July - Saint Clare's Hospital
July - Saint Clare's Hospital
July - Saint Clare's Hospital
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
VOLUME 3 ISSUE 4<br />
JULY - AUGUST 2012<br />
2012 LONDON OLYMPICS: NURSES PARTICIPATE IN<br />
OPENING CEREMONIES<br />
PRACTICE COMPETENCE AND EXCELLENCE DIMENSION<br />
DEBBIE’S NURSING NOTES<br />
KUDOS<br />
WELCOME TO<br />
ROVING NURSE REPORTER<br />
MUST READ<br />
FAREWELL<br />
DAISY NURSES<br />
PRAYERS FOR AN IV<br />
GET THE SCOOP ABOUT MENTAL HEALTH<br />
NURSING NEWS<br />
NDNQI<br />
UNDERSTANDING BULLYING IN THE WORKPLACE; PART 2,<br />
THE EFFECT ON THE NURSING TEAM<br />
EDUCATION FOR PATIENTS AND FAMILIES RELATED TO<br />
INFECTION PREVENTION<br />
FAMILY HEALTH, THE NEUMAN MODEL<br />
NEXIVA<br />
NEWLY ISSUED WARNING ON ONDANSETRON (ZOFRAN ® )<br />
DEAR ALLYSON<br />
CULTURAL COMPETENCE DAY 2012 PHOTOS<br />
1<br />
2<br />
3<br />
3<br />
4<br />
4<br />
5<br />
5<br />
5<br />
7<br />
7<br />
9<br />
10<br />
10<br />
11<br />
12<br />
12<br />
13<br />
14<br />
15<br />
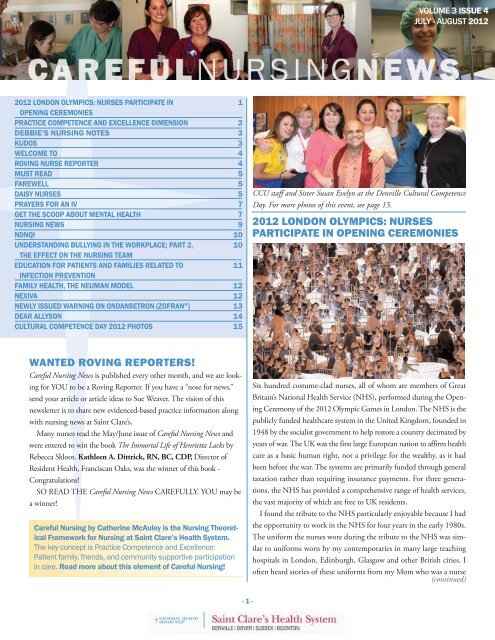
CCU staff and Sister Susan Evelyn at the Denville Cultural Competence<br />
Day. For more photos of this event, see page 15.<br />
2012 LONDON OLYMPICS: NURSES<br />
PARTICIPATE IN OPENING CEREMONIES<br />
WANTED ROVING REPORTERS!<br />
Careful Nursing News is published every other month, and we are looking<br />
for YOU to be a Roving Reporter. If you have a “nose for news,”<br />
send your article or article ideas to Sue Weaver. The vision of this<br />
newsletter is to share new evidenced-based practice information along<br />
with nursing news at <strong>Saint</strong> Clare’s.<br />
Many nurses read the May/June issue of Careful Nursing News and<br />
were entered to win the book The Immortal Life of Henrietta Lacks by<br />
Rebecca Skloot. Kathleen A. Dittrick, RN, BC, CDP, Director of<br />
Resident Health, Franciscan Oaks, was the winner of this book -<br />
Congratulations!<br />
SO READ THE Careful Nursing News CAREFULLY. YOU may be<br />
a winner!<br />
Careful Nursing by Catherine McAuley is the Nursing Theoretical<br />
Framework for Nursing at <strong>Saint</strong> Clare’s Health System.<br />
The key concept is Practice Competence and Excellence:<br />
Patient family, friends, and community supportive participation<br />
in care. Read more about this element of Careful Nursing!<br />
Six hundred costume-clad nurses, all of whom are members of Great<br />
Britain’s National Health Service (NHS), performed during the Opening<br />
Ceremony of the 2012 Olympic Games in London. The NHS is the<br />
publicly funded healthcare system in the United Kingdom, founded in<br />
1948 by the socialist government to help restore a country decimated by<br />
years of war. The UK was the first large European nation to affirm health<br />
care as a basic human right, not a privilege for the wealthy, as it had<br />
been before the war. The systems are primarily funded through general<br />
taxation rather than requiring insurance payments. For three generations,<br />
the NHS has provided a comprehensive range of health services,<br />
the vast majority of which are free to UK residents.<br />
I found the tribute to the NHS particularly enjoyable because I had<br />
the opportunity to work in the NHS for four years in the early 1980s.<br />
The uniform the nurses wore during the tribute to the NHS was similar<br />
to uniforms worn by my contemporaries in many large teaching<br />
hospitals in London, Edinburgh, Glasgow and other British cities. I<br />
often heard stories of these uniforms from my Mom who was a nurse<br />
(continued)<br />
- 1 -
VOLUME 3 ISSUE 4<br />
“This concept encompasses the need to encourage and support patient’s<br />
family members, friends and community services participation<br />
in patients’ care, according to patients’ wishes and this is possible and<br />
appropriate. In planning, implementing and evaluating patients’ care,<br />
assessment is made of needs for social support and resources. Selected<br />
family members, friends or community members are helped to dein<br />
England during World War II. If you look closely at the picture,<br />
you will see the nurses are wearing aprons and starched cuffs. English<br />
hospitals were mainly staffed by nursing students from their schools of<br />
nursing. Student nurses and single staff nurses lived in the “Nurses<br />
Home.” Before coming down to breakfast, the nurse would don her<br />
formal uniform with long sleeves and removable starched cuffs, and<br />
starched cap. After breakfast, she put on her blue cape lined in red and<br />
walked to the hospital. Upon arrival to the ward she was working on,<br />
she would take off the starched cuffs, roll her sleeves up neatly, apply<br />
her elastic cover to her rolled up sleeve, and put on her apron. The<br />
hospital ward was divided into male or female each containing 30<br />
beds; 15 on each side of the ward with curtains dividing each bed<br />
space. When baths were given, bandages changed, toileting rounds<br />
done and all the patients were sitting up in bed looking as neat as a pin,<br />
the staff nurses and sisters would remove their apron, pull their sleeves<br />
down and replace their starched cuffs before the Consultants or senior<br />
physicians would come to do rounds with the Senior Sister. The patients<br />
and the junior staff knew there was no talking while the<br />
Consultants were on the ward. When the Consultants left the ward,<br />
the nurses would once again roll up their sleeves, put their aprons on<br />
and get back to work. The last change for the nurses came at 3 p.m.,<br />
back to the formal uniform, when the afternoon tea cart arrived.<br />
I worked in the city of Manchester at<br />
Withenshaw <strong>Hospital</strong> in the Thoracic Intensive<br />
Therapy Unit (ITU). My uniform<br />
was the NHS uniform of the 80s. Staff<br />
nurses wore a pale blue and white-checked<br />
dress, similar to a shirt dress, buttoned<br />
down the front with short sleeves and a<br />
two-inch thick material belt with a wide<br />
buckle. Tan stockings, black tie shoes with<br />
a 1” stacked heel, a white starched cap,<br />
and a fob watch were also part of the staff<br />
nurse uniform. A fob watch pins to your uniform with the watch face<br />
upside down so that when you look down you can easily read it. Nurses<br />
did not wear wrist watches for infection control reasons, you can’t wash<br />
the watch between patients. I still used a fob watch when I came to <strong>Saint</strong><br />
Clare’s in 2002.<br />
When I became a “Sister,” which is comparable to our shift supervisor,<br />
my uniform changed to a navy and white-checked dress with a<br />
thick material belt with buckle. I also wore a cape when I went to<br />
lunch and dinner. The uniform had changed at my hospital since the<br />
1940s but the 30 bed wards and the rule of silence during the Con-<br />
- 2 -<br />
sultant rounds with the Senior Sister remained the same. Of course,<br />
the chatty American Sister didn’t know about the silence rule and “got<br />
a talking to” after the Senior Thoracic Surgeon, finished rounds and<br />
left the step-down ward. I returned to the U.S. in October 1985, after<br />
four years with the wonderful nurses in the UK, who have a special<br />
place in the heart’s of the British people. The nurses are kind, generous<br />
and helpful. No wonder the British people call them ”angels of<br />
mercy.”<br />
Ann McLoughlin, BSN, RN, CMSRN<br />
Admission Nurse<br />
PRACTICE COMPETENCE AND<br />
EXCELLENCE DIMENSION:<br />
PATIENT FAMILY, FRIENDS, AND COMMUNITY<br />
SUPPORTIVE PARTICIPATION IN CARE<br />
<strong>Saint</strong> Clare’s Health System Nursing has adopted Careful Nursing as<br />
its nursing theory for practice. Careful Nursing has FOUR Nursing<br />
Dimensions and 18 accompanying Key Practice Concepts. In the<br />
practice competence and excellence dimension, patient family, friends,<br />
and community supportive participation in care is one of the eight<br />
interrelated concepts of this dimension and the concept of this issue<br />
of the newsletter.<br />
I. Therapeutic Milieu<br />
II. Practice Competence and Excellence<br />
1. Great tenderness in all things<br />
2. ‘Perfect’ skill fostering safety and comfort<br />
3. Watching and assessment<br />
