Download PDF - asian pharma press
Download PDF - asian pharma press
Download PDF - asian pharma press
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Asian J. Pharm. Res. 2012; Vol. 2: Issue 1, Pg 07-18<br />
[AJPRes.]<br />
ISSN- 2231–5683 (Print)<br />
www.<strong>asian</strong><strong>pharma</strong>online.org<br />
ISSN- 2231–5691 (Online) 0974-3618<br />
REVIEW ARTICLE<br />
Floating drug delivery system: An innovative acceptable approach in<br />
Gastro retentive drug delivery.<br />
Nirav Patel 1 , Nagesh C. 1 *, Chandrashekhar S. 1 , Patel Jinal 2 and Jani Devdatt 1<br />
1 Maratha Mandal’s College of Pharmacy, Belgaum-590016, Karanataka.<br />
2 A.P.M.C. college of Pharmaceutical Education and Research, Motipura, Himatnagar-383001, Gujarat.<br />
*Corresponding Author E-mail: nagesh_73@rediffmail.com<br />
ABSTRACT:<br />
Controlled release (CR) dosage forms have been extensively used to improve therapy with several important drugs.<br />
The recent developments of floating drug delivery systems (FDDS) including the physiological and formulation<br />
variables affecting gastric retention, approaches to design single-unit and multiple-unit floating systems, and their<br />
classification and formulation aspects are covered in detail. This review also summarizes the in vitro techniques, in<br />
vivo studies to evaluate the performance and application of floating systems. Floating dosage form can be prepared as<br />
tablets, capsules by adding suitable ingredients as well as by adding gas generating agent. In this review various<br />
techniques used in floating dosage forms along with current & recent developments of stomach specific floating drug<br />
delivery system for gastro retention are discussed.<br />
KEYWORDS: Floating drug delivery systems, mechanism, single unit, multiple units, evaluation Method.<br />
INTRODUCTION:<br />
Oral administration is the most versatile, convenient and<br />
commonly employed route of drug delivery for systemic<br />
action. Indeed, for controlled release system, oral route of<br />
administration has received the more attention and success<br />
because gastrointestinal physiology offers more flexibility<br />
in dosage form design than other routes. Development of a<br />
successful oral controlled release drug delivery dosage form<br />
requires an understanding of three aspects:<br />
(1) Gastrointestinal (GI) physiology<br />
(2) Physiochemical properties of the drug and<br />
(3) Dosage form characteristics 1, 2 .<br />
Gastric emptying of dosage forms is an extremely variable<br />
process and ability to prolong and control the emptying<br />
time is a valuable asset for dosage forms, which reside in<br />
the stomach for a longer period of time than conventional<br />
dosage forms 3 .<br />
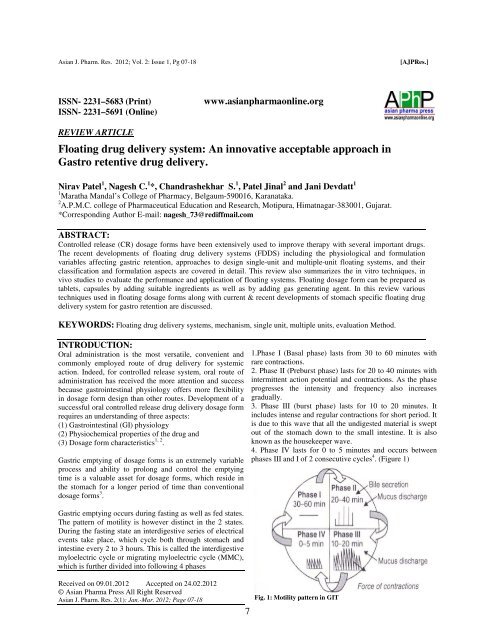
1.Phase I (Basal phase) lasts from 30 to 60 minutes with<br />
rare contractions.<br />
2. Phase II (Preburst phase) lasts for 20 to 40 minutes with<br />
intermittent action potential and contractions. As the phase<br />
progresses the intensity and frequency also increases<br />
gradually.<br />
3. Phase III (burst phase) lasts for 10 to 20 minutes. It<br />
includes intense and regular contractions for short period. It<br />
is due to this wave that all the undigested material is swept<br />
out of the stomach down to the small intestine. It is also<br />
known as the housekeeper wave.<br />
4. Phase IV lasts for 0 to 5 minutes and occurs between<br />
phases III and I of 2 consecutive cycles 4 . (Figure 1)<br />
Gastric emptying occurs during fasting as well as fed states.<br />
The pattern of motility is however distinct in the 2 states.<br />
During the fasting state an interdigestive series of electrical<br />
events take place, which cycle both through stomach and<br />
intestine every 2 to 3 hours. This is called the interdigestive<br />
myloelectric cycle or migrating myloelectric cycle (MMC),<br />
which is further divided into following 4 phases<br />
Received on 09.01.2012 Accepted on 24.02.2012<br />
© Asian Pharma Press All Right Reserved<br />
Asian J. Pharm. Res. 2(1): Jan.-Mar. 2012; Page 07-18<br />
7<br />
Fig. 1: Motility pattern in GIT
Asian J. Pharm. Res. 2012; Vol. 2: Issue 1, Pg 07-18<br />
Gastroretentive systems can remain in the gastric region for<br />
several hours and hence significantly prolong the gastric<br />
residence time of drugs. Prolonged gastric retention<br />
improves bioavailability, reduces drug waste, and improves<br />
solubility for drugs that are less soluble in a high pH<br />
environment. It has applications also for local drug delivery<br />
to the stomach and proximal small intestines. Slowed<br />
motility of the gastrointestinal tract by concomitant<br />
administration of drugs or <strong>pharma</strong>ceutical excipients also<br />
increase gastric retention of drug 5 .<br />
These efforts resulted in GRDFs that were designed, in<br />
large part, based on the following approaches. (Figure 2)<br />
1. Low density form of the DF that causes buoyancy in<br />
gastric fluid 6, 7<br />
2. High density DF that is retained in the bottom of the<br />
stomach 8, 9<br />
3. Bioadhesion to stomach mucosa 10<br />
4. Expansion by swelling or unfolding to a large size<br />
which limits passage of dosage form through the<br />
pyloric sphincter 11<br />
[AJPRes.]<br />
FACTORS AFFECTING GASTRIC RESIDENCE<br />
TIME OF FDDS<br />
a) Formulation factors<br />
Size of tablets<br />
Retention of floating dosage forms in stomach depends on<br />
the size of tablets. Small tablets are emptied from the<br />
stomach during the digestive phase, but large ones are<br />
expelled during the house keeping waves 4 .<br />
Floating and nonfloating capsules of 3 different sizes<br />
having a diameter of 4.8 mm (small units), 7.5 mm<br />
(medium units), and 9.9 mm (large units), were formulated<br />
and analyzed for their different properties. It was found that<br />
floating dosage units remained buoyant regardless of their<br />
sizes on the gastric contents throughout their residence in<br />
the gastrointestinal tract, while the nonfloating dosage units<br />
sank and remained in the lower part of the stomach.<br />
Floating units away from the gastroduodenal junction were<br />
protected from the peristaltic waves during digestive phase<br />
while the nonfloating forms stayed close to the pylorus and<br />
were subjected to propelling and retropelling waves of the<br />
digestive phase 15 .<br />
Density of tablets<br />
Density is the main factor affecting the gastric residence<br />
time of dosage form. A buoyant dosage form having a<br />
density less than that of the gastric fluids floats, since it is<br />
away from the pyloric sphincter, the dosage unit is retained<br />
in the stomach for a prolonged period. A density of less<br />
