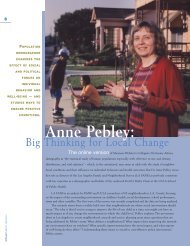
JUNE 2001 - UCLA School of Public Health
JUNE 2001 - UCLA School of Public Health
JUNE 2001 - UCLA School of Public Health
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Chiropractic Care Appears Slightly More Effective<br />
Than Medical Care for Treating Low-Back Pain<br />
PRELIMINARY FINDINGS FROM A <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong> study comparing<br />
the effectiveness <strong>of</strong> medical and chiropractic care for low-back pain indicate<br />
that chiropractic care may be slightly more effective, and physical therapy<br />
may be marginally more effective than medical care alone for reducing disability<br />
in some patients. Physical modalities such as heat therapy, electrical muscle<br />
stimulation, and ultrasound do not appear to yield additional clinical benefit for<br />
chiropractic patients, though perceived treatment effectiveness was somewhat<br />
greater in these groups.<br />
Low-back pain affects the majority <strong>of</strong> Americans at some point in their lives,<br />
and thousands every year become disabled because <strong>of</strong> chronic pain. Moreover,<br />
the rate <strong>of</strong> disabling back pain has increased steadily in recent years. “Although<br />
back-pain sufferers have many treatment options available, there is little scientific<br />
evidence showing which <strong>of</strong> the most common approaches is most effective,”<br />
says Dr. Eric Hurwitz, who conducted the study along with his colleague in the<br />
Department <strong>of</strong> Epidemiology, Dr. Hal Morgenstern, and collaborators from the<br />
<strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong> and <strong>School</strong> <strong>of</strong> Medicine.<br />
Hurwitz notes that back-pain sufferers may receive prescriptions for<br />
painkillers or muscle relaxants from conventional medical providers, or a referral<br />
to physical therapy. Still other patients may visit an alternative or complementary<br />
provider, such as a chiropractor or acupuncturist — indeed, more visits for back<br />
pain are to chiropractors than to any other type <strong>of</strong> health-care provider. The relative<br />
therapeutic benefits <strong>of</strong> each therapy, however, have not been known.<br />
From 1995 through 1998, a total <strong>of</strong> 681 low-back-pain patients were<br />
enrolled in the study and randomly assigned to one <strong>of</strong> four treatment protocols:<br />
medical care with and without physical therapy, and chiropractic care with and<br />
without physical modalities. Patients were followed up through 18 months.<br />
The researchers are now analyzing the data to address other objectives,<br />
including the cost effectiveness <strong>of</strong> low-back-pain care and the influence <strong>of</strong> occupational<br />
and psychosocial factors on low-back-pain prognosis. Patients’ satisfaction<br />
with care and their perceptions <strong>of</strong> treatment effectiveness and how these<br />
relate to clinical outcomes are also being investigated.<br />
Mental <strong>Health</strong>, Coordination <strong>of</strong> Care Reduce<br />
<strong>Health</strong> Costs for Elderly Veterans Group<br />
INTERDISCIPLINARY MENTAL HEALTH TREATMENT and care coordination<br />
can help to reduce health care costs for elderly veterans who have undiagnosed<br />
psychiatric conditions, according to a large randomized clinical trial involving<br />
more than 1,600 elderly veterans hospitalized in nine Veterans Administration<br />
sites across the country.<br />
Dr. Gerald F. Kominski and colleagues at the <strong>UCLA</strong> <strong>School</strong> <strong>of</strong> <strong>Public</strong> <strong>Health</strong><br />
evaluated data from a national clinical demonstration project with the VA known<br />
as the Unified Psychogeriatric Biopsychosocial Evaluation and Treatment<br />
(UPBEAT) program. The program, which took place from 1995 to 1998 and was<br />
headed by Dr. Lissy Jarvik <strong>of</strong> <strong>UCLA</strong>’s Neuropsychiatric Institute, provided individualized<br />
interdisciplinary mental health treatment and care coordination to elderly<br />
veterans with acute non-psychiatric conditions whose accompanying<br />
depression, anxiety, or alcohol abuse could result in overuse <strong>of</strong> inpatient services<br />
and underuse <strong>of</strong> outpatient services.<br />
continued on next page<br />
Low-back pain affects the majority <strong>of</strong><br />
Americans at some point in their lives,<br />
and thousands every year become<br />
disabled because <strong>of</strong> chronic pain.<br />
5<br />
research <strong>UCLA</strong>PUBLIC HEALTH