4. Clinical reasoning and decision-making<br />
5. Patient engagement in self-care<br />
6. Nursing diagnoses, outcomes, interventions<br />
7.Patient family, friends, and community supportive<br />
participation in care<br />
8. Health education<br />
III. Management of Practice and Influence in Health System<br />
IV. Professional Authority<br />
(continued on next page)
VOLUME 3 ISSUE 4<br />
DEBBIE’S NURSING NOTES<br />
As our new Chief Nursing Officer, Debbie Regen<br />
values and recognizes the importance of our patients’<br />
and nurses’ family and friends, the theme<br />
of this issue of the newsletter. Since Debbie is<br />
spending time with her family, she sends her regards<br />
and this special poem by Maya Angelou:<br />
Human Family<br />
I note the obvious differences<br />
in the human family.<br />
Some of us are serious,<br />
some thrive on comedy.<br />
Some declare their lives are lived<br />
as true profundity,<br />
and others claim they really live<br />
the real reality.<br />
and laugh and moan in Guinea,<br />
and thrive on Spanish shores.<br />
We seek success in Finland,<br />
are born and die in Maine.<br />
In minor ways we differ,<br />
in major we're the same.<br />
I note the obvious differences<br />
between each sort and type,<br />
but we are more alike, my friends,<br />
than we are unalike.<br />
We are more alike, my friends,<br />
than we are unalike.<br />
We are more alike, my friends,<br />
than we are unalike.<br />
The variety of our skin tones<br />
can confuse, bemuse, delight,<br />
brown and pink and beige and purple,<br />
tan and blue and white.<br />
I've sailed upon the seven seas<br />
and stopped in every land,<br />
I've seen the wonders of the world<br />
not yet one common man.<br />
I know ten thousand women<br />
called Jane and Mary Jane,<br />
but I've not seen any two<br />
who really were the same.<br />
Mirror twins are different<br />
although their features jibe,<br />
and lovers think quite different thoughts<br />
while lying side by side.<br />
(continued from previous page)<br />
velop care-giving, assistive and supportive roles as necessary.”<br />
From the beginning of my nursing career in the surgical ICU,<br />
I valued the role of the patient’s family and friends. I learned that<br />
having the family at the bedside was a benefit because at least I<br />
knew the patient would not fall out of bed when they were there.<br />
I also encouraged the family to bring in pictures of the patient<br />
and music for the patient.<br />
Meehan, T. C. (2011). Interim notes on the Theory of Careful Nursing.<br />
Sue Weaver, MSN, RN, CRNI, NEA-BC<br />
Shift Administrator<br />
KUDOS<br />
Congratulations to Andrea Sousa, MSN, RN, WHNP-BC, Urban<br />
2, Staff nurse, who graduated in January from Rutgers, the State University,<br />
Newark, with an MSN in Women's Health and passed the certification<br />
board exam in June.<br />
We love and lose in China,<br />
we weep on England's moors,<br />
- 3 -
VOLUME 3 ISSUE 4<br />
WELCOME TO...<br />
Gifty Adjin-Tettey, RN, RRC Shift Supervisor<br />
Sarah Albanese, RN, RRC Staff nurse<br />
Joan Aversa, RN, CCIS Staff nurse<br />
Paige Ballard, RN, ED Staff nurse<br />
Robin Blatzheim, BSN, RN, SCTU nurse<br />
Lenore Bodnar, RN, Maternal-Child Staff nurse<br />
Allison Brown Jones, RN, ACIS Staff nurse<br />
Angela Castellano, RN, ACDU Staff nurse<br />
Maura Donohue, RN, PES Staff nurse<br />
Heredia Filomena, RN, CCIS Staff nurse<br />
Julie Flores, RN, RRC Staff nurse<br />
Patricia Grzybowski, RN, PICU Staff nurse<br />
Fatme Keten, RN, PCU Staff nurse<br />
Hugo Nenuz, RN, OR Staff nurse<br />
Gladys Seeham, RN, ED Staff nurse<br />
Jenna Vogel, RN, ACIS Staff nurse<br />
Pamela Wohlgemuth, RN, PACU Staff nurse<br />
ROVING NURSE REPORTER<br />
The Roving Nurse Reporter asked, “Do you have any specific<br />
examples of how patient’s family members, and friends helped or<br />
participated in patients’ care?”<br />
Katie Pierson, MSN, RN-BC, ONC,<br />
Nurse Navigator, Orthopedics, states, “I<br />
consistently see family and friend involvement<br />
when it comes to our total joint replacement<br />
patients. As with maternity, we<br />
call our family and friends ‘coaches.’ They<br />
receive the ‘coach’ button at the pre-op<br />
class, come to the hospital and learn how to correctly move the patient<br />
with physical therapy, and then ensure that they provide care for them<br />
once they return home after their hospital stay.”<br />
Cristina Kowalski, RN, Case Management Specialist, states, “In the<br />
role as a case manager, I have a lot of contact<br />
with patients and their family members during<br />
their hospital stay. The majority of families are<br />
willing and able to assist their loved ones and<br />
seem very engaged in their plan of care. My<br />
role is to help the patient reach their personal<br />
goals, maintain their autonomy, and make sure they are involved in<br />
every stage of their care based on the individual’s needs and preferences.<br />
I feel this type of approach helps the patient and their family<br />
members to have more control over their own treatments.<br />
This can also foster the families to be more empathetic and understanding<br />
of the patient’s needs and desires, as well as identifying barriers<br />
to a safe discharge, such as the patient cannot manage their<br />
medications any longer. But most significantly, sometimes patients<br />
seem to lose the desire to participate in their care and this is where I<br />
see many families pull together to assist their loved one, all while still<br />
including the patient in their care.”<br />
Daniela Carrera, RN, Urban 2 Shift Supervisor<br />
and Dorothy Skordinsky, BSN,<br />
RN, Urban 2 staff nurse explain that when<br />
they had a young patient from Canada,<br />
they contacted her mother in Canada and<br />
encouraged her to come to help her daughter.<br />
While they waited for the mother’s arrival,<br />
the staff had the boyfriend and his<br />
family to provide support for this young patient. When the mother arrived<br />
she spent 24 hours a day with her daughter and was able to get<br />
her daughter to eat by recommending specific foods and encouraged<br />
her to walk.<br />
Catherine Jacinto, BSN, RN, 4B staff nurse says,<br />
“It is important to include the family in postoperative<br />
education to enhance compliance after<br />
discharge.”<br />
From the CCU perspective: Hildi Schneider,<br />
RN, CCRN, CCU Staff nurse, states,<br />
“It is important for the family to provide<br />
emotional and spiritual support for the patient<br />
and to assist in patient care as appropriate.”<br />
While Marjorie Yagumyum, BSN,<br />
RN, CCRN, CCU Staff nurse explains, “We<br />
do have some situations where a family member can help and is willing<br />
to feed the patient and even do some passive range of motion.”<br />
- 4 -<br />
(continued)
VOLUME 3 ISSUE 4<br />
MUST READ<br />
They Called Them Angels:<br />
American Military Nurses of World War II<br />
by Kathi Jackson (Jackson, K. (2000). Thy Called Them<br />
Angels: American Military Nurses of World War II. Westport,<br />
CT: Greenwood Publishing Group.)<br />
Step back in time and read about the experience<br />
of the American military nurse of<br />
World War II. These nurses volunteered to<br />
serve their country and were sent all over the<br />
world to care for American soldiers. During<br />
World War II, hospitals were brought to<br />
the patients, so the nurses took care of the<br />
soldiers on the front lines. These military<br />
nurses quickly learned to care for patients<br />
with horrific war injuries, burns, amputations,<br />
along with many medical problems such as respiratory diseases,<br />
malaria, typhus, and infectious hepatitis. It was interesting to read<br />
about things uncommon to nurses in the 21st century such as jungle<br />
rot and trench foot along with the Wangentsien apparatus. The nurses<br />
even had to deal with pressure sores, caused when the wounded soldiers<br />
laid for several days on canvas cots, under rough wet blankets,<br />
waiting to be evacuated.<br />
These military nurses adapted and adjusted to military life, varied<br />
climates, and the uniform. The best part of the uniform for these<br />
adaptable nurses was the helmet, because it could be used for everything,<br />
