MRA acquisition
MRA acquisition
MRA acquisition
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
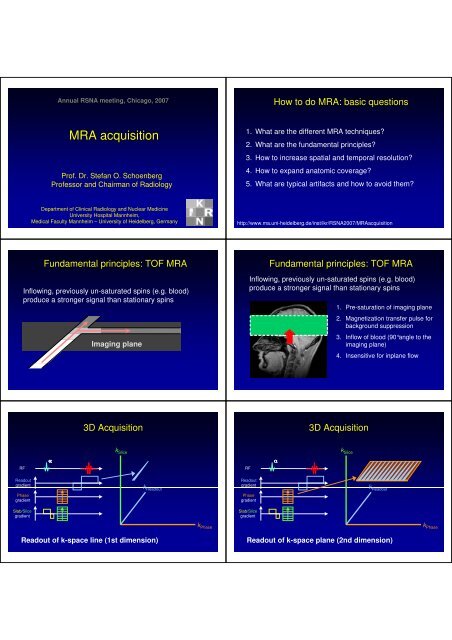
Annual RSNA meeting, Chicago, 2007<br />
How to do <strong>MRA</strong>: basic questions<br />
<strong>MRA</strong> <strong>acquisition</strong><br />
Prof. Dr. Stefan O. Schoenberg<br />
Professor and Chairman of Radiology<br />
1. What are the different <strong>MRA</strong> techniques?<br />
2. What are the fundamental principles?<br />
3. How to increase spatial and temporal resolution?<br />
4. How to expand anatomic coverage?<br />
5. What are typical artifacts and how to avoid them?<br />
Department of Clinical Radiology and Nuclear Medicine<br />
University Hospital Mannheim,<br />
Medical Faculty Mannheim – University of Heidelberg, Germany<br />
http://www.ma.uni-heidelberg.de/inst/ikr/RSNA2007/<strong>MRA</strong><strong>acquisition</strong><br />
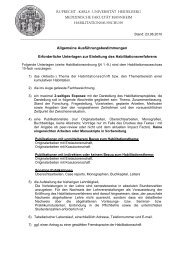
Fundamental principles: TOF <strong>MRA</strong><br />
Inflowing, previously un-saturated spins (e.g. blood)<br />
produce a stronger signal than stationary spins<br />
Imaging plane<br />
Fundamental principles: TOF <strong>MRA</strong><br />
Inflowing, previously un-saturated spins (e.g. blood)<br />
produce a stronger signal than stationary spins<br />
1. Pre-saturation of imaging plane<br />
2. Magnetization transfer pulse for<br />
background suppression<br />
3. Inflow of blood (90°angle to the<br />
imaging plane)<br />
4. Insensitive for inplane flow<br />
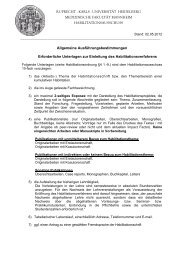
3D Acquisition<br />
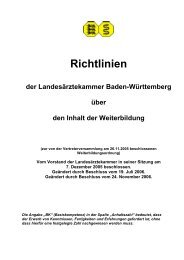
3D Acquisition<br />
k Slice<br />
k Slice<br />
RF<br />
α<br />
RF<br />
α<br />
Readout<br />
gradient<br />
k Readout<br />
Readout<br />
gradient<br />
k Readout<br />
Phase<br />
gradient<br />
Phase<br />
gradient<br />
Slab/Slice<br />
gradient<br />
Slab/Slice<br />
gradient<br />
k Phase<br />
k Phase<br />
Readout of k-space line (1st dimension)<br />
Readout of k-space plane (2nd dimension)
3D Acquisition<br />
3D Acquisition: 3D Time-of-flight<br />
k Slice<br />
RF<br />
α<br />
Readout<br />
gradient<br />
k Readout<br />
k Readout<br />
Phase<br />
gradient<br />
Slab/Slice<br />
gradient<br />
k Slice<br />
Readout of k-space volume (3rd dimension)<br />
Fourier<br />
transform<br />
k Phase<br />
k Phase<br />
Readout of k-space volume (3rd dimension)<br />
3D Time-of-flight @ 3 Tesla<br />
Time-of-flight 3T versus 7T<br />
3 Tesla 7 Tesla<br />
ACA<br />
ACA<br />
MCA<br />
MCA<br />
MCA<br />
MCA<br />
CS CS<br />
CS CS<br />
post. CA<br />
post. CA<br />
PCA<br />
PCA<br />
PCA<br />
PCA<br />
Courtesy of Paul Finn MD PhD<br />
0.3mm x 0.3mm x 0.5mm<br />
Advantages / disadvantages of TOF <strong>MRA</strong><br />
Contrast-enhanced <strong>MRA</strong><br />
Advantages<br />
• No contrast media<br />
• Easy, completely noninvasive<br />
