âMental Status Assessment of Older Adults: The Mini-Cog.â (2007) AJN
âMental Status Assessment of Older Adults: The Mini-Cog.â (2007) AJN
âMental Status Assessment of Older Adults: The Mini-Cog.â (2007) AJN
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
How To<br />
try this<br />
read it watch it try it<br />
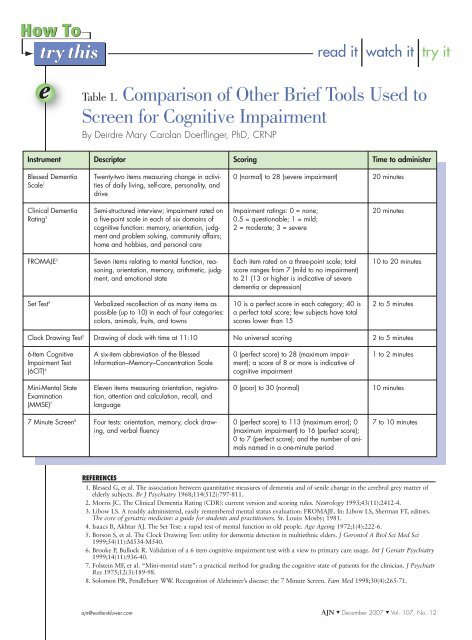
Table 1. Comparison <strong>of</strong> Other Brief Tools Used to<br />
Screen for <strong>Cog</strong>nitive Impairment<br />
By Deirdre Mary Carolan Doerflinger, PhD, CRNP<br />
Instrument Descriptor Scoring Time to administer<br />
Blessed Dementia<br />
Scale 1<br />
Twenty-two items measuring change in activities<br />
<strong>of</strong> daily living, self-care, personality, and<br />
drive<br />
0 (normal) to 28 (severe impairment) 20 minutes<br />
Clinical Dementia<br />
Rating 2<br />
Semi-structured interview; impairment rated on<br />
a five-point scale in each <strong>of</strong> six domains <strong>of</strong><br />
cognitive function: memory, orientation, judgment<br />
and problem solving, community affairs;<br />
home and hobbies, and personal care<br />
Impairment ratings: 0 = none;<br />
0.5 = questionable; 1 = mild;<br />
2 = moderate; 3 = severe<br />
20 minutes<br />
FROMAJE 3<br />
Seven items relating to mental function, reasoning,<br />
orientation, memory, arithmetic, judgment,<br />
and emotional state<br />
Each item rated on a three-point scale; total<br />
score ranges from 7 (mild to no impairment)<br />
to 21 (13 or higher is indicative <strong>of</strong> severe<br />
dementia or depression)<br />
10 to 20 minutes<br />
Set Test 4<br />
Verbalized recollection <strong>of</strong> as many items as<br />
possible (up to 10) in each <strong>of</strong> four categories:<br />
colors, animals, fruits, and towns<br />
10 is a perfect score in each category; 40 is<br />
a perfect total score; few subjects have total<br />
scores lower than 15<br />
2 to 5 minutes<br />
Clock Drawing Test 5 Drawing <strong>of</strong> clock with time at 11:10 No universal scoring 2 to 5 minutes<br />
6-Item <strong>Cog</strong>nitive<br />
Impairment Test<br />
(6CIT) 6<br />
A six-item abbreviation <strong>of</strong> the Blessed<br />
Information–Memory–Concentration Scale<br />
0 (perfect score) to 28 (maximum impairment);<br />
a score <strong>of</strong> 8 or more is indicative <strong>of</strong><br />
cognitive impairment<br />
1 to 2 minutes<br />
<strong>Mini</strong>-Mental State<br />
Examination<br />
(MMSE) 7<br />
Eleven items measuring orientation, registration,<br />
attention and calculation, recall, and<br />
language<br />
0 (poor) to 30 (normal) 10 minutes<br />
7 Minute Screen 8 Four tests: orientation, memory, clock drawing,<br />
and verbal fluency<br />
0 (perfect score) to 113 (maximum error); 0<br />
(maximum impairment) to 16 (perfect score);<br />
0 to 7 (perfect score); and the number <strong>of</strong> animals<br />
named in a one-minute period<br />
7 to 10 minutes<br />
REFERENCES<br />
1. Blessed G, et al. <strong>The</strong> association between quantitative measures <strong>of</strong> dementia and <strong>of</strong> senile change in the cerebral grey matter <strong>of</strong><br />
elderly subjects. Br J Psychiatry 1968;114(512):797-811.<br />
2. Morris JC. <strong>The</strong> Clinical Dementia Rating (CDR): current version and scoring rules. Neurology 1993;43(11):2412-4.<br />
3. Libow LS. A readily administered, easily remembered mental status evaluation: FROMAJE. In: Libow LS, Sherman FT, editors.<br />