such as a hat, bucket, washtub, bathtub, basket, and chair.<br />
These World War II nurses functioned in roles as nurse anesthetist,<br />
nurse practitioner and even primary care provider. Today, we have<br />
these varied nursing roles and this is the legacy of the World War II<br />
nurses.<br />
Several essays written by nurses are also included in this book. In<br />
one essay, nurse Frances Slanger writes a letter to Stars and Stripes<br />
about the GIs and how impressed she has been caring for these brave<br />
American soldiers. The GI’s responded to her letter and are so grateful<br />
for the caring and compassion of the American nurses.<br />
Finally, this book reminds us of why we are nurses; to help those in<br />
need and to do our best at a job worth doing.<br />
Sue Weaver, MSN, RN, CRNI, NEA-BC<br />
Shift Administrator<br />
FAREWELL<br />
We are saddened to report that Terry O’Dell,<br />
RN, Respiratory Rehabilitation Center (RRC)<br />
in Dover, passed away suddenly on Thursday,<br />
<strong>July</strong> 5, 2012. Terry began working at <strong>Saint</strong><br />
Clare’s in June 1997 and spent most of her<br />
years working in The Dwelling Place and RRC.<br />
She started as a Certified Nurse Assistant while<br />
attending William Paterson University for her BSN. Terry was kind,<br />
caring and generous to a fault. She was dedicated to her patients and<br />
colleagues so much so that RRC was her top priority. According to<br />
Terry’s son, Sean, because his mother loved being an RRC nurse at<br />
<strong>Saint</strong> Clare’s, she never considered it work. Terry will be missed greatly.<br />
She will be forever in our hearts.<br />
Love your friends in RRC<br />
DAISY NURSES<br />
Congratulations to the new DAISY nurses.<br />
April 2012 - Deborah Ginard, RN<br />
April 2012 - Jacqueline Lezcano,<br />
RN, Emergency Department<br />
Pictured (l-r): Suellyn Ellerbe, MN,<br />
RN, NEA-BC; Jan Bednar, BSN,<br />
MS, RN, CEN, Executive Director<br />
of Nursing; Jacqueline Lezcano,<br />
RN; and Cheryl Beers, DHA, RN,<br />
NE-BC, CALA, Director, Nursing<br />
Operations.<br />
Pictured (l-r): Suellyn Ellerbe,<br />
MN, RN, NEA-BC; Jan Bednar,<br />
BSN, MS, RN, CEN, Executive<br />
Director of Nursing, Tess<br />
Medina, BSN, MAS, RN, Administrative<br />
Director; Director<br />
Debbie Ginard, RN; and Mary<br />
Ann Piro, BSN, RN, CARN,<br />
Operations Manager, Adult Crisis<br />
Intervention Services.<br />
- 5 -<br />
(continued)
VOLUME 3 ISSUE 4<br />
Jacqueline Lezcano is a DAISY nurse. A patient wrote: “This past<br />
Sunday, I had the unfortunate experience of dealing with dyspnea.<br />
Given the circumstances, I had my brother bring me to the Denville<br />
ED. Considering this was the first type of such an episode for me I was<br />
very nervous. My ED nurse that day was Jacqueline Lezcano. Upon<br />
my arrival into my room, she greeted me in a way in which I immediately<br />
felt comfortable under her care. This “moment of truth” set<br />
the tone for what would be the transformation of an uncomfortable<br />
circumstance – me arriving nervous – to a controlled situation in<br />
which I fully trusted the forces of care that were being seamlessly implemented<br />
around me. Throughout my stay, Jacqueline was extremely<br />
attentive, clinically knowledgeable, and absolutely role modeled our<br />
system values in her delivery of care. Given that the disposition of my<br />
role rarely awards me the opportunity to witness the great clinical work<br />
going on here, it was a rare – albeit unfortunate – opportunity for me<br />
to dive into the clinical side of the business. As I departed from our<br />
Denville ED, I felt so proud that I work for a system which selects<br />
and develops nurses like Jacqueline. She is truly a role model for the<br />
type of behavior our values hope to inherently create in all our organizations.”<br />
May 2012<br />
Pictured (l-r): Suellyn Ellerbe,<br />
MN, RN, NEA-BC, with the<br />
May 2012 Daisy Nurses, Debbie<br />
Miller, RN, Jeanette Pascale, RN,<br />
CEN, CPEN, and Maureen<br />
O'Connell, BA, RN.<br />
May 2012 Debbie Miller, RN, 4 WEST<br />
Debbie Miller is a DAISY nurse. A patient’s family wrote: “I want<br />
you to be aware of the most wonderful and compassionate care my<br />
mother received from one of your nurses on 4 West during the final<br />
four days of her life. My mom volunteered at <strong>Saint</strong> Clare’s for 33 years<br />
helping patients, their families, and visitors as if they were her own<br />
family members. It was so fitting therefore, that she was blessed to<br />
have Debbie on duty for those final days. Debbie comforted not only<br />
my mom, but comforted my 92-year-old dad and myself, by going<br />
beyond her daily duties. She kept close watch on my mom attending<br />
to her bed sheets, washing and cleaning her many times during the<br />
day, combing her hair, and keeping her comfortable and warm. She<br />
called for a complimentary lunch cart for my dad and me so we didn't<br />
have to leave my mom’s side. When it was imminent my mom was<br />
- 6 -<br />
passing, Debbie hugged us and stayed with us helping through the<br />
initial grieving process, and waited with us until the funeral director<br />
came to mom’s room. Debbie should be exalted for her professionalism<br />
and for being a true model of our core values. My dad also wishes<br />
to thank her, and everyone at <strong>Saint</strong> Clare’s for the care his wife received<br />
from the hometown hospital that they depended on since 1945.<br />
As we both look back with sadness, we count our blessings that someone<br />
like Debbie was here for us when we needed them the most!”<br />
May 2012 Maureen O’Connell, BA, RN, Maternal Child Department<br />
Maureen O’Connell is a DAISY nurse. A few months ago, the Maternity<br />
Unit was especially busy and the nurses needed extra help, so<br />
they called “Mo,” and of course she said she would help. Upon her<br />
arrival, she learned that one particular patient was to be discharged.<br />
Mo went to the nursing office and asked the nursing supervisor what<br />
she had to do to prevent this baby from being potentially discharged<br />
to an unsafe environment. When Mo speaks, people listen. A hospital<br />
hold was placed on the baby, and DYFS (Division of Youth and<br />
Family Services) was again involved. Eventually DYFS determined it<br />
would be safe for the baby to be discharged to this mother. However,<br />
because of Mo’s due diligence during the discharge process, reevaluations<br />
were done and home visits were arranged to provide reassessment<br />
of the situation. The baby went with the mother and DYFS was<br />
to provide home support to the mother and baby. Later it was learned,<br />
the mother never followed up with her own care and DYFS took custody<br />
of the baby. Mo’s intuition about the safety of the baby was first<br />
and foremost in her mind.<br />
Other examples of Mo’s DAISY attributes include: A new father<br />
was also celebrating his birthday as well as the birth of his new baby,<br />
so Mo arranged for a birthday cake for this family. She also went out<br />
of her way after work to pick up formula for a family that had a specific<br />
request.<br />
May 2012 Jeanette Pascale, RN, CEN, CPEN, Emergency Department<br />
There are so many examples of how Jeanette is a DAISY nurse. One<br />
Sunday night there was a young patient on the Pediatric unit who<br />
needed an IV and was considered a “hard stick.” Nurses tried to insert<br />
the IV but were unsuccessful. Jeanette was asked if she could assist.<br />
The child’s parents were more than a little anxious, but they relaxed<br />
with Jeanette’s arrival and her expertise in starting the IV. Plus, Jeanette<br />
did even more. The parents could communicate in English but it was<br />
tough. Since Jeanette is bilingual, they could talk with her in Spanish<br />
and her calming reassurance made a world of a difference for them.<br />
(continued)
VOLUME 3 ISSUE 4<br />
On another weekend evening, an L&D nurse asked, “What was the<br />
name of that ED nurse? She was great!” L&D had a patient ready to<br />
deliver at any moment. At just the same time, another new L&D patient<br />
presented to Registration in the ED area. Usually an ED tech<br />