technique<br />
• Acquisition of 3D data<br />
sets possible<br />
Disadvantages<br />
• Long <strong>acquisition</strong> times<br />
motion artifacts<br />
• insensitive for slow<br />
flow and inplane flow<br />
• High background<br />
signal<br />
• High contrast due to contrast media application<br />
• Fast <strong>acquisition</strong><br />
• High isotropic spatial resolution up to 1mm 3<br />
• Acquisition of 3D data sets<br />
• Minimum artifacts<br />
• Flow-independent b/o CM imaging of slow flow<br />
• State-of-the art in clinical routine for most applications
Application of contrast agents<br />
Technical principles of <strong>MRA</strong><br />
Image<br />
Rawdata<br />
Technical principles of <strong>MRA</strong><br />
Technical principles of <strong>MRA</strong><br />
Image<br />
Rawdata<br />
Image<br />
Rawdata<br />
Technical principles of <strong>MRA</strong><br />
K-space bolus-timing<br />
Fourier-<br />
Transformation<br />
Fourier-<br />
Fast (< seconds)<br />
Transformation<br />
Fourier-<br />
Transformation<br />
Fourier-<br />
Slow (min)<br />
Transformation<br />
• Central parts of k-space CM bolus<br />
• Timing too late venous overlay<br />
• Timing too early poor vessel contrast<br />
• Determine time between injection and CM peak at the<br />
level of the target vessel<br />
test-bolus, automatic detection, fluoroscopic realtime<br />
visualization<br />
Image<br />
Rawdata
Timing is everything<br />
Test-Bolus technique<br />
Too early: “Ringing” artifact<br />
Too late: Venous overlay<br />
Courtesy of Martin Prince, MD PhD<br />
2000<br />
Automatic Gd Detection: Smartprep ®<br />
Start<br />
scanning<br />
Fluoroscopic assessment: Care Bolus®, Bolustrak®,<br />
MR Fluoroscopy®<br />
1800<br />
Integral of Echo Speed<br />
1600<br />
1400<br />
1200<br />
1000<br />
Start<br />
Injecting<br />
Gd<br />
Detect<br />
Gd<br />
2D Real time<br />
Visualization of contrast<br />
media arrival<br />
3D HR-<strong>MRA</strong><br />
MIP<br />
800<br />
0 10 20 30 40 50 60<br />
Time (sec)<br />
Courtesy of Martin R. Prince, MD PhD<br />
Problem: delay (1-5 s) for online switch between fluoroscopy<br />
and <strong>MRA</strong> <strong>acquisition</strong><br />
<strong>MRA</strong>:<br />
problem of<br />
spatial<br />
resolution<br />
Intravascular<br />
contrast agent<br />
(SHU 555C )<br />
DSA<br />
0.3 x 0.3 mm<br />
<strong>MRA</strong>: Voxel size<br />
2.5 x 1.5 x 2 mm<br />
<strong>MRA</strong>: Voxel size<br />
1.7 x 0.8 x 1.5 mm<br />
<strong>MRA</strong>: Voxel size<br />
1.2 x 0.8 x 1.0 mm<br />
CE <strong>MRA</strong> – Increase of spatial resolution /<br />
decrease of scan time<br />
• (Zero Filling)<br />
• Partial Fourier Imaging<br />
• Elliptical centric <strong>acquisition</strong><br />
• Parallel Imaging<br />
• Higher field strength<br />
• Radial Imaging
Acquired<br />
data<br />
