Managing CVA in ED Learning Objectives Is it a stroke? Diagnosis ...
Managing CVA in ED Learning Objectives Is it a stroke? Diagnosis ...
Managing CVA in ED Learning Objectives Is it a stroke? Diagnosis ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
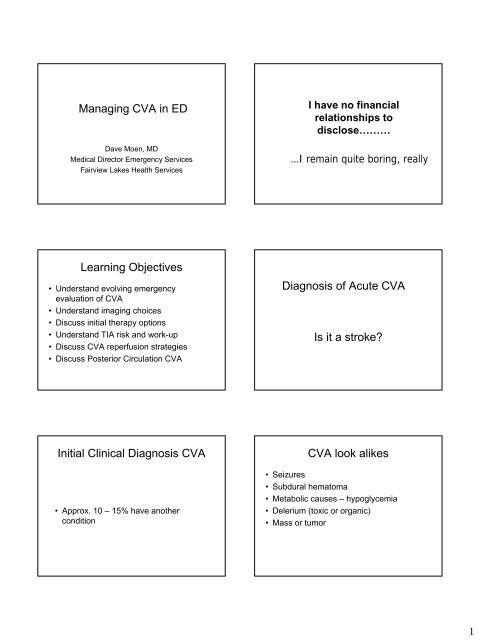
<strong>Manag<strong>in</strong>g</strong> <strong>CVA</strong> <strong>in</strong> <strong>ED</strong><br />
Dave Moen, MD<br />
Medical Director Emergency Services<br />
Fairview Lakes Health Services<br />
I have no f<strong>in</strong>ancial<br />
relationships to<br />
disclose………<br />
…I rema<strong>in</strong> qu<strong>it</strong>e bor<strong>in</strong>g, really<br />
Learn<strong>in</strong>g <strong>Objectives</strong><br />
• Understand evolv<strong>in</strong>g emergency<br />
evaluation of <strong>CVA</strong><br />
• Understand imag<strong>in</strong>g choices<br />
• Discuss <strong>in</strong><strong>it</strong>ial therapy options<br />
• Understand TIA risk and work-up<br />
• Discuss <strong>CVA</strong> reperfusion strategies<br />
• Discuss Posterior Circulation <strong>CVA</strong><br />
<strong>Diagnosis</strong> of Acute <strong>CVA</strong><br />
<strong>Is</strong> <strong>it</strong> a <strong>stroke</strong><br />
In<strong>it</strong>ial Cl<strong>in</strong>ical <strong>Diagnosis</strong> <strong>CVA</strong><br />
• Approx. 10 – 15% have another<br />
cond<strong>it</strong>ion<br />
<strong>CVA</strong> look alikes<br />
• Seizures<br />
• Subdural hematoma<br />
• Metabolic causes – hypoglycemia<br />
• Delerium (toxic or organic)<br />
• Mass or tumor<br />
1
<strong>CVA</strong> look alikes tend to:<br />
In<strong>it</strong>ial work-up<br />
• less prom<strong>in</strong>ent focal f<strong>in</strong>d<strong>in</strong>gs<br />
• Associated mental status changes<br />
(global bra<strong>in</strong> dysfunction)<br />
• History and exam<br />
• Lab work<br />
• Imag<strong>in</strong>g<br />
evolution <strong>in</strong> treatment options demand<br />
attention to pace of workup/treatments<br />
Important Acute <strong>CVA</strong><br />
complications<br />
• Hypoxia/airway<br />
• Hypo/hypertension<br />
• Hypo/hyper glycemia<br />
• Fever associated w<strong>it</strong>h poorer outcomes<br />
• Seizures<br />
Complication Caveats<br />
• Airway <strong>in</strong>terventions if needed<br />
• Oxygen for hypoxia (no help if not hypoxic)<br />
• Treat symptomatic hypoglycemia<br />
• Treat BP >220/120; no lytics till 150)<br />
<strong>CVA</strong> Etiology<br />
Tim<strong>in</strong>g/cl<strong>in</strong>ical course cr<strong>it</strong>ical<br />
15%<br />
15%<br />
hemorrhagic<br />
• When did the <strong>stroke</strong> start<br />
220%<br />
atherothrombotic<br />
cardio-embolic<br />
25%<br />
unknown/rare<br />
• <strong>Is</strong> <strong>it</strong> dense/unchang<strong>in</strong>g cl<strong>in</strong>ically<br />
• <strong>Is</strong> <strong>it</strong> “stutter<strong>in</strong>g” or fluctuat<strong>in</strong>g <strong>in</strong> symptoms<br />
• Level of sever<strong>it</strong>y (NIHSS <strong>stroke</strong> scale)<br />
lacunar<br />
25%<br />
2
What about tim<strong>in</strong>g<br />
• If therapy available under 3 hrs most now<br />
recommend <strong>in</strong>tervention<br />
• If therapy available under 4.5 hrs., some<br />
recommend<br />
• If therapy available under 6 hrs., a few still<br />
recommend<br />
NIHSS <strong>stroke</strong> scale<br />