than 1.0g/ml i.e. less than that of gastric contents has been<br />
reported. However, the floating force kinetics of such<br />
dosage form has shown that the bulk density of a dosage<br />
form is not the most appropriate parameter for describing its<br />
buoyancy capabilities 16 .<br />
Shape of tablets<br />
The shape of dosage form is one of the factors that affect its<br />
gastric residence time. Six shapes (ring tetrahedron,<br />
cloverleaf, string, pellet, and disk) were screened in vivo for<br />
their gastric retention potential. The tetrahedron (each leg<br />
2cm long) rings (3.6 cm in diameter) exhibited nearly 100%<br />
retention at 24 hr 17 .<br />
Fig. 2: Different approaches of gastric retention<br />
Novel oral controlled dosage form that is retained in the<br />
stomach for prolonged and predictable period is of major<br />
interest among academic and industrial research groups.<br />
One of the most feasible approaches for achieving<br />
prolonged and predictable drug delivery profile in the GI<br />
tract is to control gastric residence time (GRT). Dosage<br />
form with prolonged GRT or gastro-retentive dosage form<br />
(GRDF) provides an important therapeutic option 12 . Various<br />
approaches for preparation of gastroretentive drug delivery<br />
system include floating systems, swellable and expandable<br />
systems, high density systems, bioadhesive systems, altered<br />
shape systems, gel forming solution or suspension system<br />
and sachet systems. Among these, the floating dosage form<br />
has been used most commonly 13, 14 .<br />
Viscosity grade of polymer<br />
Drug release and floating properties of FDDS are greatly<br />
affected by viscosity of polymers and their interaction. Low<br />
viscosity polymers (e.g., HPMC K100 LV) were found to<br />
be more beneficial than high viscosity polymers (e.g.,<br />
HPMC K4M) in improving floating properties. In addition,<br />
a decrease in the release rate was observed with an increase<br />
in polymer viscosity 18 .<br />
b) Idiosyncratic factors<br />
Gender<br />
Women have slower gastric emptying time than do men.<br />
Mean ambulatory GRT in meals (3.4±0.4 hours) is less<br />
compared with their age and racematched female<br />
counterparts (4.6±1.2 hours), regardless of the weight,<br />
height and body surface 19 .<br />
8
Asian J. Pharm. Res. 2012; Vol. 2: Issue 1, Pg 07-18<br />
Age<br />
Low gastric emptying time is observed in elderly than do in<br />
younger subjects. Intrasubject and intersubject variations<br />
also are observed in gastric and intestinal transit time.<br />
Elderly people, especially those over 70 years have a<br />
significantly longer GRT 20 .<br />
Posture<br />
i) Upright position<br />
An upright position protects floating forms against<br />
postprandial emptying because the floating form remains<br />
above the gastric contents irrespective of its size 20 . Floating<br />
dosage forms show prolonged and more reproducible GRTs<br />
while the conventional dosage form sink to the lower part<br />
of the distal stomach from where they are expelled through<br />
the pylorus by antral peristaltic movements 21 .<br />
ii) Supine position<br />
This position offers no reliable protection against early and<br />
erratic emptying. In supine subjects large dosage forms<br />
(both conventional and floating) experience prolonged<br />
retention. The gastric retention of floating forms appear to<br />
remain buoyant anywhere between the lesser and greater<br />
curvature of the stomach. On moving distally, these units<br />
may be swept away by the peristaltic movements that<br />
propel the gastric contents towards the pylorus, leading to<br />
significant reduction in GRT compared with upright<br />
subjects 22 .<br />
Concomitant intake of drugs<br />
Drugs such as prokinetic agents (e.g., metoclopramide and<br />
cisapride), anti Cholinergics (e.g., atropine or<br />
propantheline), opiates (e.g., codeine) may affect the<br />
performance of FDDS. The coadministration of GImotility<br />
decreasing drugs can increase gastric emptying time 22 .<br />
Feeding regimen<br />
Gastric residence time increases in the presence of food,<br />
leading to increased drug dissolution of the dosage form at<br />
the most favorable site of absorption. A GRT of 410 h has<br />
been reported after a meal of fats and proteins 23 .<br />
[AJPRes.]<br />
FLOATING DRUG DELIVERY SYSTEM:<br />
Mechanism of floating systems:<br />
Various attempts have been made to retain the dosage form<br />
in the stomach as a way of increasing the retention time.<br />
These attempts include introducing floating dosage forms<br />
(gas-generating systems and swelling or expanding<br />
systems), mucoadhesive systems, high-density systems,<br />
modified shape systems, gastric-emptying delaying devices<br />
and co-administration of gastric emptying delaying drugs.<br />
Among these, the floating dosage forms are the most<br />
commonly used. Floating drug delivery systems (FDDS)<br />
have a bulk density less than gastric fluids and so remain<br />
buoyant in the stomach without affecting the gastric<br />
emptying rate for a prolonged period of time. While the<br />
system is floating on the gastric contents (given in the Fig.<br />
3A), the drug is released slowly at the desired rate from the<br />
system. After release of drug, the residual system is<br />
eliminated from the stomach. This results in an increased<br />
GRT and a better control of the fluctuations in plasma drug<br />
concentration. However, besides a minimal gastric content<br />
needed to allow the proper achievement of the buoyancy<br />
retention effect, a minimal level of floating force (F) is also<br />
required to maintain the buoyancy of the dosage form on<br />
the surface of the meal. To measure the floating force<br />
kinetics, a novel apparatus for determination of resultant<br />
weight has been reported in the literature. The apparatus<br />
operates by measuring continuously the force equivalent to<br />
F (as a function of time) that is required to maintain a<br />
submerged object. The object floats better if F is on the<br />
higher positive side (Fig. 3B). This apparatus helps in<br />
optimizing FDDS with respect to stability and sustainability<br />
of floating forces produced in order to prevent any<br />
unforeseeable variations in intragastric buoyancy 12 .<br />
F = Fbuoyancy – Fgravity = (Df – Ds) g v<br />
Where, F = total vertical force,<br />
Df = fluid density,<br />
Ds = object density,<br />
v = volume and<br />
g = acceleration due to gravity 24 .<br />
Fig. 3. Mechanism of floating systems.<br />
9
Asian J. Pharm. Res. 2012; Vol. 2: Issue 1, Pg 07-18<br />
CLASSIFICATION:<br />
Floating Oral Drug Delivery System (FDDS) are retained in<br />
the stomach and are useful for drugs that are poorly soluble<br />