Zero Filling<br />
k y<br />
k x<br />
128×128 128×128, zerofilled to 256×256<br />
Partial Fourier techniques<br />
• K-space is nearly symmetric<br />
• Acquisition of k-space parts with mirroring of the data <br />
number of phase-encoding steps ↓ <strong>acquisition</strong> time ↓<br />
k y<br />
Zerofilled<br />
C<br />
B<br />
A<br />
k y<br />
256×256<br />
256×256, zerofilled to 512×512<br />
Fill periphery of k-space with zeros<br />
Interpolation of image matrix Acquisition time ↓<br />
Partial Fourier techniques<br />
Partial Fourier techniques & zero-filling<br />
60%<br />
60% of k-space no artifacts, slight blurring<br />
40%<br />
40% of k-space few artifacts, details ↓<br />
Partial Fourier techniques & zero-filling<br />
Elliptical centric <strong>acquisition</strong>:<br />
higher spatial resolution<br />
k y<br />
k z<br />
20%<br />
20% of k-space severe truncation artifacts, details ↓
Elliptical centric: aneurysm of ACA<br />
Parallel <strong>acquisition</strong> techniques (PAT)<br />
„+“<br />
Image<br />
Rawdata<br />
Parallel <strong>acquisition</strong> techniques (PAT)<br />
Parallel <strong>acquisition</strong> techniques (PAT)<br />
Reconstruction<br />
Reconstruction<br />
Fourier-<br />
2x faster<br />
Transformation<br />
PAT-<br />
PAT-<br />
Coil-<br />
Sensitivity-<br />
Profiles<br />
Aliased image<br />
Reconstructed image<br />
High-res. <strong>MRA</strong>: cross-sectional reformats<br />
Higher acceleration factors @ 1.5 T<br />
Voxel size: 3.4 0.7 mm 3<br />
PAT (GRAPPA ×2)<br />
26 s <strong>acquisition</strong> time<br />
26 s (PAT 2) 0.9 x 0.8 x 1.0 mm 19 s (PAT3)<br />
Schoenberg SO et al. Radiology 2005; 235:687–698<br />
Michaely HM, … Schoenberg SO. JMRI 2006; 24: 95-100
Artifacts: GRAPPA vs. mSENSE<br />
CE <strong>MRA</strong> – Increase of temporal resolution<br />
• Parallel Imaging (PAT): higher acceleration<br />
factors<br />
• View-sharing: TRICKS (time-resolved imaging<br />
of contrast kinetics)<br />
• View-sharing + PAT: TREAT<br />
• Variable k-space sampling + PAT: TWIST<br />
GRAPPA<br />
SENSE<br />
Schoenberg SO et al. Radiology 2005; 235:687–698<br />
Problem:<br />
Time-resolved<br />
<strong>MRA</strong> using TRICKS<br />
Low spatial resolution of<br />
time-resolved imaging<br />
Solution:<br />
Periphery of k-space is less<br />
frequently sampled than k-<br />
space center<br />
Signal<br />
time<br />
C<br />
B<br />
A<br />
TREAT<br />
(time-resolved echo-shared angiographic technique)<br />
• Combination of parallel imaging and view-sharing<br />
2,0x2,0x2,0 mm<br />
1 Bild / 2 s<br />
5 ml KM<br />
Korosec F et al. MRM 1996<br />
TWIST: time-resolved angiography with<br />
interleaved stochastic trajectories<br />
2x 3x 4x faster<br />
Parallel <strong>acquisition</strong> techniques: noise<br />
B 12<br />
3<br />
k z<br />
v<br />
A<br />
k x<br />
SNR =<br />
