Commonwealth Care Member Guide - BMC HealthNet Plan
Commonwealth Care Member Guide - BMC HealthNet Plan
Commonwealth Care Member Guide - BMC HealthNet Plan
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
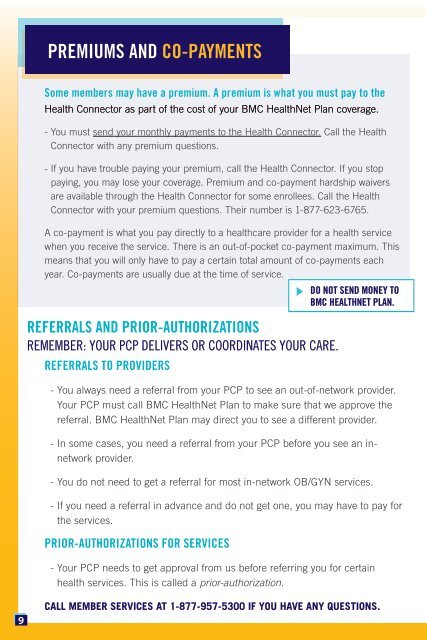
PREMIUMS AND CO-PAYMENTS<br />
Some members may have a premium. A premium is what you must pay to the<br />
Health Connector as part of the cost of your <strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong> coverage.<br />
- You must send your monthly payments to the Health Connector. Call the Health<br />
Connector with any premium questions.<br />
- If you have trouble paying your premium, call the Health Connector. If you stop<br />
paying, you may lose your coverage. Premium and co-payment hardship waivers<br />
are available through the Health Connector for some enrollees. Call the Health<br />
Connector with your premium questions. Their number is 1-877-623-6765.<br />
A co-payment is what you pay directly to a healthcare provider for a health service<br />
when you receive the service. There is an out-of-pocket co-payment maximum. This<br />
means that you will only have to pay a certain total amount of co-payments each<br />
year. Co-payments are usually due at the time of service.<br />
DO NOT SEND MONEY TO<br />
<strong>BMC</strong> HEALTHNET PLAN.<br />
REFERRALS AND PRIOR-AUTHORIZATIONS<br />
REMEMBER: YOUR PCP DELIVERS OR COORDINATES YOUR CARE.<br />
REFERRALS TO PROVIDERS<br />
- You always need a referral from your PCP to see an out-of-network provider.<br />
Your PCP must call <strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong> to make sure that we approve the<br />
referral. <strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong> may direct you to see a different provider.<br />
- In some cases, you need a referral from your PCP before you see an innetwork<br />
provider.<br />
- You do not need to get a referral for most in-network OB/GYN services.<br />
- If you need a referral in advance and do not get one, you may have to pay for<br />
the services.<br />
PRIOR-AUTHORIZATIONS FOR SERVICES<br />
- Your PCP needs to get approval from us before referring you for certain<br />
health services. This is called a prior-authorization.<br />
9<br />
CALL MEMBER SERVICES AT 1-877-957-5300 IF YOU HAVE ANY QUESTIONS.