or unstable in intestinal fluids. Floating drug delivery<br />
system (FDDS) have a bulk density less than gastric fluids<br />
and so remain buoyant in the stomach without affecting the<br />
gastric emptying rate for a prolonged period of time 13 .<br />
While the system is floating on the gastric contents, the<br />
drug is released slowly at the desired rate from the system<br />
(Figure 4). After release of drug, the residual system is<br />
emptied from the stomach. This results in an increased GRT<br />
and a better control of fluctuations in plasma drug<br />
concentration.<br />
Fig. 4: Intragastric residence positions of floating unit.<br />
[AJPRes.]<br />
A. Single unit floating system<br />
a) Noneffervescent system<br />
Hydrodyanamic balanced systems<br />
Sheth and Tossounian first designated this<br />
‘hydrodynamically balanced system’. Such a system<br />
contains drug with gel-forming hydrocolloids meant to<br />
remain buoyant on the stomach content. This prolongs GRT<br />
and maximizes the amount of drug that reaches its<br />
absorption sites in the solution form for ready absorption<br />
(Figure 5). This system incorporates a high level of one or<br />
more gel-forming highly soluble cellulose type<br />
hydrocolloid, e.g., hydroxypropylcellulose, hydoxyethyl<br />
cellulose, hydroxypropyl methyl cellulose (HPMC),<br />
polysaccharides and matrix-forming polymer such as<br />
polycarbophil, polyacrylate and polystyrene. On coming in<br />
contact with gastric fluid, the hydrocolloid in the system<br />
hydrates and forms a colloid gel barrier around its surface 25 .<br />
Yang et al developed a swellable asymmetric triple-layer<br />
tablet with floating ability to prolong the gastric residence<br />
time of triple drug regimen (tetracycline, metronidazole,<br />
and clarithromycin) in Helicobacter pylori–associated<br />
peptic ulcers using hydroxy propyl methyl cellulose<br />
(HPMC) and poly (ethylene oxide) (PEO) as the rate<br />
controlling polymeric membrane excipients. Bismuth salt<br />
was included in one of the outer layers for instant release.<br />
The floatation was accomplished by incorporating a gas<br />
generating layer consisting of sodium bicarbonate: calcium<br />
carbonate (1:2 ratios) along with the polymers 26 . (Figure 6).<br />
Fig.5: Hydrodynamically balanced system (HBS). The gelatinous polymer barrier formation results from hydrophilic polymer swelling.<br />
Drug is released by diffusion and erosion of the gel barrier.<br />
Fig. 6: Schematic presentation of working of a triple-layer system. (A) Initial configuration of triple-layer tablet. (B) On contact with the<br />
dissolution medium the bismuth layer rapidly dissolves and matrix starts swelling. (C) Tablet swells and erodes. (D) and (E) Tablet<br />
erodes completely.<br />
10
Asian J. Pharm. Res. 2012; Vol. 2: Issue 1, Pg 07-18<br />
[AJPRes.]<br />
Floating chamber<br />
Fluid- filled floating chamber which includes incorporation<br />
of a gas-filled floatation chamber into a microporous<br />
component that houses a drug reservoir. Apertures or<br />
openings are present along the top and bottom walls<br />
through which the gastrointestinal tract fluid enters to<br />
dissolve the drug. The other two walls in contact with the<br />
fluid are sealed so that the undissolved drug remains<br />
therein. The fluid present could be air, under partial vacuum<br />
or any other suitable gas, liquid, or solid having an<br />
appropriate specific gravity and an inert behaviour. The<br />
device is of swallowable size, remains a float within the<br />
stomach for a prolonged time, and after the complete<br />
release the shell disintegrates, passes off to the intestine,<br />
and is eliminated 27 . (Figure 7)<br />
b) Effervescent Floating Dosage Forms Gas Generating<br />
Systems:<br />
Floating systems containing effervescent components<br />
These are matrix type of systems prepared with the help of<br />
swellable polymers such as methylcellulose and chitosan<br />
and various effervescent compounds, e.g., sodium<br />
bicarbonate, tartaric acid, and citric acid. They are<br />
formulated in such a way that when in contact with the<br />
acidic gastric contents, co 2 is liberated and gets entrapped in<br />
swollen hydrocolloids, which provide buoyancy to the<br />
dosage forms. In vitro, the lag time before the unit floats is<br />
Asian J. Pharm. Res. 2012; Vol. 2: Issue 1, Pg 07-18<br />
[AJPRes.]<br />
Programmable drug delivery<br />
A programmable, controlled release drug delivery system<br />
has been developed in the form of a non-digestible oral<br />
capsule (containing drug in a slowly eroding matrix for<br />
controlled release) was designed to utilize an automatically<br />
operated geometric obstruction that keeps the device<br />
floating in the stomach and prevents it from passing through<br />
the remainder of the GIT. Different viscosity grades of<br />
hydroxypropyl-methyl-cellulose were employed as model<br />
eroding matrices. The duration during which the device<br />
could maintain its geometric obstruction (caused by a builtin<br />
triggering ballooning system) was dependent on the<br />
erosion rates of the incorporated polymers (the capsule inhosed<br />
core matrix). After complete core matrix erosion, the<br />
ballooning system is automatically flattened off so that the<br />
device retains its normal capsule size to be eliminated by<br />
passing through the GIT 32 .<br />
B. Multiple unit floating system<br />
a) Non-effervescent Systems:<br />
Alginate beads<br />
Alginates have received much attention in the development<br />
of multiple unit systems. Alginates are nontoxic,<br />
biodegradable linear copolymers composed of L-glucuronic<br />
and L-mannuronic acid residues. Multiple unit floating<br />
dosage forms have been developed from freezedried<br />
calcium alginate. Spherical beads of approximately 2.5 mm<br />
in diameter can be prepared by dropping a sodium alginate<br />
solution in to aqueous solutions of calcium chloride,<br />
causing precipitation of calcium alginate. The beads are<br />
then separated snap and frozen in liquid nitrogen, and freeze<br />
dried at -40°C for 24 hours, leading to the formation of<br />
porous system, which can maintain a floating force over 12<br />
hours 33, 34 . A multiple unit system can be developed<br />
comprising of calcium alginate core and calcium<br />
alginate/PVA membrane, both separated by an air<br />
compartment. Air compartment provides bouncy to beads.<br />
In presence of water, the PVA leaches out and increases the<br />
membrane permeability, maintaining the integrity of the air<br />
compartment. Increase in molecular weight and<br />
concentration of PVA, resulted in enhancement of the<br />
floating properties of the system 35 .<br />
(A)<br />