<strong>The</strong> core <strong>of</strong> geriatric medicine: a guide for students and practitioners. St. Louis: Mosby; 1981.<br />
4. Isaacs B, Akhtar AJ. <strong>The</strong> Set Test: a rapid test <strong>of</strong> mental function in old people. Age Ageing 1972;1(4):222-6.<br />
5. Borson S, et al. <strong>The</strong> Clock Drawing Test: utility for dementia detection in multiethnic elders. J Gerontol A Biol Sci Med Sci<br />
1999;54(11):M534-M540.<br />
6. Brooke P, Bullock R. Validation <strong>of</strong> a 6 item cognitive impairment test with a view to primary care usage. Int J Geriatr Psychiatry<br />
1999;14(11):936-40.<br />
7. Folstein MF, et al. “<strong>Mini</strong>-mental state”: a practical method for grading the cognitive state <strong>of</strong> patients for the clinician. J Psychiatr<br />
Res 1975;12(3):189-98.<br />
8. Solomon PR, Pendlebury WW. Recognition <strong>of</strong> Alzheimer’s disease: the 7 Minute Screen. Fam Med 1998;30(4):265-71.<br />
ajn@wolterskluwer.com <strong>AJN</strong> ▼ December <strong>2007</strong> ▼ Vol. 107, No. 12
How To<br />
try this<br />
read it watch it try it<br />
One Hospital’s Use <strong>of</strong> the <strong>Mini</strong>-<strong>Cog</strong><br />
Bronson Methodist Hospital, in Kalamazoo,<br />
Michigan, had been using the <strong>Mini</strong>-Mental<br />
State Exam to screen patients for cognitive<br />
impairment. When it became necessary to purchase<br />
this tool, a search for another evidence-based practice<br />
tool was initiated. <strong>The</strong> tool had to be easy to use,<br />
reliable, and available for free. <strong>The</strong> <strong>Mini</strong>-<strong>Cog</strong>, developed<br />
by Soo Borson, MD, and colleagues, was one<br />
such tool and was endorsed by the American<br />
Geriatrics Society. After reviewing the research,<br />
Bronson Methodist Hospital chose the <strong>Mini</strong>-<strong>Cog</strong> for<br />
use in screening older adult patients for dementia.<br />
In addition to the usual assessment <strong>of</strong> orientation<br />
to person, place, and time, nurses can use the <strong>Mini</strong>-<br />
<strong>Cog</strong> to further assess an older adult patient’s mental<br />
status. While the <strong>Mini</strong>-<strong>Cog</strong> is listed on the hospitalists’<br />
admission order form, enabling orders for<br />
screenings to be made on admission <strong>of</strong> new patients,<br />
nurses can also initiate screenings on their own; no<br />
physician’s order is required. Administration <strong>of</strong> the<br />
screening tool can be triggered by patient risk factors<br />
such as age 70 years and older and a negative<br />
score on the Confusion <strong>Assessment</strong> Method tool, or<br />
by disorientation or other patient behaviors such as<br />
• exhibiting signs <strong>of</strong> impaired working memory<br />
(being a “poor historian”).<br />
• deferring to a family member when questions are<br />
addressed to the patient.<br />
• repeatedly and apparently unintentionally failing<br />
to follow instructions.<br />
• having difficulty finding the right words or using<br />
inappropriate or incomprehensible words.<br />
• having difficulty following conversations.<br />
<strong>The</strong> completed <strong>Mini</strong>-<strong>Cog</strong> form is placed in the<br />
progress notes for physician review.<br />
At Bronson Methodist Hospital, if the screening<br />
results indicate possible impairment, nurses take<br />
the following steps:<br />
• “Confusion” is checked as a risk factor on the<br />
