SKILLED CARE DURING CHILDBIRTH - Family Care International
SKILLED CARE DURING CHILDBIRTH - Family Care International
SKILLED CARE DURING CHILDBIRTH - Family Care International
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
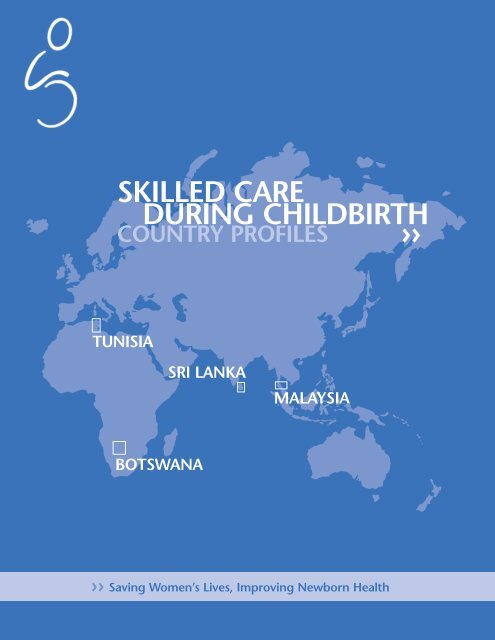
<strong>SKILLED</strong> <strong>CARE</strong><br />
<strong>DURING</strong> <strong>CHILDBIRTH</strong><br />
COUNTRY PROFILES >><br />
TUNISIA<br />
SRI LANKA<br />
MALAYSIA<br />
BOTSWANA<br />
>> Saving Women’s Lives, Improving Newborn Health
Skilled <strong>Care</strong> During Childbirth: Country Profiles<br />
Table of Contents<br />
1 Introduction<br />
22 Tunisia<br />
16 Sri Lanka<br />
10 Malaysia<br />
4 Botswana<br />
Prepared by Rahna Rizzuto and Shafia Rashid<br />
Design by Doris Halle Design, NYC<br />
© <strong>Family</strong> <strong>Care</strong> <strong>International</strong>, Inc. 2002<br />
Not-for-profit organisations may reproduce the contents of this publication freely,<br />
as long as it is not used for commercial purposes. FCI would appreciate acknowledgements<br />
and copies of any reproductions.
Skilled <strong>Care</strong> During Childbirth: Country Profiles Introduction<br />
The Scope of the Problem<br />
Globally, over half a million women die from the complications of pregnancy and childbirth each<br />
year—with nearly all of these deaths (99 percent) occurring in the developing world. For every woman<br />
who dies, 30 to 50 women suffer injury, infection, and/or disease.<br />
More than a decade of research has shown that most maternal deaths and disabilities can be prevented<br />
if women have access to good quality health services during pregnancy and childbirth. However, many<br />
women do not receive such care: just half of all deliveries in developing countries take place with a<br />
skilled attendant, with rates in some countries as low as 8%. In addition to the lack of good quality,<br />
accessible, safe motherhood services, a range of social, economic, and cultural factors contribute to<br />
women’s poor maternal health—these include women’s disproportionate poverty, unequal access to<br />
education, low social status, and lack of income and employment opportunities.<br />
While there has been limited progress at the global level in reducing maternal mortality and morbidity,<br />
a number of low- and middle-income countries have achieved measurable success in reducing maternal<br />
deaths. The four countries profiled in this report (Botswana, Malaysia, Sri Lanka, and Tunisia)<br />
demonstrate that maternal mortality can be reduced if political will and resources are mobilised<br />
around women’s health and empowerment.<br />
Ensuring Skilled <strong>Care</strong> During Childbirth<br />
In 1987, when the global Safe Motherhood Initiative was launched, representatives from a range of<br />
international agencies and governments committed themselves to the goal of reducing maternal<br />
deaths. Since then, much has been learned about which interventions are most effective, and the focus<br />
has shifted from predicting obstetric complications to managing them appropriately. Experts agree that<br />
one of the most essential interventions is to ensure that all women are cared for by a professional<br />
health worker (midwife, nurse, or doctor) with midwifery skills during the most dangerous period—during<br />
and immediately after childbirth. Skilled attendants, when supported by a functioning referral system,<br />
can fulfill the following critical functions:<br />
• Ensure that all deliveries are conducted hygienically and according to accepted medical practices,<br />
thereby preventing complications that are caused or exacerbated by poor care;<br />
• Identify complications promptly and manage them appropriately—either by treating or referring<br />
women to a higher level of care;<br />
• Provide high-quality, culturally-appropriate, and considerate care, ensuring necessary follow-up and<br />
linkages with other services, including antenatal and postpartum care, as well as family planning,<br />
postabortion care, and treatment of sexually transmitted infections.<br />
In October 1999, the Safe Motherhood Inter-Agency Group (IAG) launched a multi-step strategy to<br />
assess the importance and potential impact of skilled care during childbirth as a means of reducing<br />
maternal mortality. Key components of this strategy included:<br />
• The preparation of a comprehensive paper reviewing the evidence on skilled care during childbirth;<br />
• A Technical Consultation, held in April 2000 at World Health Organization (WHO) Headquarters in<br />
Geneva, which gathered leading experts in the field of safe motherhood to assess the evidence on<br />
skilled care during childbirth, and to develop key strategies for implementing the intervention in a<br />
range of developing country settings;<br />
• A set of informational materials relating to the critical components of skilled care during childbirth.<br />
These materials include: a policy brief, an information booklet, and country profiles on skilled care<br />
during childbirth (see country profiles in this document);<br />
1
Skilled <strong>Care</strong> During Childbirth: Country Profiles Introduction<br />
• An international conference “Saving Lives: Skilled Attendance at Childbirth” held in November,<br />
2000 in Tunisia. The aim of the conference was to facilitate the development of national-level action<br />
plans on skilled care during childbirth in selected countries in sub-Saharan Africa and South Asia.<br />
In addition, four developing countries (Botswana, Malaysia, Sri Lanka, and Tunisia) shared strategies<br />
and lessons learned in decreasing maternal mortality and increasing the coverage of skilled attendants.<br />
In preparation for the Tunisia conference, the four “low maternal mortality” countries developed<br />
case studies on their country’s experiences in implementing skilled care during childbirth as a key<br />
intervention in reducing maternal mortality. Following the conference, the profiles were expanded to<br />
serve as illustrative examples of the national-level programmatic strategies that led to high coverage<br />
of skilled care during childbirth (see country profiles highlighted in this document).<br />
Ingredients of Success<br />
Botswana, Malaysia, Sri Lanka, and Tunisia have all achieved measurable success in improving skilled<br />
care and reducing maternal mortality. In these four countries, coverage of skilled care increased<br />
significantly—with rates currently exceeding 90%. In the countries where data is available, maternal<br />
mortality ratios dramatically declined from several thousand maternal deaths per 100,000 live births<br />
to 20–60 over a span of 30–50 years.<br />
These experiences illustrate that middle- and low-income settings can achieve near-universal coverage<br />
of skilled care during childbirth if political will and resources are mobilised to improve women’s<br />
status and their access to basic health services.<br />
Employing a multi-faceted approach, these countries implemented a range of complementary,<br />
mutually-reinforcing strategies, with the goal of improving maternal health and saving women’s lives:<br />
• Mobilising political commitment at the highest level: In Botswana, a series of conferences and<br />
meetings during the 1990s galvanised political commitment to safe motherhood among high-level<br />
government officials, including the President, Members of Parliament, and the House of Chiefs.<br />
Subsequently, a national safe motherhood programme, with reduction of maternal mortality as a key<br />
goal, was established.<br />
• Investing in social and economic development—such as female literacy and education, poverty<br />
reduction, and basic human rights—with particular emphasis on the poor and vulnerable: Sri Lanka<br />
has demonstrated consistent, long-term support to ensuring the social welfare of its citizens. Since<br />
1945, free education from primary- to university-level has been made available on an equal basis<br />
for both men and women—resulting in a population with an overall literacy rate of 91%. Health care<br />
is also provided free of charge in an effort to ensure access for poor and underserved groups. All<br />
citizens enjoy basic human rights and political freedoms, which have been enshrined in the national<br />
constitution and several charters.<br />
• Professonalising midwifery care: In Malaysia and Tunisia, the Government invested in the expansion<br />
of community-based midwifery personnel who were trained and legally registered, based on a<br />
defined set of competencies. These midwives formed the backbone of each country’s rural health<br />
services system.<br />
• Strengthening health systems and promoting access to care in health facilities: Beginning in the<br />
1950s, Malaysia established a strong primary health care infrastructure—an extensive network of<br />
rural health facilities providing maternal health services was built; and skilled providers were trained<br />
and deployed to staff these facilities. The Government placed high priority on providing free health<br />
care and ensuring that health facilities were equitably distributed in an effort to reach the rural poor.<br />
2
Skilled <strong>Care</strong> During Childbirth: Country Profiles Introduction<br />
• Improving access to emergency obstetric services and establishing referral and transport systems:<br />
In Sri Lanka, the establishment of a network of primary health care centres was supported by the<br />
development of specialised obstetric services to treat emergency complications. Subsidised transport<br />
systems were established between primary and referral facilities, and from 1960–80, the number of<br />
rural facilities providing basic and comprehensive emergency obstetric care increased dramatically.<br />
• Ensuring access to family planning services: In 1965, Tunisia implemented a national family<br />
planning programme as part of its basic health care system. The Government partnered with<br />
non-governmental organisations (NGOs), religious leaders, and the media in a social mobilisation<br />
campaign to promote family planning. Midwives became the key cadres of health providers providing<br />
family planning and maternal care.<br />
• Improving the quality of available services through effective monitoring systems (e.g. maternal<br />
death audits): Developed and refined over a period of 40 years, Malaysia’s system for investigating<br />
the cause of maternal deaths provides a mechanism for continuously improving the quality of existing<br />
health services—by highlighting reasons for sub-standard care, assessing the quality of antenatal and<br />
obstetric care, and identifying improvements in maternal health programmes.<br />
• Encouraging community involvement and investment in maternal health care: Botswana has<br />
developed a range of information, education, and communication (IEC) activities to raise awareness<br />
about safe motherhood and encourage the use of services. These include printed materials, radio, and<br />
health education sessions.<br />
What These Profiles Contain<br />
Each of the country profiles includes: basic socio-demographic information; the policy and supporting<br />
framework for reducing maternal mortality and improving skilled care; the main interventions that<br />
were or are being implemented that relate to the goal of increasing skilled care during childbirth; and<br />
a box summarising the main ingredients of each country’s success story.<br />
These profiles are intended to provide a descriptive overview of the process in the four countries that<br />
led to a reduction in maternal mortality and improvements in skilled care during childbirth. Adapted<br />
from reports prepared by the “low maternal mortality” teams ✝ and supplemented from published and<br />
unpublished literature, the primary aim of these profiles is to provide concrete examples of countries<br />
that have been successful in improving maternal health through increased coverage of skilled care<br />
during childbirth. As such, the profiles complement the other components of the Skilled <strong>Care</strong> During<br />
Childbirth Information Kit, in particular the Skilled <strong>Care</strong> During Childbirth Information Booklet and<br />
Policy Brief, which provide policy and programmatic guidelines for individuals and organisations<br />
working to improve coverage of skilled care.<br />
The country profiles are designed for programme planners and managers working in governments,<br />
NGOs, and professional associations; and representatives of funding agencies, technical assistance, and<br />
research organisations active in the field. In addition, these profiles may be useful to policy-makers<br />
and members of the media interested in health and development issues.<br />
✝ The representatives of the low maternal mortality country teams included: Mabel Magowe and Lucy Sejo Maribe (Botswana);<br />
Drs. Raj Karim, Ravindran Jegasothy, and Mahani Yusoff (Malaysia); Dr. Anoma Jayathilaka and Daya Kumurage (Sri Lanka);<br />
and Dr. Mounira Garbouj and Atf Gherissi (Tunisia).<br />
3
Skilled <strong>Care</strong> During Childbirth: Country Profiles Botswana<br />
TUNISIA<br />
SRI LANKA<br />
MALAYSIA<br />
Botswana<br />
Introduction<br />
Population size (millions) (1) 1.6<br />
Population distribution (%) (1)<br />
Rural 50<br />
Urban 50<br />
Adult illiteracy rate (%) (1)<br />
Male 25<br />
Female 20<br />
GDP (US$ millions) (1) 5,285<br />
% GDP spent on health* 2.5<br />
Total fertility rate (1) 4.0<br />
Contraceptive prevalence (%) (2) 33<br />
National maternal mortality ratio ✝ 480<br />
Skilled care during childbirth<br />
requires the presence of a<br />
doctor or midwife, or a nurse<br />
with midwifery skills, who is<br />
trained to manage normal<br />
labour and delivery, recognise<br />
complications, and offer<br />
either emergency treatment<br />
or immediate referral to health<br />
centres for more advanced<br />
care. Skilled care also<br />
requires functioning referral<br />
and transport systems and<br />
necessary drugs, equipment,<br />
and supplies.<br />
