Download PDF - Emerson Hospital
Download PDF - Emerson Hospital
Download PDF - Emerson Hospital
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
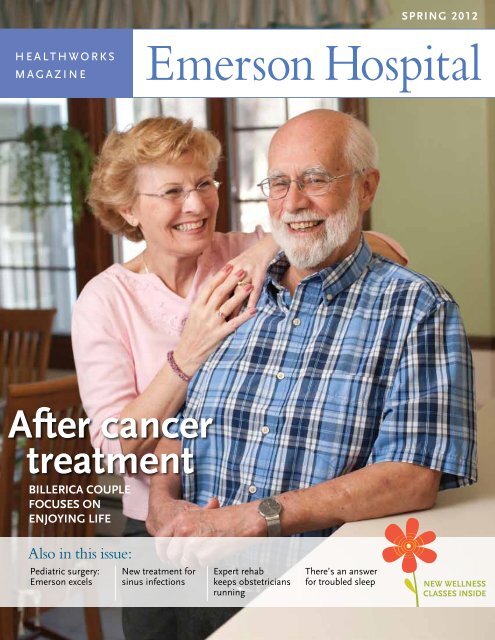
SPRING 2012<br />
healthworks<br />
magazine<br />
Title<br />
After cancer<br />
treatment<br />
Billerica couple<br />
focuses on<br />
enjoying life<br />
Also in this issue:<br />
Pediatric surgery:<br />
<strong>Emerson</strong> excels<br />
New treatment for<br />
sinus infections<br />
Expert rehab<br />
keeps obstetricians<br />
running<br />
There’s an answer<br />
for troubled sleep<br />
New Wellness<br />
Classes Inside
A Letter from<br />
Christine Schuster<br />
Dear Friends:<br />
As you will read in our cover article, <strong>Emerson</strong><br />
<strong>Hospital</strong> continues to bring world-class care to<br />
the community we serve. Our long-standing relationship<br />
with Massachusetts General <strong>Hospital</strong><br />
in cancer care recently expanded to include a<br />
collaboration with medical oncology. We are<br />
pleased to bring all cancer services under one<br />
umbrella, the Mass General Cancer Center at<br />
<strong>Emerson</strong> <strong>Hospital</strong>-Bethke.<br />
Thoughtful steps lead to a<br />
Concord family puts their trust in surgeon’s experience<br />
Brian Callahan, MD,<br />
a general surgeon<br />
at <strong>Emerson</strong>, helped<br />
Zoé Green’s parents<br />
with diagnosis and<br />
treatment decisions<br />
related to her recent<br />
appendectomy.<br />
This issue of HealthWorks also features a new<br />
technology and a new program, in keeping with<br />
<strong>Emerson</strong>’s Premium Care, Personal Touch philosophy.<br />
Balloon catheter dilation is a premium care,<br />
minimally invasive procedure that provides relief<br />
to individuals who suffer from chronic sinus infections.<br />
Our palliative care program addresses<br />
the symptoms of serious illness by focusing on<br />
what is known as “comfort care,” offering the<br />
personal touch you expect to find at <strong>Emerson</strong>.<br />
Throughout the health care industry, there is an<br />
increasing emphasis on prevention—all the ways<br />
that we can maintain health and prevent the development<br />
of medical problems. If your goal is<br />
to do something good for your health, we are<br />
here to help. Our Health & Wellness classes<br />
cover a range of topics and appeal to all ages.<br />
I hope to see you at our annual 5K Run-Walk<br />
for Cancer, sponsored by the <strong>Emerson</strong> <strong>Hospital</strong><br />
Auxiliary on Saturday, June 2. Proceeds benefit<br />
cancer services at <strong>Emerson</strong>.<br />
Christine C. Schuster<br />
President and CEO<br />
<strong>Emerson</strong> <strong>Hospital</strong> is an acute care medical center<br />
located in Concord with health centers in Bedford,<br />
Groton, Sudbury and Westford. It is well known for<br />
its medical and surgical specialists, outstanding nursing<br />
care and patient-centered services, including the<br />
Clough Birthing Center, the Mass General Cancer<br />
Center at <strong>Emerson</strong> <strong>Hospital</strong>-Bethke, the Polo Emergency<br />
Center and the Clough Surgical Center.<br />
Zoé Green seemed out of sorts that January afternoon. Initially, her symptoms<br />
made her parents think she had picked up stomach flu at school. But they were soon<br />
thinking differently.<br />
“When she got home from school that day, Zoé complained of a stomach ache and<br />
had a mild fever,” recalls Jared Green, her father. “That evening, she threw up several<br />
times, which led us to assume she had norovirus.” The highly contagious stomach flu<br />
has been pervasive during the past two winters.<br />
The next morning, Zoé felt better. However, a new symptom appeared: pain in the<br />
lower righthand side of her stomach. “We started thinking it was appendicitis,”<br />
says Mr. Green, noting that an early morning call to the office of Zoé’s pediatrician,<br />
Stephen Jenkins, MD, directed them to the Emergency Department at <strong>Emerson</strong>.<br />
In children, diagnosing appendicitis can be a challenge<br />
The Greens, who live in Concord, soon discovered that appendicitis can be difficult<br />
to diagnose, especially in children. Even if a child is old enough to describe the<br />
symptoms, such as where the pain is and what it feels like, children are not as likely<br />
as adults to have the classic signs of appendicitis, including fever, loss of appetite and<br />
elevated white blood cells. “You need to look at the individual situation,” says<br />
2<br />
www.emersonhospital.org
diagnosis<br />
– and successful<br />
pediatric surgery<br />
Brian Callahan, MD, a general surgeon at <strong>Emerson</strong>, “and you need to perform the<br />
right test at the right time.”<br />
The right tests for a seven-year-old girl – or any child – include a blood test and ultrasound<br />
exam. In Zoé’s case, neither one revealed the inflammation associated with<br />
appendicitis. Although she reacted when Dr. Callahan tapped on her stomach, it<br />
was not clear that Zoé’s problem was appendicitis. “Many kids develop enlarged<br />
lymph nodes that produce pain in the lower right side, similar to appendicitis,”<br />
Dr. Callahan explains.<br />
At that point, a CT scan may well have revealed the problem. But as Dr. Callahan<br />
told the Greens, the test should be used judiciously in children. “When children<br />
have a CT scan performed, the radiation dose is adjusted for their age and size,” he<br />
says. “Still, we worry about exposing children to radiation out of concern that it<br />
may predispose them to cancer later on.”<br />
Dr. Callahan brings perspective from having trained as a surgeon when sophisticated<br />
imaging, such as CT scans, were not available. “Back then, surgery served as both<br />
the diagnostic test and the treatment,” he notes. “We often operated – and still do –<br />
to avoid missing an appendix that goes on to rupture.” A ruptured or burst appendix<br />
can produce peritonitis, a painful and potentially life-threatening infection in the<br />
intestinal tract. “Also, we worry about the appendix rupturing in females because<br />
the fallopian tubes and ovaries are located nearby and can be damaged.”<br />
“Our initial impulse was that Zoé should have a CT scan,” says Mr. Green, “but we<br />
shared Dr. Callahan’s concern about exposing her to radiation and appreciated the<br />
fact that he steered us away from it. He told us he was 75 percent certain that Zoé<br />
had appendicitis, so we decided to proceed with surgery.” It wasn’t an easy decision,<br />
he adds. “We trusted Dr. Callahan and Dr. Street, her anesthesiologist.” James<br />
Street, PhD, MD, is chief of anesthesia at <strong>Emerson</strong>.<br />
The next question was whether Zoé’s operation should be performed in the traditional<br />
way, with one incision, or laparoscopically, the more minimally invasive<br />
approach. “We expected the surgery would be performed laparoscopically,” says<br />
Mr. Green, “but Dr. Callahan suggested the traditional surgery.”<br />
“A laparoscopic appendectomy leaves someone with four small scars scattered<br />
around the abdomen, rather than one scar that is hidden below the bikini line,” says<br />
Dr. Callahan, noting that this often matters to girls and women. “Also, in children<br />
there isn’t a significant difference in recovery time when you compare the two operations.”<br />
When he performed Zoé’s surgery, Dr. Callahan determined that she had a<br />
retrocecal appendix – that is, not in the usual location. The finding, not uncommon,<br />
explained why the ultrasound exam had not revealed her inflamed appendix.<br />
Zoé stayed two nights at <strong>Emerson</strong>, and her father stayed with her. “The nursing<br />
care was very high-quality,” says Mr. Green.<br />
Zoé appreciated how she was treated at <strong>Emerson</strong>. “When I first got to the hospital,<br />
I didn’t know what was happening,” she recalls. “But by the time I went for the<br />
surgery, I wasn’t really scared. I was nervous, but not too much because the doctors<br />
explained what was going to happen.” Her mother is French, so Zoé made a drawing<br />
of the Eiffel Tower and mailed it to Dr. Callahan as a way to say “thanks.”<br />
“In hindsight, we know that we made the right decision,” says Mr. Green. “We<br />
appreciate all the help Dr. Callahan gave us that day.”<br />
Children often head into the operating room with Mallory<br />
Harrison, a member of the Pediatric Intervention Team.<br />
<strong>Emerson</strong> has pediatric surgery covered<br />
For children having surgery, <strong>Emerson</strong>’s system of care is<br />
designed to deliver a high-quality care experience.<br />
<strong>Hospital</strong> staff provide all the support that the child and<br />
the parents need.<br />
When Zoé Green and her parents arrived at <strong>Emerson</strong><br />
<strong>Hospital</strong>’s Emergency Department (ED) that morning,<br />
she was examined by ED staff who receive consistently<br />
high marks for the care they provide to children. Soon, a<br />
member of the Pediatric Intervention Team (PIT) – staff<br />
whose focus is to help children and families cope with<br />
the hospital experience – appeared with the hospital’s<br />
famous coping kit, a bag of age-appropriate toys, something<br />
the Greens appreciated.<br />
Once her parents decided to proceed with surgery, a<br />
member of the PIT explained to Zoé what would happen,<br />
including that she would wear a mask and select an anesthesia<br />
“flavor,” and accompanied her to the operating<br />
room. Dr. Street spent time with Zoé and her parents to<br />
explain anesthesia and describe the techniques and<br />
monitoring used to ensure her safety.<br />
“When a child has surgery, you’re taking care of the<br />