hospital’s Fall Risk Pathway Interventions<br />
Addendum form.<br />
• Associated interventions listed on the form are<br />
implemented (for example, using bed and chair<br />
alarms, reorienting patients, and evaluating the<br />
patient’s medications).<br />
• Possible cognitive impairment is documented in<br />
the neurologic assessment section <strong>of</strong> the hospital’s<br />
electronic medical–nursing documentation system.<br />
• Referrals to be handled by case managers following<br />
up with patients and family members are<br />
either conveyed verbally or entered in the electronic<br />
documentation system.<br />
Patients whose <strong>Mini</strong>-<strong>Cog</strong> results are positive<br />
(indicating cognitive impairment) are at increased<br />
risk for delirium, falls, dehydration, inadequate<br />
nutrition, untreated pain, and medication-related<br />
problems. <strong>The</strong> following are some interventions<br />
nurses should consider initiating if a positive screen<br />
is obtained:<br />
• Review medications for adverse effects.<br />
• Assess for acute changes in mental status.<br />
• Assess for depression.<br />
• Assess for fall risk.<br />
• Assess for malnutrition and dehydration.<br />
• Encourage fluid intake unless contraindicated.<br />
• Monitor for adequate nutritional intake.<br />
• Assess for pain.<br />
• Assess for constipation and fecal impaction.<br />
• Assess for pressure ulcer risk.<br />
• Collaborate with interdisciplinary team members.<br />
• Monitor laboratory results.<br />
—Rita LaReau MSN, APRN,BC, GNP, geriatric<br />
clinical nurse specialist, Bronson Methodist Hospital,<br />
Kalamazoo, MI. Contact author: lareaur@<br />
bronsonhg.org<br />
ajn@wolterskluwer.com <strong>AJN</strong> ▼ December <strong>2007</strong> ▼ Vol. 107, No. 12
How To<br />
try this<br />
read it watch it try it<br />
How to Use the Try This Series for Assessing<br />
Delirium and Dementia<br />
Change in Mental <strong>Status</strong> or Other Behaviors That Would Trigger <strong>Assessment</strong><br />
Agitation or lethargy<br />
Fluctuating or altered LOC<br />
Memory impairment or disorganized thinking<br />
Wandering<br />
Uncooperativeness or failure to follow instructions<br />
Change in behavior or function<br />
Inattentiveness<br />
Stupor<br />
Assess for delirium<br />
CAM + facility’s mental status evaluation<br />
Possible delirium<br />
with dementia<br />
Possible delirium<br />
without dementia<br />
Probably<br />
not delirium<br />
Use the<br />
Delirium<br />
Superimposed<br />
on Dementia<br />
Algorithm<br />
Contact primary<br />
care provider<br />
to investigate<br />
the cause <strong>of</strong><br />
behavior change<br />
Treat and manage: use facility protocol<br />
to determine cause, modify risk factors,<br />
protect patient, and perform ongoing<br />
assessments to monitor response.<br />
Assess for dementia using the<br />
<strong>Mini</strong>-<strong>Cog</strong> or Recognition<br />
<strong>of</strong> Dementia in Hospitalized<br />
<strong>Older</strong> <strong>Adults</strong><br />
LOC = level <strong>of</strong> consciousness; CAM = Confusion <strong>Assessment</strong> Method<br />
Note: bold text indicates instrument is part <strong>of</strong> the Try This series.<br />
Probably<br />
not dementia<br />
Possible<br />
dementia<br />
Further assess<br />
patients using<br />
Try This best<br />
practices for<br />
dementia series<br />
ajn@wolterskluwer.com <strong>AJN</strong> ▼ December <strong>2007</strong> ▼ Vol. 107, No. 12