WHO guidelines for the management of postpartum haemorrhage ...
WHO guidelines for the management of postpartum haemorrhage ...
WHO guidelines for the management of postpartum haemorrhage ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>WHO</strong> <strong>guidelines</strong> <strong>for</strong> <strong>the</strong> <strong>management</strong> <strong>of</strong> <strong>postpartum</strong> <strong>haemorrhage</strong> and retained placenta<br />
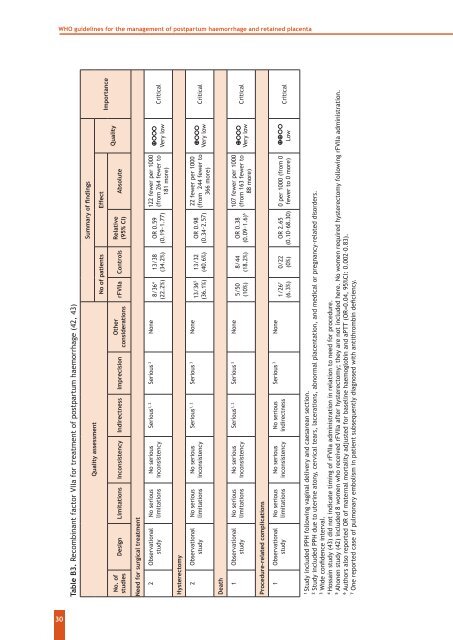
Table B3. Recombinant factor VIIa <strong>for</strong> treatment <strong>of</strong> <strong>postpartum</strong> <strong>haemorrhage</strong> (42, 43)<br />
No. <strong>of</strong><br />
studies<br />
Quality assessment<br />
Design Limitations Inconsistency Indirectness Imprecision<br />
O<strong>the</strong>r<br />
considerations<br />
Summary <strong>of</strong> findings<br />
No <strong>of</strong> patients Effect<br />
rFVIIa Controls<br />
Relative<br />
(95% CI)<br />
Absolute<br />
Quality<br />
Importance<br />
Need <strong>for</strong> surgical treatment<br />
2 Observational<br />
study<br />
No serious<br />
limitations<br />
No serious<br />
inconsistency<br />
Serious 1, 2 Serious 3 None<br />
8/36 4<br />
(22.2%)<br />
13/38<br />
(34.2%)<br />
OR 0.59<br />
(0.19–1.77)<br />
122 fewer per 1000<br />
(from 264 fewer to<br />
181 more)<br />
Very low<br />
Critical<br />
Hysterectomy<br />
2 Observational<br />
study<br />
No serious<br />
limitations<br />
No serious<br />
inconsistency<br />
Serious 1, 2 Serious 3 None<br />
13/36 5<br />
(36.1%)<br />
13/32<br />
(40.6%)<br />
OR 0.98<br />
(0.34–2.57)<br />
22 fewer per 1000<br />
(from 244 fewer to<br />
366 more)<br />
Very low<br />
Critical<br />
Death<br />
1 Observational<br />
study<br />
No serious<br />
limitations<br />
No serious<br />
inconsistency<br />
Serious 1, 2 Serious 3 None<br />
5/50<br />
(10%)<br />
8/44<br />
(18.2%)<br />
107 fewer per 1000<br />
OR 0.38<br />
(from 163 fewer to<br />
(0.09–1.6) 6 88 more)<br />
Very low<br />
Critical<br />
Procedure-related complications<br />
1 Observational<br />
study<br />
No serious<br />
limitations<br />
No serious<br />
inconsistency<br />
No serious<br />
indirectness<br />
Serious 3 None<br />
1/26 7<br />
(6.3%)<br />
0/22<br />
(0%)<br />
OR 2.65<br />
(0.10–68.30)<br />
0 per 1000 (from 0<br />
fewer to 0 more) Low<br />
Critical<br />
1<br />
Study included PPH following vaginal delivery and caesarean section.<br />
2<br />
Study included PPH due to uterine atony, cervical tears, lacerations, abnormal placentation, and medical or pregnancy-related disorders.<br />
3<br />
Wide confidence interval.<br />
4<br />
Hossain study (43) did not indicate timing <strong>of</strong> rFVIIa administration in relation to need <strong>for</strong> procedure.<br />
5<br />
Ahonen study (42) included 8 women who received rFVIIa after hysterectomy; <strong>the</strong>y are not included here. No women required hysterectomy following rFVIIa administration.<br />
6<br />
Authors also reported OR <strong>of</strong> maternal mortality adjusted <strong>for</strong> baseline haemoglobin and aPTT (OR=0.04, 95%CI: 0.002–0.83).<br />
7<br />
One reported case <strong>of</strong> pulmonary embolism in patient subsequently diagnosed with antithrombin deficiency.<br />
30