whole family,” says Dr. Street, who oversees a staff of<br />
board-certified anesthesiologists and certified registered<br />
nurse-anesthetists, most with more than ten years of experience.<br />
“We provide excellent anesthesia care; however,<br />
parents need to be reassured that their child will be<br />
safe. Part of my job is to take the worry off their<br />
shoulders.”<br />
Parents are not the only ones with questions about anesthesia.<br />
“Even small kids will sometimes ask very<br />
thoughtful questions, such as ‘am I going to wake up<br />
during surgery?’ or ‘how do you know I’m really asleep?’”<br />
says Dr. Street. “So I describe in simple terms how we<br />
carefully monitor their vital signs and level of consciousness<br />
throughout their surgery and adjust the level of anesthesia<br />
accordingly.”<br />
During her two-day stay, Zoé was cared for by experienced<br />
pediatric hospitalists – pediatricians who are onsite<br />
at <strong>Emerson</strong> 24 hours a day – and pediatric nursing<br />
staff on the hospital’s newly renovated pediatric unit.<br />
3
Ann Snow, RN,<br />
was singled out<br />
for an important<br />
honor.<br />
ann snow, rn, and radiation<br />
oncology team are honored<br />
The Mass General Cancer Center has a special way of<br />
honoring those who have helped advance the fight<br />
against cancer in a meaningful way. Each year, they<br />
select 100 individuals, groups and organizations for<br />
their extraordinary contributions to the cancer community<br />
and showcase them at the annual fundraiser,<br />
known as the one hundred, held on June 7 at the<br />
Westin Boston Waterfront.<br />
Those who are acquainted with Ann Snow, RN, manager<br />
of radiation oncology nursing at the Mass<br />
General Cancer Center at <strong>Emerson</strong> <strong>Hospital</strong>-Bethke,<br />
weren’t surprised to hear that she was selected as a<br />
member of the one hundred. Her colleagues, the<br />
entire radiation oncology team at <strong>Emerson</strong>, were also<br />
selected to be among the one hundred recognized<br />
this year. The radiation oncology team includes physicians,<br />
nurses, radiation therapists and technical<br />
and administrative staff.<br />
Ms. Snow is quick to note that her nomination is a<br />
reflection of what they provide together every day. “I<br />
was just blown away by it,” she says of hearing that<br />
she would be honored. “But it’s because of the people<br />
I work with, from the top down. For example, our<br />
radiation therapists are outstanding; we couldn’t do<br />
it without them.”<br />
Ms. Snow has been there since <strong>Emerson</strong> first opened<br />
a cancer center in 1997. “Thanks to the technology,<br />
treatment has improved so much since then,” she<br />
says. “We see far fewer complications, and we know<br />
how to treat side effects with IV hydration and medications<br />
for nausea and pain.”<br />
Being honored as a member of the one hundred is a<br />
thrill, she says. “Along with the other nursing staff, I<br />
try to guide our patients through the experience by<br />
serving as a coach and friend. I think I can speak for<br />
all my colleagues in radiation oncology in saying that<br />
the patients make you come back every day. We<br />
make a difference in their lives.”<br />
Together – that is how Donald and Paula Beardsley faced his diagnosis, treatment and recovery.<br />
Couple faces esophageal cancer<br />
and finds ways to enjoy life<br />
Last summer, Donald Beardsley developed a suspicious pain near his collarbone and<br />
decided to make an appointment with his primary care physician. Nagy Mikael, MD,<br />
MPH, was concerned that Mr. Beardsley had lost 30 pounds since his last appointment.<br />
Mr. Beardsley’s wife, Paula, knew that her husband, who typically has a good appetite,<br />
had started to feel full well before he had finished a meal. The couple also wondered<br />
why Mr. Beardsley’s long-standing gastric esophageal reflux disease (GERD) had suddenly<br />
disappeared and shared this concern with Dr. Mikael.<br />
Dr. Mikael referred Mr. Beardsley for testing at the office of Raj Devarajan, MD, an<br />
<strong>Emerson</strong> gastroenterologist. “When I look back, I realize that Don and I went into that<br />
appointment so blindly,” says Mrs. Beardsley. “I had no fear that there was anything<br />
life-threatening going on. I just thought Don’s GERD had probably come back.”<br />
But there was more going on. The diagnosis was stage III esophageal cancer – cancer<br />
that had spread to the lymph nodes and adjacent structures. In Mr. Beardsley’s case,<br />
the cancer was blocking his esophagus and had spread to the top of his stomach.<br />
“Hearing ‘you’ve got cancer’ is a real smack upside the head,” says Mr. Beardsley. “As<br />
time went on, and I began treatment, I accepted the fact that I had cancer. There was<br />
nothing I could do to change it. Overall, I think that period of time was more stressful<br />
for Paula than for me.”<br />
4
collaboration with the mass general cancer center expands<br />
The long-standing relationship between <strong>Emerson</strong> <strong>Hospital</strong> and Massachusetts<br />
General <strong>Hospital</strong> recently expanded to include a collaboration with medical oncology.<br />
Since 1997, area residents have benefited from <strong>Emerson</strong>’s joint program<br />
with Mass General. In bringing all cancer services under one umbrella, the<br />
Mass General Cancer Center at <strong>Emerson</strong> <strong>Hospital</strong>-Bethke is designed to achieve<br />
highly coordinated care and incorporate a number<br />
of important new features.<br />
“We’re enhancing several services, including social<br />
work, pain management and nutrition support,”<br />
notes Jon DuBois, MD, medical director of<br />
medical oncology. “Also, our clinical trials program<br />
at <strong>Emerson</strong> will be strengthened by access<br />
to the much larger one at the Mass General<br />
Cancer Center.” Communication among clinicians<br />
will benefit from the sharing of common<br />
electronic medical records.<br />
David Ryan, MD, clinical director at the Mass<br />
General Cancer Center, who now works closely with Dr. DuBois and the other<br />
medical oncologists, including Ewa Niemierko, MD, Humberto Rossi, MD, and<br />
Susan Sajer, MD, cites several behind-the-scenes features. “The oncology pharmacy<br />
is currently being upgraded, and we are developing a more collaborative<br />
relationship on tumor boards with our <strong>Emerson</strong> colleagues,” notes Dr. Ryan in<br />
reference to the forum where treatment plans are reviewed by a team of clinical<br />
experts, including medical, surgical and radiation oncologists. Additionally,<br />
Mass General surgeons who provide subspecialty care in areas not currently<br />
offered, such as head and neck cancer, are expected to operate at <strong>Emerson</strong> in<br />
the near future.<br />
Mass General Cancer Center at <strong>Emerson</strong> <strong>Hospital</strong>-Bethke<br />
physicians include (left to right): Robin Schoenthaler, MD,<br />
Susan Sajer, MD, Humberto Rossi, MD, Ewa Niemierko,<br />
MD, Jon DuBois, MD, and Jack McGrath, MD.<br />
Paul Busse, MD, clinical director at Mass General, who oversees radiation oncology<br />
at <strong>Emerson</strong>, says there are benefits to working under the same umbrella.<br />
“The closeness among physicians leads to a common sense of mission that<br />
patients and family members appreciate,” says Dr. Busse. “They are relieved<br />
to see that we’re all in the room together sharing the same information about<br />
the patient.”<br />
The strong working bond between Dr. Busse and<br />
Dr. McGrath benefits patients. “I am at Mass<br />
General weekly to connect with my colleagues<br />
and make sure the quality of care in Concord is<br />
the same as in Boston,” says Dr. McGrath. He<br />
cites the installation last year of a state-of-the-art<br />
linear accelerator in collaboration with Mass<br />
General as evidence of a strong commitment.<br />
“Mass General is serious about investing in<br />
<strong>Emerson</strong> in order to keep the quality of the care<br />
very high.”<br />
All agree that the goal is for patients to continue to receive their care in the community.<br />
“We regularly encourage patients to receive their care close to home at<br />
<strong>Emerson</strong>,” Dr. Ryan notes. “But our new, expanded collaboration with <strong>Emerson</strong><br />
provides patients with more coordinated care with clinicians at Mass General’s<br />
main campus downtown should they need access to more specialized<br />
services.”<br />
According to Dr. DuBois, the new collaboration should make patients feel more<br />
confident than ever about the cancer care that is available at <strong>Emerson</strong>. “Our<br />
center has always been known for providing high-quality care with a personal<br />
touch,” he says.<br />
Decisions aimed at living well<br />
Once the Billerica couple absorbed the news, they quickly began<br />
discussions about treatment. After consultation with his surgeon; Jack<br />
McGrath, MD, medical director of radiation oncology; and Susan<br />
Sajer, MD, his medical oncologist, Mr. Beardsley elected to proceed<br />
with a combination of chemotherapy and radiation. If he had a good<br />
response to treatment, he would then undergo surgery.<br />
“I explained to Mr. Beardsley that, for his type of cancer, this threepart<br />
approach was the standard of care,” Dr. Sajer notes. “There is<br />
likely to be a small benefit to having surgery after the initial combination<br />
therapy.”<br />
Dr. Sajer described the six-week treatment regimen designed to reduce<br />
the size of his esophageal tumor. “It consists of weekly chemotherapy<br />
and radiation five days a week,” she says. “The coordination<br />