• Tool for communication/decision-mak<strong>in</strong>g<br />
• Higher scores correlate w<strong>it</strong>h higher<br />
mortal<strong>it</strong>y<br />
• www.<strong>stroke</strong>center.org<br />
<strong>CVA</strong> Patient<br />
Imag<strong>in</strong>g Options<br />
Acute Symptoms<br />
< 5 hrs.<br />
Or “stutter<strong>in</strong>g”<br />
Assess/address<br />
complications<br />
Determ<strong>in</strong>e<br />
NIHSS Score<br />
Subacute<br />
>5hrs<br />
• CT scan<br />
• CT w<strong>it</strong>h contrast (CTA or CTP)<br />
Imag<strong>in</strong>g<br />
•MRI<br />
Acute <strong>CVA</strong> <strong>ED</strong> Goal – Evaluation to CT read = 45 m<strong>in</strong>s.<br />
CT scan (no contrast)<br />
• Rema<strong>in</strong>s as standard of care due to availabil<strong>it</strong>y<br />
and sens<strong>it</strong>iv<strong>it</strong>y exclud<strong>in</strong>g blood<br />
• More sens<strong>it</strong>ive than MRI for detect<strong>in</strong>g blood<br />
• ECASS trial demonstrated that early signs of<br />
major cerebral <strong>in</strong>farction (e.g. sulcal effacement,<br />
mass effect, edema, and loss of the <strong>in</strong>sular<br />
ribbon) are associated w<strong>it</strong>h an <strong>in</strong>creased risk for<br />
<strong>in</strong>tracerebral hemorrhage <strong>in</strong> patients who<br />
receive thrombolytic therapy.<br />
Subtle CT f<strong>in</strong>d<strong>in</strong>gs may <strong>in</strong>crease<br />
risk of bleeds w<strong>it</strong>h lytics<br />
• Sulcal effacement<br />
• Edema<br />
• Mass effect<br />
• Loss of <strong>in</strong>sular ribbon<br />
If you are certa<strong>in</strong> that onset
CT Scan (w<strong>it</strong>h contrast) - CTA<br />
• 98% sens<strong>it</strong>iv<strong>it</strong>y for large vessel occlusion<br />
• Shows thicken<strong>in</strong>g/calcification vessel wall<br />
• Better sens<strong>it</strong>iv<strong>it</strong>y for ischemia<br />
• Adds approx. 10-15 m<strong>in</strong>s. to study<br />
• Includ<strong>in</strong>g neck to aortic arch def<strong>in</strong>es<br />
important vascular anatomy<br />
Diffusion-weighted MRI<br />
• 94% sens<strong>it</strong>iv<strong>it</strong>y/96% specific<strong>it</strong>y <strong>in</strong> early<br />
ischemic <strong>stroke</strong><br />
• More accurate from lacunar/bra<strong>in</strong>stem<br />
<strong>in</strong>farcts<br />
• Changes progress <strong>in</strong> a fashion that allows<br />
tim<strong>in</strong>g of <strong>stroke</strong> onset (wake up <strong>stroke</strong>)<br />
Lim<strong>it</strong>ations MRI<br />
• Take a long time<br />
• Tough to mon<strong>it</strong>or patients<br />
• Not widely available for emergencies<br />
• Not as sens<strong>it</strong>ive for detect<strong>in</strong>g blood<br />
Review Imag<strong>in</strong>g Options<br />
• CT – Still the gold standard; better for<br />
blood<br />
• Consider CTA if acute, large <strong>CVA</strong> and<br />
consider<strong>in</strong>g aggressive <strong>in</strong>tervention and<br />
readily available<br />
• MRI – bra<strong>in</strong>stem <strong>stroke</strong>s and “wake up”<br />
<strong>stroke</strong>s; better posterior circulation<br />
<strong>CVA</strong> Patient<br />
Sub-acute <strong>CVA</strong> management<br />
Acute Symptoms<br />
< 5 hrs.<br />
Or “stutter<strong>in</strong>g”<br />
Assess/address<br />
complications<br />
Determ<strong>in</strong>e<br />
NIHSS Score<br />
Subacute<br />
>5hrs<br />
• Etiology<br />