R<br />
SNR<br />
0<br />
g R<br />
R = 1<br />
Higher R = 2 field strength R = 3<br />
R = 4
Contrast-enhanced <strong>MRA</strong> at 3T<br />
Signal ratio: contrast-enhanced arterial blood – fat tissue<br />
T 1<br />
arterial blood<br />
T 1<br />
fat<br />
R 1<br />
Magnevist<br />
T 1<br />
blood + Gad (5 mmol/L)<br />
Signal ratio blood/fat<br />
TR=3.5 ms, a = 30°, C blood<br />
= 5 mmol/L<br />
1.5 T<br />
1250 ms<br />
343 ms<br />
4.1 L/mmol/s<br />
47 ms<br />
5.15<br />
3.0 T<br />
1650 ms<br />
382 ms<br />
3.7 L/mmol/s<br />
52 ms<br />
5.30<br />
High-resolution <strong>MRA</strong> @ 3 Tesla<br />
1.5T <strong>MRA</strong><br />
3.0T <strong>MRA</strong><br />
TR / TE [ms]<br />
3.77 / 1.39<br />
3.14 / 1.1<br />
Flip angle [°]<br />
25<br />
23<br />
Bandwidth [Hz/Px] ∆: 1.5T 3.0T350<br />
510<br />
Matrix<br />
512 x 80%<br />
Voxel volume -28%<br />
512 x 80%<br />
FOV [mm²]<br />
400 x 87%<br />
400 x 81%<br />
Slab thickness +8%<br />
Phase Oversampling [%]<br />
0<br />
8<br />
Voxel size [mm³] Scan time 0.8 -6%<br />
0.65<br />
Spatial resolution [mm³]<br />
1 x 0.8 x 1<br />
0.9 x 0.8 x 0.9<br />
Better background (fat) suppression for <strong>MRA</strong><br />
Higher vessel contrast!<br />
Decrease contrast amount by 10%-20%<br />
Scan time [s]<br />
19<br />
Partitions<br />
80<br />
Parallel imaging<br />
GRAPPA factor 3<br />
Michaely HJ, Nael K et al. Rofo. 2005; 177: 800-804<br />
18<br />
96<br />
GRAPPA factor 3<br />
From spatial to temporal resolution<br />
1.5T<br />
3.0T<br />
Spatial resolution 1.4 x 1.4 x 1.5 mm, 10 ml CM<br />
3.7 s (PAT3) Temporal Resolution 2.9 s (PAT4)<br />
3T<br />
Michaely HJ, et al. Radiology 2007; 244: 907-913<br />
Kramer H, et al.<br />
Invest Radiol 2007; 42: 477-483<br />
From spatial to temporal resolution<br />
(2D-)PAT and image geometry<br />
TWIST at 3 Tesla<br />
Courtesy of Mike Notohamiprodjo MD and Christian Glaser MD, LMU Munich
Further gains in <strong>acquisition</strong> speed:<br />
Parallel imaging with acceleration in 2D (PAT 2 )<br />
Radial <strong>acquisition</strong><br />
Rawdata<br />
Arteriogram (PAT 6 – 3x2):<br />
mild disease<br />
Courtesy of Paul Finn MD PhD, UCLA<br />
Venogram (PAT 6 – 3x2)<br />
Fenchel M, Invest Radiol 2006<br />
Willinek WA, ISMRM 2006<br />
Conventional cartesian readout<br />
in parallel lines<br />
Radial readout<br />
(rotating lines)<br />
Rawdata<br />
Radial <strong>acquisition</strong>: Streak artifacts<br />
Image<br />
Radial <strong>acquisition</strong>: Streak artifacts<br />
Fourier-<br />
32× faster<br />
Transformation<br />
but severe streak artifacts<br />
32× 16× 8× 4× 2×<br />
Extended anatomic coverage<br />
• Moving-table technique<br />
• Whole-body scanners<br />
• Continuous table movement (move during<br />
scan)<br />
CM<br />
Whole Body <strong>MRA</strong><br />
standard MR System<br />