would bring such a patient up to L&D from Registration. But Jeanette<br />
had done an “eyeball assessment” and decided to put this very soonto-be<br />
mom in a wheelchair and bring her to L&D herself. Upon entering<br />
L&D, Jeanette saw how busy it was. So, she asked someone<br />
where the IV tray was. She helped the patient change into a gown, assisted<br />
the patient to a bed, obtained blood samples, started the IV and<br />
reported off to an L&D nurse. Jeanette’s patient delivered about 15<br />
minutes later, just 40 minutes after arriving to the hospital.<br />
Jeanette is willing to help just about everybody, any department,<br />
and any campus.<br />
May 2012 Vincenta Balbin, RN, Respiratory Rehab Unit<br />
Pictured (l-r): Cheryl Beers, DHA, RN, NE-BC, CALA, Director, Nursing<br />
Operations; Timothy Doyle, Administrator RRC; Vincenta (Vicki)<br />
Balbin, RN; Marianne DeAlessi, BSN, MPA, RN, CSN-NJ, Director of<br />
Nursing RRC; and Suellyn Ellerbe, MN, RN, NEA-BC.<br />
Vincenta or “Vicki” is a night-shift nurse, and two hours prior to<br />
Vicki’s arrival to work on RRC, a resident began her “terminal wean”<br />
process. Over a three-hour period, Vicki continually assessed the<br />
resident’s response to the weaning process. Using her critical thinking<br />
skills and compassion, Vicki initiated ongoing communication with<br />
the physician. Medication orders were changed promptly to make her<br />
more comfortable. Vicki was empathetic and compassionate to both<br />
the resident and her family. She was a support for the family, she<br />
prayed with them as they watched their loved one journey through<br />
the end-of-life process.<br />
Two days after the resident died, the family members called to express<br />
their gratitude to Vicki for providing a calming and spiritual atmosphere<br />
during this journey.<br />
The DAISY Award<br />
The DAISY Award is a nationwide program that rewards and celebrates<br />
the extraordinary clinical skill and compassionate care given by<br />
nurses every day. DAISY Nurses are the kind of nurses about whom<br />
other RNs say, “I would want this nurse to take care of my mother.”<br />
<strong>Saint</strong> Clare’s Health System is proud to participate in the DAISY<br />
award program and presents 12 DAISY awards each year.<br />
The nomination process is simple; just provide a specific story about<br />
why a nurse or colleague should receive this award. Nominations can<br />
be made on the intranet – Nursing Departments – DAISY Award.<br />
PRAYERS FOR AN IV<br />
Recently I was called to start an IV on a patient who was dying. As I<br />
entered the room, I saw a frail, cachectic elderly woman with no visible<br />
veins who was moaning in pain. This patient's daughter was pacing<br />
in the room, and most anxious because she wanted her mother to<br />
receive medication for her pain. I prepared to start the IV, selected a<br />
24-gauge catheter and prayed, “Hail Mary full of grace, put this vein<br />
in its place.” Only by prayer and divine intervention, did this IV<br />
catheter slip into the vein and we were able to administer pain medication.<br />
And let's not forget the namesake of our hospital when starting an<br />
IV. When we think we feel but don't even see the vein, pray the following<br />
silently, “Dear and holy, good <strong>Saint</strong> Clare, I pray to you a vein<br />
be there.” Harmony McConnell, BSN, RN, CEN, ED staff nurse<br />
also has an IV prayer, “Lord help this man and guide my hand.”<br />
Now I hope you will join us in saying a prayer whenever starting IVs.<br />
Martha Bittner, RN<br />
Shift Administrator<br />
GET THE SCOOP ABOUT MENTAL HEALTH<br />
The World Health Organization gives the following as a definition of<br />
mental health: “A state of emotional and psychological well-being in<br />
which an individual is able to use his or her cognitive and emotional<br />
capabilities, function in society, and meet the ordinary demands of<br />
everyday life” (WHO, 2010).<br />
Mental illness impacts the lives of at least one in four adults and<br />
- 7 -<br />
(continued)
VOLUME 3 ISSUE 4<br />
one in 10 children or 60 million Americans. To<br />
support someone you love who suffers from<br />
mental illness can present a multitude of challenges.<br />
These clients did not seek out this disease,<br />
they or their loved ones can’t “cure it” and<br />
those who are part of their world need to accept<br />
that there is no “blame” to be placed for<br />
having a mental illness. There are however, Susanne J. Graham<br />
many things that we can do to help people with mental illness to seek<br />
treatment, help those around them to understand and become educated<br />
on the various forms of mental illness and treatments available,<br />
and how to envelop the client with care and support in their environment<br />
and community.<br />
Having a mental illness is extremely stressful for the client, the family,<br />
and their community. Often, the designated client cannot understand<br />
or verbalize everything that is happening to them when they are<br />
symptomatic. The more that those in his/her world ask “why are you<br />
doing, saying this” the more difficult and frustrating it becomes for the<br />
client. They don’t have the answers, they did not choose for this to<br />
happen, they don’t mean to upset, anger, embarrass or disappoint<br />
those who love and care about them. If you would like to be entered<br />
to win a copy of the book featured in this issue, They Called Them<br />
Angels: American Military Nurses of World War II, please email Sue<br />
Weaver at sweaver@saintclares.org.<br />
So when you ask, “what can I do to help,” the first answer is to ED-<br />
UCATE yourself about the illness. Knowing what to expect, the symptoms<br />
and treatments, will allow you to offer support without<br />
personalizing some of the negative behaviors and consequences you<br />
may be encountering. When you create an environment of understanding<br />
and a community of acceptance for our clients, they will have<br />
a greater chance to flourish and thus minimize the stigma that many<br />
feel is associated with having a mental illness.<br />
To partner with the team of professionals who stand ready to help<br />
your loved one is a matter of trust. It will require a “leap of faith”<br />
sometimes that you place the emergent or immediate care of your family<br />
member in the hands of someone you might not know. However,<br />
if you continue to reach out and ask questions, <strong>Saint</strong> Clare’s Hotline<br />
973-625-0280, we can hopefully earn that trust by connecting you<br />
with the provider that will best help you along your journey.<br />
In Morris County, indeed within <strong>Saint</strong> Clare’s, we are extremely fortunate<br />
to have an outpatient system with programs that are focused on<br />
promoting the health and recovery of our Behavioral Health clients.<br />
We have Intensive Family Support Services (IFSS) 973-625-<br />
7095. This team of professionals will work with family members or<br />
significant others who have a loved one with mental illness. They provide<br />
emotional support, educational opportunities, group discussions,<br />
professional speakers, and a host of other opportunities that will help<br />
a family or community to better support their family member in treatment.<br />
The Wellness and Recovery Center, 973-625-0096, is a non-hospital<br />
setting in which a client in crisis can be seen by a team of professionals<br />
and develop a plan of care to mitigate the crisis while being<br />
able to remain in their own home or with family support for up to 30<br />
days, and then transition the client to a next level of care, if needed.<br />
The Self Help Clearinghouse, 973-989-1122, provides a listing<br />
of all the Self-Help Support groups in the area for just about any topic,<br />
and includes how to begin a group of your own.<br />
The Supported Education Program, 973-625-7124, the staff in<br />
this program will help the client seek educational opportunities within<br />
their community to promote their personal growth and future opportunities<br />
and assist them in achieving their goals, promoting a sense of<br />
accomplishment and self worth.<br />
The Supported Employment Program, 973-625-7070, works<br />
with local community businesses and matches clients with employment<br />