Botswana is a landlocked country in the centre of Southern Africa, bordered by Namibia, South Africa,<br />
Zambia, and Zimbabwe. Its population is small but rapidly growing, with a trend toward urbanisation.<br />
Botswana is also youthful: in 2000, approximately 42% of its citizens were under the age of 15. (1)<br />
At independence in 1966, Botswana was one of the poorest countries in Africa with Gross National<br />
Product (GNP) per capita of about US$12. However, the discovery of diamonds, coupled with prudent<br />
economic management and political stability, dramatically increased the GNP per capita to US$3,300<br />
by the year 2000.<br />
Trends in health and development: Government spending on the public sector exceeds 30% of Gross<br />
Domestic Product (GDP), of which 8% is spent on health. (3) This investment in infrastructure and<br />
services has led to tremendous improvements in a number of health and social indicators, including<br />
the under-five mortality rate, access to clean drinking water, and life expectancy at birth. Botswana’s<br />
total fertility rate experienced a steady decline, from 6.1 children per woman in 1980 to 4.0 children<br />
in 2000. (1) In education, Botswana has achieved significant improvements in female primary<br />
education enrolment and adult literacy levels.<br />
Despite these achievements in health and development, Botswana is now struggling with one of the<br />
highest HIV infection rates in the world. An estimated 35% of the adult population is HIV infected, ✦<br />
and in 1998 approximately 35% of pregnant women were HIV positive. +<br />
Maternal health: In 1973, the Ministry of Health (MOH) formally established a national Maternal and<br />
Child Health/<strong>Family</strong> Planning (MCH/FP) programme, coordinated by the MCH/FP Unit in the MOH. As<br />
part of the national programme, the Government developed a network of health care infrastructure<br />
throughout the country for provision of integrated MCH/FP services (see section on Developing Health<br />
Services Infrastructure).<br />
Although antenatal, delivery, and postnatal services were made available to women in the 1970s,<br />
Botswana’s maternal health situation did not improve. In 1984, one-third of women gave birth without<br />
a skilled attendant present during childbirth and just over half sought postpartum care. In 1993, a<br />
study of maternal deaths found that haemorrhage, sepsis, and obstructed labour accounted for almost<br />
* This reflects public health expenditures, as percentage of GDP, and consist of recurrent and capital spending from government<br />
budgets and social health insurance funds.<br />
✝ The maternal mortality ratio or MMR is the number of women who die during pregnancy or childbirth per 100,000 live births.<br />
This estimate is from the publication, Maternal Mortality in 1995: Estimates developed by WHO, UNICEF, UNFPA, and is assumed<br />
to be high given the relatively high coverage and good quality services of Botswana’s health system. The government conducted<br />
a pilot study to test data collection tools for an upcoming study that will produce a revised estimate of maternal mortality and<br />
provide data on the leading causes of maternal mortality and circumstances surrounding maternal deaths.<br />
✦ 1999.<br />
+ 1998, sentinel surveillance.<br />
4
Skilled <strong>Care</strong> During Childbirth: Country Profiles Botswana<br />
60% of maternal deaths (see Figure 1). (4) In addition, 18% of maternal deaths were among teenagers<br />
between 15 to 19 years, and sepsis (mainly due to unsafe abortion) accounted for 33% of these deaths.<br />
FIGURE 1 ><br />
CAUSES OF MATERNAL MORTALITY<br />
Botswana’s response has been a focused, carefully planned safe motherhood programme (see next<br />
section), which aims to significantly improve the quality and coverage of maternal health care. The<br />
1996 Botswana <strong>Family</strong> Health Survey indicates that use of maternal health services has improved (see<br />
Figure 2): coverage of antenatal care (ANC) has increased to 94%; the percentage of assisted deliveries<br />
increased to 87%; and postpartum coverage to 85%.<br />
16%<br />
17%<br />
9%<br />
28%<br />
30%<br />
FIGURE 2 ><br />
SELECTED INDICATORS FROM THREE BOTSWANA FAMILY HEALTH SURVEYS<br />
100%<br />
80%<br />
60%<br />
40%<br />
1984<br />
Haemorrhage<br />
Sepsis<br />
Hypertension<br />
Indirect causes<br />
Obstructed labour<br />
20%<br />
0%<br />
23 24 17 23 33 42 90 92 94 66 78 87 54 71 85<br />
Teenage<br />
Pregnancy<br />
Contraceptive<br />
Prevalence<br />
ANC<br />
Attendance<br />
Supervised<br />
Deliveries<br />
Postnatal <strong>Care</strong><br />
*ANC attendance is at least 4–5 times during pregnancy, starting before 24 weeks.<br />
1988<br />
1996<br />
Laws, Policies, and Related Programmes<br />
Laying the groundwork: In October 1990, a high-level delegation led by the current President,<br />
Mr. Festus Mogae, attended the Southern African Development Cooperation (SADCC) Safe Motherhood<br />
Conference in Zimbabwe. Following the conference, a series of activities were undertaken to raise<br />
awareness, involve local organisations, and gather specific information about the problem so that a<br />
national plan could be developed (see sidebar on next page).<br />
The National Programme: Safe motherhood is an integral component of the broader health<br />
programme. The MCH/FP Unit in the <strong>Family</strong> Health Division is responsible for coordinating the safe<br />
motherhood programme using a broad-based, multi-sectoral approach to address the wider range<br />
of problems that increase maternal morbidity and mortality. The programme’s overall goals include: (5)<br />
• Improving the quality, efficiency, and effectiveness of MCH/FP services;<br />
• Increasing the accessibility of services;<br />
• Strengthening and developing IEC and data collection systems;<br />
• Improving organisation and management of MCH/FP services; and<br />
• Reducing the incidence and consequences of unsafe induced abortion.*<br />
The supporting policy framework: As part of its holistic approach to women’s health and development,<br />
the Government has formulated a series of policies that bolster safe motherhood goals, including:<br />
• <strong>Family</strong> Planning Policy Guidelines and Services Standards (1987) confirm the right of all individuals<br />
to reproductive health services based on choice; and specify the types of services to be provided, the<br />
cadres of staff to provide these services, and the groups to receive them. These guidelines were<br />
revised in 1994 to remove medical barriers to family planning.<br />
• National Health Policy (1995) recommends public and private sector partnership in matters of health<br />
and attention to high-risk groups.<br />
* Abortion in Botswana is permitted in the following circumstances: if the pregnancy could endanger the pregnant woman’s life;<br />
if the pregnancy is a result of rape case or incest; or if a serious disability of the foetus can be determined.<br />
5
Skilled <strong>Care</strong> During Childbirth: Country Profiles Botswana<br />
SAFE MOTHERHOOD:<br />
STEP-BY-STEP<br />
In November 1990, a<br />
conference for the Members<br />
of Parliament and the House<br />
of Chiefs was held in<br />
Gaborone to publicise the<br />
issue and mobilise political<br />
support. At the same time,<br />
the <strong>Family</strong> Health Division<br />
of the Ministry of Health<br />
organised a workshop on<br />
communication strategies<br />
for safe motherhood<br />
and HIV/AIDS prevention.<br />
In 1992, a multisectoral<br />
Safe Motherhood Task Force<br />
was established to help<br />
develop, implement, and<br />
monitor a national safe<br />
motherhood programme.<br />
The Task Force meets regularly<br />
and includes representatives<br />
from the government,<br />
NGOs, and training institutions,<br />
among others.<br />
In 1993, two key studies<br />
were conducted to help<br />
formulate a national plan:<br />
> Safe Motherhood in<br />
Botswana: Situation Analysis<br />
which reviewed available<br />
information on the extent of<br />
maternal mortality and its<br />
causes and consequences, as<br />
well as other women’s health<br />
issues, and recommended<br />
corrective strategies;<br />
> Determinants of Maternal<br />
Mortality in Botswana:<br />
An institutional, household and<br />
community perspective,<br />
conducted by the MCH/FP<br />
Unit and UNICEF, which<br />
examined maternal mortality<br />
records between 1990–1992<br />
to identify direct and<br />
indirect causes of maternal<br />
mortality.<br />
• Policy on Women and Development (1995) advocates adolescent-friendly reproductive health<br />
services in the context of women and development.<br />
• National Population Policy (1996) states that the individual is central to development efforts and that<br />
the goal of health and social services is “improved quality of life and living standards of all people<br />
in Botswana.”<br />
Critical Interventions to Increase Skilled <strong>Care</strong> During Childbirth<br />
A series of focused interventions have contributed to Botswana’s success in lowering maternal<br />
mortality and increasing rates of skilled care during childbirth:<br />
Developing Health Services Infrastructure<br />
Botswana has developed a well-distributed health services network such that the majority of the<br />
population (86%) lives within 15 km of a health facility. The health care system is structured along<br />
the following lines:<br />
• District/referral hospitals (1:100,000–350,000 population) have an operating theatre to perform<br />
C-sections, blood transfusions, and other advanced services.<br />
• Primary hospitals (1:12,000–35,000 population) are found in remote, low-density areas and staffed<br />
by medical officers and registered nurse-midwives. These facilities provide the same advanced<br />
emergency services available in district hospitals.<br />
• Health clinics (1:5,000–10,000 population) are staffed by registered nurses and family welfare<br />
educators (FWEs), and provide MCH services, treatment and diagnosis of common diseases, and<br />
simple laboratory tests.<br />
• Health posts emphasise preventive care (basic MCH/FP services, environmental health, first aid, and<br />
diagnosis and treatment of common diseases). Health posts are staffed primarily by FWEs, although<br />
some have nurses on staff. Each village with a population of 500–1,000 has a health post.<br />
• Mobile clinics reach remote populations on a monthly schedule, and are staffed by registered nurses<br />
or midwives. The mobile clinics provide limited primary health services (simple curative and basic<br />
MCH services).<br />
Health posts are open from 7:30AM to 4:30PM five days a week, while health clinics, primary hospitals,<br />
and district/referral facilities are open around the clock.<br />
Access to facilities and services varies and remains problematic in remote areas (such as the western,<br />
northern and northwestern parts of the country), though many facilities have been upgraded and new<br />
health units are being developed as an ongoing government project. Since 1996, there has been greater<br />
emphasis on increasing the number of health clinics and posts with trained nurses and midwives who<br />
provide basic maternal health services in communities (see Figure 3), and improving links to referral<br />
levels for emergency care.<br />
FIGURE 3 ><br />
NUMBER OF HEALTH FACILITIES BY TYPE (HEALTH STATISTICS REPORT 1997)<br />
800<br />
600<br />
720 710<br />
400<br />
253 273<br />
133 146<br />
200<br />
1996/1997<br />
77 86<br />
63 51<br />
16 16 14 17<br />
0 2000<br />
District<br />
Hospital<br />
Primary<br />
Hospital<br />
Clinic<br />
with<br />
Maternity<br />
Clinic<br />
without<br />
Maternity<br />
Health<br />
Post with<br />
Nurse<br />
Health<br />
Post<br />
without<br />
Nurse<br />
Mobile<br />
Stops<br />
6
Skilled <strong>Care</strong> During Childbirth: Country Profiles Botswana<br />
Drugs are provided under the rules of the Drugs Regulatory Committee, and are generally available,<br />
although some shortages exist, mainly in very remote areas. Equipment and supplies for basic maternal<br />
health services are also generally available (6) , though distribution and logistical problems do result in<br />
the frequent unavailability of such small yet necessary items as the angle poise lamp or blood<br />
pressure machines. Emerging programmes (i.e. the Programme for the Prevention of Mother-to-Child<br />
Transmission of HIV) have helped secure more and better equipment (i.e., silicon vacuum cups have<br />
replaced metal cups for vacuum extraction).<br />
Establishing Transport & Referral Systems<br />
A referral system links health posts with health clinics and hospitals. Protocols have been developed that<br />
allow a health provider to send a patient directly to a facility where specific services can be obtained<br />
(for example, in an emergency, a woman may be referred directly from a health post to a<br />
district hospital). For referral, most health facilities have a radio and receiver, at least one vehicle, and<br />
a telephone. In cases where the only vehicle is unavailable, paid transport from private sources will<br />
be arranged.<br />
Investing in Health Personnel<br />
Botswana has invested in improving the training and distribution of key cadres of health providers<br />
providing maternity services. Nurses and midwives form the backbone of the health care system<br />
and are the main providers of maternal health care. Most nurses provide routine antenatal and family<br />
planning services; those with midwifery skills provide the more complex family planning, antenatal,<br />
delivery, and postpartum care. Midwives trained in life-saving skills attend obstetric emergencies and<br />
co-manage obstetric medical/surgical complications with doctors.<br />
In addition to doctors, nurses, and midwives, FWEs play a role in providing maternal health services.<br />
They are primary school graduates who educate and motivate the community on issues related to safe<br />