(B)<br />
Fig. 9: (A) Multiple-unit oral floating drug delivery system. (B)<br />
Working principle of effervescent floating drug delivery system.<br />
C) Hollow Microspheres:<br />
Hollow microspheres are considered as one of the most<br />
promising buoyant systems, as they possess the unique<br />
advantages of multiple unit systems as well as better<br />
floating properties, because of central hollow space inside<br />
the microsphere(Figure 10). The general techniques<br />
involved in their preparation include simple solvent<br />
evaporation, and solvent diffusion and evaporation.<br />
Polycarbonate, Eudragit S, cellulose acetate, calcium<br />
alginate, agar and low methoxylated pectin are commonly<br />
used as polymers in preparation of hollow microsphere.<br />
Buoyancy and drug release are dependent on quantity of<br />
polymer, the plasticizer–polymer ratio and the solvent<br />
used 7, 37, 38 .<br />
b) Effervescent systems:<br />
Floating pills<br />
Ichikawa et al developed a new multiple type of floating<br />
dosage system composed of effervescent layers and<br />
swellable membrane layers coated on sustained release<br />
pills. The inner layer of effervescent agents containing<br />
sodium bicarbonate and tartaric acid was divided into 2<br />
sublayers to avoid direct contact between the 2 agents. This<br />
is surrounded by a swellable polymer membrane containing<br />
polyvinyl acetate and purified shellac. When this system<br />
was immersed in the buffer at 37ºC, produce swollen pills<br />
(like balloons) with a density less than 1.0 g/mL due to<br />
incorporation of co 2 36 .(Figure 9)<br />
12<br />
Fig. 10: Micro balloons
Asian J. Pharm. Res. 2012; Vol. 2: Issue 1, Pg 07-18<br />
[AJPRes.]<br />
D. Raft forming system<br />
Raft-forming systems<br />
On contact with Gastric fluid A gel-forming solution (e.g.<br />
sodium alginate solution containing carbonates or<br />
bicarbonates) swells and forms a viscous cohesive gel<br />
containing entrapped CO 2 bubbles. This forms raft layer on<br />
top of gastric fluid which releases drug slowly in stomach.<br />
Such formulation typically contains antacids such as<br />
aluminium hydroxide or calcium carbonate to reduce gastric<br />
acidity. They are often used for gastro esophageal reflux<br />
treatment as with Liquid Gaviscon (GlaxoSmithKline) 39 .<br />
(Figure 11)<br />
Fig. 11: Barrier formed by a raft-forming system<br />
Drugs Used In the Formulations of Stomach Specific<br />
Floating Dosage Forms<br />
1. Floating microspheres – Aspirin, Griseofulvin,<br />
pnitroaniline, Ibuprofen, Ketoprofen 40 , Piroxicam,<br />
Verapamil HCl, Cholestyramine, Theophylline,<br />
Nifedipine, Nicardipine, Dipyridamol, Tranilast 41 and<br />
Terfinadine 42<br />
2. Floating granules - Diclofenac sodium, Indomethacin<br />
and Prednisolone<br />
1. Films 43 – Cinnarizine, Albendazole<br />
1. Floating tablets and Pills - Isosorbide mononitrate 37 ,<br />
Diltiazem 44 , Acetylsalicylic acid 45 , Piretanide 46 ,<br />
Sotalol 47 , carbamazepine, Furosamide 48 ,<br />
Pentoxyphylline 49 , captopril 50 , Nimodipine 51 ,<br />
Acetaminophen 52 , Amoxicillin trihydrate 53 , Diazepam 54<br />
2. Floating Capsules –Diazepam 55 , Ursodeoxycholic<br />
acid 49 , Verapamil HCl 56 , Nicardipine 57 , Furosemide 58 ,<br />
Misoprostal 4<br />
Table 1. Marketed Preparations of Floating Drug Delivery<br />
Systems:<br />
S.<br />
no.<br />
Product Active Ingredient Reference<br />
No.<br />
1 Madopar Levodopa and benserzide 59<br />
2 Valrelease Diazepam 25<br />
3 Topalkan Aluminum magnesium<br />
60<br />
antacid<br />
4 Almagate Antacid 61<br />
flatcoat<br />
5 Liquid<br />
gavison<br />
Alginic acid and sodium<br />
bicarbonate<br />
62<br />
13<br />
Application:<br />
Floating drug delivery offers several applications for drugs<br />
having poor bioavailability because of the narrow<br />
absorption window in the upper part of the gastrointestinal<br />
tract. It retains the dosage form at the site of absorption and<br />
thus enhances the bioavailability. These are summarized as<br />
follows.<br />
1. Sustained Drug Delivery<br />
HBS systems can remain in the stomach for long periods<br />
and hence can release the drug over a prolonged period of<br />
time. The problem of short gastric residence time<br />
encountered with an oral CR formulation hence can be<br />
overcome with these systems. These systems have a bulk<br />
density of G1 as a result of which they can float on the<br />
gastric contents. These systems are relatively large in size<br />
and passing from the pyloric opening is prohibited.<br />
Recently sustained release floating capsules of nicardipine<br />
hydrochloride were developed and were evaluated in vivo.<br />
The formulation compared with commercially available<br />
MICARD capsules using rabbits. Plasma concentration time<br />
curves showed a longer duration for administration (16<br />
hours) in the sustained release floating capsules as<br />
compared with conventional MICARD capsules (8 hours)<br />
57 . Similarly a comparative study between the Madopar<br />
HBS and Madopar standard formulation was done and it<br />
was shown that the drug was released up to 8 hours in vitro<br />
in the former case and the release was essentially complete<br />
in less than 30 minutes in the latter case 59 .<br />
2. Site-Specific Drug Delivery<br />
These systems are particularly advantageous for drugs that<br />
are specifically absorbed from stomach or the proximal part<br />
of the small intestine, e.g. riboflavin and furosemide.<br />
Furosemide is primarily absorbed from the stomach<br />
followed by the duodenum. It has been reported that a<br />
monolithic floating dosage form with prolonged gastric<br />
residence time was developed and the bioavailability was<br />
increased. AUC obtained with the floating tablets was<br />
approximately 1.8 times those of conventional furosemide<br />
tablets 58 . A bilayer-floating capsule was developed for local<br />
delivery of misoprostol, which is a synthetic analog of<br />
prostaglandin E1 used as a protectant of gastric ulcers<br />
caused by administration of NSAIDs. By targeting slow<br />
delivery of misoprostol to the stomach, desired therapeutic<br />
levels could be achieved and drug waste could be reduced 4 .<br />
3. Absorption Enhancement:<br />
Drugs that have poor bioavailability because of sitespecific<br />
absorption from the upper part of the gastrointestinal tract<br />
are potential candidates to be formulated as floating drug<br />
delivery systems, thereby maximizing their absorption.<br />
E.g. A significantly increase in the bioavailability of<br />
floating dosage forms(42.9%) could be achieved as<br />
compared with commercially available LASIX tablets<br />
(33.4%) and enteric coated LASIX-long product (29.5%) 57 .