• Acute treatment<br />
• Hosp<strong>it</strong>alize or not<br />
Imag<strong>in</strong>g<br />
Subacute <strong>CVA</strong><br />
4
Cl<strong>in</strong>ical Caveats<br />
• ASA w<strong>it</strong>h<strong>in</strong> 24 hrs. <strong>CVA</strong> improves<br />
outcomes slightly (1 <strong>in</strong> 100 treated)<br />
• Hepar<strong>in</strong> not useful except <strong>in</strong> known cardioembolic<br />
causes (A.Fib, AMI, PFO)<br />
• Cyto-protective agents under study; some<br />
promise<br />
Hosp<strong>it</strong>alize or not<br />
• Safety at home<br />
• Cardiac mon<strong>it</strong>or<strong>in</strong>g<br />
• Pace of work-up<br />
• Medical Home<br />
• Open discussion of risks/available<br />
<strong>in</strong>terventions<br />
<strong>CVA</strong> Patient<br />
TIA<br />
Acute Symptoms<br />
< 5 hrs.<br />
Or “stutter<strong>in</strong>g”<br />
Imag<strong>in</strong>g<br />
Subacute<br />
>5hrs<br />
• Evolv<strong>in</strong>g def<strong>in</strong><strong>it</strong>ion<br />
• Many now consider TIA as focal neuro<br />
defic<strong>it</strong> last<strong>in</strong>g < 60 m<strong>in</strong>s. (w<strong>it</strong>h no<br />
subsequent imag<strong>in</strong>g f<strong>in</strong>d<strong>in</strong>gs)<br />
No Bleed<br />
No Bleed<br />
Improv<strong>in</strong>g!<br />
Bleed<br />
TIA facts<br />
TIA w<strong>it</strong>h higher <strong>stroke</strong> risk<br />
• 10% TIA patients have <strong>CVA</strong> w<strong>it</strong>h<strong>in</strong> 90<br />
days<br />
• 5% have <strong>CVA</strong> w<strong>it</strong>h<strong>in</strong> 48 hrs.<br />
“TIA should be promptly evaluated<br />
because delay<strong>in</strong>g diagnosis risks<br />
preventable <strong>stroke</strong>.” AHA Council on<br />
Stroke Update<br />
• Age > 60<br />
• Sign or symptom of weakness<br />
• Speech disturbance<br />
• diabetes<br />
• Symptoms last<strong>in</strong>g > 10 m<strong>in</strong>s.<br />
5
Relative 90 day risk of <strong>CVA</strong><br />
• One risk 3%<br />
• Two risks 7% >1700<br />
patients<br />
• Three risks 11%<br />
• Four risks 15%<br />
• Five risks 34%<br />
Relative 90 day Risk of Adverse<br />
Event<br />
• >25% have an adverse event<br />
12.7% recurrent TIA<br />
10% <strong>CVA</strong><br />
2.6% cardiac event<br />
2.6% deaths<br />
Johnson, C. et al; Short term prognosis after emergency department diagnosisof TIA; JAMA 2000 Vol 284<br />
No. 22<br />
Johnson, C. et al; Short term prognosis after emergency department diagnosisof TIA; JAMA 2000 Vol 284 No.<br />
22<br />
TIA work-up<br />
• Carotid evaluation (MRI/MRA, CTA, U/S)<br />
• ECHO bubble study (r/o PDA)<br />
• Lab work<br />
• EKG, telemetry to r/o paroxysmal A.fib.<br />
Reduc<strong>in</strong>g <strong>CVA</strong> risk w<strong>it</strong>h TIA<br />
patients<br />
• ASA and other anti-platelet meds<br />
• HTN management<br />
• Diabetes management<br />
• Endarterectomy or stent<strong>in</strong>g for carotid<br />
disease<br />
• Anticoagulation w<strong>it</strong>h atrial Fib.<br />
• Stat<strong>in</strong>s<br />
Cl<strong>in</strong>ical approach to TIA<br />
<strong>CVA</strong> Patient<br />
• Appropriate discussion/disclosure of risk<br />
• Timely work-up to rule out treatable<br />
causes<br />
• ASA or other antiplatelet meds<br />
• Cl<strong>in</strong>ical home to address risk factor<br />
management<br />
Acute Symptoms<br />
< 5 hrs.<br />
Or “stutter<strong>in</strong>g”<br />
No Bleed<br />