motherhood—encouraging women to deliver in an institutional setting, and providing counselling and<br />
health education to communities living within a five kilometre radius of health posts.<br />
Training programmes: Over the last ten years, Botswana has improved and expanded training of<br />
health personnel providing midwifery care. In 1993, the National Task Force for Safe Motherhood<br />
commissioned a small expert group to review training for health providers. This group reviewed existing<br />
standards, protocols, and training manuals, and made the following improvements:<br />
• Pre-service midwifery training: The midwifery curriculum was increased to an 18-month programme<br />
with greater emphasis on antenatal care, labour, and delivery. It emphasised prevention and care<br />
strategies to improve maternal well-being. New content was added on the underlying causes of poor<br />
maternal health; safety and care during pregnancy, childbirth, and post-partum; and emergency care.<br />
• Since 1994, 562 midwives have gone through the training programme. Plans to increase the number<br />
of midwives to meet national targets and service requirements are underway. One obstacle to meeting<br />
this goal is the limited capacity of training institutions. Currently, there are only three midwifery<br />
training schools, as opposed to eight registered nurse training schools. Additional training sites for<br />
midwives are planned in the Southeast region of the country.<br />
• Other reproductive health training: Training for midwives in family planning has also been<br />
strengthened under the Botswana Population Sector Assistance Programme. Emphasis is placed on<br />
clinical skills and counselling, integration of STI/HIV/AIDS into family planning, and prevention,<br />
screening, and management of sexually transmitted infections.<br />
• In-service life-saving skills education: A six-week curriculum on high-risk pregnancies and life-saving<br />
skills has also been introduced for midwives and doctors. Skills include: procedures for completion<br />
7
Skilled <strong>Care</strong> During Childbirth: Country Profiles Botswana<br />
of delivery (such as evacuation of the uterus for incomplete, inevitable abortion; vacuum extraction;<br />
and manual removal of retained placenta), repair of third degree lacerations, breech extraction, and<br />
newborn resuscitation. In addition, doctors receive training in the repair of fourth degree lacerations<br />
and emergency caesarean section. Between 1994–1995, 68 midwives and 12 medical officers were<br />
trained in this programme.<br />
Competency-based training is provided to all existing staff to ensure that they have the necessary<br />
skills in:<br />
• Counselling and communicating with patients;<br />
• General programme management;<br />
• Treatment of high-risk and complicated maternity cases;<br />
• New developments in contraceptive technology; and<br />
• Management of STIs, particularly AIDS.<br />
Supervision: The senior staff member within each unit is responsible for the daily supervision of<br />
midwives. The MCH/FP Unit in the MOH conducts yearly supervisory visits at the district level to<br />
monitor progress in implementation of programmes.<br />
Despite considerable improvements, Botswana suffers from a shortage of qualified health personnel.<br />
The HIV/AIDS situation has further exacerbated the already inadequate levels of personnel. Specialists<br />
such as obstetricians, paediatricians, and surgeons are only found in the country’s two referral hospitals.<br />
Since Botswana does not have a medical training school for doctors, 85% of the doctors employed by<br />
the Government are expatriates.<br />
Nurses and midwives are also in critically short supply (see Table 1). In 1997, there were only<br />
41.3 nurses (including midwives, registered nurses without midwifery skills, and enrolled nurses) per<br />
10,000 population.<br />
TABLE 1 ><br />
RATIO OF HEALTH PERSONNEL (PER 10,000 PEOPLE)<br />
1991<br />
1993<br />
1996<br />
1997<br />
Doctors<br />
2.3<br />
2.3<br />
4.0<br />
4.2<br />
Nurses<br />
(includes midwives)<br />
22.3<br />
23.1<br />
39.6<br />
41.3<br />
<strong>Family</strong> Welfare Educators<br />
(FWEs)<br />
5.0<br />
5.0<br />
7.3<br />
7.5<br />
Total<br />
29.6<br />
30.4<br />
50.9<br />
53.0<br />
Establishing Standards and Protocols<br />
Standards and protocols for routine maternity care and the management of high-risk and emergency<br />
services have been reviewed and improved. Protocols have been developed for general care, to specify<br />
which services will be provided at each type of facility, and for referral. These tools are used to guide<br />
in-service and pre-service training for midwives and other health providers.<br />
The obstetric record, a tool for recording the progress of pregnancy, labour, delivery and postpartum<br />
care, was revised in 1995. The tool provides a mechanism for monitoring women during antenatal<br />
care, delivery (it includes a partograph), and postnatal care. A woman retains this record throughout<br />
pregnancy, and she is free to visit any health facility for antenatal, delivery, and postnatal services.<br />
8
Skilled <strong>Care</strong> During Childbirth: Country Profiles Botswana<br />
Community Outreach<br />
An IEC strategy was developed during the 1990s to raise awareness within communities and to<br />
encourage the use of services. The strategy included materials such as posters, wall charts, and<br />
pamphlets, as well as a video in local languages and English, with an accompanying booklet for more<br />
information. Radio is also used extensively. Health talks are given every morning at the clinics on a<br />
range of topics including the need for skilled care during childbirth. However, monitoring shows that<br />
most facilities still do not have these materials. (6) Where they are available, the nurses and midwives<br />
do not use them adequately as reference.<br />
Monitoring and Evaluating the Safe Motherhood Programme<br />
Monitoring and evaluation is an integral part of the national safe motherhood programme. While the<br />
programme has not been evaluated as an entity, the <strong>Family</strong> Health Division monitors and evaluates<br />
its progress on an on-going basis through support visits, and conducts more targeted research as the<br />
need arises. It also releases yearly statistical reports, which are used to help evaluate the performance<br />
of its programmes.<br />
In 1996, two studies helped to highlight the strengths and weaknesses of the evolving safe motherhood<br />
programme. The Situation Analysis of the Maternal and Child and <strong>Family</strong> Planning Programme and<br />
the Botswana <strong>Family</strong> Health Survey identified a number of areas for improvement (such as inadequacies<br />
in training, staffing, and equipment, and access to care in remote areas), along with strategies to<br />
address them.<br />
Public Expenditure on Health<br />
As Table 2 indicates, government expenditure in the public sector has generally exceeded 35% of GDP.<br />
Since 1995, government expenditures on health have almost doubled (from US$45 million to US$89<br />
million in 1999). (7) With the advent of HIV/AIDS, however, the government has had to reprogramme<br />
funds to address the epidemic, reducing the already inadequate levels of funding for current<br />
programmes such as life-saving skills training.<br />
For additional information about<br />
Botswana’s safe motherhood programme, contact:<br />
Mrs. Lucy Maribe<br />
Principal Health Officer, MCH/FP Division<br />
Ministry of Health<br />
P.O. Box 992<br />
<strong>Family</strong> Health Division<br />
Gaborone Botswana<br />
Tel: 267 353 561<br />
Fax: 267 302 092<br />
E-mail: lmaribe@gov.bw<br />
TABLE 2 ><br />
PUBLIC AND HEALTH EXPENDITURES<br />
(SELECTED YEARS)<br />
YEAR<br />
1981<br />
1991<br />
1994<br />
1996<br />
2000<br />
Public<br />
Expenditure<br />
(% of GDP)<br />
37.9<br />
43.2<br />
34.1<br />
35.5<br />
39.6<br />
THE KEYS TO BOTSWANA’S<br />
SUCCESS ARE:<br />
> A carefully planned national<br />
strategy based on research and<br />
pronounced political support.<br />
> Collaboration and integration<br />
at all levels.<br />
> Significant resources invested<br />
in health, in real value and<br />
as percentage of Government<br />
spending.<br />
> Trained personnel for management<br />
of obstetric emergencies.<br />
> Improved access to health<br />
facilities and services.<br />
> Integrated MCH/FP services<br />
(supermarket approach).<br />
> Availability of midwives at all<br />
levels of the health care system.<br />
> Good referral system from<br />
the lowest level facility to the<br />
highest level.<br />
> Availability of emergency<br />
obstetric services in hospitals.<br />
Health Share<br />
of Public<br />
Expenditure<br />
5.2<br />
5.1<br />
6.1<br />
6.0<br />
8.0<br />
Sources<br />
1 World Development Indicators 2002. World Bank, Washington DC, 2002.<br />
2 1988, any method. World Contraceptive Use 2001. United Nations Population Division. Department of Social and Economic Affairs. New York, May, 2002.<br />
3 2000; Common Country Assessment (CCA) 2001.<br />
4 L. Owuor-Omondi, et al., Determinants of Maternal Mortality in Botswana: An Institutional, Household and Community Perspective, Ministry of Health, 1993.<br />
5 Safe Motherhood Task Force, Safe Motherhood in Botswana: A Situation Analysis, 1992.<br />
6 B. Baakile, L. Maribe, et al. A Situational Analysis of the Maternal and Child and <strong>Family</strong> Planning. Africa Project II, Population Council, Nairobi, Kenya, 1996.<br />
7 Statistical Bulletin, Central Statistics Office, Botswana Ministry of Finance and Development Planning, 1999.<br />
9
Skilled <strong>Care</strong> During Childbirth: Country Profiles Malaysia<br />
TUNISIA<br />
SRI LANKA<br />
Malaysia<br />
BOTSWANA<br />
Introduction<br />
Population size (millions) (1) 23.3<br />
Population distribution (%) (1)<br />
Rural 43<br />
Urban 57<br />
Adult illiteracy rate (%) (1)<br />
Male 9<br />
Female 17<br />
GDP (US$ millions) (1) 89,659<br />
% GDP spent on health 1.4<br />
Total fertility rate (1) 3.0<br />
Contraceptive prevalence (%) (2) 55<br />
National maternal<br />
mortality ratio (3) 39<br />
Skilled care during childbirth<br />
requires the presence of a doctor<br />
or midwife, or a nurse with<br />
midwifery skills, who is trained<br />
to manage normal labour and<br />
delivery, recognise complications,<br />
and offer either emergency<br />
treatment or immediate referral<br />
to health centres for more<br />
advanced care. Skilled care<br />
also requires functioning referral<br />
and transport systems and<br />
necessary drugs, equipment,<br />
and supplies.<br />
Malaysia lies in the heart of Southeast Asia. It is an extremely diverse country with numerous<br />
ethnic groups in 13 states and 2 federal territories. It has a steadily growing population, with a trend<br />
toward urbanisation.<br />
Since its independence in 1957, Malaysia has made a strong commitment to health and development,<br />
especially in the area of women’s health and safe motherhood. Malaysia has moved from a fragmented,<br />
rudimentary health care system, especially in rural areas, to an extensive infrastructure that provides<br />
comprehensive health care to more than 90% of its population, with many services (antenatal care,<br />
immunisations) free of charge.<br />
As a result of this investment, life expectancy in Malaysia has risen to 73 years for women and 70 for<br />
men (from less than 50 years in 1957); infant mortality has dropped from 30 deaths per 1,000 live<br />
births in 1980 to 8 in 2000; and the total fertility rate declined from 6.7 in 1957 to 3.0 in 2000.<br />
Malaysia’s commitment to women extends into all areas of development: women have equal rights in<br />
education, voting, and employment. Over the last decade, more girls than boys have enrolled in tertiary<br />
education. Approximately 48% of women are in the paid workforce, and women hold senior<br />
government positions.<br />
Maternal health: Maternal mortality has fallen dramatically in Malaysia over a period of 60 years,<br />
from 1,100 per 100,000 live births in 1933 to 39 deaths per 100,000 live births in 1995 (3,4) (see Figure 1).<br />
A central factor in this decline has been high-level government commitment to ensuring that<br />
quality maternal health services are accessible to the vast majority of the population, particularly in<br />
underserved and rural areas.<br />
An extensive community-based programme provides primary health care services, including<br />
immunisations, antenatal care, and delivery services, to the rural population. Skilled birth attendants<br />
(primarily midwives) are the first point of contact for maternity care through home visits, and in<br />
village health clinics and hospitals. (4)<br />
Between 1949–1997, the percentage of live births attended by a skilled health provider increased<br />
dramatically—from approximately 30% to over 95%. (4) During this period, government midwives<br />
increasingly conducted home deliveries and demand for childbirth in public sector hospitals expanded<br />
considerably. In 1995, of the 98% of births attended by skilled health providers, 66% were delivered<br />
in government hospitals, 20% in private hospitals or maternity homes, and 12% at home. (5)<br />
Currently, most maternal deaths are due to: postpartum haemorrhage, severe anaemia, hypertensive<br />
disorders of pregnancy, puerperal sepsis, and obstructed labour. Abortion is permitted to save the life<br />
of the pregnant woman and to preserve her physical or mental health; deaths from unsafe abortion<br />
account for less than 1% of total maternal deaths. (6)<br />
10
Skilled <strong>Care</strong> During Childbirth: Country Profiles Malaysia<br />
FIGURE 1 ><br />
MATERNAL MORTALITY TREND IN PENINSULAR MALAYSIA (1933–1995)<br />
1200<br />
MATERNAL DEATHS PER<br />
100,000 LIVE BIRTHS<br />
1000<br />
800<br />
600<br />
400<br />
200<br />
0<br />
1930 1940 1950 1960 1970 1980 1990<br />
YEAR<br />
Laws, Policies, and Related Programmes<br />