opportunities available. This enables many of our clients to live<br />
independently, and have independence.<br />
The Supported Living Program, 973-298-8640, seeks out affordable<br />
housing opportunities in local communities that will allow our<br />
clients to live independently, with the least amount of support necessary,<br />
to enable them to enjoy personal freedom, while letting them<br />
know that they are a phone call away from assistance, if needed.<br />
The most important message the Behavioral Health Team can convey<br />
to you is, YOU ARE NOT ALONE! When in doubt…Reach<br />
Out! We are here to help!<br />
References:<br />
World Health Organization. (2010). Mental health: strengthening our<br />
response. WHO Media Centre: Fact Sheet N 220 September 2010.<br />
http://www.who.int/mediacentre/factsheets/fs220/en/<br />
Susanne J. Graham, MA, RN-BC<br />
Psychiatric Emergency Service<br />
- 8 -<br />
(continued)
VOLUME 3 ISSUE 4<br />
NURSING<br />
NEWS<br />
CAGE (Cut - Annoyed - Guilt - Eye Opener)<br />
Upon admission, when completing the patient history, the<br />
nurses questions the patient about alcohol use. When the<br />
patient indicates that they drink alcohol daily or weekly consider<br />
asking the following CAGE questions:<br />
1. Have you felt you ought to Cut down on your drinking?<br />
2. Have people Annoyed you by criticizing your drinking?<br />
3. Have you ever felt Guilty about your drinking?<br />
4. Have you ever had a drink first thing in the morning<br />
(Eye opener) to steady your nerves or get rid of a hangover?<br />
If the patient answers more than two of these questions positively,<br />
they are considered alcohol dependent.<br />
Reference:<br />
McKinley, M. (2005). Alcohol withdrawal syndrome: overlooked<br />
and mismanaged? Critical Care Nurse, 25(3), 40.<br />
HINDU<br />
Asian Indians are the second largest Asian group in the United<br />
States.<br />
Eighty five percent of Asian Indians are Hindu.<br />
The Hindu believe in:<br />
• one God,<br />
• Karma, from this life or a past life, influences one’s health,<br />
• reincarnation of the soul until all of the Karma’s are resolved,<br />
• the endless cycle of the universe.<br />
The Hindu has a tight-knit, extended family who usually all live together.<br />
The grandparents aid in raising the children.<br />
A family member will usually stay with the patient while he or she<br />
is in the hospital to aid with the care of the patient. The entire family<br />
is involved in the decision making process.<br />
The Hindu are strict vegetarians. They do not believe in killing animals<br />
or fish, as they feel that all life is sacred.<br />
The Hindu may utilize Ayurevdic medicine which incorporates the<br />
body, mind, and soul.<br />
They are predisposed to metabolic syndrome due a genetic resistance<br />
to insulin.<br />
Hindu patients are very modest and prefer that they be cared for<br />
by someone of the same gender, if possible.<br />
They believe in a natural death that is calm and pain free surrounded<br />
by their family. They do not believe in artificially prolonging life.<br />
Lisa Grath, BSN, RN, NE-BC<br />
Shift Administrator<br />
HPV<br />
Genital human papillomavirus (also called HPV) is the most common<br />
sexually transmitted infection (STI). Most people who become<br />
infected with HPV do not develop symptoms or health problems<br />
and their body’s immune system clears HPV naturally within two<br />
years. But some people who get HPV will go on to develop cancer<br />
or other health problems.<br />
• HPV can cause genital warts in males and females.<br />
• HPV can cause cervical cancer and other, less-common cancers,<br />
including cancers of the vulva, vagina, penis, anus, and<br />
head and neck (tongue, tonsils and throat).<br />
Since 2006, HPV vaccines have been available as three shots to<br />
protect against HPV infection and HPV-related diseases. Two vaccines<br />
(Cervarix and Gardasil) have been shown to protect against<br />
most cervical cancers in women. One vaccine (Gardasil) also protects<br />
against genital warts and has been shown to protect against<br />
cancers of the anus, vagina and vulva. Both vaccines are available<br />
for females. In 2009, Gardasil was approved for males.<br />
HPV vaccines offer the greatest health benefits to individuals<br />
who receive all three doses before having any type of sexual activity.<br />
That’s why HPV vaccination is recommended for preteen girls<br />
and boys at age 11 or 12 years. Nurses should provide information<br />
and encourage parents and students to receive the HPV vaccine.<br />
References:<br />
Centers for Disease Control and Prevention,<br />
http://www.cdc.gov/hpv/vaccine.html<br />
Johnson-Mallard, V., Thomas, T., Kostas-Polston, Barta, M.,<br />
Lengacher, C., & Rivers, D. (2012). The nurse’s role in preventing<br />
cervical cancer: A cultural framework. American Nurse Today, 7(7),<br />
37-40.<br />
- 9 -<br />
(continued)
VOLUME 3 ISSUE 4<br />
NDNQI<br />
This October, <strong>Saint</strong><br />
Clare’s Health System<br />
will again participate in<br />
the National Database<br />
of Nursing Quality Indicators<br />
RN Survey. The survey is offered to direct care RNs in member<br />
hospitals. According to the NDNQI, in 2011 over 325,000 RNs<br />
from 893 hospitals responded to the survey. The purpose of the survey<br />
is to obtain a picture of the RN work climate on every participating<br />
unit in <strong>Saint</strong> Clare’s. This year, the Maternal Child units will<br />
participate for the first time and <strong>Saint</strong> Clare’s will utilize the long form.<br />
Confidentiality is protected and reported information is summarized<br />
for the entire hospital as a whole and individual units. Details will<br />
emerge as the October start date gets closer.<br />
Marianne DeAlessi, BSN, MPA, RN, CSN-NJ<br />
Director of Nursing, RRC<br />
UNDERSTANDING BULLYING IN THE<br />
WORKPLACE: PART 2, THE EFFECT ON<br />
THE NURSING TEAM<br />
In Part 1, what is bullying? a definition of bullying/workplace violence<br />
and five types of bullying were discussed. To review, bullying is<br />
consistent, repeated, offensive behavior that undermines employees<br />
and creates a stressful work environment for the victim and the other<br />
employees (Beers, 2012). Bullying can be both covert, subtle rude behaviors<br />
and innuendos, or overt, openly abusive, physical or psychological<br />
(Lesley, 2006). The five categories of bullying include: 1) threat<br />
to professional status, 2) threat to personal standing, 3) isolation, 4)<br />
overwork, and 5) destabilization (Rayner & Hoel, 1997). The challenge<br />
to the reader at the end of Part 1 was to observe the personal<br />
work environment to identify any bullying behaviors that may fit into<br />
one of the five categories. Nurses often tolerate bullying as part of the<br />
job and unless nurse leaders provide training, nursing staff may not<br />
identify the behaviors toward them as bullying. Identification of bullying<br />
is necessary to prevent deterioration of the nursing team, which<br />
promotes a safe patient care environment.<br />
The effects of bullying on the nursing team result in decreased<br />
motivation, decreased morale, decreased productivity, increased error<br />
rates, increased turnover, and increased stress (Martin, Gray & Adam,<br />
2008; Yildirum, 2009). Verbal abuse is the most common but least addressed<br />
behavior on the nursing unit. The verbal abuse behaviors of<br />
- 10 -<br />
the bully include aggressive communication behavior, sarcasm, insults,<br />
and refusal to support the nursing team. On nursing units, the staff<br />
sometimes creates work-a-rounds to reduce interaction with a bully.<br />
An example of subordinate to manager vertical workplace violence<br />
is when a unit secretary is rude or sarcastic toward the charge<br />
nurse. The nurse may ask the unit secretary to place a call to a physician<br />
and the unit secretary responds with undertones, nasty facial expressions,<br />
or does not make the call. The charge nurse is intimidated<br />
and may create a work-a-round such as asking a nursing assistant to<br />
perform the task, or doing the task herself so that she does not have<br />