Asian J. Pharm. Res. 2012; Vol. 2: Issue 1, Pg 07-18<br />
[AJPRes.]<br />
EVALUATION OF GASTRORETENTIVE<br />
DOSAGEFORM<br />
A) IN-VITRO EVALUATION 62 , 63<br />
i) Floating systems<br />
a) Buoyancy Lag Time<br />
It is determined in order to assess the time taken by the<br />
dosage form to float on the top of the dissolution medium,<br />
after it is placed in the medium. These parameters can be<br />
measured as a part of the dissolution test 64 .<br />
b) Floating Time<br />
Test for buoyancy is usually performed in SGF-Simulated<br />
Gastric Fluid maintained at 37 0 C. The time for which the<br />
dosage form continuously floats on the dissolution media is<br />
termed as floating time 65 .<br />
c) Specific Gravity / Density<br />
Density can be determined by the displacement method<br />
using Benzene as displacement medium.<br />
d) Resultant Weight<br />
Now we know that bulk density and floating time are the<br />
main parameters for describing buoyancy. But only single<br />
determination of density is not sufficient to describe the<br />
buoyancy because density changes with change in resultant<br />
weight as a function of time.<br />
For example a matrix tablet with bicarbonate and matrixing<br />
polymer floats initially by gas generation and entrapment<br />
but after some time, some drug is released and<br />
simultaneously some outer part of matrixing polymer may<br />
erode out leading to change in resultant weight of dosage<br />
form. The magnitude and direction of force/resultant weight<br />
(up or down) is corresponding to its buoyancy force<br />
(Fbuoy) and gravity force (Fgrav) acting on dosage form<br />
F = F buoy - F grav F = D f g V – D s g V F = (D f – D s ) g V<br />
F = (D f – M/V) g V<br />
Where,<br />
F = resultant weight of object<br />
D f = Density of Fluid<br />
D S = Density of Solid object<br />
g = Gravitational force<br />
M = Mass of dosage form<br />
V = Volume of dosage form<br />
So when Ds, density of dosage form is lower, F force is<br />
positive gives buoyancy and when it is Ds is higher, F will<br />
negative shows sinking 21 .<br />
ii) Swelling systems<br />
a) Swelling Index<br />
After immersion of swelling dosage form into SGF at 37 0 C,<br />
dosage form is removed out at regular interval and<br />
dimensional changes are measured in terms of increase in<br />
tablet thickness / diameter with time.<br />
b) Water Uptake<br />
It is an indirect measurement of swelling property of<br />
swellable matrix. Here dosage form is removed out at<br />
regular interval and weight changes are determined with<br />
respect to time. So it is also termed as Weight Gain.<br />
Water uptake = WU = (Wt – Wo) * 100 / Wo<br />
Where, Wt = weight of dosage form at time t<br />
Wo = initial weight of dosage form<br />
B) IN-VITRO DISSOLUTION TESTS<br />
A. In vitro dissolution test is generally done by using USP<br />
apparatus with paddle and GRDDS is placed normally as<br />
for other conventional tablets. But sometimes as the vessel<br />
is large and paddles are at bottom, there is much lesser<br />
paddle force acts on floating dosage form which generally<br />
floats on surface. As floating dosage form not rotates may<br />
not give proper result and also not reproducible results.<br />
Similar problem occur with swellable dosage form, as they<br />
are hydrogel may stick to surface of vessel or paddle and<br />
gives irreproducible results. In order to prevent such<br />
problems, various types of modification in dissolution<br />
assembly made are as follows.<br />
B. To prevent sticking at vessel or paddle and to improve<br />
movement of dosage form, method suggested is to keep<br />
paddle at surface and not too deep inside dissolution<br />
medium.<br />
14
Asian J. Pharm. Res. 2012; Vol. 2: Issue 1, Pg 07-18<br />
[AJPRes.]<br />
Fig. 12 dissolution of floating dosage form<br />
C. Floating unit can be made fully submerged, by attaching<br />
some small, loose, non- reacting material, such as few turns<br />
of wire helix, around dosage form. However this method<br />
can inhibit three dimensional swelling of some dosage form<br />
and also affects drug release.<br />
D. Other modification is to make floating unit fully<br />
submerged under ring or mesh assembly and paddle is just<br />
over ring that gives better force for movement of unit.<br />
E. Other method suggests placing dosage form between 2<br />
ring/meshes.<br />
F. In previous methods unit have very small area, which<br />
can inhibit 3D swelling of swellable units, another method<br />
suggest the change in dissolution vessel that is indented at<br />
some above place from bottom and mesh is place on<br />
indented protrusions, this gives more area for dosage form.<br />
G. Inspite of the various modifications done to get the<br />
reproducible results, none of them showed co-relation with<br />
the in-vivo conditions. So a novel dissolution test apparatus<br />
with modification of Rossett-Rice test Apparatus was<br />
proposed 65, 67 .<br />
C) IN-VIVO EVALUATION<br />
a) Radiology<br />
X-ray is widely used for examination of internal body<br />
systems. Barium Sulphate is widely used Radio Opaque<br />
Marker. So, BaSO 4 is incorporated inside dosage form and<br />
X-ray images are taken at various intervals to view GR.<br />
b) Scintigraphy<br />
Similar to X-ray, emitting materials are incorporated into<br />
dosage form and then images are taken by scintigraphy.<br />
Widely used emitting material is 99 Tc.<br />
c) Gastroscopy<br />
Gastroscopy is peroral endoscopy used with fiber optics or<br />
video systems. Gastroscopy is used to inspect visually the<br />
effect of prolongation in stomach. It can also give the<br />
detailed evaluation of GRDDS.<br />
d) Magnetic Marker Monitoring<br />
In this technique, dosage form is magnetically marked with<br />
incorporating iron powder inside, and images can be taken<br />
by very sensitive bio-magnetic measurement equipment.<br />
Advantage of this method is that it is radiation less and so<br />
not hazardous.<br />
e) Ultrasonography<br />
Used sometimes, not used generally because it is not<br />
traceable at intestine.<br />
f) 13 C Octanoic Acid Breath Test<br />
13 C Octanoic acid is incorporated into GRDDS. In stomach<br />
due to chemical reaction, octanoic acid liberates CO 2 gas<br />
which comes out in breath. The important Carbon atom<br />
which will come in CO 2 is replaced with 13 C isotope. So<br />
time up to which 13 CO 2 gas is observed in breath can be<br />
considered as gastric retention time of dosage form. As the<br />
dosage form moves to intestine, there is no reaction and no<br />
CO 2 release. So this method is cheaper than other.<br />
ADVANTAGES:<br />
1. Enhanced bioavailability the bioavailability of some<br />
drugs (e.g. riboflavin and levodopa) CR-GRDF is<br />
significantly enhanced in comparison to administration of<br />
non- GRDF CR polymeric formulations 68 .<br />
2. Enhanced first-pass biotransformation when the drug<br />
is presented to the metabolic enzymes (cytochrome P-450,<br />
in particular CYP-3A4) in a sustained manner, the<br />
presystemic metabolism of the tested compound may be<br />