Laws and policies supportive of maternal health in general and skilled care during childbirth in<br />
particular have been in place since the colonial period. After independence, the national government<br />
accorded high priority to the goal of maternal mortality reduction by investing in a range of<br />
programmes and strategies to improve MCH (see next section).<br />
Professionalisation of midwifery: In 1932, legislation was introduced to regulate the practice of<br />
midwifery. Midwives as a cadre of health personnel were trained, certified, and legally registered based<br />
on demonstrated competency in a defined list of clinical skills. They were deployed as front-line<br />
community health workers to provide maternal care (see section Investing in Midwifery Personnel for<br />
information on training and supervision of midwifery personnel). (4)<br />
Registration of Births and Deaths: A system for the registration of births and deaths was introduced<br />
in the colonial period; in the 1950s a national civil registration system, based on the issuance of a<br />
personal identity card, provided a means of obtaining reliable vital statistics.<br />
Investments in Women: Several laws and policies that aim to improve women’s economic and social<br />
status, and foster equal access to educational opportunities, have provided an enabling environment<br />
for expanding access to skilled care:<br />
• National Women’s Policy ensures equal opportunities for education, employment, and access to basic<br />
health and social services; prevents discriminatory policies and practises; and empowers women.<br />
• Education Policy provides equal access for girls (and boys) to free primary and secondary education,<br />
and assistance with school uniforms, textbooks, and school meals for the poor.<br />
• Rural Development Policy provides basic infrastructure, including housing, schools, clinics, roads,<br />
transport, communication, and poverty alleviation programmes.<br />
• Vision 2020, a forward-looking policy, includes reduction of mortality within its nine priority actions<br />
for a caring society.<br />
Emphasis on Poverty Reduction: Malaysia’s efforts to improve maternal health and increase access to<br />
skilled care were implemented within the context of a poverty alleviation strategy that emphasised<br />
reducing gaps between the rich and poor. This has ensured that disadvantaged groups, particularly the<br />
rural poor, benefit more proportionately from health and social programmes. (4)<br />
Collaboration: With the goal of improving the quality of maternal health services, the Government<br />
has fostered a high level of collaboration at the policy, programme, and community levels:<br />
• Policies and standards: In 1971, National, State, and District MCH Committees were formed to help<br />
develop and oversee programme strategies and standards for care. These multi-sectoral committees<br />
draw on the expertise of medical specialists and public health personnel as well as key state- and<br />
district-level decision-makers. National policies, manuals, and protocols are developed by the<br />
National Committee and its task forces. Local maternal and child health problems are discussed at<br />
the district level and referred for policy or technical guidance as needed.<br />
NATIONAL SAFE<br />
MOTHERHOOD PROGRAMME<br />
Malaysia’s national safe motherhood<br />
programme has employed a<br />
multi-strategy approach to reducing<br />
maternal death, focusing on:<br />
> improving coverage by ensuring<br />
access to basic health services;<br />
> upgrading the quality of essential<br />
obstetric care in district hositals;<br />
> streamlining and improving<br />
referral and feedback systems;<br />
> enhancing providers’ capacity<br />
and skills for managing pregnancy<br />
and delivery complications; and<br />
> reporting maternal deaths. (7)<br />
11
Skilled <strong>Care</strong> During Childbirth: Country Profiles Malaysia<br />
• Programme development: Since the early 1990s, strategies to reduce maternal mortality have been<br />
developed at the local level using an inclusive District Team Problem Solving Approach. Teams identify<br />
their own problems, decide on the best solutions, design appropriate interventions, and formulate a<br />
district plan of action (see section Evaluation and Review of the Safe Motherhood Programme for<br />
further information).<br />
• Staff involvement: Medical, nursing, and midwifery associations are consulted to upgrade training for<br />
life-saving skills, and training curricula are reviewed by nursing and midwifery regulatory boards.<br />
• Community outreach: Women’s NGOs, community, and religious groups have played a role in<br />
community and family education, and increasing awareness in communities.<br />
Critical Interventions to Increase Skilled <strong>Care</strong> During Childbirth<br />
Within the context of supportive policies and legislation to improve maternal health (see previous<br />
section), Malaysia implemented a series of phased interventions to expand access of the rural poor to<br />
health services and increase the quality of existing services through improved management and<br />
community mobilisation.<br />
Expanding Community Access to Health Services<br />
In 1955 the Government implemented an extensive rural health programme, with the aim of providing<br />
primary health care (including such maternity services as antenatal care, delivery services, and<br />
postpartum care) at the community level. Rural health clinics were built, public hospital services<br />
expanded, and increased numbers of skilled providers (principally midwives and nurses) were trained<br />
and deployed to serve rural communities. By 1977 most of the rural population lived within two-four<br />
kilometres of a health facility by tarred road. Those who live far from health clinics are served by<br />
mobile health teams.<br />
Investing in Midwifery Personnel<br />
Health workers that provide maternity care include midwives,* nurses, medical officers, and specialist<br />
obstetricians. Midwives are the front-line providers of maternity care in rural areas—they provide<br />
antenatal and postnatal care and perform all normal deliveries at health facilities or through home<br />
visits. Nurses provide back-up support to midwives by handling emergencies in cases where a doctor<br />
with obstetrical training is not available. While midwives and nurses are the first point of contact for<br />
maternity services, medical officers and specialist obstetricians provide the first line of referral care.<br />
Reorganisation of Rural Health <strong>Care</strong><br />
In 1975, the existing three-tiered rural health system was reorganised into a two-tier system<br />
in order to widen the scope of services offered to mothers at first contact, provide greater access<br />
to doctors, and streamline the referral system. Community-based midwives were upgraded to<br />
multi-purpose nurses with additional skills (see footnote below). (6)<br />
Health Centres (1:20,000) Community Clinics (1:4,000)<br />
Staff<br />
Services<br />
Doctor, dental officer, medical<br />
assistants, public health nurse, assistant<br />
nurses, staff nurses, midwives, lab<br />
assistant, dispenser, clerical assistant.<br />
Out-patient care, MCH care,<br />
environmental health, health education,<br />
family planning, dispensary.<br />
Community health nurse/midwife.<br />
MCH care, home delivery,<br />
home visiting, minor ailments,<br />
family planning, immunisation.<br />
* Before 1978, midwives were trained as single purpose health providers; their training was subsequently expanded to include<br />
child health and basic outpatient care, while retaining their core midwifery functions. As a cadre of health professionals,<br />
midwives have become known as community nurses.<br />
12
Skilled <strong>Care</strong> During Childbirth: Country Profiles Malaysia<br />
Training programmes: All professional health personnel receive midwifery training that emphasises<br />
hands-on practical experience and mastery of clinical skills:<br />
• Midwives/community nurses undergo 2 1/2 years of competency-based training in midwifery and<br />
basic outpatient care, which includes a practical internship in district hospitals and health centres.<br />
Since 1987, community nurses have been trained to administer oxytocics and intravenous infusions<br />
for postpartum haemorrhage; since 1993, they have been trained in the use of the partograph to help<br />
prevent delay in referral.<br />
• Staff nurses and public health nurses undergo a 3 1/2 year nursing course; staff nurses receive an<br />
additional year of midwifery training, and public health nurses receive an additional year of public<br />
health training.<br />
• Since 1987, all medical officers posted in health clinics and hospitals undergo a 4 to 7 month<br />
training in obstetrics and gynaecology to improve their proficiency in handling pregnancy and<br />
obstetric complications.<br />
Supervision: Based on a supportive, competency-based approach, supervision takes place according<br />
to established protocols and manuals. A written supervisory checklist, covering such areas as facility<br />
maintenance, record keeping, and interpersonal skills, guides the supervision of midwifery personnel.<br />
Supervisory staff provide on-the-spot feedback on clinical and programmatic matters; visits take place<br />
on a regular, preset schedule, though surprise visits are also conducted. Midwives are supervised<br />
by nurses, and doctors are supervised through regular case audits. The obstetrician covering a district<br />
hospital holds discussions on emergency management of complications and the appropriateness of referral.<br />
Establishing Transport and Referral Systems<br />
Systems for communication, transport, and referral ensure that all health facilities have transport<br />
(e.g. ambulance) to a higher level of care and that communication mechanisms (e.g. telephone) allow<br />
staff to discuss management of cases with senior personnel. In addition, midwives link the community<br />
with institutional health facilities by recognising complications and referring women requiring<br />
emergency care to the nearest health clinic.<br />
As referral systems were established, health facilities were upgraded in phases to provide essential<br />
obstetric care. Standardised equipment, supply, and essential drug lists ensure that necessary equipment<br />
and supplies (e.g. drugs, blood) are available in all appropriate health facilities.<br />
Referral systems may cut across state boundaries for the speedy referral and treatment of emergency<br />
cases. In river, coastal, and island areas, police and marine boats are mobilised to transport near-term<br />
pregnant women to the nearest health facility before the flood season.<br />
Community Outreach<br />
In an effort to improve the quality of health care services and increase utilisation, continuous<br />
education and community involvement have been a central component of the Government’s rural<br />
health services programme:<br />
• Community and religious leaders and influential individuals encourage women with identified<br />
pregnancy risks to deliver in hospitals.<br />
• Women who have survived a complicated delivery share their experiences with other women<br />
and families.<br />
• TBAs, who are respected community members, have been made partners in a critical network that<br />
links the health system, TBAs, and the community (see sidebar).<br />
INVOLVING TRADITIONAL<br />
BIRTH ATTENDANTS<br />
Until the 1960s, TBAs conducted<br />
most deliveries in rural and<br />
remote areas. As part of its rural<br />
health services programme,<br />
the Government worked with<br />
TBAs as partners to improve<br />
women’s access to a skilled<br />
midwife or nurse at the time<br />
of childbirth. For a limited time,<br />
TBAs were trained in basic<br />
hygiene care and in recognising<br />
and referring complications<br />
to the health centre. TBAs also<br />
became registered and<br />
certified partners in the health<br />
care system.<br />
TBAs were encouraged to<br />
continue a range of traditional<br />
services (e.g. accompanying<br />
mothers to hospitals,<br />
being present during delivery<br />
to attend to customary rituals,<br />
and providing care for the<br />
mother and newborn) considered<br />
valuable to women. Health<br />
workers were trained to value<br />
the role of TBAs in providing<br />
such services and to work<br />
with them as full partners. As<br />
a result of this approach, most<br />
deliveries are now conducted<br />
by government midwives.<br />
TBAs still play a key role in<br />
certain remote and underserved<br />
communities. For example, in<br />
Sabah (East Malaysia) TBAs<br />
conducted 12% of total deliveries<br />
in 1994.<br />
13
Skilled <strong>Care</strong> During Childbirth: Country Profiles Malaysia<br />
Health workers offer community education in health clinics and at home. Community midwives<br />
conduct antenatal home visits to ensure that families and communities are aware of the need for<br />
skilled care during childbirth and to make advance arrangements for transport, child care, etc. to<br />
prevent delays. Mass media has been used extensively through national and regional networks to offer<br />
weekly programmes on women’s health issues.<br />
Improved Quality and Management<br />
of the Maternal Health Programme<br />
While the period following independence was focused on increasing access to basic maternity care (see<br />
previous section), subsequent efforts (between the 1970s and 1990s) emphasised improving the quality<br />
of available services through better management. Since the 1970s, the primary indicator used for<br />
evaluating the maternal health programme has been the proportion of births attended by a skilled<br />
attendant, with districts evaluated based on their performance on this key indicator.<br />
Monitoring Maternal Deaths: The system for monitoring maternal deaths evolved over a period of 40<br />
years—from informal, sporadic investigations to the systematic programme in place today. During the<br />