Courtesy of Anna Gerlach, MD, Katherinenhospital Stuttgart
2 Pelvis<br />
1.5x0.7x1.5 mm<br />
19 sec<br />
3 Thigh<br />
1.5x0.7x1.4 mm<br />
13 sec<br />
Conflict to current clinical<br />
approaches<br />
4 Proximal Calf<br />
1.5x0.7x1.25 mm<br />
18 sec<br />
A<br />
B<br />
Problem: venous overlay occurring<br />
in step-by-step angiography. C<br />
Solution on a dedicated whole-body<br />
scanner:<br />
First carotids and calves<br />
then abdomen and thighs.<br />
Whole Body <strong>MRA</strong><br />
CM<br />
whole-body MRI System<br />
+ matrix coils<br />
1 Lower Calf/<br />
Forefoot<br />
1.4x0.7x0.9 mm<br />
32 sec / phase<br />
Meissner OA, …, Schoenberg SO. Radiology 2005; 235: 308–318<br />
Pereless FS, et al. Radiology. 2006; 240: 283-290<br />
Kramer H, Schoenberg SO, et al. Radiology 2005; 236: 300-310<br />
Recent studies on whole-body <strong>MRA</strong><br />
Whole-body<br />
<strong>MRA</strong>: 1.5 vs. 3 Tesla<br />
Author<br />
Field<br />
strength<br />
Minimum acquired<br />
resolution [mm]<br />
Accuracy for significant<br />
disease<br />
> 50% (* ≥70%)<br />
Interobserver<br />
variability [κ]<br />
1.5T<br />
Nael 2007<br />
1.5 T<br />
1.1 x 1.0 x 1.8<br />
SN 93%, SP 97%<br />
0.84<br />
Nael 2007<br />
3T<br />
0.87 x 0.94 x 1.0<br />
0.92<br />
Goyen 2006<br />
1.5 T<br />
1.7 x 1.5 x 2.9<br />
wb-<strong>MRA</strong> ready for clinical routine<br />
PPV 100%, NPV?<br />
3T<br />
Hansen 2006<br />
1.5 T<br />
1.76 x 1.76 x 4.0<br />
SN 83%, SP 94%<br />
Fenchel 2006*<br />
1.5 T<br />
1.6 x 1.0 x 1.5<br />
SN 96%, SP 96%<br />
Fenchel 2005*<br />
1.5 T<br />
1.6 x 1.0 x 1.5<br />
SN 96%, SP 95%<br />
0.93<br />
B1-Inhomogeneity<br />
“Move During Scan” MR Angiography @ 3Tesla<br />
=<br />
constructive<br />
=<br />
destructive<br />
RF Coil<br />
Phase<br />
B0=1.5T<br />
λH O = 52 cm<br />
2<br />
Exclusively constructive<br />
Readout<br />
B0=3T<br />
λH O = 26 cm<br />
2<br />
constructive und destructive<br />
interferences<br />
Courtesy of Harald Kramer MD, LMU Munich<br />
Reconstruction: 1. Fourier transform in readout direction<br />
2. Move data in readout direction<br />
3. Fourier transform in phase direction
How to do <strong>MRA</strong>: basic questions<br />
1. What are the different <strong>MRA</strong> techniques?<br />
2. What are the fundamental principles?<br />
3. How to increase spatial and temporal resolution?<br />
4. How to expand anatomic coverage?<br />
5. What are typical artifacts and how to avoid them?<br />
http://www.radiologie-lmu.de/RSNA2006/<strong>MRA</strong><strong>acquisition</strong><br />
Acknowledgment<br />
• Department of Radiology and Nuclear Medicine, University Hospital Mannheim,<br />
Germany: Henrik Michaely MD, Christian Fink MD<br />
• Department of Radiology, LMU Munich, Germany:<br />
Olaf Dietrich PhD, Harald Kramer MD, Mike Notohamiprodjo MD, Christian Glaser MD<br />