considerably increased rather than by a bolus input 69 .<br />
3. Sustained drug delivery/reduced frequency of dosing<br />
the drugs having short biological half life, a sustained and<br />
slow input from FDDS may result in a flip-flop<br />
<strong>pharma</strong>cokinetics and it reduces the dose frequency. This<br />
feature is associated with improved patient compliance and<br />
thus improves the therapy 69 .<br />
4. Targeted therapy for local ailments in the upper GIT<br />
the prolonged and sustained administration of the drug from<br />
15
Asian J. Pharm. Res. 2012; Vol. 2: Issue 1, Pg 07-18<br />
[AJPRes.]<br />
FDDS to the stomach may be useful for local therapy in the<br />
stomach.<br />
5. Reduced fluctuations of drug concentration the<br />
fluctuations in plasma drug concentration are minimized,<br />
and concentration-dependent adverse effects that are<br />
associated with peak concentrations can be prevented. This<br />
feature is of special importance for drugs with a narrow<br />
therapeutic index 70 .<br />
6. Improved receptor activation selectivity FDDS reduces<br />
the drug concentration fluctuation that makes it possible to<br />
obtain certain selectivity in the elicited <strong>pharma</strong>cological<br />
effect of drugs that activate different types of receptors at<br />
different concentrations 69 .<br />
7. Reduced counter-activity of the body slow release of<br />
the drug into the body minimizes the counter activity<br />
leading to higher drug efficiency.<br />
8. Extended time over critical (effective) concentration<br />
the sustained mode of administration enables extension of<br />
the time over a critical concentration and thus enhances the<br />
<strong>pharma</strong>cological effects and improves the clinical<br />
outcomes.<br />
9. Minimized adverse activity at the colon Retention of<br />
the drug in GRDF at stomach minimizes the amount of<br />
drugs that reaches the colon and hence prevents the<br />
degradation of drug that degraded in the colon.<br />
10. Site specific drug delivery a floating dosage form is a<br />
widely accepted approach especially for drugs which have<br />
limited absorption sites in upper small intestine.<br />
71, 72<br />
Limitations/Disadvantages<br />
1. These systems require a high level of fluid in the<br />
stomach for drug delivery tom float and work<br />
efficiently-coat, water.<br />
2. Not suitable for drugs that have solubility or stability<br />
problem in GIT.<br />
3. Drugs such as Nifedipine which is well absorbed along<br />
the entire GIT and which undergoes first pass<br />
metabolism, may not be desirable.<br />
4. Drugs which are irritant to Gastric mucosa are also not<br />
desirable or suitable.<br />
5. The drug substances that are unstable in the acidic<br />
environment of the stomach are not suitable candidates<br />
to be incorporated in the systems.<br />
6. The dosage form should be administered with a full<br />
glass of water (200-250 ml).<br />
These systems do not offer significant advantages over the<br />
conventional dosage forms for drugs, which are absorbed<br />
throughout the gastrointestinal tract.<br />
CONCLUSION:<br />
Drug absorption in the gastrointestinal tract is a highly<br />
variable procedure and prolonging gastric retention of the<br />
dosage form extends the time for drug absorption. FDDS<br />
16<br />
promises to be a potential approach for gastric retention.<br />
The FDDS proves advantageous for drugs that are absorbed<br />
primarily in the upper segments of GI tract, i.e., the<br />
stomach, duodenum, and jejunum when compared to the<br />
conventional dosage form. Due to the complexity of<br />
<strong>pharma</strong>cokinetic and <strong>pharma</strong>codynamic parameters, in vivo<br />
studies are required to establish the optimal dosage form for<br />
a specific drug. For a certain drug, interplay of its<br />
<strong>pharma</strong>cokinetic and <strong>pharma</strong>codynamic parameters will<br />
determine the effectiveness and benefits of the CRGRDF<br />
compared to the other dosage forms.<br />
REFERENCES:<br />
1. Robinson J.R, Lee V.H.L. Controlled drug delivery:<br />
fundamentals and applications. 2 nd ed.<br />
1. Marcel Dekker Inc; NY 1987.<br />
2. Chien Y.W. Novel drug delivery systems. 2 nd ed. Marcel Dekker<br />
Inc; NY 1992.<br />
3. 3.Hirtz J. The git absorption of drugs in man: a review of current<br />
concepts and methods of investigation. Br J Clin Pharmacol.<br />
1985;19:77-83.<br />
4. Oth M, Franze M, Timmermans J, Moes A. The bilayerfloating<br />
capsule: a stomach directed drug delivery system for misoprostol.<br />
Pharm Res. 1992;9:298302.<br />
5. Groning R, Heun G. Oral dosage forms with controlled<br />
gastrointestinal transit. Drug Dev Ind Pharm. 1984;10:527-539.<br />
6. Deshpande A.A, Shah N.H, Rhodes C.T, Malick W.<br />
Development of a novel controlled release system for gastric<br />
retention. Pharm Res. 1997;14:815-819.<br />
7. Kawashinia Y, Niwa T, Takcuchi H, Hino T, Itoh Y. Hallow<br />
microspheres for use as a floating controlled drug delivery system<br />
in the stomach. J.Pharm. Sci. 1992;81(2):135-140.<br />
8. Bechgaard H, Ladefoged K. Distribution of pellets in the<br />
gastrointestinal tract: The influence on transit time exerted by<br />
density or diameter of pellets. J.Pharm. Pharmacol. 1978;30:690-<br />
692.<br />
9. Davis S.S, Stockwell S.F, Taylor M.J, Hardy J.G, Whelley D.R.<br />
The effect on density on the gastric emptying of Single and<br />
multiple-unit dosage form. Pharm Res. 1986;3:208-213.<br />
10. Ponchel G, Irache J.M. Specific and nonspecific bioadhesive<br />
particulate system for Oral delivery to the gastrointestinal tract.<br />
Adv.Drug.Del.Rev. 1998;34:191-219.<br />
11. Klausner EA, Lavy E, Friedman M, Hoffman A. Expandable<br />
gastroretentive dosage forms. J Control Release. 2003;90:143-<br />
162.<br />
12. S. Garg, S. Sharma. Gastroretentive drug delivery system.<br />
Business Briefing: Pharmatech. 2003;160-166.<br />
13. Singh BN, Kim KH. Floating drug delivery systems: an approach<br />
to oral controlled drug delivery via gastric retention. J Control<br />
Release. 2000; 63:235-59.<br />
14. Kim C.J. Dosage Form Design, Lancaster: Technomic Pub; Basel<br />
2000.<br />
15. Timmermans J, Gasnsbeka BV, Moes A. Accessing by<br />
gammascintigraphy the in vivo buoyancy of dosage form having<br />
known size and floating force profiles as a function of time.<br />
Pharm Tech. 1989;1:4251.<br />
16. Gergogiannis YS, Rekkas DM, Dallos PP, Chailis NH. Floating<br />
and swelling characteristics of various excipients used in<br />
controlled release technology. Drug Dev Ind Pharm. 1993;19:<br />
10611081.<br />
17. Cargill R, Cadwell LJ, Engle K, Fix JA, Porter PA, Gardner CR.<br />
Controlled gastric emptying: I. Effects of physical properties on<br />
gastric residence times of non disintegrating geometric shapes in<br />
beagle dogs. Pharm Res. 1988;5:533536.<br />
18. Li S, Lin S, Daggy BP, Mirchandani HL, Chien YW. Effect of<br />
HPMC and Carbopol on the release and floating properties of<br />
gastric floating drug delivery system using factorial design. Int J<br />
Pharm. 2003;253:1322.
