003<br />
Bachellier et al. Am J Surg 2001<br />
Roder et al. Am J Surg 2004<br />
Siriwardana HP, et al. Br J Surg 2006
Multivisceral <strong>Resections</strong><br />
<strong>Pancreatic</strong> <strong>Cancer</strong><br />
with enbloc<br />
Splenectomy <strong>and</strong><br />
Colectomy<br />
Transverse Colon<br />
Stapled Pancreas
A r<strong>and</strong>omized multicenter trial comparing<br />
resection <strong>and</strong> radiochemotherapy for<br />
resectable locally invasive pancreatic cancer<br />
Imamura et al., Surgery 2004 <strong>and</strong> *Surgery 2008<br />
Resection<br />
Radiochemotherapy<br />
Patients 20 22<br />
1-year survival 62% 32% p17 months 11 months p
Multivisceral <strong>Resections</strong><br />
Kleeff J et al., Ann Surg 2007
Multivisceral <strong>Resections</strong><br />
Technically feasible under elective conditions<br />
Higher surgical morbidity <strong>and</strong> mortality<br />
Longer ICU <strong>and</strong> hospital stay<br />
No real data concerning<br />
oncological outcomes<br />
No follow-up studies<br />
Sasson et al., J Gastrointest Surg 2002<br />
Shoup et al., J Gastrointest Surg 2003<br />
Nikfarjam et al. J Gastrointest Surg 2009
<strong>Pancreatic</strong> resection for M1 cancer<br />
Aortocaval LN metastasis<br />
<strong>Pancreatic</strong>oduodenectomy<br />
Liver metastasis<br />
Shrikh<strong>and</strong>e SV, Kleeff J et al., Ann. Surg. Oncol. 2006
<strong>Pancreatic</strong> resection for M1 cancer<br />
100<br />
l distribution<br />
function<br />
Surviva<br />
80<br />
60<br />
40<br />
20<br />
California <strong>Cancer</strong> Registry 1994-2000<br />
1-year survival rate: 61.5%<br />
Median survival : 13.8 months<br />
0<br />
0 6 12 18 24<br />
Months after resection<br />
30<br />
Shrikh<strong>and</strong>e SV, Kleeff J et al., Ann. Surg. Oncol. 2006
<strong>Pancreatic</strong> resection for M1 cancer<br />
%<br />
100<br />
l distribution<br />
function<br />
Surviva<br />
80<br />
60<br />
40<br />
20<br />
0<br />
P-value aue= 0.1445<br />
Liver metastases<br />
(n = 11)<br />
Lymph node metastases (n = 9)<br />
(aortocaval lymph nodes)<br />
Peritoneal / other metastases<br />
(n = 9)<br />
0 6 12 18 24 30<br />
Months after resection<br />
Shrikh<strong>and</strong>e SV, Kleeff J et al., Ann. Surg. Oncol. 2006
Conclusions..<br />
No difference in morbidity <strong>and</strong> mortality<br />
“Median survival of 27 months after<br />
interaortocaval lymph node dissection i is no<br />
different from that of other lymph nodes…”<br />
“..may be an option for intra-operatively<br />
discovered metastatic but locally<br />
resectable pancreatic cancer …”<br />
Shrikh<strong>and</strong>e SV, Kleeff J et al., Ann. Surg. Oncol. 2006
Michalski CW et al. Dig Surg 2008
Summary...<br />
Conventional lymphadenectomy (I)<br />
Improve LN yield by better surgery /<br />
pathology<br />
PPPD appears popular but cWhipple is not<br />
inferior (I)<br />
SMV / PV resection (R0) is justified in<br />
expert h<strong>and</strong>s (III) – to generate evidence<br />
is difficult. Does it improve survival?
Summary...<br />
Neoadjuvant approach in BR tumors<br />
will aided extended pancreatectomy<br />
Multivisceral resections – feasible but more<br />
data needs to be generated<br />
Resection in M1 disease – not justified<br />
currently, but RCT’s should be done (III)<br />
Evaluate outcomes of inter-aortocaval<br />
node resection
TATA MEMORIAL HOSPITAL<br />
www.pancreaticcancerindia.com