to interact with the bully. All of the nursing team members, including<br />
the manager, are probably aware of the situation and bullying behaviors,<br />
but no action is taken to address the behavior. The result is a<br />
devalued feeling among the rest of the nursing team. One concern is<br />
that if an emergency occurs on the nursing unit, and the unit secretary<br />
is scheduled to leave the unit for a break, the deflated charge nurse<br />
may not confront the bully and ask her to take her break at a later<br />
time. The message the nurse leader is sending to the staff is that the<br />
bullying behavior is acceptable, which further demoralizes the staff<br />
and creates a stressful environment.<br />
Verbal abuse by power and status occurs between a physician and<br />
a nurse or a patient and a nurse. The literature documents several studies<br />
where nurses fall prey to the verbal abuse of physicians. Physicians<br />
may scold, demean, or behave in an intimidating manner to nurses in<br />
public areas and in front of patients. Physician intimidation may result<br />
in delays in patient care because nurses may become afraid to call<br />
with abnormal blood values or change in status. A novice nurse may<br />
be intimidated to the point that she is unable to critically think in an<br />
emergent situation in the presence of a physician who is intimidating<br />
(Berry, Gillespie, Gates, & Schafer, 2011). Patients may be verbally<br />
and at times, physically abusive to nursing team members citing the<br />
Patient Bill of Rights as a license to be abusive.<br />
The patient is a passive victim of bullying behaviors for several<br />
reasons. Morale is low on the unit which results is decreased team<br />
work that causes delays to patient call bell requests and may result in<br />
care delays if a nurse or nursing assistant is tied up with a patient and<br />
can’t attend to other patients or round hourly. A positive correlation<br />
between nursing staff illness and bullying results in increased sick calls<br />
and turnover rates, which in turn may result in short staffing and increased<br />
agency nurse usage (Berry, Gillespie, Gates, & Schafer, 2011).<br />
Bullying behaviors of seasoned nursing staff impedes the ability of the<br />
novice nurse to focus on critical thinking skills, and cope in complex<br />
situations. The delay in gaining competency skills results in decreased<br />
(continued)
VOLUME 3 ISSUE 4<br />
productivity and increased error rates. Workplace violence increases<br />
turnover rates of the novice nurse within the first two years as a result of<br />
increased stress and physical illness. A new nurse may adapt to the behavior<br />
and intimidate the behavior of the bully creating a bullying cycle as<br />
a means of survival in the culture of the organization (Thomas, 2010).<br />
Nurse leaders and educators are responsible to create a safe environment<br />
for employees and patients. In 2009, The Joint Commission<br />
mandated a leadership standard that accredited health care organizations<br />
implement a code of conduct for employees that creates a culture<br />
of safety (Thomas, 2009). The culture of safety standard requires<br />
the leadership team to execute a code of conduct that defines acceptable<br />
and unacceptable behaviors and a plan of action to address unacceptable<br />
behaviors. An educational program and discipline policy,<br />
which protects employees from intimidation, sarcasm, and other bullying<br />
behaviors, must be documented. Nurses must be empowered to<br />
report bullying behaviors of peers, physicians, managers, and patients<br />
so that the leadership team has the information necessary to address<br />
the unwanted behaviors (Berry, Gillespie, Gates, & Schafer, 2011,<br />
Thomas, 2010). Nurse productivity, error rates, morale and retention<br />
will improve in a culture of zero tolerance and safety.<br />
If you are a victim of workplace violence or bullying, report the incident<br />
to your manager immediately. At the end of Part 1, the author<br />
challenged the reader to observe the environment for bullying behaviors.<br />
The challenge for Part 2 is to report those unacceptable behaviors<br />
so that nursing leadership can intervene. Any employee who wants to<br />
make a confidential report can call the ethics hotline for assistance.<br />
The entire health care team must work together to promote a Culture<br />
of Safety for our employees, patients, physicians, and families.<br />
Rayner, C. & Hoel, H. (1997). A summary review of literature relating<br />
to workplace bullying. Journal of Community and Applied Social<br />
Psychology, 7, 181-191.<br />
Thomas, C. (2010). Teaching nursing students and newly registered<br />
nurses strategies to deal with violent behaviors in the professional<br />
nurse practice environment. The Journal of Continuing Education in<br />
Nursing, 41(7), 299-308.<br />
Yildirim, D. (2009). Bullying among nurses and its effects. International<br />
Nursing Review, 56, 504-511.<br />
Cheryl Beers, DHA, RN, NE-BC, CALA<br />
Director, Nursing Operations<br />
EDUCATION FOR PATIENTS AND FAMILIES<br />
RELATED TO INFECTION PREVENTION<br />
References:<br />
Beers, C. (2012). Understanding bullying in the workplace: Part 1,<br />
what is bullying? Careful Nursing Newsletter, 3(3), 7.<br />
Berry, P., Gillespie, G., Gates, D., & Schafer, J. (2011). Novice nurse<br />
productivity following workplace bullying. Journal of Nursing Scholarship,<br />
44(1), 80-87.<br />
Gray, A., Gray, C., & Adam, C. (2008). Nurse’s responses to workplace<br />
verbal abuse: A scenario study of the impact of situational and<br />
individual factor. Research and Practice in Human Resources Management,<br />
15(2), 1-17.<br />
Lesley, F. (2006). Why, when we are deemed to be Carers, are we so<br />
mean to our colleagues? Canadian Operating Room Nursing Journal,<br />
24(4), 13-16.<br />
- 11 -<br />
What can we do to help our patients and their families have a better<br />
understanding of what we will do and what they can do to help prevent<br />
healthcare-acquired infections? It all starts with education. Studies<br />
show that patients who are on isolation feel like they do not get the<br />
same care from the nursing staff that the other patients receive. It is<br />
important to explain to them and their families why isolation is in<br />
place and how organisms are spread.<br />
Patient education sheets are available in English and Spanish in your<br />
isolation books on your units for:<br />
• MRSA<br />
• C-Diff<br />
• ESBL<br />
• Tuberculosis<br />
• VRE<br />
(continued)
VOLUME 3 ISSUE 4<br />
The Infection Control Nurses are always available to help answer<br />
questions your patients and their families may have.<br />
Remember to also give your patients the education sheets attached<br />
to the start kits for Central Lines and Indwelling Catheters when these<br />
devices are inserted. These sheets explain to them what the device is,<br />
how we will prevent infections and what they can do to prevent infections.<br />
….and of course remember to document all the education you<br />
provide!!<br />
Hand hygiene continues to be the backbone of good infection prevention.<br />
All visitors need to be encouraged to perform hand hygiene when<br />
they come in to visit and when they leave to go home. If their family<br />
member is on isolation they need to be instructed if they need to wear<br />
PPE and that they should be washing their hands when they leave the<br />
room to go out to the nurses’ station, into the nourishment center, etc.<br />
Encourage having your patients and visitors ask questions. Again,<br />
we are always here to help answer any questions they or you may have.<br />
Laura Anderson, MSN, RN, CIC<br />
Infection Control, Nurse Epidemiology<br />
Sarah Granda, RN, APN<br />
Infection Control, Nurse Epidemiology<br />
FAMILY HEALTH, THE NEUMAN MODEL<br />
For those who have studied the Betty Neuman Systems Model, (and<br />
I’ll bet there are plenty of us), the influence of the family in health<br />
promotion coincides with nurse practice beliefs. The Neuman Systems<br />
Model expands to include the family members as an extension<br />
of the patient to become an inclusive primary focus (Neuman, 1995).<br />
The concept of family health has two distinct aspects: it may include<br />