of that care must be perfect.” Prior to beginning treatment, Mr.<br />
Beardsley had a feeding tube inserted in his intestine that bypassed the<br />
stomach. It would ensure his ability to eat despite potential complications.<br />
Also, he would need it if he chose to have surgery later.<br />
“He’s the Energizer bunny,” says his wife of 24 years. “Don has<br />
come back from all kinds of medical maladies. We began hoping he’d<br />
bounce back from this one, too.”<br />
Hitting bottom and bouncing back<br />
Initially, Mr. Beardsley’s treatment was uneventful. Despite warnings<br />
that he would encounter eating problems, he helped himself to anything<br />
he wanted. “Dr. McGrath kept shaking his head and saying ‘you’re eating<br />
what?’ when we described Don’s diet,” says Mrs. Beardsley.<br />
Throughout the summer, the couple found ways to enjoy themselves.<br />
“To get away from the elephant in the room – Don’s cancer – we’d take<br />
our motor home to our favorite campground in Littleton,” Mrs.<br />
Beardsley recalls. “We drove our RV over to <strong>Emerson</strong>, Don would run<br />
in to have his radiation treatment, and in a few minutes we were on our<br />
way. After escaping for the weekend, we felt like our old selves again.”<br />
Once his treatment was over, Mr. Beardsley could no longer eat or<br />
drink and depended entirely on the feeding tube to receive nutrition.<br />
He became dehydrated, which necessitated regular visits to <strong>Emerson</strong><br />
to receive IV fluids. Ena Sandler, RD, an <strong>Emerson</strong> dietitian, worked<br />
with Mr. Beardsley to keep him from losing weight. “She tried her<br />
darnedest to find things like smoothies to pump me up,” says Mr.<br />
Beardsley. “I couldn’t get any food past my nose.”<br />
Mrs. Beardsley was sensitive to the situation. “I didn’t want to cook<br />
and have the smell of food in the house, so I became a closet eater,”<br />
she says. “I’d grab something on the way home and eat it in the car.”<br />
> Continued on page 18<br />
5
A leg injury prior to a long-awaited marathon brought Timothy Hale, MD,<br />
to Zoltan Callaghan for a treatment plan that proved successful.<br />
Blithen Davis worked with Rachel Kramer, MD, before and after she ran<br />
in her third marathon in three years.<br />
Successful Sports Rehab<br />
keeps emerson obstetricians running<br />
Two physicians put their trust in <strong>Emerson</strong> Center’s physical therapy<br />
Sports injuries are tough – physically and mentally. Committed athletes, distance runners and gym addicts<br />
know it can be devastating to sit on the sideline when you are used to being active.<br />
Timothy Hale, MD, an obstetrician/gynecologist with Kramer<br />
Ob/Gyn Associates, got a taste of that last fall. After many<br />
months of training for a marathon that was just a few weeks<br />
away, he injured his leg and was forced to a grinding halt.<br />
“I was training for the Philadelphia Marathon, which is held at<br />
the end of November, and pushed myself a little too hard,”<br />
explains Dr. Hale. “I thought I had no chance of running in<br />
the marathon.”<br />
After Rachel Kramer, MD, had challenged her office staff and<br />
colleagues to get in shape and choose a specific goal, Dr. Hale<br />
did just that. “I started running in November 2010 and ran my<br />
first race, which was a 10K, a few months later,” he says. “I love<br />
the challenge of setting new goals and achieving them.”<br />
So with his goal of running in Philadelphia slipping away, he<br />
sought help from Zoltan Callaghan, a doctor of physical therapy<br />
at <strong>Emerson</strong>’s Center for Sports Rehabilitation and Specialty<br />
Services in Concord. Dr. Callaghan carefully diagnosed Dr.<br />
Hale and developed a plan to prepare him for the upcoming<br />
marathon. “He had sprained his anterior tibialis, which is near<br />
the muscle that causes ‘shin splints,’” says Dr. Callaghan. “I told<br />
him we would use ice and rest to reduce the inflammation, followed<br />
by stretching and massage before beginning aggressive<br />
strength and endurance training. We did everything we could<br />
within the short timeframe.”<br />
Dr. Hale was immediately impressed with Dr. Callaghan’s<br />
knowledge and positive approach. “He was confident and reassuring,<br />
which is what I needed,” he says, “because I had<br />
6
“The facility is great,<br />
the equipment is great,<br />
and the staff is fantastic.<br />
I feel well taken care of there.”<br />
– Rachel Kramer, MD, Obstetrician/Gynecologist<br />
Their medals tell the story: Timothy Hale, MD, and Rachel Kramer, MD,<br />
are committed runners and fans of Zoltan Callaghan (left) and Blithen Davis<br />
(right), who work at <strong>Emerson</strong>’s Center for Sports Rehabilitation and<br />
Specialty Services in Concord.<br />
invested many months in training. I’ve never received a more<br />
thorough evaluation.”<br />
He was able to run ten pain-free miles prior to the Philadelphia<br />
Marathon, which he went on to complete with no problem.<br />
“Everything Zolie taught me, including stretching and core<br />
work, I now do on a daily basis,” he says. “Meeting him was a<br />
huge wake-up call.”<br />
Slow, steady rehab pays off<br />
For Dr. Kramer, last fall’s Marine Corps Marathon in Arlington,<br />
Virginia, represented her third marathon in three years. “I’ve<br />
been running since 2006 and participate in two triathlons a<br />
year,” she says. When sciatic nerve pain threatened to derail her<br />
plans, Dr. Kramer went to see Blithen Davis, physical therapist.<br />
“Dr. Kramer definitely had disc issues and back pain, but she<br />
did her exercises to keep it under control,” says Ms. Davis,<br />
who runs a spine rehab group at the center. “I knew what the<br />
marathon meant to her, so I gave her the phone number for<br />
the physiatrists at the Lahey Spine Program at <strong>Emerson</strong> <strong>Hospital</strong><br />
– just in case she got into trouble.”<br />
The October marathon went well, but trouble arrived four<br />
weeks later. “I was working out at the gym when the disc ruptured,<br />
which left me in severe pain,” says Dr. Kramer, who used<br />
the phone number Ms. Davis had given her to seek care from<br />
Arthur Lee, MD, who diagnosed her problem, and James<br />
Spinelli, MD, who administered a pain injection. “They are<br />
outstanding; I’ve sent a lot of people to them.”<br />
Once she was out of acute pain, Dr. Kramer’s challenge was to<br />
function during her busy workdays. She again put her trust in<br />
Ms. Davis. “Our goal was to get her moving without irritating<br />
the nerve,” says Ms. Davis. “Dr. Kramer’s work is physical; she<br />
stands during surgery and sits to perform exams. We began<br />
with easy stretching to help her regain mobility in her spine and<br />
then added strengthening exercises from there.”<br />
“Blithen told me what I could and couldn’t do, and that we’d<br />
build back my strength slowly,” says Dr. Kramer. “I saw her<br />
twice a week for two months and did everything she told me,<br />
which included that I would be running again.” On St.<br />
Patrick’s Day, Dr. Kramer ran in the Shamrock Shuffle, a 5K<br />
race in Winchendon, Massachusetts. “I felt great – no pain.”<br />
For the two obstetricians, the Center for Sports Rehabilitation<br />
and Specialty Services at <strong>Emerson</strong> has become a valuable<br />
resource.<br />
“The facility is great, the equipment is great, and the staff is fantastic,”<br />
says Dr. Kramer. “I feel well taken care of there.”<br />
Running tips to live by<br />
• Replace your running shoes every 350-550 miles.<br />
• Perform a dynamic warm-up prior to running and a static stretching<br />
routine after your run.<br />
• Vary your running surface and avoid concrete sidewalks.<br />
• Avoid running on the same side of the road all the time.<br />
• Drink at least half of your body weight in ounces of water per day to<br />
avoid dehydration.<br />
• Seek the advice of your healthcare provider if you have any pain that<br />
lasts longer than two to three weeks.<br />
7
Ayesha Khalid, MD,<br />
an ear, nose and<br />
throat specialist,<br />
performs balloon<br />
catheter dilation, a<br />
minimally invasive<br />
surgical procedure<br />
that opens up the<br />
sinuses and reestablishes<br />
normal<br />
airflow.<br />
New procedure OPENS UP the sinuses<br />
Tiny balloon reestablishes airflow in those with chronic sinus infections<br />
Our sinuses are supposed to be filled with air. But<br />
when they become blocked with fluid, the result<br />
can be a sinus infection, also known as sinusitis.<br />
For some people, the condition appears at the end<br />
of a cold or the flu; for others, it is due to an allergy.<br />
When it keeps happening over time, it is<br />
called recurrent acute sinusitis.<br />
“That is the term we now use when someone has<br />
three or more sinus infections in a year,” explains<br />
Ayesha Khalid, MD, an ear, nose and throat specialist<br />
at <strong>Emerson</strong> <strong>Hospital</strong>. “Inflammation is the<br />
problem. Whether the sinus infections are caused<br />
by bacteria, viruses, fungus, polyps or anatomy —<br />
such as a deviated septum — they all have inflammation<br />
in common.” Symptoms of sinusitis<br />
include generalized facial pain, pressure around<br />
the eyes, pain in the upper teeth and thick drainage<br />
through the nose and down the back of the<br />
throat.<br />
“Too often, antibiotics are prescribed but are only<br />
effective for bacterial infections,” notes Dr. Khalid,<br />
adding that there is no way to determine if the infection<br />
is caused by bacteria. “I’ve seen patients<br />
who have been on antibiotics for as long as a<br />
month with no improvement, which doesn’t make<br />
sense.” A recent study confirmed that antibiotic<br />
treatment is largely ineffective for sinus infections.<br />
