Doctors' Newsletter - Autumn 2008 - Douglass Hanly Moir Pathology
Doctors' Newsletter - Autumn 2008 - Douglass Hanly Moir Pathology
Doctors' Newsletter - Autumn 2008 - Douglass Hanly Moir Pathology
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
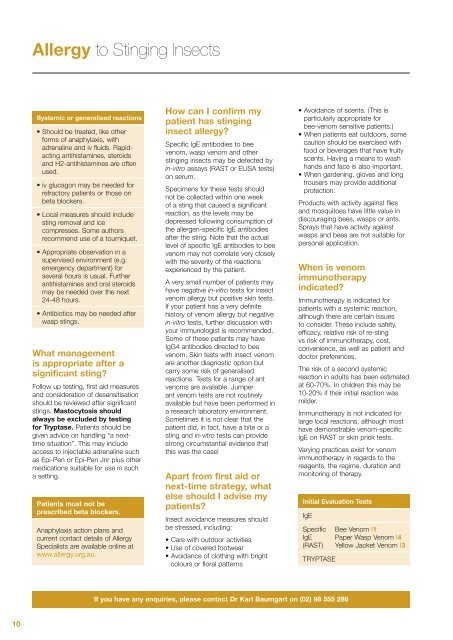
Allergy to Stinging Insects<br />
Systemic or generalised reactions<br />
• Should be treated, like other<br />
forms of anaphylaxis, with<br />
adrenaline and iv fluids. Rapidacting<br />
antihistamines, steroids<br />
and H2-antihistamines are often<br />
used.<br />
• iv glucagon may be needed for<br />
refractory patients or those on<br />
beta blockers.<br />
• Local measures should include<br />
sting removal and ice<br />
compresses. Some authors<br />
recommend use of a tourniquet.<br />
• Appropriate observation in a<br />
supervised environment (e.g.<br />
emergency department) for<br />
several hours is usual. Further<br />
antihistamines and oral steroids<br />
may be needed over the next<br />
24-48 hours.<br />
• Antibiotics may be needed after<br />
wasp stings.<br />
What management<br />
is appropriate after a<br />
significant sting<br />
Follow up testing, first aid measures<br />
and consideration of desensitisation<br />
should be reviewed after significant<br />
stings. Mastocytosis should<br />
always be excluded by testing<br />
for Tryptase. Patients should be<br />
given advice on handling “a nexttime<br />
situation”. This may include<br />
access to injectable adrenaline such<br />
as Epi-Pen or Epi-Pen Jnr plus other<br />
medications suitable for use in such<br />
a setting.<br />
Patients must not be<br />
prescribed beta blockers.<br />
Anaphylaxis action plans and<br />
current contact details of Allergy<br />
Specialists are available online at<br />
www.allergy.org.au.<br />
How can I confirm my<br />
patient has stinging<br />
insect allergy<br />
Specific IgE antibodies to bee<br />
venom, wasp venom and other<br />
stinging insects may be detected by<br />
in-vitro assays (RAST or ELISA tests)<br />
on serum.<br />
Specimens for these tests should<br />
not be collected within one week<br />
of a sting that caused a significant<br />
reaction, as the levels may be<br />
depressed following consumption of<br />
the allergen-specific IgE antibodies<br />
after the sting. Note that the actual<br />
level of specific IgE antibodies to bee<br />
venom may not correlate very closely<br />
with the severity of the reactions<br />
experienced by the patient.<br />
A very small number of patients may<br />
have negative in-vitro tests for insect<br />
venom allergy but positive skin tests.<br />
If your patient has a very definite<br />
history of venom allergy but negative<br />
in-vitro tests, further discussion with<br />
your immunologist is recommended.<br />
Some of these patients may have<br />
IgG4 antibodies directed to bee<br />
venom. Skin tests with insect venom<br />
are another diagnostic option but<br />
carry some risk of generalised<br />
reactions. Tests for a range of ant<br />
venoms are available. Jumper<br />
ant venom tests are not routinely<br />
available but have been performed in<br />
a research laboratory environment.<br />
Sometimes it is not clear that the<br />
patient did, in fact, have a bite or a<br />
sting and in-vitro tests can provide<br />
strong circumstantial evidence that<br />
this was the case!<br />
Apart from first aid or<br />
next-time strategy, what<br />
else should I advise my<br />
patients<br />
Insect avoidance measures should<br />
be stressed, including:<br />
• Care with outdoor activities<br />
• Use of covered footwear<br />
• Avoidance of clothing with bright<br />
colours or floral patterns<br />
• Avoidance of scents. (This is<br />
particularly appropriate for<br />
bee-venom sensitive patients.)<br />
• When patients eat outdoors, some<br />
caution should be exercised with<br />
food or beverages that have fruity<br />
scents. Having a means to wash<br />
hands and face is also important.<br />
• When gardening, gloves and long<br />
trousers may provide additional<br />
protection.<br />
Products with activity against flies<br />
and mosquitoes have little value in<br />
discouraging bees, wasps or ants.<br />
Sprays that have activity against<br />
wasps and bees are not suitable for<br />
personal application.<br />
When is venom<br />
immunotherapy<br />
indicated<br />
Immunotherapy is indicated for<br />
patients with a systemic reaction,<br />
although there are certain issues<br />
to consider. These include safety,<br />
efficacy, relative risk of re-sting<br />
vs risk of immunotherapy, cost,<br />
convenience, as well as patient and<br />
doctor preferences.<br />
The risk of a second systemic<br />
reaction in adults has been estimated<br />
at 60-70%. In children this may be<br />
10-20% if their initial reaction was<br />
milder.<br />
Immunotherapy is not indicated for<br />
large local reactions, although most<br />
have demonstrable venom-specific<br />
IgE on RAST or skin prick tests.<br />
Varying practices exist for venom<br />
immunotherapy in regards to the<br />
reagents, the regime, duration and<br />
monitoring of therapy.<br />
Initial Evaluation Tests<br />
IgE<br />
Specific<br />
IgE<br />
(RAST)<br />
TRYPTASE<br />
Bee Venom I1<br />
Paper Wasp Venom I4<br />
Yellow Jacket Venom I3<br />
If you have any enquiries, please contact Dr Karl Baumgart on (02) 98 555 286<br />
10