colonial period, deaths were reported to local police authorities, and the government midwife would<br />
obtain information on maternal deaths. Such investigations involved hospital and district-level<br />
administrators working with members of the family and community. High-level officials visited areas<br />
where a maternal death occurred to draw attention to the event and raise awareness about the<br />
possible cause and means of preventing the death in question. It was made clear that this was a<br />
non-punitive review with the aim of learning the cause and circumstances of the death, and addressing<br />
deficiencies in the health system.<br />
In the 1980s, standard forms and procedures were developed in an effort to formalize the process of<br />
maternal death investigation; community leaders and supervisory personnel were involved in the<br />
investigation. In 1991, the existing system of maternal death investigations, the Confidential Enquiry<br />
of Maternal Deaths (CEMD), was established. Each maternal death is reviewed by committees at district,<br />
state, and national levels in a confidential, non-punitive, and timely manner to assess quality of<br />
antenatal and obstetric care, identify weaknesses and reasons for substandard care, and recommend<br />
improvements in maternal health programmes.<br />
Developing Standards and Protocols: The National MCH Committee (which consists of midwives,<br />
nurses, obstetricians, and representatives from academic and training institutions) defines standards<br />
for clinical care and referral through the development of manuals and protocols for different cadres<br />
of health providers, in collaboration with a range of stakeholders (see previous section on Laws,<br />
Policies, and Related Programmes).<br />
Standards and protocols are continuously revised and updated to reflect changing realities. In 1984<br />
national guidelines for antenatal and obstetric care were formulated and management protocols were<br />
developed for major causes of maternal mortality (postpartum haemorrhage, severe anaemia,<br />
hypertensive disorders of pregnancy, puerperal sepsis, and obstructed labour). These guidelines were<br />
amended in 1996 to include obstetric indicators that reflect quality of care.<br />
Norms, procedures, and standards for maternal care have also been developed for upgrading training<br />
and skills of midwifery and nursing personnel, and strategies to increase deliveries by professional<br />
health workers. For example, a colour-coded system was developed for evaluating pregnant women to<br />
try to identify those at risk of complications so that they can receive appropriate care.<br />
14
Skilled <strong>Care</strong> During Childbirth: Country Profiles Malaysia<br />
Evaluation and Review of the Safe Motherhood Programme: Regular, periodic evaluations and<br />
assessments are conducted on specific aspects of maternal care, and the results are used to modify and<br />
improve services. For example:<br />
• In 1984, a functional analysis of the health care system found deficiencies in training and supervision,<br />
as well as hostile environments in facilities, long waiting times, and non-systematic patient flow in<br />
clinics. As a result, norms and procedures were revised to reduce unnecessary procedures, and<br />
increase antenatal and postpartum visits; adapt the nursing and midwifery curriculum; improve<br />
interpersonal communication; and formulate a standard checklist for supportive supervision.<br />
• The Quality Assurance Programme was introduced in 1986 as a continuous assessment system for<br />
quality of care. Indicators of antenatal and obstetric quality of care were used to correct weaknesses<br />
in the health system and improve substandard care. In 1999, process indicators were added to ensure<br />
early action could be taken to avert maternal death.<br />
• Since the early 1990s, maternal mortality reduction strategies have been identified through a District<br />
Team Problem-Solving Approach, where districts identify deficiencies in care, determine<br />
strategies/solutions, and design interventions to address these difficulties through the development<br />
of a district plan of action. In 1999, a review found that the team approach to problem solving<br />
between health and hospital personnel was not easy to sustain, but that community outreach and<br />
mobilisation had increased women’s willingness to deliver in hospitals, reduced the incidence of<br />
births before arrival, and increased skilled care during deliveries.<br />
TABLE 1 ><br />
PUBLIC EXPENDITURE ON HEALTH<br />
SERVICES AND MATERNAL HEALTH<br />
<strong>CARE</strong> AS PERCENT OF GDP (4)<br />
Total Maternal<br />
Period Health Health<br />
Services <strong>Care</strong><br />
1950–55 NA NA<br />
1956–60 1.54 NA<br />
1961–65 1.71 NA<br />
1966–70 NA NA<br />
1971–75 1.79 0.32<br />
1976–80 1.63 0.36<br />
1981–85 1.59 0.41<br />
1986–90 1.51 0.40<br />
1991–95 1.44 0.37<br />
Public Expenditure on Maternal Health<br />
Since the 1950s, total public expenditure for health care has averaged about 1.4 to 1.8% of GDP; total<br />
expenditure on maternal health care in public sector hospitals and community services has been at<br />
modest levels—averaging 0.38% of GDP (see Table 1). (4)<br />
Maternal health services are largely provided through the public sector, and services, including skilled<br />
care at childbirth, are free-of-charge to the poor and mostly free to other groups. The Government has<br />
made concerted efforts to remove financial barriers, such as subsidising transport for emergency cases.<br />
For additional information about Malaysia’s<br />
safe motherhood programme contact:<br />
Raj Karim<br />
Regional Director<br />
<strong>International</strong> Planned Parenthood Federation<br />
246 Lorong Enau, off Jalan Ampang<br />
East and South East Asia and Oceania Regional Office (ESEAOR)<br />
Kuala Lumpur 50450 Malaysia<br />
Tel: 60 3 456 61 22/246/308<br />
Fax: 60 3 456 6386<br />
E-mail: rk@ippf.po.my<br />
THE KEYS TO MALAYSIA’S<br />
SUCCESS ARE:<br />
> High-level policy commitment<br />
to the goal of reducing maternal<br />
deaths and improving skilled<br />
care during childbirth.<br />
> Decentralized, multi-strategy<br />
approach which targets<br />
specific problems and addresses<br />
them through incremental<br />
and systematic improvements<br />
in health services, and hospital<br />
and community systems.<br />
> Collaboration at the policy,<br />
programme, and community levels.<br />
> Monitoring and evaluation<br />
systems to track improvements<br />
and determine deficiencies<br />
in care.<br />
> Community involvement<br />
and empowerment, including<br />
partnership with TBAs.<br />
Sources<br />
1 World Development Indicators 2002. World Bank, Washington DC, 2002.<br />
2 1994, any method. World Contraceptive Use 2001. United Nations Population Division. Department of Social and Economic Affairs. New York, May 2002.<br />
3 1995; Maternal Mortality in 1995: Estimates developed by WHO, UNICEF, UNFPA. WHO, Geneva, 2001.<br />
4 Indra Pathmanathan and Jerker Liljestrand, eds. Investing Effectively in Maternal Health: Malaysia and Sri Lanka. World Bank, Washington DC, 2002. In process.<br />
5 Safe Motherhood and the World Bank: Lessons from 10 years of Experience, Human Development Network Series, World Bank, 1999.<br />
6 1996; Report on the Confidential Enquiries into Maternal Deaths in Malaysia 1995-1996. Ministry of Health, Malaysia, 2000.<br />
7 A.T. Lim, Sharifah Tahir, and A. Vasanthamala. Combating Maternal Mortality: Lessons from Pasir Mas, Malaysia. <strong>International</strong> Council on Management<br />
of Population Programmes, 1998.<br />
15
Skilled <strong>Care</strong> During Childbirth: Country Profiles Sri Lanka<br />
TUNISIA<br />
Sri Lanka<br />
MALAYSIA<br />
BOTSWANA<br />
Introduction<br />
Population size (millions) (1) 19.4<br />
Population distribution (%)<br />
Rural 76<br />
Urban 24<br />
Adult illiteracy rate (%) (1)<br />
Male 6<br />
Female 11<br />
GDP (US$ millions) (1) 16,305<br />
% GDP spent on health 1.7<br />
Total fertility rate (1) 2.1<br />
Contraceptive prevalence (%) (2) 66<br />
National maternal<br />
mortality ratio (3) 60<br />
Skilled care during childbirth<br />
requires the presence of a doctor<br />
or midwife, or a nurse with<br />
midwifery skills, who is trained to<br />
manage normal labour and<br />
delivery, recognise complications,<br />
and offer either emergency<br />
treatment or immediate referral<br />
to health centres for more<br />
advanced care. Skilled care<br />
also requires functioning referral<br />
and transport systems and<br />
necessary drugs, equipment,<br />
and supplies.<br />
The Democratic Socialist Republic of Sri Lanka is an island situated in the Indian Ocean. The<br />
population is primarily rural with an agriculturally-based economy.<br />
Sri Lanka has long been dedicated to ensuring the social welfare and health of its citizens. Since<br />
the 1930s, comprehensive health services have been free of charge, and in 1945, the Government<br />
established a policy of universal free education from year one to university level—resulting in an overall<br />
literacy rate of 91% by 2000.*<br />
Sri Lanka has seen similar improvements in other health and social indicators: infant mortality fell<br />
from 82 deaths per 1,000 live births in 1950 to 15 deaths per 1,000 live births in 1997, (4) life expectancy<br />
has risen to 73 years; fertility declined steadily from 5.1 in 1953 to 2.1 in 2000; use of both traditional<br />
and modern contraceptive methods rose to 66% by 1993. (2)<br />
Investments in women’s health and development have been a central component of Sri Lanka’s<br />
success story. Women have equal rights in education, voting, and employment. They are guaranteed<br />
equality under the national constitution (1978), and are accorded human rights and freedoms on an<br />
equal basis with men. (5)<br />
Maternal health: Maternal mortality has declined considerably over the past five decades—from 1,660<br />
deaths per 100,000 live births in 1947 (5) to 60 deaths in 1995. (3) Skilled care during childbirth increased<br />
from 27% in 1939 to 89% in 1996. (4) Today, most women in Sri Lanka have access to skilled care<br />
during pregnancy and labour—almost all women (99%) receive antenatal care, 90% of women deliver<br />
in institutional settings, and 95% of births are assisted by a skilled attendant.<br />
MCH has received high priority in the Government’s primary health care policy and infrastructure.<br />
Since the mid-1920s, a wide network of community-based health facilities have provided basic<br />
preventive services—including antenatal care, skilled care during childbirth, and postpartum care—in<br />
domiciliary and clinic settings. (6)<br />
Although Sri Lanka has the lowest maternal mortality ratio in South Asia (as well as the highest<br />
contraceptive prevalence rate), (6) it is continuing to refine its programme to reduce deaths and disability<br />
even further. In provinces where civil unrest continues to be a problem, maternal mortality is twice as<br />
high. It is estimated that approximately 3–4% of deliveries (amounting to a total of 14,000 deliveries<br />
each year) do not receive any skilled assistance. These take place mainly in remote areas (such as the<br />
plantation sector) and areas subjected to civil conflict. In addition, some women still prefer to deliver<br />
* % age 15 and above. Human Development Report 2002, United Nations Development Programme, New York, 2002.<br />
16
Skilled <strong>Care</strong> During Childbirth: Country Profiles Sri Lanka<br />
at home, unassisted by a skilled attendant, for cultural reasons. Research also shows that two thirds<br />
of maternal mortality and morbidity is due to preventable causes and over 70% of infant deaths take<br />
place during the neonatal period. Abortion is illegal in all circumstances except to save the life of the<br />
woman, and unsafe abortion is estimated to cause approximately 7–10% of maternal deaths (see Figure 1).<br />
Laws, Policies, and Related Programmes<br />
Sri Lanka has demonstrated sustained, high-level commitment to safe motherhood during the colonial<br />
and post-independence periods. A number of legal and policy initiatives have helped to create a<br />
supportive framework for reducing maternal mortality and improving access to skilled care during<br />
childbirth, including:<br />
Professionalisation of midwifery: Beginning in the late 1800s, midwives were trained to competency<br />
in clinical skills and officially registered as a cadre of health personnel. These health providers were<br />
deployed to an extensive network of domiciliary and institutional rural health services. Midwifery<br />
became a highly prestigious profession, and midwives were well-respected in the communities they<br />
served. The situation remains the same today.<br />
Vital registration system: As far back as 1897, a system for the registration of births and deaths was<br />
in place, and since 1921 a special section on maternal mortality was included. Not only does the<br />
availability of vital statistics make it possible to create awareness of the extent of the problem and<br />
mobilise action, but it also provides a mechanism to evaluate and improve MCH services.<br />
Integration of family planning services: <strong>Family</strong> planning services have been available as part of MCH<br />
care since 1965. The integration of these services facilitated the wide acceptance of family planning<br />
and fuelled a sharp decline in fertility rates. (4)<br />
Investments in women: As outlined in the previous section, Sri Lanka has made significant investments<br />
in elevating the status of women through policies that promote female education and facilitate<br />
women’s participation in political and social life.<br />
Collaboration: In recent times, the President or Minister of Health appoints a multi-sectoral task force<br />
with representation from relevant ministries, professional bodies, and NGOs for the formulation of<br />