Imag<strong>in</strong>g<br />
Subacute<br />
>5hrs<br />
No Bleed<br />
Persistent Neuro<br />
Defic<strong>it</strong><br />
Bleed<br />
6
Aggressive Interventional<br />
Options<br />
• Systemic rTPA<br />
• Neuro cath w<strong>it</strong>h targeted lytics<br />
• Neuro cath w<strong>it</strong>h lytics/embolectomy<br />
Systemic rTPA<br />
• Still controversial after all these years!<br />
• Generally accepted caveats:<br />
-no mortal<strong>it</strong>y impact (save some, lose some)<br />
-improves neuro outcome <strong>in</strong> 12 patients/100<br />
treat.<br />
-MUST do <strong>it</strong> right to receive benef<strong>it</strong>!<br />
(overdos<strong>in</strong>g is most common error)<br />
-NIHSS >22; severe <strong>stroke</strong>s = no benef<strong>it</strong><br />
-Cost/benef<strong>it</strong> is pos<strong>it</strong>ive<br />
Systemic rTPA<br />
Neuro-<strong>in</strong>terventional<br />
approaches<br />
• Earlier <strong>in</strong> course is better<br />
• Exped<strong>it</strong>ious process and decisionmak<strong>in</strong>g<br />
will change outcomes (m<strong>in</strong>utes<br />
matter)<br />
• Commun<strong>it</strong>y <strong>in</strong>st<strong>it</strong>utions can do this well<br />
• Appropriate disclosure of risk/benef<strong>it</strong><br />
-12 improved outcomes/100 treated<br />
-1 <strong>in</strong> 15 have severe bleed<br />
• Targeted approach – fewer<br />
complications<br />
• Can cause delays <strong>in</strong> treatment<br />
• Lim<strong>it</strong>ed resources<br />
• Lim<strong>it</strong>ed efficacy data<br />
S<strong>in</strong>gle Center Experience W<strong>it</strong>h IA Intervention <strong>in</strong><br />
177 Consecutive Patients W<strong>it</strong>h Angiographically<br />
Confirmed Large Vessel <strong>Is</strong>chemic Stroke from<br />
2003–2007<br />
Michael T. Madison M.D., James K. Goddard, III. M.D.,<br />
Jeffrey P. Lassig M.D., Mark E. Myers M.D.<br />
Background<br />
• IA thrombolytics and mechanical <strong>in</strong>tervention have been<br />
shown to recanalize acute ischemic <strong>stroke</strong>s at high rates<br />
(PROACT II = 66%; Multi MERCI = 68%)<br />
• Less data has been presented on use of these<br />
<strong>in</strong>terventions <strong>in</strong> commun<strong>it</strong>y based sett<strong>in</strong>gs<br />
• Goal: to see if results from our group of 4 Neuro-<br />
Interventionalists cover<strong>in</strong>g acute <strong>stroke</strong> at 5 hosp<strong>it</strong>als <strong>in</strong><br />
the M<strong>in</strong>neapolis/St. Paul area were consistent w<strong>it</strong>h<br />
outcomes presented <strong>in</strong> other trials<br />
St. Paul Radiology, St. Paul, MN<br />
7
Protocol<br />
• Neurologic exam<strong>in</strong>ation suggest<strong>in</strong>g a major <strong>stroke</strong><br />
syndrome (NIHSS >8) of recent onset<br />
– 6 hours or less for thrombolysis<br />
– 8 hours or less for mechanical thrombectomy<br />
• Non-contrast head CT (patients w<strong>it</strong>h def<strong>in</strong>ed<br />
<strong>in</strong>farcts, hemorrhage or tumors are excluded)<br />
– CTA Circle of Willis, CT perfusion, MRI<br />
• Discuss and formulate treatment plan w<strong>it</strong>h Stroke<br />
Neurologist<br />
• Cerebral angiography to confirm large vessel<br />
occlusion<br />
Protocol<br />
• Direct <strong>in</strong>tra-arterial thrombolysis w<strong>it</strong>h tPA<br />
dose < 40 mg) and Integril<strong>in</strong> ®<br />