Another concern, notes Dr. Khalid, is what can<br />
happen when chronic inflammation goes on un-<br />
8<br />
treated. “In some individuals, it can lead to asthma<br />
and bronchitis,” she says.<br />
So what is someone with recurrent acute sinusitis<br />
to do? Dr. Khalid performs a minimally invasive<br />
surgical procedure called balloon catheter dilation<br />
that debuted about three years ago. “With this<br />
procedure, we use a balloon to carefully open up<br />
the sinuses and reestablish normal airflow,” she<br />
says. “Once the sinuses are open, mucus can be<br />
effectively cleared before an infection occurs.”<br />
It is the first sinus surgery that does not remove<br />
tissue and can be likened to angioplasty, which<br />
uses a balloon to clear blockages in coronary arteries.<br />
Data show that symptom improvement may<br />
last for two years.<br />
Carlisle student finally finds relief<br />
Hillary Cook, a 20-year-old Carlisle resident, had<br />
balloon catheter dilation in December 2011, after a<br />
year of almost non-stop sinus infections. “I got<br />
sick with walking pneumonia and never fully recovered,”<br />
she says. “I had a total of eight sinus infections<br />
with a low-grade fever, even in the summer,<br />
despite taking round after round of antibiotics.”<br />
Ms. Cook was highly motivated to get better: during<br />
her year off from college, she planned to spend<br />
four months in Cambodia, beginning in February<br />
2012, working with a Catholic charity. If she wasn’t<br />
healthy, she couldn’t go. “Dr. Stephen Jenkins, my<br />
Healthy again: after having balloon catheter dilation,<br />
Hillary Cook of Carlisle was able to proceed with her<br />
plan to work in Cambodia this past winter.<br />
pediatrician, recommended that I see Dr. Khalid,<br />
who described the procedure to me. I wasn’t expecting<br />
to have surgery, but she explained everything,<br />
including that <strong>Emerson</strong> has state-of-the-art<br />
technology. Dr. Khalid has a great manner and<br />
immediately put me at ease. I decided to<br />
proceed.”<br />
Dr. Khalid performed balloon catheter dilation,<br />
which requires no hospital stay, as well as septuplasty<br />
to remove cartilage and bone that were further<br />
impeding airflow. Ms. Cook spent a couple of<br />
days recovering and waited for the results. “Within<br />
a week, I felt fantastic,” she says, “and I have remained<br />
healthy and full of energy. I had no idea<br />
> Continued on page 18
health & wellness classes<br />
Visit www.emersonhealthyliving.org to register online. Call 978-287-3777 to register or for more information.<br />
Some classes are ongoing; you can join in at any time.<br />
Classes are located at <strong>Emerson</strong> <strong>Hospital</strong>’s new Integrative Health & Wellness Center, 310 Baker Ave Ext, Concord<br />
(unless otherwise noted).<br />
PREPARE FOR SURGERY, HEAL FASTER WORKSHOP<br />
Prepare for an upcoming surgical or medical procedure: feel calmer,<br />
have less pain and fewer complications and recover sooner. Please call<br />
to arrange a convenient, private workshop.<br />
$95 includes book/relaxation CD<br />
One surgery companion may attend for free.<br />
YOGA & MEDITATION<br />
Reduce stress and tension, improve flexibility and strength and learn<br />
breathing techniques for emotional balance. Wear loose, comfortable<br />
clothing and bring a yoga mat and a sturdy blanket. Not for expectant<br />
mothers. Taught by Pam Vlahakis, registered yoga teacher.<br />
$98 for a seven-week session beginning May 7; classes are Monday<br />
5:30-6:45 pm. Classes are ongoing; you can join in at any time.<br />
GENTLE YOGA<br />
For beginners and experienced practitioners who wish to review postures<br />
with a beginner’s mind. Stretch and tone muscles, release chronic<br />
tension and improve balance and flexibility. Bring a yoga mat. Not suitable<br />
for expectant mothers. Taught by Nancy Dorenfeld, RYT, Kripalucertified<br />
instructor.<br />
$98 for each seven-week session beginning June 15;<br />
classes are Friday, 9:30-10:45 am<br />
NEW!<br />
LUNCH BREAK YOGA for afternoon energy and focus<br />
De-stress from your workday and tap into<br />
your inner energy and serenity. Experience<br />
the union of breath and movement, strength<br />
and balance through a series of postures.<br />
All levels are welcome. Bring a yoga mat.<br />
Taught by Nancy Wolfe, Kripalu-certified<br />
instructor.<br />
$60 for a six-week session beginning June 6;<br />
classes are Thursday, 12:00-1:00 pm<br />
PRENATAL YOGA for a healthier pregnancy<br />
Mixed-level yoga class teaches postural<br />
strengthening, safe stretching, breathing<br />
and relaxation techniques. Bring a yoga<br />
mat, water bottle and signed permission<br />
form from your obstetrician or midwife.<br />
No previous yoga experience required. Led<br />
by Michele O’Toole, RN, certified prenatal<br />
yoga instructor.<br />
$85 for a six-week session beginning:<br />
Monday, May 7, or July 9, 7:00-8:30 pm or<br />
NEW! Thursday, beginning May 10, or June 28, 5:30-7:00 pm<br />
Classes continued on next page
health & wellness classes continued<br />
Visit www.emersonhealthyliving.org to register online. Call 978-287-3777 to register or for more information.<br />
Some classes are ongoing; you can join in at any time.<br />
NEW! POSTNATAL MOM & BABY YOGA<br />
Reconnect in a new way with your body, spirit and breath with other new<br />
moms in a relaxed environment. Begin to regain your pre-baby body.<br />
Students must be at least six weeks post-delivery. Bring a yoga mat,<br />
water bottle and signed permission slip from your obstetrician or midwife,<br />
as well as a soft blanket or bouncy seat for your baby. No previous<br />
yoga experience required. Led by Michele O’ Toole, RN, certified yoga<br />
instructor.<br />
$85 for a six-week session beginning Thursday, May 10, or June 28,<br />
4:00-5:30 pm<br />
BABYSITTING TRAINING<br />
One-day class for ages 10-13 covers everything<br />
you need to know to be a great<br />
babysitter! Certificate of participation<br />
awarded upon completion. Taught by<br />
educator Becky Patterson. Pre-registration<br />
is required. Classes meet on the main<br />
hospital campus.<br />
Choose a Saturday: May 12, June 23, July 14<br />
or August 18<br />
All classes held 9:00 am-2:00 pm<br />
$45 per person or 2/$80 when registering together<br />
TAI CHI<br />
Tai Chi, an ancient Chinese martial art, is practiced to achieve therapeutic<br />
benefits such as reduced pain and to promote balance and overall<br />
strength. The instructor is Ming Wu, PhD.<br />
$98 for an eight-week session<br />
Intermediate/Advanced Level: Wednesday 9:30-10:30 am<br />
Session begins May 9 or July 11<br />
Beginner Level: Thursday, 6:00-7:00 pm<br />
Session begins May 10 or July 12<br />
QI GONG<br />
Qi gong integrates physical postures, breathing techniques and focused<br />
intentions. The gentle, rhythmic movements of qi gong reduce stress,<br />
build stamina and increase vitality. The instructor is Ming Wu, PhD.<br />
$98 for an eight-week session<br />
Intermediate/Advanced Level: Wednesday 10:30-11:30 am<br />
Session begins May 9 or July 11<br />
Beginner Level: Wednesday, 6:00-7:00 pm<br />
Session begins May 9 or July 11<br />
PILATES – mixed level<br />
This exercise program focuses on improving flexibility, strength and<br />
body awareness. Pilates helps develop proper postural alignment and<br />
increases core muscle strength in the abdomen, pelvis and hips for more<br />
uniform and longer, leaner muscles. Bring an exercise mat. Presented<br />
by Tiarra Bentley, IM=X pilates certified instructor.<br />
$98 for each six-week session; Wednesday, 6:00-7:00 pm, beginning<br />
June 13<br />
NEW! QUICK FIT<br />
The class combines strength training exercises with cardio-intervals for<br />
the maximum benefits. Focus on building your core strength, end with<br />
stretches to help soothe your muscles and leave class feeling ready and<br />
energized to start your day. Bring dumbbells (5- or 8-lb), mat, water<br />
bottle and a can-do attitude! The instructor is Holly Kouvo, CPT, CNS.<br />
$90 for each six-week session. Wednesday, 7:15-8:15 am beginning<br />
May 23 or July 11<br />
DANCE AND MOVEMENT FOR PARKINSONS<br />
Based on the acclaimed Dance for PD ® program developed by the<br />
Mark Morris Dance Group and Brooklyn Parkinson Group, this class<br />
utilizes various dance techniques and styles to address balance, flexibility,<br />
movement range and rhythm in a safe and enjoyable environment.<br />
Research has found that dance techniques can be helpful to those with<br />
Parkinson’s. Families, friends and care partners are also welcome to<br />
participate. Taught by Susanne Liebich, who is trained as a Dance for<br />
PD ® instructor.<br />
$75 for a six-week session; Thursday, 10:30-11:30 am beginning May<br />
10. Classes are ongoing; you can join in at any time.<br />
ORGANIZING WORKS!<br />
Our expert organizer will give you the best tips<br />
and ideas on how to bring order to your home<br />
this spring. Reduce the stress and clutter, and<br />
make way for simpler summer days! Presented by<br />
Karen L. Kenney, a professional organizer from<br />
OrganizingWORKS.<br />
$35 Monday, June 4, 7:00-9:00 pm<br />
NEW! POWER OF THE MIND – mind-body connection<br />
Learn techniques that professional and Olympic athletes use and how<br />
your thoughts, words, emotions and intentions have an impact on<br />
school work, relationships, sports, home life and health. This program<br />
is for teens and adults. Presented by Fran Spayne, MA, holistic therapist/life<br />
coach.<br />
$35 Saturday, June 9, 10:00 am -12:30 pm<br />
All Health & Wellness classes must be paid for in full 48 hours in advance of the class. Refunds for cancellations will not be issued after<br />
10 this time.