national policies. Sometimes, subcommittees are appointed to ensure that the various sectors (central<br />
and regional) and professional bodies (i.e. College of Obstetricians, midwifery associations, etc.) can<br />
consider details of implementation before the policy is formulated. The 1998 Population and<br />
Reproductive Health Policy, which includes safe motherhood as one of its goals, was developed by a<br />
task force consisting of representatives from the MOH, Ministry of Women’s Affairs, the Women’s<br />
Bureau, academics, and NGOs.<br />
Critical Interventions to Increase Skilled <strong>Care</strong> During Childbirth<br />
Between the 1940s and 1990s, Sri Lanka invested in a series of phased strategies to improve maternal<br />
and child health:<br />
• Improving access to community health services, including antenatal care and skilled care during<br />
childbirth, that are free of charge to the population;<br />
• Expanding specialised obstetric services; and<br />
FIGURE 1 ><br />
CAUSES OF MATERNAL MORTALITY<br />
33%<br />
10%<br />
7%<br />
26%<br />
13%<br />
11%<br />
Haemorrhage<br />
Hypertension<br />
Heart Disease<br />
Abortion<br />
Sepsis<br />
Other causes<br />
NATIONAL SAFE MOTHERHOOD<br />
PROGRAMME<br />
Reducing maternal mortality is a<br />
key goal in broad health policies<br />
and in the MCH Programme.<br />
At the national level, the<br />
<strong>Family</strong> Health Bureau, under<br />
the leadership of a MCH Director,<br />
is the central unit within the<br />
MOH responsible for planning,<br />
implementing, and monitoring<br />
all maternal health<br />
activities. The main priorities for<br />
safe motherhood include:<br />
> Promoting the equitable<br />
distribution of maternal health<br />
services to reduce intra- and<br />
inter-district disparities;<br />
> Improving the quality of antenatal,<br />
intranatal, and postnatal services<br />
through training and supervision;<br />
introduction of the partograph<br />
in certain hospitals; and a checklist<br />
of essential supplies and equipment;<br />
> Upgrading the process of risk<br />
assessment and referral, with<br />
an emphasis on essential and<br />
emergency obstetric care; and<br />
• Developing monitoring and evaluation systems to improve the quality of services. (4) > Systematic review of maternal<br />
deaths.<br />
17
Skilled <strong>Care</strong> During Childbirth: Country Profiles Sri Lanka<br />
THE PUBLIC HEALTH MIDWIFE<br />
The Public Health Midwife (PHM)<br />
is the “front line” health worker<br />
for providing domiciliary MCH and<br />
family planning services in the<br />
community. There are approximately<br />
4,600 PHMs in service through<br />
the health unit system, each serving<br />
a population ranging from<br />
3,000–5,000 people. Through<br />
systematic home visits, these<br />
midwives provide care to pregnant<br />
women, infants, and pre-school<br />
children, including:<br />
> One-on-one health education<br />
and counselling;<br />
> Identification and registration<br />
of all pregnant women;<br />
> Antenatal care;<br />
> Helping mothers plan their place<br />
of delivery;<br />
> Assisting with home deliveries<br />
as necessary;<br />
> Postpartum care and counselling;<br />
> <strong>Family</strong> planning counselling<br />
and provision of contraceptive pills<br />
and condoms to couples of<br />
reproductive age;<br />
> Reproductive health education<br />
for adolescents;<br />
> Encouraging women to seek<br />
screening for reproductive organ<br />
malignancies and schedule regular<br />
check-ups.<br />
Backed up by a well-structured<br />
institutional health system,<br />
PHMs link domiciliary services<br />
with clinic services. Their activities<br />
are supported by a system<br />
of record keeping which enables<br />
them to plan and monitor their<br />
routine activities.<br />
Through encouraging women to<br />
plan their delivery setting,<br />
PHMs are responsible for a high<br />
proportion of women (88%)<br />
delivering in government health<br />
facilities. They also ensure that<br />
about 65% of women receive<br />
postnatal care at least once during<br />
the first ten days after delivery.<br />
Improving Access to Community-Based Health <strong>Care</strong><br />
In 1926, the Government established a “health unit” system to deliver community-based services,<br />
including MCH and family planning, to the vast majority of the population. Providing services at both<br />
the institutional (through health centres located in the community) and domiciliary level, each health<br />
unit serves populations ranging from 40,000–70,000. Health units are staffed by a Medical Officer of<br />
Health (in charge of the unit) and a team consisting of Public Health Nursing Sisters and Public Health<br />
Midwives (PHM) (see sidebar). Each health unit is further subdivided into PHM areas, which constitute<br />
the smallest working unit in the Government’s field health care system.<br />
By 1948, the health unit system had expanded to cover the entire country, and health workers were<br />
trained and deployed to staff health centres and provide services to women at home. By 1975, most<br />
of the population were living within 1.3 km of a health care facility. (4)<br />
Community-based health staff are trained and supervised according to the following:<br />
• The Public Health Midwife receives competency-based training in midwifery for a period of 18<br />
months (12 months at a school of nursing and six months in the community in a field training area).<br />
• The Public Health Nursing Sister receives three years of training at a School of Nursing, followed by<br />
six months of midwifery training, one-year of training in a post-basic nursing school, and six<br />
months of training in the field.<br />
• Medical Officers receive five years of training at the Faculty of Medicine, followed by one-year<br />
internship period (consisting of two appointments of six months each). Since 1915, all medical<br />
students are required to complete midwifery training.<br />
Regular in-service training for field staff is conducted to update knowledge and skills in MCH and<br />
family planning. Staff from each health unit attend monthly conferences where they receive training,<br />
supervision, and skills development.<br />
Supervision: Based on a supportive and non-punitive approach, supervision and monitoring is conducted<br />
at many levels and by several categories of staff. Medical Officers provide overall guidance and<br />
supervision of maternal health services within each health unit. Public Health Midwives are supervised<br />
by Supervising Public Health Midwives, who are in turn supervised by Public Health Nursing Sisters.<br />
The Public Health Midwife maintains records and registers which are reviewed by supervisory staff.<br />
Referral and Transport Systems: A system of ambulance services was instituted in 1926, and rapidly<br />
expanded by 1950 such that emergency transport was available in most health facilities. In cases<br />
where ambulances are unavailable, health staff can make arrangements for paying for other transport,<br />
for which they are reimbursed by the MOH. (4)<br />
Midwives working at the field level can call the Public Health Nursing Sister or the Medical Officer in<br />
their health unit to discuss emergency cases, and can refer women to the nearest clinic or hospital or<br />
directly to a higher-level referral facility.<br />
Community Outreach: The Ministry of Health conducts IEC activities to motivate mothers to attend<br />
health clinics and deliver in hospitals. Materials have been produced by the <strong>Family</strong> Health Bureau and<br />
the Health Education Bureau of the Ministry of Health to educate mothers on the health benefits of<br />
skilled care during childbirth. TV and radio programmes also provide useful information on health,<br />
nutrition, and other health-related topics by specialists in those fields. A highly educated population has<br />
been more receptive to health education activities, which has fostered increased utilisation of services.<br />
18
Skilled <strong>Care</strong> During Childbirth: Country Profiles Sri Lanka<br />
Expanding Access to Specialised Obstetric Services<br />
Sri Lanka’s community-based health system (see previous section) is linked to a three-tiered network<br />
of institutional facilities that provide a range of obstetric services:<br />
• Specialist hospitals (Teaching, Provincial, and Base Hospitals) are tertiary-level facilities that provide<br />
emergency obstetric care and other advanced services. Currently, there is a total of 50 specialist<br />
hospitals (1:400,000 population) staffed by specialist obstetricians.<br />
• Intermediate/Secondary institutions (District Hospitals and Peripheral Units) offer a wide range of<br />
in-patient care in addition to maternal health services. These institutions provide basic essential<br />
obstetric care, and refer women to specialist hospitals (by ambulance) if needed.<br />
• Primary institutions (Rural Hospitals, Cottage Hospitals, and Maternity Homes) provide services for<br />
outpatient care and normal deliveries.<br />
TABLE 1 ><br />
EXPANSION OF MATERNAL AND CHILD HEALTH SERVICES<br />
Maternity<br />
Health<br />
Hospitals* Homes Midwives + Centres<br />
1941 129 12 347 NA<br />
1945 153 34 542 503<br />
1950 263 99 1053 701<br />
1954 270 104 1854 NA<br />
1970 NA 128 2680 1122<br />
1980 357 100 3350 1344<br />
1986 389 88 4652 1778<br />
1989 400 83 5030 1880<br />
1993 410 78 6533 1905<br />
1996 426 60 6745 1950<br />
* Includes Teaching, Provincial, Base, District, Peripheral Units and Rural Hospitals, all of which have<br />
maternity unit facilities for deliveries.<br />
+ Includes both hospital and field midwives.<br />
Since the 1950s, the number of specialised institutions grew steadily (see Table 1), thus providing<br />
women with greater access to a physician (including specialist obstetricians) for maternity care. During<br />
the period between 1964–1983, the number of provincial and base hospitals increased by 30% and the<br />
number of district and peripheral hospitals by 41%. (4)<br />
As Figure 2 illustrates, institutional deliveries have progressively increased during the past four<br />
decades, due to improved access to facilities and regular contact with the Public Health Midwife. Of<br />
the total deliveries that take place in government facilities, nearly 70% occur in specialist hospitals,<br />
where ob/gyns, midwives, or nurses with midwifery skills conduct deliveries; over 20% occur at the<br />
secondary level; and approximately 10% at the primary level. A small percentage (3%) are conducted<br />
by government midwives at home.<br />
Referral and Transport Systems: All major hospitals have ambulance services for emergency transport<br />
to higher-level referral facilities. If ambulances or other hospital vehicles are not available, health staff<br />
can make arrangements to fund alternative transport services, to be paid for by the MOH.<br />
19
Skilled <strong>Care</strong> During Childbirth: Country Profiles Sri Lanka<br />
FIGURE 2 ><br />
PERCENTAGE OF DELIVERIES IN GOVERNMENT HOSPITALS<br />
INVESTIGATING EACH<br />
MATERNAL DEATH<br />
A system to investigate maternal<br />
deaths has been in place<br />
since the late 1950s. Initially,<br />
the Medical Officer of Health<br />
conducted the investigation into<br />
a maternal death using a prescribed<br />
form, and determined<br />
whether any follow-up action<br />
was necessary. In the 1980s, a<br />
formal system of maternal death<br />
reviews was introduced where<br />
a committee—chaired by the<br />
Director General of Health<br />
Services and comprising administrators,<br />
obstetricians, Medical<br />
Officers of Health,<br />
and members of the medical<br />
professional organisations—<br />
reviews the cause and<br />
circumstances surrounding<br />
each maternal death.<br />
Annual and quarterly maternal<br />
death reviews are conducted<br />
at the regional and central levels.<br />
Each death is analysed in-depth<br />
(not to find fault but to<br />
identify corrective action) using<br />
the Three Delays model. The<br />
appropriate measures that<br />
need to be taken to prevent<br />
such deaths are discussed with<br />
programme managers and<br />
service providers. The <strong>Family</strong><br />
Health Bureau acts as the focal<br />
point for this system, and<br />
provides feedback on the issues<br />
discussed and the appropriate<br />
corrective actions needed<br />
for the future. Some examples<br />
of action taken as a result of<br />
maternal death reviews:<br />
establishing 24-hour ambulance<br />
systems, and appointing<br />
two specialist obstetricians to<br />
a referral institution. (4)<br />
PERCENT %<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
1960 1965 1970 1975 1980 1985 1990 1995<br />
YEAR<br />
Monitoring & Evaluation Systems to Improve the Quality of Services<br />
In the period between 1960–1990, the Government placed greater emphasis on improving the quality<br />
of services through developing monitoring and evaluation systems. At the national level, all MCH and<br />
family planning activities were brought under one division, the Bureau of <strong>Family</strong> Health, headed by<br />
a MCH Director. The field reporting system was revamped in an effort to provide regular, systematic<br />
assessments of the programme and to identify areas needing improvement. (4)<br />
The <strong>Family</strong> Health Bureau coordinates routine monitoring and evaluation activities, including:<br />
• Annual maternal death audits at the regional and central levels (see sidebar);<br />
• Quarterly and annual maternal death reviews at the district level.<br />
A set of MCH-Management Information System (MIS) indicators has been developed for each of these<br />
activities, to guide supervision of health workers at the district, province, and national levels.<br />
Feedback and corrective guidance is promptly offered to health workers.<br />
Standards and protocols: Standards and protocols have been developed for most MCH activities. They<br />