• Department of Radiology, Ohio State University Medical Center:<br />
Johannes Heverhagen MD, Michael V. Knopp MD<br />
• Department of Radiology, UCLA:<br />
J Paul Finn MD, Gerhard Laub PhD<br />
• Department of Radiology, Cornell University:<br />
Martin R Prince MD PhD<br />
• Department of Radiology, University of Wisconsin:<br />
Thomas Grist MD<br />
• Department of Radiology, University of Michigan:<br />
Frank Londy RT<br />
http://www.ma.uni-heidelberg.de/inst/ikr/RSNA2007/<strong>MRA</strong><strong>acquisition</strong><br />
Question to Dr. Martin Prince<br />
How do you prevent venous overlay?<br />
Decreased Venous<br />
Contamination Using Thigh<br />
Compression on Peripheral <strong>MRA</strong><br />
• Thigh cuffs with long extension tubing<br />
• Inflation pressure = 60 mmHg<br />
• Inflate just prior to mask <strong>acquisition</strong><br />
• Venous contamination is delayed<br />
• ↑ calf station to 60 seconds<br />
Zhang et al: AJR 2004; 183:1041-10<br />
• Supra-systolic in arm (200mmHghand <strong>MRA</strong>)<br />
Wentz et al: Lancet 2003;361:49-50<br />
Bilecen et al: AJR 2004; 182:180-2<br />
• Sub-systolic in legs (40 to 60 mm Hg)<br />
Meaney et al: US Patent 5,924,987<br />
Herborn et al: Radiology 2004; 230:872-8<br />
Bilecen et al: JMRI 2004; 20:347-51<br />
Vogt et al: Radiology 2004; 233:913-20<br />
60 mm<br />
Hg<br />
w/o thigh compression<br />
with thigh compression<br />
Question to Dr. Tom Grist<br />
Benefits of time-resolved imaging protocol<br />
When do you use time-resolved imaging?<br />
Left Popliteal Occlusion
Benefits of time-resolved imaging protocol<br />
Benefits of time-resolved imaging protocol<br />
Causes of early venous enhancement<br />
• Ulceration<br />
• Phlebitis<br />
• Neuropathic joint<br />
• Reduced muscle mass<br />
Neuropathic joint with hyper-enhancement<br />
enhancement<br />
58 year-old male post repair of ASD and PAPVR<br />
TR – 3.3 ms<br />
TE – 0.9 ms<br />
Flip - 30 0<br />
BW – 62.5 kHz<br />
FOV - 400 x 400 mm<br />
Matrix – 256 x 192<br />
24 x 10 mm slices (Zip 2)<br />
31 x 0:02.9 time frames<br />
15 cc at 3.0 cc/s Gadolinium<br />
Relative SNR% - 245%<br />
Scan Time 1:53 (Mask – 0:13)<br />
“Pause On” with separate mask and post-contrast<br />
<strong>acquisition</strong> breath-hold<br />
Incidentally diagnosed Right Pulmonary Venous Varix<br />
45 year-old patient with chronic pelvic pain<br />
Radial <strong>acquisition</strong>: HYPR<br />
• HYPR: HighlY constrained back-PRojection<br />
• Single radial readout used to reconstruct<br />
projection data<br />
• Very efficient for time-resolved <strong>MRA</strong><br />
TRICKS<br />
Radial readout<br />
(rotating lines)<br />
Mistretta CA, Wieben O, Velikina J, Block W, Perry J, Wu Y, Johnson K, Wu Y. Highly<br />
constrained backprojection for time-resolved MRI. Magn Reson Med. 2006;55:30-40.