the health or absence of disease of family members, or it may include<br />
the condition of the family itself. Therefore, the concept of<br />
“family health” can refer to an individual within that group, or of the<br />
family as a whole. This can also pertain to physical or emotional wellness<br />
or illness (Neuman, 1995). Neuman’s idea of family health includes<br />
a concept of holistic family health, body/mind/spirit and<br />
incorporates wellness and illness in interaction with the environment<br />
(Neuman, 1995). Five processes are included within this theory:<br />
1. Interactive processes: inclusive of family relationships, communication,<br />
nurturance, intimacy, and social structure.<br />
2. Developmental processes: inclusive of family transitions and the<br />
dynamic interaction between family development and individual<br />
developmental experience in both health and illness.<br />
- 12 -<br />
3. Coping processes which includes decision making, problem solving,<br />
and adaptation to stressors that are part of health promotion<br />
and health maintenance.<br />
4. Integrity processes which includes such concepts as shared meaning<br />
of experiences, family identity and commitment, family history,<br />
values, boundary maintenance and family rituals that relate<br />
to health experiences.<br />
5. Health processes that embrace family health beliefs, family health<br />
status, family health responses and lifestyle practices, and familycentered<br />
health care provision during illness and wellness (Neuman,<br />
1995).<br />
Neuman’s primary health care goal is to “facilitate optimum level<br />
wellness for the client by retaining, attaining, and maintaining client<br />
system stability” (Neuman, 1995, 139). As those of us who are familiar<br />
with Neuman’s theory, stressors from the internal or external environment<br />
can penetrate the flexible and normal lines of defense,<br />
causing a systemic reaction of varying degrees or deviation from wellness<br />
(Neuman, 1995). Our primary goal as nurses includes decreasing<br />
the stressors within the patient’s environment and maximizing cohesive<br />
and positive health influences within the patient’s life. We can<br />
utilize our assessment skills to identify positive and negative resources<br />
within the family unit, and introduce healthy coping measures for all.<br />
Sometimes this might include the use of resources outside of nursing;<br />
however, our commitment to the family reduces individual illness<br />
within a solitary member, and strengthens the family as a whole.<br />
Reference:<br />
Neuman, B. (1995). The Neuman systems model (3rd ed.). Norwalk,<br />
CT: Appleton & Lange.<br />
Sandy Clark, BSN, MHA, RN, NE-BC<br />
Boonton Shift Administrator<br />
NEXIVA<br />
After much discussion, research, unit-based trials and with support of<br />
the Nurse Practice Council, <strong>Saint</strong> <strong>Clare's</strong> began using the BD Nexiva<br />
closed catheter IV system. The primary reason for conversion to this<br />
closed IV catheter is there is no exposure to blood during insertion. One<br />
research study found there was a statistically significant difference in<br />
nurses exposure to blood between insertion with the BD Nexiva closed<br />
IV catheter and Braun Introcan Safety Catheter (Bausone-Gazda,<br />
Lefaiver, Walters, 2010). With the Nexiva catheter, the Statlock IV start<br />
kit was eliminated and the 3M Tegaderm IV securement dressing intro-<br />
(continued)
VOLUME 3 ISSUE 4<br />
duced. Stabilization and securement<br />
of IV catheters are<br />
critical in reducing IV<br />
restarts and preventing IV<br />
complications such as infiltration<br />
and phlebitis. So take<br />
your time getting used to<br />
this new IV Nexiva catheter, it will benefit you and your patients.<br />
Reference<br />
Bausone-Gazda, D., Lefaiver, C., & Walters, S. 2010. A randomized controlled<br />
trial to compare the complications of 2 peripheral intravenous<br />
catheter-stabilization systems. Journal of Infusion Nursing, 33(6).<br />
Sue Weaver, MSN, RN, CRNI, NEA-BC<br />
Co-Chair, Patient Care Value Analysis Committee<br />
Kathy Basile, MS, MSN, RN, ONC<br />
Project Lead, Nexiva IV Catheter<br />
At the June Careful Nursing News Editorial Board meeting, it<br />
was suggested that we have a Letter to the Editor column. So if<br />
you have comments about articles in newsletter, please send to the<br />
Editor at nurse@saintclares.org and your letters will be published<br />
in the next issue.<br />
Careful Nursing Newsletter Editorial Board pictured after annual<br />
meeting from left to right: William L. Holzemer, RN, PhD, FAAN,<br />
Dean and Professor, Rutgers, The State University of New Jersey;<br />
Megan Weller, BSN, RN, Staff Writer; Sue Weaver, MSN, RN, NEA-<br />
BC, CRNI, Editor; Beth Smith, BSN, RN, Staff Writer; Suellyn<br />
Ellerbe, MN, RN, NEA-BC, former Executive Editor; Robert Hess,<br />
PhD, RN, FAAN, Executive Vice President, Global Programming<br />
Gannett Education, Gannett Healthcare Group; Janice Lynch, MSN,<br />
RN, Regional Nurse Executive, Nurse.com; Lori Price, Columnist,<br />
New Jersey Herald.<br />
NEWLY ISSUED WARNING ON<br />
ONDANSETRON (ZOFRAN ® )<br />
The Food and Drug Administration (FDA) issued a warning on the<br />
anti-nausea medication ondansetron (Zofran®, GlaxoSmithKline) on<br />
June 29, 2012. A recently completed clinical study suggested that a 32<br />
mg single intravenous dose of ondansetron may affect the electrical<br />
activity of the heart, causing QT interval prolongation and predispose<br />
patients to develop abnormal heart rhythm that can potentially be<br />
fatal, such as Torsades de Pointes. 1<br />
Ondansetron is a selective serotonin receptor antagonist that is available<br />
in both oral and parenteral dosage forms. Ondansetron is FDAapproved<br />
for the treatment of chemotherapy-induced nausea and<br />
vomiting (CINV) and also for the treatment and prophylaxis of postoperative<br />
nausea and vomiting (PONV). The higher dose of 32 mg intravenous<br />
injection was used for pre-chemotherapy prophylaxis. The<br />
FDA had previous noted cardiac side effects that are associated with<br />
ondansetron. 2-3 GlaxoSmithKline, the manufacturer of Zofran, was<br />
required by the FDA to conduct a thorough QT study to assess the<br />
cardiovascular side effects of the drug. Preliminary review of the study<br />
suggests that QT prolongation caused by ondansetron occurs in a<br />
dose-dependent fashion, with the largest mean QT difference of 20<br />
msec occurring with the highest single intravenous dose of 32 mg<br />
when compared to placebo. 1<br />
With the newly issued warning, the FDA also provided additional<br />
recommendations to the healthcare professionals on the use of ondansetron,<br />
some of the recommendations are listed below: 1<br />
• The use of a single 32 mg intravenous dose of ondansetron<br />
should be avoided.<br />
• For CINV patients, the lower dose of 0.15 mg/kg every 4 hours<br />
for three doses can be used; however, No single intravenous dose<br />
of ondansetron should exceed 16 mg.<br />
• Patients who may be at particular risk for QT prolongation with<br />
ondansetron are those with congenital long QT syndrome, con-<br />
- 13 -<br />
(continued)
VOLUME 3 ISSUE 4<br />
gestive heart failure, bradyarrhythmias, or patients taking concomitant<br />
medications that prolong the QT interval.<br />
• Electrolyte abnormalities, such as hypokalemia or hypomagnesemia<br />
should be corrected prior to the infusion of ondansetron.<br />
This warning does not affect the recommended oral ondansetron<br />
dosing regimen which includes a maximum of 24 mg per day, or the<br />
lower intravenous dose for PONV.<br />
In response to the FDA’s recommendation, the Pharmacy and Therapeutic<br />
Committee at SCHS has voted to implement an automatic<br />
truncation policy where all pre-chemotherapy intravenous ondansetron<br />
orders will be automatically capped at 16 mg. If you have<br />
any questions on the dosing or side effect of ondansetron, please contact<br />
the pharmacy department.<br />
Janet Shen, Pharm.D.<br />
Clinical Pharmacist<br />
References<br />
1. FDA Drug Safety communication: new information regarding QT<br />
prolongation with ondansetron (Zofran). Available at:<br />