Asian J. Pharm. Res. 2012; Vol. 2: Issue 1, Pg 07-18<br />
19. Patel GM. Floating drug delivery system: An innovative<br />
approach to prolong gastric retention. www.<strong>pharma</strong>info.net;2007.<br />
20. Mojaverian P, Vlasses PH, Kellner PE, Rocci ML. Effects of<br />
gender, posture, and age on gastric residence time of indigestible<br />
solid: <strong>pharma</strong>ceutical considerations. Pharm Res. 1988;10: 639<br />
664.<br />
21. Timmermans J, Moes AJ. Factors controlling the buoyancy and<br />
gastric retention capabilities of floating matrix capsules: new data<br />
for reconsidering the controversy. J Pharm Sci. 1994;83:1824.<br />
22. Chawla G, Gupta P, Koradia V, Bansal AK. Gastroretention: A<br />
Means to address regional variability in intestinal drug<br />
absorption. Pharm Tech. 2003;27:250268.<br />
23. MullerLissner SA, Blum AL. The effect of specific gravity and<br />
eating on gastric emptying of slowrelease capsules. New Engl J<br />
Med. 1981;304:13651366.<br />
24. A. Rubinstein, D. R. Friend. Specific delivery to the<br />
gastrointestinal tract, in: A. J. Domb (Ed.), polymeric sitespecific<br />
Pharmacotherapy. Wiley, Chichester. 1994.282-283.<br />
25. Seth P.R, Tossounian J. The hydrodynamically balanced system,<br />
a novel drug delivery system for oral use. Drug Dev. Ind Pharm.<br />
1984;10:313-339.<br />
26. Yang L, Esharghi J, Fassihi R. A new intra gastric delivery<br />
system for the treatment of helicobacter pylori associated gastric<br />
ulcers: in vitro evaluation. J. Cont. Rel. 1999;57:215- 222.<br />
27. Joseph N.H, Laxmi S, Jayakrishnan A. A floating type oral<br />
dosage form for piroxicam based on hollow microspheres: in<br />
vitro and in vivo evaluation in rabbits. J. Cont. Rel. 2002;79:71-<br />
79.<br />
28. Krogel I, Bodmeier R. Floating or pulsatile drug delivery systems<br />
based on coated effervescent cores. Int. J. Pharm. 1999;187:175-<br />
184.<br />
29. Mitra, S.B.W, MN. Sustained release oral medicinal delivery<br />
device. Minnesota Mining and Manufacturing Company (St.<br />
Paul, MN). United States;1984.<br />
30. Ingani H.M, Timmermans J, Moes, A.J. Conception and in vivo<br />
investigation of peroral sustained release floating dosage forms<br />
with enhanced gastrointestinal transit. Int. J. Pharm. 1987;35:157-<br />
164.<br />
31. Atyabi F,Sharma H.L, Mohammad H. AH, Fell J. T. Controlled<br />
drug release from coated floating ion exchange resin beads.<br />
Journal of Controlled Release.1996;42:25-28.<br />
32. Bashaw, J.D.P.A., CA), Zaffaroni, Alejandro (Atherton, CA),<br />
Michaels, Alan S. (Atherton, CA), 1976. Self-monitored device<br />
for releasing agent at functional rate. ALZA Corporation (Palo<br />
Alto, CA), United States.<br />
33. Sakr F.M. A programmable drug delivery system for oral<br />
administration. International Journal of Pharmaceutics.<br />
1999;184(1):131-139.<br />
34. Vyas S.P, Khar R.K. Targetted and controlled Drug Delivery<br />
Novel carrier system. 1 st ed. New Delhi: CBS Publishers and<br />
distributors; 2002.196- 217.<br />
35. Jain N.K. Progress in Controlled and Novel Drug Delivery<br />
Systems. 1 st ed. New Delhi: CBS Publishers and Distributors;<br />
2004.84-85.<br />
36. Iannuccelli V, Coppi G, Bernabei M.T, Cameroni R. Air<br />
compartment multiple-unit system for prolonged gastric<br />
residence. Part I. Formulation study. Int.J.Pharm. 1998;174:47-<br />
54.<br />
37. Ichikawa M, Watanabe S, Miyake Y. A new multiple unit oral<br />
floating dosage system. I: Prepration and in vitro evaluation of<br />
floating and sustained-release kinetics. J Pharm Sci.<br />
1991;80:1062-1066.<br />
38. Sato Y, Kawashima Y, Takeuchi H, Yamamoto H. In vivo<br />
evaluation of riboflavin containing microballoons for floating<br />
controlled drug delivery system in healthy human volunteers. J.<br />
Cont. Rel. 2003;93:39- 47.<br />
39. Washington N. Investigation into the barrier action of an alginate<br />
gastric reflux sup<strong>press</strong>ant, Liquid Gaviscon, Drug Investig.<br />
1987;2:23-30.<br />
[AJPRes.]<br />
40. El-Kamel A.H, Sokar M.S, Algamal S.S, Naggar V.F.<br />
Preparation and evaluation of ketoprofen floating oral drug<br />
delivery system. Int. J. Pharm. 2001;220:13-21.<br />
41. Kawashima Y, Niwa T, Takeuchi H, Hino T, ItoY. Preparation of<br />
multiple unit hollow microspheres (microballoons) with acrylic<br />
resins containing tranilast and their drugrelease characteristics (in<br />
vivo). J. Cont. Rel. 1991;16:279-290.<br />
42. Jayanthi G, Jayaswal S.B, Srivastava A.K. Formulation and<br />
evaluation of terfenadine microballoons for oral controlled<br />
release. Pharmazie. 1995;50:769-770.<br />
43. Harrigan RM. Drug delivery device for preventing contact of<br />
undissolved drug with the stomach lining, US Patent 4, 055, 178,<br />
October 25, 1977.<br />
44. Gu T.H. Pharmacokinetics and <strong>pharma</strong>codynamics of diltiazem<br />
floating tablets. Chung Kao Yao Li Hsuesh Pao. 1992;13:527-<br />