Visit www.emersonhealthyliving.org to register online. Call 978-287-3777 to register or for more information.<br />
Some classes are ongoing; you can join in at any time.<br />
PRACTICAL AND EFFECTIVE SELF-DEFENSE<br />
for teens and adults<br />
Learn physical and verbal techniques for self-defense in these ongoing<br />
Japanese martial arts classes. Each session builds on the one prior for<br />
returning students; beginners can start at any session.<br />
Evening Seirenkai Karate: June 14-July 19 (half-session for the summer)<br />
Thursday, 7:30-9:00 pm<br />
Attend one free sample class; call for details.<br />
Instructor: Stephen Lisauskas, fourth-degree black belt<br />
$75 for an individual student<br />
ARTHRITIS FOUNDATION EXERCISE PROGRAM SM<br />
This low-impact, joint-safe exercise program<br />
helps decrease arthritis pain and relieve stiffness<br />
while improving balance, your ability to perform<br />
more daily activities and your general health.<br />
Led by Linda May Sieck, certified personal trainer<br />
and Arthritis Foundation-certified instructor.<br />
$75 for an eight-week session beginning<br />
Monday, June 11, 1:30-2:30 pm<br />
HYPNOSIS FOR WEIGHT LOSS<br />
The natural and safe process of hypnosis<br />
uncovers underlying emotions, feelings,<br />
thoughts and attitudes and guides you toward<br />
healthy eating patterns. Presented by Joseph<br />
Packard, board-certified hypnotherapist.<br />
$100 for 3 sessions; classes are Tuesday,<br />
5:00-7:00 pm, June 19, 26, July 3 or July 31,<br />
August 7, August 14<br />
QUIT SMOKING WITH HYPNOSIS<br />
Hypnosis can be a solid tool to help you quit<br />
smoking by reducing the symptoms of withdrawal<br />
and cravings. Come to class with a mindset<br />
to give up the habit tonight. Presented by<br />
Joseph Packard, board-certified hypnotherapist.<br />
$100 for 3 sessions. Classes are Tuesday,<br />
7:00-9:00 pm, on June 19, 26, July 3 or July 31,<br />
August 7, August 14<br />
MINDFULNESS-BASED STRESS REDUCTION PROGRAM<br />
This highly effective eight-week program was<br />
developed by Jon Kabat-Zinn at University of<br />
Massachusetts Medical Center for the treatment<br />
of stress-related disorders. Participants will<br />
learn how to develop their own practice of centering,<br />
grounding and living life in the present<br />
moment. Presented by Patricia Howard, who<br />
has completed teacher training at the Center for<br />
Mindfulness at UMass.<br />
Attend a free introductory lecture Tuesday, June 26, 9:30–11:30 am.<br />
Eight-week program begins Tuesday, July 10, 9:30–11:30 am (plus all<br />
day August 18, 10:00-4:00 pm)<br />
$540 plus $45 for required course materials/CD set<br />
STRESS REDUCTION AND FOCUSING TOOLS FOR TEENS<br />
The teenage years can be times of rapid change. This course will provide<br />
your teen with a new set of skills so they can weather this journey with<br />
more awareness. Presented by Patricia Howard, who has completed<br />
teacher training at the Center for Mindfulness at UMass.<br />
Attend a free introductory lecture: Tuesday, June 26, 12:00–2:00 pm.<br />
Eight-week program begins Tuesday, July 10, 12:00–2:00 pm (plus all<br />
day August 18, 10:00 am-4:00 pm)<br />
$420 (discount for siblings) plus $45 for required course materials/<br />
CD set<br />
NEW! ENLIGHTEN UP: yoga, nutrition and wellness workshop<br />
During this one-evening workshop, you<br />
will learn about a unique wellness weight<br />
management program that integrates<br />
eastern practices, such as yoga and meditation,<br />
and western principles of nutrition<br />
science and psychology. Bring a yoga mat.<br />
Presented by Pam Vlahakis, MEd, RD, a<br />
registered dietitian and registered yoga<br />
teacher.<br />
$25 Tuesday, May 22, or June 12, 6:30-8:00 pm<br />
FINDING FOCUS: ADULT ADD/ADHD<br />
This workshop will address facts and myths about adult attention deficit<br />
disorder, including the impact of attention deficits on productivity, relationships<br />
and life success. Assessment, diagnosis and treatment will<br />
be discussed. Participants will receive information on various resources<br />
and support for adults with ADD/ADHD. Presented by Alexandra<br />
Watkins, LMHC, psychotherapist.<br />
$35 Friday, August 3, 7:00-9:00 pm<br />
<strong>Emerson</strong> <strong>Hospital</strong> reserves the right to cancel any program due to insufficient enrollment or inclement weather. There is no tuition<br />
reduction if a student is unable to attend all classes.<br />
11
health & wellness classes continued<br />
Visit www.emersonhealthyliving.org to register online. Call 978-287-3777 to register or for more information.<br />
Some classes are ongoing; you can join in at any time.<br />
NEW! GAME PLAN – injury prevention for young athletes<br />
Help your kids to stay in the game by learning<br />
techniques that will minimize their chance of<br />
sports injury. Muscular tightness and weakness<br />
increase the risk for injury and will be discussed,<br />
along with off-season conditioning and game<br />
day preparation. The class is appropriate for<br />
all ages and sports. Presented by Nicki Barker,<br />
CPT, from Personal Training International.<br />
$35 Monday, May 21, 6:30-8:30 pm<br />
NEW! PINK RIBBON YOGA – you can still live your life<br />
to the fullest!<br />
This workshop offers physical, emotional and<br />
spiritual support for women who have experienced<br />
breast cancer — recently diagnosed, in treatment<br />
or a long-term survivor. The class includes<br />
healing meditation, breathing techniques, gentle<br />
yogic stretching and relaxation. Taught by Nancy<br />
Dorenfeld, RYT, Kripalu-certified yoga instructor and<br />
survivor. Please bring a yoga mat, small pillow or towel and water.<br />
$20 Saturday, June 2, June 30 or July 21, 10:30 am-12:00 noon<br />
Part of the proceeds from this class will be donated to the National<br />
Breast Cancer Foundation, a non-profit organization devoted to providing<br />
mammograms and breast care to underserved women.<br />
NEW! TOTAL BODY RESISTANCE BAND WORKOUT<br />
Just as effective as free weights, this class will teach you how to maximize<br />
your time and still get a complete workout — anytime, anywhere.<br />
You will learn a variety of exercises for the major muscle groups and<br />
stretch with bands to cool down. Presented by Nicki Barker, CPT, from<br />
Personal Training International. Participants will take home a resistance<br />
band kit. Suitable for all ages and fitness levels. Bring an exercise mat.<br />
$65 for a four-week session beginning Tuesday, May 22, 7:00-8:00 pm<br />
NEW! KIDS FIT+FUN CAMP<br />
This one-week weight-loss day camp for children and adolescents, age<br />
8-14, includes strength training, cardio exercises, fun group games,<br />
education on healthy eating habits, music and more. The instructor is<br />
Holly Kouvo, CPT, CNS. The camp is held at the Fitting Fitness In<br />
studio in Boxborough.<br />
$175 Classes are Monday-Friday 9:00-11:30 am, July 23-27, or<br />
August 6-10<br />
Parent orientation is on Monday, July 23, or August 6, 6:30 pm<br />
REIKI Training Classes<br />
Discover this hands-on energy therapy that can be used to encourage<br />
relaxation, manage pain, provide comfort and promote overall wellness.<br />
Learn to give reiki to yourself, others and pets. Receive reiki practitioner<br />
certification. Approved for five contact hours for nursing for each full<br />
day of attendance. Contact hours for massage therapy and social work<br />
also are available. Presented by Libby Barnett, MSW, reiki master and<br />
teacher at the Reiki Healing Connection.<br />
REIKI-Level I Training: Saturday, June 23, 9:00 am-3:00 pm $145<br />
REIKI-Level II Training: Sunday, June 24, 9:00 am-3:00 pm $160<br />
NEW! OLD AGE ISN’T FOR SISSIES – know your own health<br />
care and the system that supports it<br />
This workshop will include information on<br />
public and private community services and support<br />
for the caregiver. Housing and homecare<br />
options will also be covered along with changes<br />
in the health care system that may affect your<br />
medical care in the future. Presented by Anne<br />
Marie Rowse, CMC, certified care manager and<br />
principal, Senior Care Advisors, LLC. Also presenting<br />
is David Green, MD, critical care medicine and pulmonary<br />
medicine, <strong>Emerson</strong> <strong>Hospital</strong>.<br />
$35 Monday, June 11, 7:00-9:00 pm<br />
NEW! REFLEXOLOGY – the joy of touch<br />
Experience the positive joy of communication and touch through reflex<br />
points on the feet to improve health, relax the mind and invite a feeling<br />
of peacefulness. Program presented by Jane Aire Beckwith, licensed<br />
massage therapist.<br />
$35 Tuesday, June 5, 7:00-9:00 pm<br />
TAMING ANXIETY<br />
This workshop introduces ten effective strategies for managing anxiety<br />
and obsessive thought. We will discuss the importance of addressing<br />
your overall levels of stress and conflict with the goal of lessening anxiety<br />
and unproductive worry. Presented by Frances Bigda-Peyton, EdD,<br />
certified psychoanalyst.<br />
$35 Monday, June 25, 7:00-9:00 pm<br />
NEW! REFLEXOLOGY FOR THE RESPIRATORY AND<br />
CIRCULATORY SYSTEMS<br />
Learn gentle, focused compression on the hands and feet that, along<br />
with deep breathing, can alleviate sinus headaches, allergies and hay<br />
fever. Bring a small pillow. Presented by Jane Aire Beckwith, licensed<br />
massage therapist.<br />
$35 Tuesday, June 26, 7:00-9:00 pm<br />
12
LIVING WELL WITH FIBROMYALGIA<br />
NEW! IMPROVING THROUGH FITNESS<br />
Exercise is the healthiest approach to fibromyalgia treatment. This<br />
non-aerobic program, taught by an instructor with fibromyalgia, is designed<br />
to prevent or counter the deconditioning that may result from<br />
exercise intolerance in individuals with fibromyalgia or chronic fatigue.<br />
Taught by Diane Gallagher, certified fitness instructor. Bring an exercise<br />
mat and light (1-5-lb) hand weights.<br />
$168 for a six-week session. Monday and Thursday, 3:00-4:00 pm<br />
Beginning May 14 or June 25.<br />
NEW! STRESS REDUCTION FOR FIBROMYALGIA AND<br />
CHRONIC FATIGUE<br />
Finding healthy ways to lower your stress can reduce symptoms,<br />
including pain and sleep problems. You will learn about habits that<br />
can interrupt circulation and produce pain and how to cultivate new<br />
ways to respond to life’s challenges. Presented by Patricia Howard,<br />
who has completed teacher training at the Center for Mindfulness at<br />
UMass.<br />
$90 Saturday, June 9, 10:00 am-4:00 pm<br />
NEW! A DAY OF MINDFULNESS FOR THE FAMILY<br />
In this workshop, we will take an open look at the<br />
interpersonal dynamics of the family, how to get<br />
along better and work through conflicts in positive<br />
ways. You will learn practices that allow you to be<br />
surrounded by intense emotions but not be affected<br />
negatively. Parents, young adults and teens are<br />
welcome.<br />
$90 Saturday, August 4, 10:00 am-4:00 pm ($45 for children 17 and<br />
younger)<br />
WOMEN’S SELF-DEFENSE SEMINAR for 8th grade and up<br />
This seminar will focus on hands-on self-defense techniques, strategies<br />
and tips for staying safe in common situations. The topics covered may<br />
be particularly beneficial to girls and women who are going through a<br />
transition at home, in school or at work, but are useful to all participants.<br />
