Journal_1_2014_final_WEB
Journal_1_2014_final_WEB
Journal_1_2014_final_WEB
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Science, Practice and Education<br />
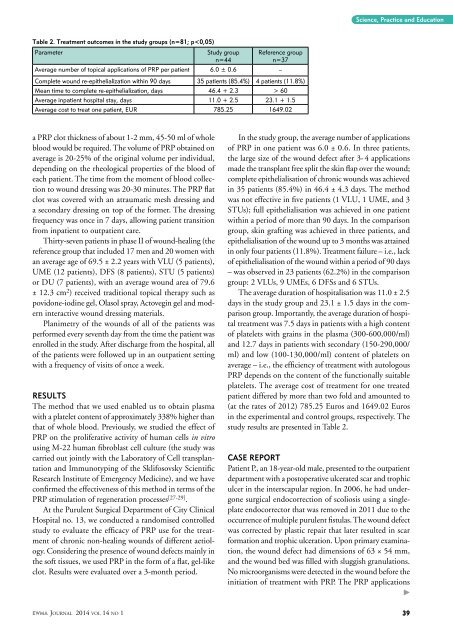
Table 2. Treatment outcomes in the study groups (n=81; p 60<br />
Average inpatient hospital stay, days 11.0 + 2.5 23.1 + 1.5<br />
Average cost to treat one patient, EUR 785.25 1649.02<br />
a PRP clot thickness of about 1-2 mm, 45-50 ml of whole<br />
blood would be required. The volume of PRP obtained on<br />
average is 20-25% of the original volume per individual,<br />
depending on the rheological properties of the blood of<br />
each patient. The time from the moment of blood collection<br />
to wound dressing was 20-30 minutes. The PRP flat<br />
clot was covered with an atraumatic mesh dressing and<br />
a secondary dressing on top of the former. The dressing<br />
frequency was once in 7 days, allowing patient transition<br />
from inpatient to outpatient care.<br />
Thirty-seven patients in phase II of wound-healing (the<br />
reference group that included 17 men and 20 women with<br />
an average age of 69.5 ± 2.2 years with VLU (5 patients),<br />
UME (12 patients), DFS (8 patients), STU (5 patients)<br />
or DU (7 patients), with an average wound area of 79.6<br />
± 12.3 cm 2 ) received traditional topical therapy such as<br />
povidone-iodine gel, Olasol spray, Actovegin gel and modern<br />
interactive wound dressing materials.<br />
Planimetry of the wounds of all of the patients was<br />
performed every seventh day from the time the patient was<br />
enrolled in the study. After discharge from the hospital, all<br />
of the patients were followed up in an outpatient setting<br />
with a frequency of visits of once a week.<br />
Results<br />
The method that we used enabled us to obtain plasma<br />
with a platelet content of approximately 338% higher than<br />
that of whole blood. Previously, we studied the effect of<br />
PRP on the proliferative activity of human cells in vitro<br />
using M-22 human fibroblast cell culture (the study was<br />
carried out jointly with the Laboratory of Cell transplantation<br />
and Immunotyping of the Sklifosovsky Scientific<br />
Research Institute of Emergency Medicine), and we have<br />
confirmed the effectiveness of this method in terms of the<br />
PRP stimulation of regeneration processes [27-29] .<br />
At the Purulent Surgical Department of City Clinical<br />
Hospital no. 13, we conducted a randomised controlled<br />
study to evaluate the efficacy of PRP use for the treatment<br />
of chronic non-healing wounds of different aetiology.<br />
Considering the presence of wound defects mainly in<br />
the soft tissues, we used PRP in the form of a flat, gel-like<br />
clot. Results were evaluated over a 3-month period.<br />
In the study group, the average number of applications<br />
of PRP in one patient was 6.0 ± 0.6. In three patients,<br />
the large size of the wound defect after 3- 4 applications<br />
made the transplant free split the skin flap over the wound;<br />
complete epithelialisation of chronic wounds was achieved<br />
in 35 patients (85.4%) in 46.4 ± 4.3 days. The method<br />
was not effective in five patients (1 VLU, 1 UME, and 3<br />
STUs); full epithelialisation was achieved in one patient<br />
within a period of more than 90 days. In the comparison<br />
group, skin grafting was achieved in three patients, and<br />
epithelialisation of the wound up to 3 months was attained<br />
in only four patients (11.8%). Treatment failure – i.e., lack<br />
of epithelialisation of the wound within a period of 90 days<br />
– was observed in 23 patients (62.2%) in the comparison<br />
group: 2 VLUs, 9 UMEs, 6 DFSs and 6 STUs.<br />
The average duration of hospitalisation was 11.0 ± 2.5<br />
days in the study group and 23.1 ± 1.5 days in the comparison<br />
group. Importantly, the average duration of hospital<br />
treatment was 7.5 days in patients with a high content<br />
of platelets with grains in the plasma (300-600,000/ml)<br />
and 12.7 days in patients with secondary (150-290,000/<br />
ml) and low (100-130,000/ml) content of platelets on<br />
average – i.e., the efficiency of treatment with autologous<br />
PRP depends on the content of the functionally suitable<br />
platelets. The average cost of treatment for one treated<br />
patient differed by more than two fold and amounted to<br />
(at the rates of 2012) 785.25 Euros and 1649.02 Euros<br />
in the experimental and control groups, respectively. The<br />
study results are presented in Table 2.<br />
Case report<br />
Patient P., an 18-year-old male, presented to the outpatient<br />
department with a postoperative ulcerated scar and trophic<br />
ulcer in the interscapular region. In 2006, he had undergone<br />
surgical endocorrection of scoliosis using a singleplate<br />
endocorrector that was removed in 2011 due to the<br />
occurrence of multiple purulent fistulas. The wound defect<br />
was corrected by plastic repair that later resulted in scar<br />
formation and trophic ulceration. Upon primary examination,<br />
the wound defect had dimensions of 63 × 54 mm,<br />
and the wound bed was filled with sluggish granulations.<br />
No microorganisms were detected in the wound before the<br />
initiation of treatment with PRP. The PRP applications<br />
<br />
EWMA <strong>Journal</strong> <strong>2014</strong> vol 14 no 1 39