guide training and organisation of health services, and are also prepared and circulated periodically<br />
among health workers to update their knowledge. Examples include:<br />
• A comprehensive manual for peripheral-level health workers on MCH and family planning (currently<br />
being revised) is used as a reference by health staff in their daily activities.<br />
• Protocols on management of obstetric emergencies and resuscitation of newborn infants have been<br />
prepared and given to the relevant staff.<br />
• Two new manuals are currently being prepared on Management of Obstetric Emergencies in the<br />
Periphery and Human Resource Development for Health Personnel with assistance from expert agencies<br />
in the field.<br />
• A national system has been developed to review each maternal death (see sidebar).<br />
A recent quality assessment of maternal care has identified some deficiencies in primary-level<br />
institutions, specifically with regard to communication and transport systems. For example, although<br />
most hospitals have ambulances and telephones, smaller institutions still lack such services and face<br />
difficulties in emergency transfer of patients to referral centres. Shortages of certain categories of<br />
health staff exist in particular regions of the country, and have hampered the provision of better<br />
quality care.<br />
20
Skilled <strong>Care</strong> During Childbirth: Country Profiles Sri Lanka<br />
Public Expenditure on Maternal Health<br />
Total government expenditure on health has ranged from 1.47 to 2.12 percent of GDP; of the total<br />
expenditure on health services, a modest percentage is spent on maternal health care (see Table 2).<br />
Prior to the 1990s, health services were funded primarily by the Government; funding to support<br />
health services has subsequently been provided by both government and household expenditures. (4)<br />
In addition to government funding, the safe motherhood programme also receives financial and<br />
technical support from international agencies; the main supporting agencies are UNICEF, WHO,<br />
UNFPA, and the World Bank.<br />
TABLE 2 ><br />
EXPENDITURE ON MATERNAL HEALTH <strong>CARE</strong> IN SRI LANKA:<br />
1950–1999 (4)<br />
Decade<br />
1950s<br />
1960s<br />
1970s<br />
Expenditure on<br />
Maternal Health <strong>Care</strong><br />
0.28<br />
0.30<br />
0.26<br />
Total Government<br />
Health Expenditure<br />
1.95<br />
2.12<br />
1.81<br />
THE KEYS TO SRI LANKA’S<br />
SUCCESS ARE:<br />
> Consistent, long-term<br />
government commitment to<br />
health and development,<br />
with an emphasis on women’s<br />
equality.<br />
1980s<br />
1990s<br />
0.18<br />
0.16<br />
1.47<br />
1.53<br />
> Integration of maternal<br />
health into a broad health<br />
and development policy.<br />
1950–1999<br />
0.23<br />
1.79<br />
> Community-based health<br />
care, free of charge and<br />
widely accessible.<br />
For additional information about Sri Lanka’s<br />
safe motherhood programme contact:<br />
Dr. Anoma Jayathilaka<br />
Ministry of Health<br />
<strong>Family</strong> Health Bureau<br />
No. 231, De Saram Place<br />
Colombo, Sri Lanka<br />
Tel: 94 1 696 508<br />
Fax: 94 1 823 012<br />
E-mail: jayandse@sltnet.lk<br />
> Emphasis on training and<br />
quality of care.<br />
> Routine monitoring<br />
and review, including maternal<br />
death audits.<br />
Sources<br />
1 World Development Indicators 2002. World Bank, Washington DC, 2002.<br />
2 World Contraceptive Use 2001. United Nations Population Division, Department of Social and Economic Affairs. New York, May, 2001.<br />
3 1995; Maternal Mortality in 1995: Estimates developed by WHO, UNICEF, UNFPA. WHO, Geneva, 2001. A maternal mortality study<br />
[Maternal deaths in Sri Lanka: A review of estimates and causes 1996. Authors J. Nalin Rodrigo, Lakshman Fernando, Lakshman Senanayaka,<br />
Prasanna Gunasekara, Soma da Silva. UNICEF-assisted study] conducted in 1996 generated an MMR of 92 deaths per 100,000 live births.<br />
The study found that utilising vital registration systems to measure MMR can seriously undercount maternal deaths.<br />
4 Indra Pathmanathan and Jerker Liljestrand, eds. Investing Effectively in Maternal Health: Malaysia and Sri Lanka. World Bank, Washington DC, 2002. In process.<br />
5 World Bank Case Study on Sri Lanka, Institute on Reproductive Health and Health Reform, 2000.<br />
6 H.R. Seneviratne and L.C. Rajapaksa. “Safe Motherhood in Sri Lanka: A 100-year March.” <strong>International</strong> Journal of Gynaecology and Obstetrics 70 (2000): 113–124.<br />
21
Skilled <strong>Care</strong> During Childbirth: Country Profiles Tunisia<br />
Tunisia<br />
SRI LANKA<br />
MALAYSIA<br />
BOTSWANA<br />
Introduction<br />
Population size (millions) (1) 9.6<br />
Population distribution (%) (1)<br />
Rural 35<br />
Urban 65<br />
Adult illiteracy rate (%) (1)<br />
Male 19<br />
Female 39<br />
GDP (US$ millions) (1) 19,462<br />
% GDP spent on health 2.2<br />
Total fertility rate (1) 2.1<br />
Contraceptive prevalence (%) (2) 60<br />
National maternal<br />
mortality ratio (3) 70<br />
Skilled care during childbirth<br />
requires the presence of a<br />
doctor or midwife, or a nurse<br />
with midwifery skills, who is<br />
trained to manage normal<br />
labour and delivery, recognise<br />
complications, and offer<br />
either emergency treatment<br />
or immediate referral to health<br />
centres for more advanced<br />
care. Skilled care also requires<br />
functioning referral and<br />
transport systems and necessary<br />
drugs, equipment, and supplies.<br />
Tunisia is the smallest of the North African countries, bordering Algeria, Libya, and the Mediterranean Sea.<br />
The health and living standards of all Tunisians have improved substantially in recent decades. For<br />
example, between 1970 and 2000, life expectancy increased from 55.6 to 72 years. In addition, infant<br />
mortality decreased from 135 to 26 deaths per 1,000 live births over the period 1970–2000.<br />
Since its independence in 1956, Tunisia has placed high priority on women’s health and well-being.<br />
Polygamy was abolished, education made mandatory for boys and girls, and in 1959, women were<br />
guaranteed equal rights, making them eligible to vote and hold public office. In the mid-sixties,<br />
Tunisia legalised abortion and began implementing a national family planning programme, which<br />
helped fuel a sharp decline in the total fertility rate from 6.2 in 1970 to 2.1 in 2000.<br />
Maternal health: Tunisia’s maternal mortality ratio has fallen dramatically over the past several<br />
decades—by 80 percent between 1971–1994—to its current level of 70 deaths per 100,000 live births. (2)<br />
Use of maternal health services has also increased impressively (see Figure 1): 92% of women receive<br />
antenatal care, and 82% deliver with a skilled attendant present.<br />
Since the 1960s, Tunisia has made a concerted effort to reduce maternal mortality. Maternal and infant<br />
health centres were established throughout the country, with midwives playing a primary role in<br />
delivering maternal health and family planning services. Several policies supportive of improving<br />
maternal health were instituted during the 1960s and 1970s (see next section). In 1990, a national<br />
maternal health programme was launched.<br />
FIGURE 1 ><br />
USE OF MATERNAL HEALTH AND FAMILY PLANNING<br />
100%<br />
80%<br />
60%<br />
40%<br />
1989<br />
20%<br />
1997<br />
0%<br />
2000<br />
Prenatal <strong>Care</strong><br />
Skilled <strong>Care</strong><br />
During Childbirth<br />
Postpartum <strong>Care</strong><br />
Contraceptive<br />
Prevalence<br />
22
Skilled <strong>Care</strong> During Childbirth: Country Profiles Tunisia<br />
Laws, Policies, and Related Programmes<br />
Between 1950–1970, Tunisia instituted a series of policies to promote women’s equality and status:<br />
• Personal Status Code (1956, 1964) abolished polygamy and repudiation, and raised the legal age of<br />
marriage (17 years for girls; 20 years for boys).*<br />
• Mandatory Schooling (1958) was instituted free of charge for girls and boys from the age of six.<br />
• National Constitution (1959) accorded women equal rights in social, economic, and administrative<br />
affairs; women were granted the right to vote and hold public office.<br />
In addition to establishing a supportive policy framework for improving maternal health and increasing<br />
access to skilled care during childbirth, Tunisia implemented a national family planning programme<br />
(1965) that was integrated into its basic health care system. Midwives became the key cadre of health<br />
personnel that provided family planning and maternal care. Also in 1965, abortion was made legal for<br />
women with 5 or more children during the first trimester; this law was subsequently amended to<br />
permit abortion on request during the first three months. ✝<br />
In 1981, Tunisia developed a primary health care policy that prioritised maternal mortality reduction<br />
as a key objective. In the early 1990s, a number of oversight bodies were established to advise on<br />
women’s issues, including maternal health:<br />
• The Centre of Research, Study, Documentation, and Information on Women;<br />
• The Ministry in Charge of Women and <strong>Family</strong> Issues (responsible to the Prime Minister);<br />
• The National Council on Women;<br />
• The National Perinatal Commission, which was created to advise the Ministry of Health on maternal<br />
health strategies and standards. The Commission includes specialists in the field of perinatology,<br />
directors of pre-service training, heads of ob/gyn services (university and/or regional), national and<br />
regional planners, and midwives, as well as a representative of the National Office of <strong>Family</strong> and<br />
Population (ONFP).<br />
National Programme: While MCH has been identified as a priority issue since Tunisia’s independence,<br />
a national-level safe motherhood programme was not launched until 1990. During the period before<br />
1990, the main strategies to improve maternal health included:<br />
• Development of primary MCH infrastructure and services;<br />
• Implementation of a national family planning programme.<br />
In 1973, a separate division under the Ministry of Health, the Office of <strong>Family</strong> and Population (ONFP)<br />
was created to oversee the maternal health and family planning programmes.<br />
In 1989, Tunisia assessed its existing MCH services, and in 1990 developed a National Perinatal<br />
Programme to improve their quality and coordination. The programme has moved from a focus on<br />
the development and implementation of services based on the risk approach (Phase One) to a more<br />
targeted effort to reduce maternal mortality through specific goals for skilled care during childbirth<br />
(Phase Two).<br />
The 1990 National Perinatal<br />
Programme was designed to<br />
address insufficiencies in<br />
maternal services especially in<br />
rural areas, in particular:<br />
> A lack of human resources,<br />
especially midwives;<br />
> A lack of material resources;<br />
> The weak integration of<br />
MCH/FP activities in primary<br />
health centres (i.e., only<br />
47% offered antenatal care);<br />
> The absence of standards<br />
for care and of a clear definition<br />
of tasks;<br />
> Poor coordination between<br />
peripheral and referral facilities;<br />
and<br />
> Low utilisation of services<br />
by pregnant women: 50% did<br />
not seek antenatal care and<br />
35% of those who did attend<br />
their first visit did not return<br />
for follow-up.<br />
* The minimum age of marriage was raised to 17 for girls and 20 for boys in 1964.<br />
✝ After the first trimester, abortion can be performed on physical and mental health grounds.<br />
23
Skilled <strong>Care</strong> During Childbirth: Country Profiles Tunisia<br />
PHASE TWO:<br />
SETTING NEW GOALS<br />
Statistics on health and use of<br />
services gathered in 1994 were<br />
used to refine the National<br />
Perinatal Programme. Some of<br />
those findings were:<br />
> The national maternal<br />
mortality ratio was 69 deaths<br />
per 100,000 live births, varying<br />
from 54 in the east to 99 in<br />
the west;<br />
> Main causes of death:<br />
haemorrhage (31%), hypertension<br />
(19%), infection (11%),<br />
and cardiovascular disease<br />
(11%);<br />
> Time of death: at delivery<br />
(36%), within 42 days<br />
postpartum (34%), during<br />
pregnancy (22%);<br />
> Place of death: 72% in public<br />
health facilities (39% at the<br />
regional level, 23% in university<br />
facilities and 10% at the<br />
peripheral level), 3% in private<br />
facilities, and 19% at home;<br />
> Indirect causes of death:<br />
cultural inaccessibility (67%),<br />
non-use of antenatal care<br />
(57%), lack of family planning<br />
(38%).<br />
Phase One (1990–1996):<br />
Key strategies:<br />
• Defining service standards for antenatal and postnatal care;<br />
• Upgrading the skills of midwives and public health doctors and improving the quality of care<br />
through refresher training, supportive supervision, and curriculum integration;<br />
• Health education to promote each component of maternal care;<br />
• Research and evaluation (i.e., surveys, health information systems, monitoring and evaluation of<br />
activities);<br />
• Integrating maternal health and family planning promotion into the National Solidarity Funds<br />
26/26, a national initiative which aims to improve living conditions in underprivileged areas<br />
(e.g. drinking water, electricity, housing, literacy and education, health, local employment, and road<br />
infrastructure); and<br />
• Reducing inter- and intra-regional disparities through the Population and <strong>Family</strong> Health Project<br />
(1992–1996), financed by the World Bank to integrate maternal health and family planning services<br />
at peripheral health centres.<br />
Phase Two (1997–2000): To reduce maternal mortality to less than 50 deaths per 100,000 live births<br />
by ensuring that 90% of deliveries occur in attended environments.<br />