Taught by Johanna Glazer and Len Glazer, internationally certified<br />
third-degree black belt instructors.<br />
$40 Wednesday, August 15, 7:30-9:30 pm<br />
Ongoing Sunday and Thursday evening weekly classes are also<br />
available; next session starts in September.<br />
Tender Beginnings:<br />
classes in preparation<br />
for childbirth and parenting<br />
<strong>Emerson</strong> <strong>Hospital</strong> offers tours, classes and support groups for those<br />
who are having a baby or are at home with a newborn. For dates of<br />
classes, to register or for other information, please call 978-287-3268.<br />
GROUP TOURS<br />
Free tours of the Birthing Center are given on a regular basis.<br />
Registration is required, so call the number above.<br />
CLASSES<br />
• Prenatal Childbirth<br />
Choose a five-week class, a oneday<br />
class or a refresher course,<br />
which covers vaginal and cesarean<br />
deliveries. For pregnant<br />
women and their partners.<br />
• Natural Childbirth<br />
Three-session course<br />
• Sibling Preparation<br />
For children between 2½ and 6<br />
• Bed Rest Loaner Kit<br />
Includes videos, books and a<br />
home visit<br />
• Infant Care<br />
Learn bathing, diapering<br />
and holding<br />
• Breastfeeding<br />
Covers the benefits and<br />
challenges of breastfeeding<br />
• Infant CPR Anytime Program<br />
One-hour introductory<br />
class and kit<br />
• Getting Ready for Multiples<br />
For parents expecting twins,<br />
triplets or more<br />
• The Happiest Baby on the<br />
Block<br />
Learn how to calm your baby<br />
• HypnoBirthing ®<br />
Supports a natural childbirth<br />
experience using hypnosis<br />
SUPPORT GROUPS<br />
• Lactation Consultation<br />
<strong>Emerson</strong> offers a certified lactation consultant who can help resolve<br />
difficulty with breastfeeding. Check with your health plan to determine<br />
coverage. For more information about <strong>Emerson</strong>’s lactation<br />
consultation, please call 978-287-3317.<br />
• Mothers Offering Mothers Support (MOMS)<br />
For new mothers who may feel overwhelmed and alone, <strong>Emerson</strong><br />
has experienced volunteer MOMS who are available to offer support.<br />
For more information, please call 978-287-3176.<br />
• New Mothers Group<br />
Bring your questions and concerns, or just come to meet and share<br />
experiences with other mothers. Join them and their babies to<br />
discuss the challenges of those early months. For more information,<br />
please call 978-287-3176.<br />
13
on call<br />
emerson hospital is pleased to<br />
introduce the following new physicians.<br />
<strong>Hospital</strong> Medicine – Adult and Pediatric<br />
Timothy W. Baba, MD, PhD<br />
<strong>Emerson</strong> <strong>Hospital</strong><br />
133 ORNAC, Concord<br />
978-369-1400<br />
Dr. Baba earned his graduate and medical degrees<br />
from The University of Texas, Southwestern Medical<br />
School at Dallas and completed an internship<br />
in pediatrics at Children’s <strong>Hospital</strong> Boston, where<br />
he also completed a residency in pediatrics and fellowship<br />
in neonatology. Dr. Baba is board-certified<br />
in pediatrics and neonatal/perinatal medicine. His<br />
clinical interests include asthma management, vaccine<br />
development and prevention of neonatal and<br />
pediatric infectious disease. He is a hospital-based<br />
physician who cares for pediatric inpatients, as well<br />
as newborns, in <strong>Emerson</strong>’s well-baby and special care<br />
nurseries. He does not have a private office practice.<br />
Shaolay X. Jiang, MD<br />
<strong>Emerson</strong> <strong>Hospital</strong><br />
133 ORNAC, Concord<br />
978-369-1400<br />
Dr. Jiang graduated from St. George’s University<br />
School of Medicine in Grenada. She completed her<br />
residency in internal medicine at New York University<br />
Downtown <strong>Hospital</strong>. Dr. Jiang is board-certified in<br />
internal medicine. She is a hospital-based internist<br />
who treats adult inpatients and does not have a<br />
private office practice.<br />
Emily Kung, MD<br />
<strong>Emerson</strong> <strong>Hospital</strong><br />
133 ORNAC, Concord<br />
978-369-1400<br />
Dr. Kung earned her medical degree from University<br />
of California, San Francisco School of Medicine. She<br />
completed a residency in pediatrics at MassGeneral<br />
<strong>Hospital</strong> for Children, where she served as chief resident.<br />
Dr. Kung is board-certified in pediatrics, and<br />
her clinical interests include health advocacy, obesity<br />
and the care of medically complex patients. She is a<br />
hospital-based physician who cares for pediatric inpatients<br />
and does not have a private office practice.<br />
Rositsa Petrova, MD<br />
<strong>Emerson</strong> <strong>Hospital</strong><br />
133 ORNAC, Concord<br />
978-369-1400<br />
Dr. Petrova graduated from the Medical University<br />
of Sofia in Bulgaria and completed her residency at<br />
Lincoln Medical and Mental Health Center in New<br />
York City. She is board-certified in internal medicine.<br />
Dr. Petrova is a hospital-based internist who treats<br />
adult inpatients and does not have a private office<br />
practice.<br />
Obstetrics and Gynecology<br />
Christina T. Thomas, MD<br />
Concord OB/GYN Associates<br />
59 ORNAC, Suite 1, Concord<br />
978-369-7627<br />
Dr. Thomas attended State University of New York<br />
at Buffalo School of Medicine and completed her<br />
residency at Tufts-New England Medical Center. She<br />
is board-certified in obstetrics and gynecology and<br />
recently was on staff at South Shore <strong>Hospital</strong> in Weymouth,<br />
Massachusetts. Her areas of special interest<br />
include minimally invasive surgery, colposcopy and<br />
obstetrics.<br />
Palliative Care<br />
Alyssa C. Luddy, MD<br />
Hospice of the North Shore & Greater Boston<br />
75 Sylvan Street, Suite B-102, Danvers<br />
978-774-7566<br />
Dr. Luddy graduated from New York Medical College<br />
and completed her residency at Beth Israel Medical<br />
Center in New York City and her fellowship in palliative<br />
care at Oregon Health and Sciences University<br />
in Portland. She is board-certified in family medicine<br />
and hospice and palliative medicine. Her clinical<br />
interests are pain management and ensuring quality<br />
end-of-life care.<br />
Pediatric Dentistry<br />
Evan M. Shaw, DMD<br />
Pediatric Dentistry, Inc.<br />
290 Baker Avenue Extension, Suite N228, Concord<br />
978-369-7771<br />
Dr. Shaw graduated from the University of Pennsylvania<br />
School of Dental Medicine in Philadelphia<br />
and completed his residency in pediatric dentistry at<br />
Children’s <strong>Hospital</strong> Boston. He is board-eligible in<br />
pediatric dentistry.<br />
14
Donating blood:<br />
Donating blood is a<br />
generous thing to do.<br />
It benefits patients<br />
who need blood, and<br />
it saves <strong>Emerson</strong> the<br />
expense of having<br />
to purchase blood.<br />
It also benefits the<br />
donors themselves,<br />
who often say they<br />
feel good – even<br />
elated – after giving<br />
blood.<br />
it’s generous, easy and feels good<br />
18-year-old says it is her way of volunteering<br />
Katie Moreau, an 18-year-old Chelmsford resident,<br />
says that’s how she feels after making a<br />
donation at <strong>Emerson</strong>’s Blood Donor Center.<br />
“The nurses always say to me ‘you’re so young.’<br />
But by donating locally, I’m helping someone in<br />
my community. It is my way of volunteering. I<br />
wish more young people gave blood because it<br />
lifts your spirits.”<br />
Katie stands out among blood donors, says<br />
Linda Dolan, blood donation recruiter. “I’d<br />
say the average age of those who donate is about 50,” says Ms. Dolan, who<br />
adds that, when it comes to blood donation, the hospital faces a challenge.<br />
“Only 60 percent of the population can give blood; health conditions or<br />
medications prevent many people from being eligible. Of that 60 percent,<br />
however, only 5 percent actually donate.”<br />
Each donation potentially benefits multiple patients. “At <strong>Emerson</strong>, one unit<br />
of whole blood collected can be used to provide red blood cells and plasma<br />
components, thus helping two patients,” says Ms. Dolan. “Blood donated<br />
at <strong>Emerson</strong> remains at <strong>Emerson</strong>.” Donating blood only takes about 30<br />
minutes. Once donors are screened for eligibility, the donation itself takes<br />
about ten minutes, after which they are served refreshments, including fluid<br />
to replace the donated blood. “We keep an eye on donors to make sure they<br />
feel okay before they leave.”<br />
Katie enjoys relaxing with juice and a snack after donating blood. “The<br />
nurses are so nice,” she says. “They take good care of me.” Parking is free<br />
Katie Moreau relaxes while Rosemary Woitowicz, RN, draws blood.<br />
for those who donate blood, and the staff offers a number of incentives,<br />
from T-shirts to gift cards for coffee, ice cream and a car wash. Each month,<br />
all donors are entered into a raffle.<br />
Donate blood. Save a life.<br />
The <strong>Emerson</strong> Blood Donor Center is located on the first floor of the<br />
hospital’s John Cuming Building in Concord. Please call 978-287-3390<br />
to schedule an appointment or to verify hours. Walk-ins are welcome.<br />
Regular hours are:<br />
Monday 8:00 am - 3:00 pm Wednesday 9:00 am - 2:30 pm<br />
Tuesday 9:00 am - 5:00 pm Thursday 9:00 am - 7:30 pm<br />
Note the blood donor center closes for lunch: 1:00-1:30 pm on Monday,<br />
Tuesday and Thursday; and 12:00-12:30 pm on Wednesday.<br />
New palliative care program is established<br />
emerson is working with hospice of the north shore & greater boston<br />
<strong>Emerson</strong> <strong>Hospital</strong> recently expanded its successful relationship with<br />
Hospice of the North Shore & Greater Boston (HNSGB) to provide<br />
patients with a comprehensive approach to palliative care. Palliative care<br />
addresses the symptoms and stresses of serious illness.<br />
“Palliative care often is referred to as ‘pain and comfort care,’” explains<br />
Joyce Welsh, vice president and chief nursing officer at <strong>Emerson</strong>. Ms.<br />
Welsh is on the committee that integrated a new program of palliative<br />
care with the existing hospice care program, which HNSGB already provides.<br />
“We have been working with them on hospice care for two years,<br />
and it is a positive, wonderful relationship.” Hospice of the North Shore<br />
& Greater Boston is the largest and most comprehensive hospice provider<br />
in Massachusetts.<br />
Unlike hospice care, which typically is provided for six months or less, palliative<br />
care is a consultative service with no general time limit. “Patients<br />
may continue to receive treatment and will benefit from palliative care because<br />
of ongoing symptoms,” says Ms. Welsh. Common illnesses requiring<br />
palliative care include heart failure, chronic obstructive pulmonary<br />
disease (COPD), cancer and Alzheimer’s disease. For example, COPD<br />
patients who are having difficulty breathing often benefit from having a<br />
consultation with the Hospice of the North Shore & Greater Boston team.<br />
“There are several situations that merit a palliative care consultation tied<br />
to the goals of care,” says Stephanie Patel, MD, the organization’s vicepresident<br />