531.<br />
45. Sheth P.R., Tossounian J.L., Novel sustained release tablet<br />
formulations. U.S.patent 4167558. September 11, 1979.<br />
46. Rouge N, Cole E.T, Doelker E, Buri P. Buoyancy and drug<br />
release patterns of floating mini tablets containing piretanide and<br />
atenolol as model drugs. Pharm. Dev. Technol. 1998;3:73-84.<br />
47. Cheuh H.R, Zia H, Rhodes C.T. Optimization of Sotalol floating<br />
and bioadhesive extended release tablet formulation. Drug Dev.<br />
Ind. Pharm. 1995;21:1725-1747.<br />
48. Ozdemir N, Ordu S, Ozkan Y. Studies of floating dosage forms<br />
of furosemide: in vitro and in vivo evaluation of bilayer tablet<br />
formulation. Drug Dev Ind Pharm. 2000;26(8):857-866.<br />
49. Simoni P, Cerre C, Cipolla A. Bioavailabilty study of a new<br />
sinking, enteric coated ursodeoxycholic acid formulation.<br />
Pharmacol. Res. 1995;31:115-119.<br />
50. Nur A.O, Zhang J.S. Captopril floating and/or bioadhesive<br />
tablets: design and release kinetics. Drug Dev Ind Pharm.<br />
2000;26:965-969.<br />
51. Wu W, Zhou Q, Zhang H.B, Ma G.D, Fu C.D. Studies on<br />
nimodipine sustained release tablet capable of floating on gastric<br />
fluids with prolonged gastric resident time. Yao Xue Xue Bao.<br />
1997;32:786-790.<br />
52. Phuapradit W. Influence of Tablet Buoyancy on Oral Absorption<br />
of Sustained Release Acetaminophen Matrix Tablets<br />
[dissertation]. Jamaica, NY, St John’s University;1989.<br />
53. Hilton A.K, Deasy P.B. In vitro and in vivo evaluation of an oral<br />
sustained release floating dosage form of amoxycillin trihydrate.<br />
Int J Pharm. 1992;86:79-88.<br />
54. Gustafson J.H, Weissman L, Weinfeld R.T. Clinical<br />
bioavailability evaluation of a controlled release formulation of<br />
diazepam. J. Pharmacokinet. Biopharm. 1981;9:679-691.<br />
55. Gansbeke B.V, Timmermans J, Schoutens A, Moes A.J.<br />
Intragastric positioning of two concurrently ingested<br />
<strong>pharma</strong>ceutical matrix dosage forms. Nucl Med Biol.<br />
1991;18:711-718.<br />
56. Chen G.L, Hao W.H. In vitro performance of floating sustained<br />
release capsules of verapamil. Drug Dev Ind<br />
Pharm.1998;24:1067-1072.<br />
57. Moursy N.M, Afifi N.N, Ghorab D.M, El-Saharty Y. Formulation<br />
and evaluation of sustained release floating capsules of<br />
Nicardipine hydrochloride. Pharmazie. 2003;58:38-43.<br />
58. Menon A, Ritschel W.A, Sakr A. Development and evaluation of<br />
a monolithic floating dosage form for furosemide. J Pharm Sci.<br />
1994;83:239-245.<br />
59. Erni W, Held K. The hydrodynamically balanced system: a novel<br />
principle of controlled drug release. Eur Neurol. 1987;27:215-<br />
275.<br />
60. Degtiareva H, Bogdanov A, Kahtib Z. The use of third generation<br />
antacid preparations for the treatment of patients with<br />
nonulcerous dyspeosia and peptic ulcer complicated by reflux<br />
esophagus [in Chinese]. Liakrs’ ka sprava. 1994;5-6:119-122.<br />
61. Fabregas JL, Claramunt J, Cucala J, Pous R, Siles A. In vitro<br />
testing of an antacid formulation with prolonged gastric residence<br />
time (Almagate flot coat). Drug Dev Ind Pharm. 1994;20:1199-<br />
1212.<br />
17
Asian J. Pharm. Res. 2012; Vol. 2: Issue 1, Pg 07-18<br />
[AJPRes.]<br />
62. Washington N, Washington C, Wilson CG, Davis SS. What is<br />
liquid Graviscon? A comparison of four international<br />
formulations. Int J Pharm. 1986;34:105-109.<br />
63. Desai S, Bolton S. A floating controlled release system: Invitro –<br />
Invivo evaluation. Pharm. Res. 1993;10:13211325.<br />
64. Patel, V.F, Patel, N.M, Yeole P.G. Studies on formulation and<br />
evaluation Ranitidine floating tablets. Ind. J. Pharm. Sci.<br />
2005;67(6):703709.<br />
65. Arrora S, Ali J, Khar RK, Baboota S. Floatng drug delivery<br />
systems: A review. AAPS Pharm Sci Tech. 2005;6(3):372-90.<br />
66. Burns SJ, Corness D, Hay G. Development and validation of an<br />
in vitro dissolution method for a floating dosage form with<br />
biphasic release characteristics. Int. J. Pharm. 1995;121:37-34.<br />
67. Pillay V, Fassihi R. Evaluation and comparision of dissolution<br />
data derived from different modified release dosage forms: an<br />
alternative method. J Control Release. 1998;55:45-55.<br />
68. Hoffman A. Pharmacodynamic aspects of sustained release<br />
preparations. Adv. Drug Deliv. Rev. 1998;33:185-199.<br />
69. Garg R, Gupta GD. Progress in Controlled Gastroretentive<br />
Delivery Systems. Tropical Journal of Pharmaceutical Research.<br />
2008;7 (3):1055-1066.<br />
70. Hoffman, A, Stepensky D. Pharmacodynamic aspects of modes<br />
of drug administration for optimization of drug therapy. Crit.<br />
Rev. Ther. Drug Carr. Syst. 1999;16(6):571-639.<br />
71. Shivkumar HG, Vishakante Gwdaand D, Pramod Kumar TM.<br />
Indian J Pharm Educ. 2004;38(4):172-179.<br />
72. Sangekar S. Evaluation of effect of food and specific gravity of<br />
the tablets on gastric retention time. Int.J.Pharm. 1987;35(3):34-<br />
53.<br />
18