Key Strategies: In addition to focusing on priorities established in Phase One, the following strategies<br />
were identified:<br />
• Improving the quality of maternal care and family planning by creating partnerships among different<br />
levels of care;<br />
• Encouraging women to use health facilities; and<br />
• Establishing a system of maternal death audits in public sector hospitals.<br />
Critical Interventions to Increase Skilled <strong>Care</strong> During Childbirth<br />
To increase the coverage of births that occur in a skilled environment, Tunisia implemented a series<br />
of focused interventions in maternal health:<br />
• Developing health services infrastructure;<br />
• Investing in midwifery personnel;<br />
• Community outreach;<br />
• Establishing monitoring and evaluating systems.<br />
Developing Health Services Infrastructure<br />
During the 1960s and 1970s, Tunisia invested in the development of primary MCH centres to provide<br />
family planning services, immunisation, antenatal care, and skilled assistance during childbirth. In<br />
1966, there were 89 such centres; by 1984, the number had increased to 141.<br />
At present, Tunisia is equipped with 152 public maternities, which provide a total of 2,847 ob/gyn<br />
beds. In 1998, there was one ob/gyn bed for every 61 births. The health infrastructure is organised<br />
along three levels:<br />
• The peripheral level: There are 112 peripheral maternities to ensure geographic access to skilled care.<br />
Eighty percent have a laboratory and a radiology service, and all have at least one ambulance.<br />
Almost one-quarter of public sector deliveries take place in these maternities. A public health physician<br />
oversees each peripheral maternity to ensure quality of care.<br />
The Government also runs some 1,957 public health centres (one for every 4,825 inhabitants); 90%<br />
of these centres provide integrated antenatal, postpartum, and family planning services.<br />
24
Skilled <strong>Care</strong> During Childbirth: Country Profiles Tunisia<br />
• The regional level: The 31 regional maternities are the “nerve centre” that links the peripheral and<br />
university facilities. Each has an operating theatre, laboratory, radiology service, and three<br />
ambulances, and each is staffed by a pool of nine midwives and 3–4 ob/gyns. These maternities<br />
account for 43% of all deliveries in public facilities. The rate of transfer to regional obstetrical units<br />
from peripheral maternities is 19%.<br />
The regional maternities were targeted in the second phase of the national programme. Efforts have<br />
been made to improve equipment and competencies, notably by creating partnerships between the<br />
regional and university maternity teams.<br />
• The university level: There are nine referral hospitals, located mainly in the Greater Tunis area,<br />
in three large university cities (Sousse, Monastir), and in the south (Sfax) of the country. Each has<br />
an operating wing and a 24-hour specialised medical service which enables them to deal with<br />
life-threatening complications.<br />
In addition, mobile teams provide family planning and basic maternal health services to semi-urban<br />
and rural areas without health facilities and health personnel. Currently, there are 54 mobile teams and<br />
12 mobile clinics operating in Tunisia. (3)<br />
TABLE 1 ><br />
SELECTED SERVICES PROVIDED BY HEALTH PERSONNEL (1988) (4)<br />
TBA<br />
Midwife Physician (Matrone) Other None<br />
Antenatal care (total) 34% 24% - - 42%<br />
Urban 35% 36% - - 28%<br />
Rural 31% 11% - - 57%<br />
<strong>Care</strong> during delivery (total) 53% 16% 18% 13% -<br />
Urban 61% 26% 8% 4% -<br />
Rural 43% 7% 28% 22% -<br />
Investing in Midwifery Personnel<br />
Investments in midwifery personnel have been a consistent strategy since the 1950s. In 1957, a<br />
ministerial decree established the scope of midwives’ preventive and curative roles in MCH, and in the<br />
1970s, the MOH developed a job description (profil du poste) for the midwife.<br />
Midwives are key providers of family planning services and the main cadre of health providers to<br />
attend deliveries, particularly in rural areas (see Table 1). Midwives are often the first point of contact<br />
for women seeking health services, with physicians providing more specialised services at higher<br />
levels of care.<br />
Training and Supervision Programmes: Training programmes have continuously been revised to<br />
upgrade the skills of midwives and public health doctors:<br />
• A mandatory four-month training course in obstetrics and gynaecology was added as a component<br />
of the two-year internship for general practitioners.<br />
• During the 1970s, pre-service training for midwives was extended to three years, and reformed based<br />
on a modular teaching approach focusing on three main topics: paediatrics, community health,<br />
and contraception.<br />
25
Skilled <strong>Care</strong> During Childbirth: Country Profiles Tunisia<br />
The National Perinatal Programme has established mechanisms for in-service training and supportive<br />
supervision:<br />
• A self-evaluation tool, called an “internship notebook,” was developed for midwifery students<br />
during the internship (practical training) period to monitor their progress in meeting training objectives;<br />
the notebook is reviewed by the internship supervisor, and at the end of the internship period is<br />
handed over to the student who remits it to the training instructor.<br />
• Refresher training was decentralised at the peripheral and regional levels of the health infrastructure.<br />
The frequency and content of refresher training is therefore determined locally, based on needs identified<br />
during supervision, as a result of evaluation findings, and at the request of health practitioners<br />
during meetings.<br />
• Supervisory guidelines were developed by the Ministry of Health as a standard tool for assessing<br />
practioners’ performance. Supervision is decentralised at the peripheral and regional health levels,<br />
and regional and peripheral teams are able to modify/adapt the tool according to local needs.<br />
Standards and protocols: Standards for provision of care are developed in collaboration with<br />
the National Perinatal Commission (as are the objectives and content of in-service training, and the<br />
choice of service strategies). A number of laws have been passed regulating the use of medication and<br />
attendance at delivery, including a decree by the Ministry of Public Health establishing the list of drugs<br />
that midwives may possess and prescribe.<br />
Similarly, “technical cards” on clinical management practices provide an official reference in defining<br />
the scope of intervention by midwives and physicians in the provision of maternal care.<br />
Community Outreach<br />
The National Perinatal Programme conducts education and information activities (using printed<br />
materials and audiovisual media) to highlight the benefits of maternal care for both maternal and child<br />
health. Materials are distributed to women in health facilities or during group education sessions<br />
organised and led by health workers. Raising community awareness about pregnancy complications<br />
and risk factors, and encouraging women to use appropriate services, are of the highest priority,<br />
especially in rural areas.<br />
A 1997 study found that, in spite of all efforts, problems of cultural accessibility persist. For example,<br />
60% of the women who delivered at home came from rural areas. Psychological and emotional<br />
reasons motivated the choice for 40% of them. Lack of knowledge was also a factor; for example, of<br />
the 46% of women who did not seek postpartum care, 73% said they were unaware of the schedule<br />
for postpartum care.<br />
Therefore, in collaboration with the National Solidarity Funds, which aim to improve living conditions<br />
in rural areas, the National Perinatal Programme is promoting integrated family and reproductive<br />
health in more than 800 underprivileged areas. A separate but related strategy is being developed to<br />
improve the atmosphere and acceptability of peripheral maternities to encourage women to use them.<br />
The National Perinatal Programme also works in coordination with the National Health Education<br />
Committee, a consortium of groups that include NGOs (e.g. the National Union of Tunisian Women,<br />
the Tunisian <strong>Family</strong> Planning Association, etc.), the majority political party (the Democratic<br />
Constitutional Assembly) and the Scouts. The Committee organises IEC activities at both the national<br />
and local levels.<br />
26
Skilled <strong>Care</strong> During Childbirth: Country Profiles Tunisia<br />
Establishing Monitoring & Evaluation Systems<br />
Evaluation and research are built into the National Perinatal Programme. A data collection system was<br />
developed and put into place in 1994 in order to provide a statistical record of MCH and family<br />
planning activities, and it has shown steady increases in the use of services.<br />
According to these statistics, the stated national goal for skilled care during childbirth has been met,<br />
though there are still problems in rural areas. In addition, seven national studies have been conducted<br />
to gauge the evolution and impact of the programme. As described in the preceding sections, the<br />
results from these studies have been used to refine the strategies, targets, and goals of the National<br />
Perinatal Programme. In the third phase of the programme, studies point to the need to expand<br />
services to focus on anaemia prevention and additional reproductive health problems (genital cancers,<br />
menopause, etc.), and also to introduce a new medical death certificate and extend maternal death<br />
audits to the private sector and domestic sphere.<br />
Public Expenditure on Maternal Health<br />
Tunisia spends 2.2% of its GDP on health. Government funding covers 91.5% of the national MCH<br />
budget, and the remaining 8.5% is contributed by international agencies. The National Perinatal<br />
Programme benefits from sustained cooperation with UNICEF, the World Bank, and WHO.<br />
For additional information about Tunisia’s<br />
safe motherhood programme contact:<br />
Dr. Mounira Garbouj<br />
Director of Primary Health <strong>Care</strong><br />
Ministry of Health<br />
31 rue Khartoum<br />
Tunis 1002 Tunisia<br />
Tel: 216 1 789 148<br />
Fax: 216 1 789 679<br />
THE KEYS TO TUNISIA’S<br />
SUCCESS ARE:<br />
> Investing in women’s health<br />
and development, with an emphasis<br />
on promoting gender equality.<br />
> Ensuring skilled care for deliveries<br />
at all levels of the health care<br />
infrastructure.<br />
> Retaining midwives as the<br />
central maternal health providers,<br />
and the point of first contact<br />
for pregnant women.<br />
> Continual revision and updating<br />
of the midwifery curriculum.<br />
> Ensuring continuity of care<br />
through each stage of pregnancy,<br />
childbirth, and immediate<br />
postpartum period.<br />
> Multi-sectoral collaboration<br />
to tap the strengths of all potential<br />
partners, both public and private.<br />
> Conducting community outreach<br />
in underprivileged areas<br />
and addressing regional disparities.<br />
> Integrating the quality assurance<br />
process in maternal care.<br />
Sources:<br />
1 World Development Indicators 2002. World Bank, Washington DC, 2002.<br />
2 1995; Maternal Mortality in 1995: Estimates developed by WHO, UNICEF, UNFPA. WHO, Geneva, 2001.<br />
3 M. Boukhris. <strong>Family</strong> Health and Population Policy in Tunisia, 1992.<br />
4 Enquete Demographique et de Sante en Tunisie 1988. Ministère de la Sante Publique, Office National de la Famille<br />
et de la Population, Direction de la Population, Tunis, Tunisie and Institute for Resource Development/Macro Systems, Inc.,<br />
October, 1989.<br />
27
Skilled <strong>Care</strong> During Childbirth: Country Profiles<br />
Acronyms<br />
ANC<br />
CEMD<br />
FWE<br />
FP<br />
GDP<br />
GNP<br />
HIV<br />
IAG<br />
IEC<br />
MCH<br />
MOH<br />
NGO<br />
ONFP<br />
PHM<br />
SADCC<br />
STI<br />
TBA<br />
UNICEF<br />
UNFPA<br />
WHO<br />
Antenatal <strong>Care</strong><br />
Confidential Enquiry of Maternal Deaths<br />
<strong>Family</strong> Welfare Educator<br />
<strong>Family</strong> Planning<br />
Gross Domestic Product<br />
Gross National Product<br />
Human Immunodeficiency Virus<br />
Safe Motherhood Inter-Agency Group<br />
Information, Education, and Communication<br />
Maternal and Child Health<br />
Ministry of Health<br />
Non-governmental Organisation<br />
Office of <strong>Family</strong> and Population (Tunisia)<br />
Public Health Midwife<br />
Southern Africa Development Cooperation<br />
Sexually Transmitted Infection<br />
Traditional Birth Attendant<br />
United Nations Children’s Fund<br />
United Nations Population Fund<br />
World Health Organization
Safe<br />
Motherhood<br />
For further information, please contact the<br />
secretariat of the Safe Motherhood Inter-Agency Group:<br />
<strong>Family</strong> <strong>Care</strong> <strong>International</strong><br />
588 Broadway, Suite 503<br />
New York, NY 10012 USA<br />
1.212.941.5300 Telephone<br />
1.212.941.5563 Facsimile<br />
smi@familycareintl.org E-mail<br />
http://www.safemotherhood.org Web site<br />
United Nations Population Fund<br />
(UNFPA)<br />
World Bank<br />
<strong>International</strong> Planned Parenthood<br />
Federation (IPPF)<br />
World Health Organization<br />
<strong>International</strong> Confederation<br />
of Midwives<br />
Population Council<br />
<strong>International</strong> Federation<br />
of Gynecology and Obstetrics<br />
Safe Motherhood Network of Nepal<br />
Regional Prevention of Maternal<br />
Mortality Network (Africa)<br />
The principles and policies of each agency are governed by the relevant decisions of each agency’s<br />
governing body. Each agency implements the interventions described in this document in accordance<br />
with these principles and policies and within the scope of its mandate.