and chief medical officer, who is on staff at <strong>Emerson</strong>. “They include<br />
when patients present complex pain and symptom management<br />
needs, are struggling with difficult decisions about care, have a chronic,<br />
progressive illness and unclear life expectancy or are newly diagnosed with<br />
a life-limiting illness.” Dr Patel is one of HNSGB’s five palliative care physicians;<br />
there are also five nurse practitioners on the staff. The palliative<br />
care team works closely with the patient’s own physician.<br />
“Patients are benefiting from our new palliative care program,” says Ms.<br />
Welsh. “Working with our Hospice of the North Shore & Greater Boston<br />
colleagues, we are committed to providing our patients with the highest<br />
quality palliative and end-of-life-care.”<br />
15
emerson<br />
ADVISOR<br />
For more information on care at <strong>Emerson</strong><br />
<strong>Hospital</strong>, call the toll-free Physician Referral Line:<br />
1-877-9-EMERSON (1-877-936-3776) or visit the<br />
hospital’s web site at www.emersonhospital.org.<br />
Haran Ramachandran, MD<br />
Neurosurgery<br />
Lahey Spine Program at <strong>Emerson</strong><br />
Ana L. Jacobellis, DO<br />
Internal Medicine<br />
Westford Internal Medicine<br />
Tania Bandak, MD, MPH<br />
Internal Medicine<br />
Concord Hillside Medical Associates<br />
When should I consider seeking surgery<br />
for my back pain?<br />
Back pain can be due to many causes, including<br />
muscular strain, herniated discs, bony fractures<br />
and traumatic injury. Treatment options<br />
include anti-inflammatory medications, a short<br />
course of oral steroids, local injections and<br />
physical therapy. Surgery is considered if medical<br />
treatment fails or progressive nerve damage<br />
is suspected.<br />
You should almost always seek medical care<br />
within a day or two of the onset of severe back<br />
pain. Pain shooting down the leg is usually due<br />
to a herniated disc pressing on a nerve; consultation<br />
with your primary care physician may be<br />
appropriate. However, weakness in the foot,<br />
numbness in the toes or urinary incontinence<br />
may indicate nerve damage and warrant a visit<br />
to the Emergency Department.<br />
Back pain due to muscular causes or a herniated<br />
disc usually resolves with medications and physical<br />
therapy. Further investigations like an MRI<br />
scan of the back is necessary if nerve damage is<br />
suspected or if symptoms do not resolve within<br />
six weeks. If the symptoms are severe, you<br />
may be referred to a back specialist. Surgery is<br />
appropriate if the MRI scan definitively shows<br />
the causative factor.<br />
How can I protect myself from Lyme<br />
disease this summer?<br />
Wearing long sleeves, keeping your pant legs<br />
tucked into your boots and using insect repellent<br />
are all useful in the outdoors. However,<br />
the most important thing is to be diligent about<br />
checking yourself for deer ticks after you have<br />
spent time in tick-infested areas such as woods<br />
or fields. Ticks hide in grassy areas and on<br />
leaves, waiting for a chance to attach themselves<br />
to potential meal tickets in the form of passing<br />
animals – and people.<br />
Once a tick infected with the Lyme disease<br />
bacteria attaches itself to your skin, it aims to<br />
feed on your blood. The danger occurs during<br />
the tick’s larval stage, when it is the size of a<br />
poppy seed. As it feeds, its body swells. After<br />
a full feeding, which takes 36 to 72 hours, it<br />
can deposit the bacteria into your bloodstream,<br />
causing Lyme disease.<br />
If you find a tick that has only recently become<br />
attached to your body, you can most likely<br />
remove it safely. If it has been there for at least<br />
36 hours, it may be prudent to see your physician<br />
for a preventive dose of antibiotics.<br />
I don’t have any diagnosed medical<br />
problems. Why should I see my<br />
physician yearly?<br />
Our society has traditionally defined health as<br />
the absence of disease. However, it is possible<br />
to be healthy from a strict medical perspective<br />
but to not feel healthy. Many people do<br />
not have any disease, yet they do not feel well.<br />
Other individuals may feel fine but are silently<br />
developing the foundations for certain diseases<br />
to take root.<br />
This could be due to poor lifestyle habits, such<br />
as an unhealthy diet, not exercising or sleeping<br />
regularly or from stress at home or at work.<br />
It may take years – even decades – of living<br />
“unwell” for someone to develop medical<br />
problems like obesity, heart disease or diabetes.<br />
Why wait until disease develops, when treatment<br />
can be cumbersome and intrusive, to seek<br />
medical attention? I believe that through a<br />
strong, trusting relationship with one’s primary<br />
care provider, individuals can discover paths<br />
to living and feeling well in all aspects of their<br />
lives. This is the most powerful “prescription”<br />
for living a full and meaningful life, and it<br />
begins with an annual appointment.<br />
16
‘‘<br />
karen hamlin<br />
IN MY<br />
OWN<br />
VOICE<br />
Plenty of people live with obstructive sleep apnea (OSA), which<br />
leaves them gasping for breath, waking throughout the night and<br />
tired the next day. Fortunately, the establishment of sleep labs like<br />
the one at <strong>Emerson</strong>’s Sleep Disorders Center has helped reveal an<br />
epidemic of OSA, which is estimated to affect approximately 18 million<br />
Americans. Among those who come for overnight sleep testing,<br />
84 percent are found to have the disorder, approximately 35 percent<br />
with severe cases. That was true of Karen Hamlin of Boxborough,<br />
52, who credits Dan Tilles, MD, her primary care physician, with<br />
encouraging her to get a diagnosis, which led to successful treatment:<br />
regular use of a continuous positive airway pressure (CPAP)<br />
machine when she sleeps.<br />
Karen Hamlin is sleeping well these days, thanks to being diagnosed and treated<br />
for longstanding sleep apnea.<br />
“I knew I had sleeping issues for a couple of years. My husband regularly<br />
told me that I wasn’t breathing – sometimes for as long as 30 seconds –<br />
during the middle of the night. Then I’d gasp for air.<br />
“For many years, I always felt tired during the day, never felt rested upon<br />
waking and wanted to take naps. I often was afraid I would fall asleep while<br />
I was driving; there were times when I worried about making it home safely.<br />
I chalked it up to having a stressful lifestyle – working full-time, being a<br />
mom, staying up too late. I also blamed much of my sleep problem on my<br />
husband’s snoring. I lived with it.<br />
“Last October, I went for my annual physical, and Dr. Tilles asked me ‘how<br />
are you sleeping?’ I told him my sleep was horrible; I didn’t have trouble<br />
falling asleep, but I woke up throughout the night. He told me it sounded<br />
like a classic case of sleep apnea and that I should be evaluated at <strong>Emerson</strong>’s<br />
sleep lab. He told me that treatment could really change my life.<br />
“I knew the treatment for sleep apnea was to wear a mask that was attached<br />
to a machine, and I was sure I would never do that. On the other hand, I<br />
didn’t feel good.<br />
“In November, I spent a night in the sleep lab. The technician was helpful<br />
and knowledgeable. She told me that if I stopped breathing a certain<br />
number of times per hour, she would wake me up so that I could try the<br />
machine. After being hooked up for the sleep test, I fell asleep without<br />
a problem.<br />
‘‘<br />
“Late that night, the technician woke me up and told me that I had stopped<br />
breathing more than 20 times every hour. I was shocked to hear that. She<br />
fitted me with a CPAP mask, and I went back to sleep. I slept for three and a<br />
half hours without interruption; when I woke up, I could tell that I had slept<br />
soundly.<br />
“I wanted to talk with Dr. Tilles about the test and what to do. At the appointment,<br />
he told me that I have severe sleep apnea. He said there was<br />
no question about it; I should be treated. I realized it was time to face the<br />
problem, so Dr. Tilles wrote the prescription, and a representative from the<br />
CPAP company came to the house to explain all the details. He also fitted<br />
me with the right kind of mask.<br />
“At first, it’s a real adjustment to sleeping with the mask and the CPAP<br />
machine, but I decided to stick with it. By the fourth week, I was sleeping<br />
better. The machine is whisper-quiet, and the air is humidified, which is<br />
very helpful.<br />
“The good news is that my sleep is so sound now. I’m not tired in the<br />
afternoon, and I have more energy, so I’ve started a more strenuous exercise<br />
program. I can handle it.<br />
“I’ve been using the CPAP for three months now. After thinking that I<br />
would never use the CPAP machine, now I almost look forward to putting it<br />
on at night. As I tell my husband, I sleep so soundly that I don’t even hear<br />
him snoring anymore.”<br />
<strong>Emerson</strong> <strong>Hospital</strong> has several sleep specialists on the medical staff. Contact the Sleep Disorders Center at 1-800-432-8808 for more information.<br />
17
Couple faces esophageal cancer<br />
> Continued from page 5<br />
By the fall, his energy was depleted. “I really hit bottom,” he says.<br />
“The recliner and I became good friends. But I knew my team at<br />
<strong>Emerson</strong> was behind me and wouldn’t let me down.” Just as he<br />
was beginning to regain his strength, it was time to make a decision<br />
about surgery.<br />
In counseling Mr. Beardsley, Dr. Sajer considered the side effects he<br />
experienced during his combination therapy, as well as his entire<br />
health history, which includes having a quadruple coronary bypass,<br />
cardiac ablation, insertion of a pacemaker and suffering a serious fall<br />
from a ladder the previous year where he suffered major blood loss,<br />
broken ribs and a broken wrist and required facial reconstruction.<br />
“The surgery requires incisions in both the chest and the abdomen,”<br />
explains Dr. Sajer, “and the associated risks are not insignificant.”<br />
“It would involve removing all the cancer and pulling the stomach<br />
up to create a new esophagus,” says Mr. Beardsley, now 75. “I<br />
would then be on a very limited diet. At my age, I didn’t feel that I<br />
would come through the surgery and still be the same person afterward.”<br />
After hearing the pros and cons of having difficult surgery<br />
followed by a three- to six-month recovery, he decided against it.<br />
In November, Dr. Sajer told Mr. Beardsley that the treatment had<br />
been successful in controlling his cancer. However, it could recur,<br />
and she urged him to use his time wisely. When Dr. Sajer offered<br />
additional treatment, Mr. Beardsley declined.<br />
The couple grew close to the staff at <strong>Emerson</strong>. “Everybody there,<br />
without exception, was positive, uplifting and made it a good experience,”<br />
says Mr. Beardsley. “The people were tremendous, and it<br />
really helped.”<br />
At one point, Ann Snow, RN, nurse manager in radiation oncology,<br />
thought the Beardsleys might each benefit from massage therapy<br />
and arranged appointments for them, which was funded by the<br />