(eptifibatide) (s<strong>in</strong>gle weight-based bolus)<br />
to treat vascular occlusions correlat<strong>in</strong>g<br />
w<strong>it</strong>h cl<strong>in</strong>ical <strong>stroke</strong> syndrome<br />
• Concentric Merci ® retriever device<br />
• Penumbra ® mechanical thrombectomy<br />
devices (FDA trial)<br />
Stroke Interventions by Year<br />
Demographics<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
54<br />
43 43<br />
17<br />
20<br />
2003 2004 2005 2006 2007<br />
• Mean basel<strong>in</strong>e NIHSS: 14.4 (Range 8–29)<br />
• Mean time from symptom onset to <strong>in</strong>tervention:<br />
4 hrs 11 m<strong>in</strong>utes (Range 1–7.5 hrs)<br />
• Etiology of Strokes:<br />
– Atrial Fibrillation 43%<br />
– Unknown 20%<br />
– Carotid Atherosclerosis 11%<br />
– PFO 9%<br />
– Intracranial Stenosis 5%<br />
– Other (mural thrombus, 9%<br />
atrial myxoma, hypercoagulable)<br />
IC<br />
Stenosis<br />
5% Other<br />
9%<br />
PFO<br />
9%<br />
Carotid<br />
Athero<br />
11%<br />
Unknown<br />
20%<br />
Afib<br />
43%<br />
Demographics: Occlusion<br />
Locations<br />
Procedural Data & Outcomes<br />
• ICA 18%<br />
• MCA 71%<br />
• Vertebrobasilar 7%<br />
• PCA 2%<br />
• ACA 2%<br />
PCA<br />
2%<br />
VB<br />
7%<br />
MCA<br />
71%<br />
ACA<br />
2%<br />
ICA<br />
18%<br />
• IA thrombolytics used <strong>in</strong> 87% (154/177)<br />
– Mean dose of IA tPA: 24.6 mg (Range: 9-42 mg)<br />
• Mean dose of IA eptifibatide (Integril<strong>in</strong> ® ): 4.6 mg (Range:<br />
0-9.5 mg)<br />
• Merci ® Retriever used <strong>in</strong> 40% (71/177)<br />
– Immediate post-retriever recanalization was 52%<br />
• F<strong>in</strong>al angiographic recanalization for the overall cohort<br />
was 81%<br />
– TIMI III Flow 59%<br />
– TIMI II Flow 22%<br />
8
Cl<strong>in</strong>ical Outcomes<br />
Cl<strong>in</strong>ical Outcomes (Cont.)<br />
• Average NIHSS (24-48 hrs) post-treatment was 7.4<br />
(Range 0-30)<br />
• Pos<strong>it</strong>ive cl<strong>in</strong>ical outcomes (NIHSS
<strong>ED</strong> evaluation<br />
• In<strong>it</strong>ial same as other <strong>CVA</strong><br />
• Anatomy best def<strong>in</strong>ed w<strong>it</strong>h MRI/MRA or<br />
CTA<br />
• Treatment (same)<br />
In patients dizz<strong>in</strong>ess or vertigo or<br />
HA w<strong>it</strong>h accompany<strong>in</strong>g neuro<br />
symptoms – posterior circulation<br />
vascular disease must be ruled<br />
out<br />
Summary<br />
• Evolv<strong>in</strong>g treatment options make pace of <strong>CVA</strong><br />
workup and treatment important<br />
• CT still gold standard but CTA and MRA add<br />
important vessel anatomy def<strong>in</strong><strong>it</strong>ion<br />
• TIA’s are high risk events; understand<strong>in</strong>g and<br />
communication are cr<strong>it</strong>ical<br />
• Reperfusion strategies improve outcomes <strong>in</strong><br />
selected patients<br />
• Posterior <strong>CVA</strong>’s are difficult to diagnose and<br />
must be thought of and looked for<br />
References<br />
1. Stroke. 2003;34:1056-1083<br />
doi: 10.1161/01.STR.0000064841.47697.22<br />
2. http://www.aafp.org/afp/990515ap/2828.html<br />
3. Stroke. 1999;30:1440-1443<br />
4. http://www.americanheart.org/presenter.jhtmlidentifier=4724<br />
5. ACEP EMCREG Monograph: Advanc<strong>in</strong>g the Standard of Care<br />
Cardiovascular, Neurovascular, and Infectious Emergencies; Oct 2007<br />
10