http://www.fda.gov/Drugs/DrugSafety/ucm271913.htm, accessed<br />
2 August, 2012.<br />
2. Charbit et al. Droperidol and ondansetron-induced QT interval<br />
prolongation. Anesthesiology 2008; 109(2): 206-212.<br />
3. Charbit et al. Prolongation of QTc interval after postoperative nausea<br />
and vomiting treatment by droperidol or ondansetron. Anesthesiology<br />
2005; 102(6): 1094-1100.<br />
DEAR ALLYSON<br />
As nursing students and others graduate and we<br />
begin recruiting for our 5th Nurse Residency program,<br />
the advice by Karen Roush, MS, RN, FNP-<br />
C, clinical managing editor for the American<br />
Journal of Nursing, is relevant to us all in staying<br />
well-rounded as nurses.<br />
Stay alert. Be vital. Sharpen your mind and your skills. Read journals<br />
for nurses and on health care in general. But don’t limit your knowledge<br />
to health-related information. Read political discourse, economic<br />
theory, and great literature. At the time of this writing, a book of<br />
poems, Slope of the Child Everlasting by Laurie Kutchins, sits on my<br />
desk at home. Each evening it pulls me into a deep reflection that informs<br />
my practice in a way clinical study alone can’t possibly do.<br />
- 14 -<br />
Keep moving. Learn, change, uncover, discover. There’s no other profession<br />
that allows you to do this like nursing. Whether it’s within<br />
your facility or as a travel nurse exploring the country, or perhaps<br />
going from clinical care to a policy-making position, movement will<br />
awaken the anticipation and excitement that you felt in the beginning<br />
of your career.<br />
Look beyond your borders. Whether they’re a shift, a hospital, a specialty,<br />
a state, a country. Reach outside of what you know. See yourself<br />
as part of something bigger than nursing.<br />
Act out. Be willing to anger people. Remember, you are valuable and<br />
necessary. Get your facts straight, then speak up loud and often. Make<br />
some noise and get some attention. And then be ready to back up<br />
your words with actions.<br />
Become nursing’s biggest fan. Promote it. Boast about it. It will go<br />
a long way in making nursing what it should be—well paid, well understood,<br />
and respected. It will draw talented people to the profession.<br />
Nursing suffers from gender bias, this is important to recognize<br />
whichever gender you happen to be. It affects who goes into nursing,<br />
how your role is allowed to evolve, and how much you get paid. The<br />
answer isn’t in making the profession good enough for men; it’s in<br />
making the profession good enough.<br />
Lastly, don’t let nursing define your whole being. Be a baker, a runner,<br />
a book club member, a father, a wife. Whatever it is, be it totally,<br />
ferociously, and separate from nursing. As a writer of poetry, I am<br />
often referred to as a nurse-poet and I always protest. I am not a nursepoet<br />
or a nurse-anything. I am a nurse and a poet . . . among other<br />
things. Nursing takes incredible mental and physical energy. Shelter<br />
that part of you that is away from nursing and it will energize your<br />
presence as a nurse.<br />
If you have a question for Allyson Bakewell, <strong>Saint</strong> Clare’s Nurse Recruiter,<br />
please email her at AllysonBakewell@saintclares.org and your question<br />
might be featured next month in her Dear Allyson column.<br />
“is not only to carry out the proper measures<br />
yourself but to see that everyone else does so too.”<br />
— Florence Nightingale<br />
(continued)
VOLUME 3 ISSUE 4<br />
CULTURAL COMPETENCE DAY 2012<br />
For Denville Cultural Competence Day on May 10, 2012, Ann<br />
McLoughlin, BSN, RN, CMSRN, Admission Nurse represents Ireland<br />
and served her world-famous Irish soda bread with Irish butter.<br />
Dana Palmer, BSN, RN, CCU Staff nurse represents Deutschland<br />
(aka Germany) serving apple cake and German chocolate cake at<br />
Denville Cultural Competence Day.<br />
Enjoying a bit of Poland at the Annual <strong>Saint</strong> <strong>Clare's</strong> Cultural<br />
Competence Day, pictured (l-r) are: Stacey Rodimer, BSN, RN,<br />
Quality Management Specialist; Ruth Alea, BSN, RN, CCRN, CCU<br />
staff nurse; Maryanne Onuegbu, Lauren Krause, BSN, MBA, RN,<br />
Quality Management Specialist; Sarah Granda, RN, APN-C,<br />
Infection Control, Nurse Epidemiology; and Auston Halverson,<br />
Sustainability Supervisor, Housekeeping Department.<br />
For Denville Cultural Competence Day, Jaricsa Lopera, 4B Unit Service<br />
Coordinator, Nancy Corrales, BSN, RN-BC, 4B Shift Supervisor,<br />
Natalia Gutierrez, NA, and Angela Garces, RN, 3 Hope Clinical Educator,<br />
represent Colombia in colorful outfits serving delicious empanadas,<br />
chicken and rice, rice pudding, and coffee hard candy while playing videos<br />
of the exotic Colombia displaying all their beauty, color, music, culture,<br />
and amazing vacation spots. They also added flavor to the Nurse's Week<br />
celebration by bringing two Colombian salsa professional dancers who<br />
made everyone want to get off their chairs and do some dancing.<br />
The dancers of "The Pagdiwata Dance" an ethnic Filipino dance are congratulated<br />
by nursing leadership, pictured (l-r) are: Maridel Tenned, BSN,<br />
RN, OCN, ATU staff nurse; Arlene Fidellaga, Choreographer; Dannette<br />
Marin, BSN, RN, RNFA, CNOR, OR staff nurse; Jan Bednar, BSN,<br />
MS, RN, CEN, Executive Director of Nursing; Jean Gloria, RN,<br />
Maternal-Child staff nurse; Debbie Regen, BSN, MS, RN, Chief Nursing<br />
Officer; Desiree Besana, RN, ED staff nurse; Martina Mendoza, RN,<br />
OR staff nurse; and Josie Nemeth, RN, ED staff nurse.<br />
- 15 -<br />
For Denville Cultural Competence Day, Brian Chan, BSN, RN,<br />
OR staff nurse, represents China with a colorful poster depicting the<br />
country's rich culture, and serving popular snacks and desserts.<br />
(continued)
VOLUME 3 ISSUE 4<br />
One of the highlights of the Denville Cultural Competence Day was<br />
"The Pagdiwata Dance" an ethnic Filipino dance performed by Ruth<br />
Alea, BSN, RN, CCRN, CCU staff nurse; Desiree Besana, RN, ED<br />
staff Nurse; Arlene Fidellaga, Choreographer; Jean Gloria, RN,<br />
Maternal-Child staff nurse; Martina Mendoza, RN, OR staff nurse;<br />
and Dannette Marin, BSN, RN, RNFA, CNOR, OR staff nurse.<br />
Reunion – Rose Crist, RN, Same Day Surgery; Robert Hess,<br />
PhD, RN, FAAN, Executive Vice President, Global Programming<br />
Gannett Education, Gannett Healthcare Group; and<br />
Lorraine Lewandowski, RN, Same Day Surgery; reminisce<br />
about when they worked together in <strong>Saint</strong> Clare’s Denville<br />
ICU. Bob was the Director of the ICU, Lorraine worked the<br />
day shift, and Rose was in charge on the night shift.<br />
Careful Nursing Newsletter<br />
For Denville Cultural Competence Day, Veronica Garces, BSN, RN,<br />
Urban 2 staff nurse, and Andrea Alcocer, BSN, RN, Maternal-Child<br />
staff nurse, represent their country of Ecuador by highlighting the<br />
country's many festivities and sites along with serving a dish of ceviche.<br />
Editor:<br />
Staff Writers:<br />
Production<br />
Director:<br />
Editorial Board:<br />
Sue Weaver, MSN, RN, NEA-BC, CRNI<br />
Scott Freitag, BSN, RN, JD<br />
Megan A. Weller, BSN, RN<br />
Beth Smith, BSN, RN<br />
Cathy Dunn, Marketing Communications<br />
Cheryl Beers, DHA, RN, NE-BC, CALA,<br />
Director of Nursing, Operations<br />
Jeannie P. Cimiotti, DnSc, RN, Executive Director,<br />
NJ Collaborating Center for Nursing<br />
Robert Hess, PhD, RN, FAAN,<br />
Executive Vice President, Global Programming<br />
Gannett Education, Gannett Healthcare Group<br />
CCU staff were delighted and proud to share their unique cultures at the<br />
Denville Cultural Competence Day. Pictured (l-r) are: Natalia Gutierrez,<br />
NA; Tracy Oster, BSN, RN, CCU Clinical Educator; Pat Kruse,<br />
RN, CCU Shift Supervisor; Vivek Agnihotri, MSN, RN, CCRN, APN,<br />
CCU staff nurse; Ruth Alea, BSN, RN, CCRN, CCU staff nurse; Dana<br />
Palmer, BSN, RN, CCU staff nurse; and Sister Susan Evelyn.<br />
- 16 -<br />
William L. Holzemer, RN, PhD, FAAN,<br />
Dean and Professor, Rutgers, The State University<br />
of New Jersey<br />
Janice Lynch, MSN, RN, Regional Nurse Executive,<br />
Nurse.com<br />
Lori Price, Columnist, New Jersey Herald