<strong>Emerson</strong> <strong>Hospital</strong> Auxiliary. “That was a great thing for both of<br />
us,” says Mr. Beardsley.<br />
As winter approached, the couple made plans to take a cruise in the<br />
Caribbean, where the sun and relaxation benefited Mr. Beardsley. “I<br />
brought a new man back from that trip,” his wife says with a smile.<br />
Once they were home again, one of Mr. Beardsley’s sons called to<br />
announce that he had Super Bowl tickets for them. “It was Paula’s<br />
reward for taking such good care of me,” says Mr. Beardsley. “It was<br />
a once-in-a-lifetime opportunity, and something we’ll never forget.”<br />
Next, Mr. Beardsley, a manufacturing engineer, was contacted<br />
about returning to work after having been laid off from his job last<br />
May, prior to his diagnosis. “That felt great,” he says. “I may be<br />
75 years old, but I enjoy what I do.”<br />
Looking back, the Beardsleys are grateful for the treatment, the care<br />
and the support they found at <strong>Emerson</strong>. “We never questioned<br />
whether we should go anywhere else,” says Mrs. Beardsley. “From<br />
the start, we had a real comfort level with Dr. Sajer, who is clearly<br />
very knowledgeable. She and her staff, Dr. McGrath and his team –<br />
everyone at <strong>Emerson</strong> – wrapped us in comfort and total care.”<br />
Mr. Beardsley agrees. “Everything that we needed was at<br />
<strong>Emerson</strong>,” he says, “and Paula was always by my side. I’m feeling<br />
fine, and we’re enjoying every day.”<br />
New procedure opens up the sinuses<br />
> Continued from page 8<br />
that breathing out of one nostril had been a problem. Having the procedure<br />
was one of the best decisions of my life.”<br />
In Pailin, Cambodia, her days were filled with teaching English, playing sports<br />
with local children, working in the library and helping at a feeding program. “I<br />
know I helped make a difference in the lives of the kids and families there,”<br />
she says.<br />
Balloon catheter dilation is proving to be an effective treatment for individuals<br />
with chronic sinus infections. “It is a particularly safe procedure and not associated<br />
with any complications,” says Dr. Khalid. “I encourage patients to use<br />
a salt water rinse after the surgery as a preventive measure to keep things<br />
moving in the sinuses.”<br />
In some patients, the improvement is dramatic. “Hillary’s mother told me<br />
she hadn’t been herself for a long time,” Dr. Khalid recalls. “When I saw<br />
Hillary after she had the procedure, I understood what her mother meant,<br />
because I met the healthy Hillary, who was smiling.”<br />
Balloon catheter dilation requires no hospital stay; results can be dramatic.<br />
For more information, Dr. Khalid may be reached at 978-287-7499.<br />
18
emerson hospital<br />
Support Groups<br />
& Special Services NEWS<br />
f r o m emerson<br />
Support Groups<br />
Alcohol and Substance Abuse Support 978-287-3520<br />
Breast Cancer Support Group-Virginia Thurston<br />
Healing Garden 978-456-3532<br />
Diabetes Support 978-287-3054<br />
Melanoma Support 1-800-557-6352<br />
M.O.M.S (Mothers Offering Mothers Support) 978-287-3176<br />
New Mothers Group 978-287-3176<br />
Oral, Head and Neck Cancer Support 978-287-3189<br />
Parkinson’s Support 978-443-5742<br />
Sleep Disorders Support 978-287-3735<br />
Surgical Weight Loss Support 978-287-3532<br />
Widowed Outreach Support 1-800-696-6424<br />
Special Services<br />
Alzheimer’s Information 978-287-3170<br />
Body Composition Analysis 978-287-3782<br />
CPR 978-287-3050<br />
Cardiac Rehabilitation 978-287-3732<br />
Chronic Lung Disease Program 978-287-8300<br />
Gambling Problems 978-287-3520<br />
Heart Failure Program 978-287-8300<br />
Home Health Service 978-287-8300<br />
Hospice & Palliative Care Federation of Mass. 1-800-962-2973<br />
Lifeline 1-800-543-3546<br />
Look Good…Feel Better 978-287-3788<br />
Nutritional Counseling 978-287-3782<br />
Pastoral Care 978-287-3015<br />
Pediatric Bereavement Workshop 978-287-3422<br />
Pediatric Pre-Admission Program 978-287-3420<br />
Pelvic Health/Bladder Control 978-287-8200<br />
Physician Referral 1-877-9-EMERSON or 1-877-936-3776<br />
Pulmonary — Better Breathers Club 978-287-3715<br />
REACH (hotline for domestic violence) 1-800-899-4000<br />
SHINE Program 781-272-7177<br />
Speech and Language Screening for Preschoolers 978-287-8200<br />
Sports Rehabilitation 978-287-8200<br />
Volunteer Program 978-287-3200<br />
Wound Care Center 978-287-8550<br />
<strong>Emerson</strong>’s main entrance is named for Teresa E. DiGiovanni<br />
The hospital’s main entrance is being renovated<br />
to modernize the area and provide a more welcoming<br />
feel, thanks to a significant donation<br />
from the DiGiovanni family of Concord. The<br />
main entrance will be named for Teresa E.<br />
DiGiovanni (shown at left with her husband,<br />
Guy), who passed away in November 2011. The donation was made in gratitude<br />
for the care that Mrs. DiGiovanni and other family members have received<br />
at <strong>Emerson</strong>, as well as to honor the leadership of Christine Schuster,<br />
president and CEO. Mrs. DiGiovanni’s son, James DiGiovanni, is a member<br />
of the hospital’s Board of Directors.<br />
Centennial wall display recently unveiled<br />
In May, a permanent wall display about<br />
<strong>Emerson</strong>’s history was installed in the<br />
third-floor corridor of the John Cuming<br />
Building. The display, which features<br />
several vintage photographs, marks the hospital’s centennial and includes a<br />
timeline of historical milestones, including clinical programs and progress<br />
on the hospital campus. It also reflects the enduring bond between <strong>Emerson</strong><br />
and the community, seen through its volunteers, the <strong>Emerson</strong> <strong>Hospital</strong><br />
Auxiliary and the tradition of philanthropy. The hospital’s growing presence<br />
throughout the service area is featured through the establishment of hospital-affiliated<br />
satellites. Stop by to see the display!<br />
New art exhibition opens at <strong>Emerson</strong> Medical at Sudbury<br />
<strong>Emerson</strong>’s ongoing commitment to displaying<br />
the work of talented local artists continues this<br />
spring with an exhibition of new work by Liza<br />
Carter at <strong>Emerson</strong> Medical at Sudbury, located<br />
at 490 Boston Post Road (Route 20 in Chiswick<br />
Park). Ms. Carter, a Concord resident, is showing<br />
watercolors and nature photography. She has exhibited throughout the<br />
region, including at <strong>Emerson</strong> Umbrella Center for the Arts in Concord. The<br />
exhibition runs from May through October.<br />
Safe driving assessment is available<br />
Adults who have undergone a change in health<br />
status may need to be evaluated before driving<br />
again. The clinical driver assessment program<br />
includes an evaluation by a certified occupational<br />
therapist (fee is $300) and, for those who<br />
pass the evaluation, an on-road test conducted by a professional driving instructor<br />
or certified driver rehabilitation specialist (fee is $200). A physician<br />
referral is required. Please call 978-287-8200 for more information.<br />
19
133 ORNAC, Concord, MA 01742<br />
978-369-1400<br />
www.emersonhospital.org<br />
<strong>Emerson</strong> <strong>Hospital</strong> is is an acute care medical center<br />
located in Concord with health centers in in Bedford,<br />
Groton, Sudbury and Westford. It It is is well well known for for<br />
its medical and surgical specialists, outstanding<br />
nursing care and patient-centered services, including<br />
the Clough Birthing Center, the Bethke Mass General Cancer<br />
Cancer Center, Center the Polo at <strong>Emerson</strong> Emergency <strong>Hospital</strong>-Bethke, Center, the Clough the Polo<br />
Surgical Emergency Center Center and and the the Center Clough for Specialty Surgical Care. Center.<br />
www.emersonhospital.org<br />
HealthWorks, published by <strong>Emerson</strong> <strong>Hospital</strong>, is<br />
mailed to residents in the hospital’s service area<br />
and is distributed to the employees and physicians’<br />
offices affiliated with <strong>Emerson</strong> <strong>Hospital</strong>.<br />
If you would prefer not to receive such mailings in<br />
the future, please let us know by calling 978-287-<br />
3458 or send an email to pr@emersonhosp.org.<br />
<strong>Emerson</strong> <strong>Hospital</strong> President and CEO<br />
Christine C. Schuster<br />
HealthWorks Magazine editorial staff<br />
Christine Gallery, Bonnie Goldsmith<br />
Writers<br />
Laura Duffy, Ralph Fuller<br />
Photography<br />
Tony Rinaldo<br />
Design and Printing<br />
Fassino/Design and Signature Printing & Consulting<br />
The information included here is intended to educate<br />
readers about health issues, but it is not a substitute<br />
for consultation with a personal physician.<br />
The mission of <strong>Emerson</strong> <strong>Hospital</strong> is to deliver<br />
high-quality care to our community that is safe,<br />
compassionate, accessible, appropriate, efficient<br />
and coordinated.<br />
<strong>Emerson</strong> <strong>Hospital</strong> Auxiliary Hosts 12th Annual<br />
5K Run ~Walk & Family Funday for Cancer on June 2<br />
The <strong>Emerson</strong> <strong>Hospital</strong> Auxiliary will hold its 12th annual 5K Run~Walk & Family Funday for Cancer on<br />
Saturday, June 2, at the Thoreau Club, 275 Forest Ridge Road in Concord.<br />
The event is sponsored by Concord Mews, Thoreau Club and Marx Running & Fitness Center. Activities<br />
will include a barbeque, tot trot for ages 5 and under, tie-dye T-shirt-making, inflatable obstacle<br />
course, volleyball, badminton and recreational swimming. Registration begins at 8:30 am. The onemile<br />
kids’ fun run (for ages 5-12) leaves at 9:15 am, and the 5K begins at 10:00 am.<br />
“This is a fun-filled, multi-generational event that keeps growing in participation, business partnerships<br />
and donations from the community,” said Karen Maines, president of the <strong>Emerson</strong> <strong>Hospital</strong><br />
Auxiliary. Last year’s event attracted nearly 450 participants and raised a record $42,000.<br />
Funds raised from the 5K Run~Walk and Family Funday for Cancer will support cancer services at<br />
<strong>Emerson</strong> <strong>Hospital</strong>. Earlier this year, the longstanding relationship in cancer care between <strong>Emerson</strong><br />
and Massachusetts General <strong>Hospital</strong> expanded to include a collaboration with medical oncology<br />
(see story on page 4).<br />
To register for the 5K Run~Walk & Family Funday for Cancer, visit www.firstgiving.com/<strong>Emerson</strong><br />
<strong>Hospital</strong>Auxiliary/5krunwalk. Entry fees, which include the post-race barbecue, are $25 for adults<br />
until May 30 and $30 until the day of the event, and $12 for the kids’ fun run. To volunteer at the<br />
event, contact Barbara Boardman at 978-371-1158 or bsboard@comcast.net.<br />
The <strong>Emerson</strong> <strong>Hospital</strong> Auxiliary supports the hospital with community awareness, patient support<br />
and fundraising. For more information on the auxiliary, visit www.emersonhospital.org/support.<br />
FPO<br />
Front cover: Donald Beardsley of Billerica, shown with his wife, Paula, found everything he needed<br />
at <strong>Emerson</strong>.