pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
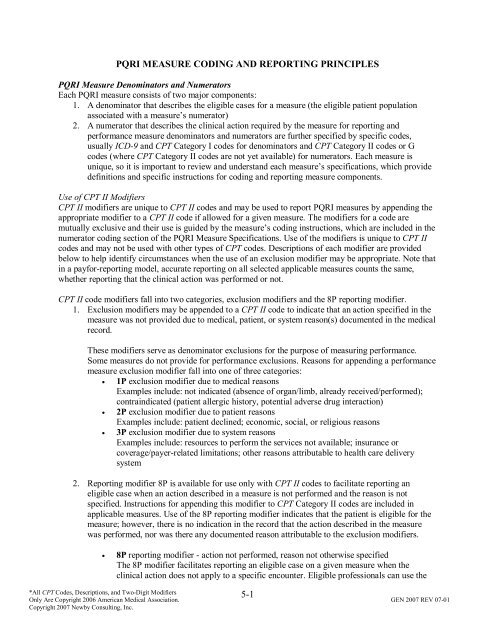
PQRI MEASURE CODING AND REPORTING PRINCIPLES<br />
PQRI Measure Denominators <strong>and</strong> Numerators<br />
Each PQRI <strong>measure</strong> consists <strong>of</strong> two major components:<br />
1. A denominator that describes the eligible cases for a <strong>measure</strong> (the eligible patient population<br />
associated with a <strong>measure</strong>’s numerator)<br />
2. A numerator that describes the clinical action required by the <strong>measure</strong> for <strong>reporting</strong> <strong>and</strong><br />
performance <strong>measure</strong> denominators <strong>and</strong> numerators are further specified by specific codes,<br />
usually ICD-9 <strong>and</strong> CPT Category I codes for denominators <strong>and</strong> CPT Category II codes or G<br />
codes (where CPT Category II codes are not yet available) for numerators. Each <strong>measure</strong> is<br />
unique, so it is important to review <strong>and</strong> underst<strong>and</strong> each <strong>measure</strong>’s specifications, which provide<br />
definitions <strong>and</strong> specific instructions for <strong>coding</strong> <strong>and</strong> <strong>reporting</strong> <strong>measure</strong> components.<br />
Use <strong>of</strong> CPT II Modifiers<br />
CPT II modifiers are unique to CPT II codes <strong>and</strong> may be used to report PQRI <strong>measure</strong>s by appending the<br />
appropriate modifier to a CPT II code if allowed for a given <strong>measure</strong>. The modifiers for a code are<br />
mutually exclusive <strong>and</strong> their use is guided by the <strong>measure</strong>’s <strong>coding</strong> instructions, which are included in the<br />
numerator <strong>coding</strong> section <strong>of</strong> the PQRI Measure Specifications. Use <strong>of</strong> the modifiers is unique to CPT II<br />
codes <strong>and</strong> may not be used with other types <strong>of</strong> CPT codes. Descriptions <strong>of</strong> each modifier are provided<br />
below to help identify circumstances when the use <strong>of</strong> an exclusion modifier may be appropriate. Note that<br />
in a payfor-<strong>reporting</strong> model, accurate <strong>reporting</strong> on all selected applicable <strong>measure</strong>s counts the same,<br />
whether <strong>reporting</strong> that the clinical action was performed or not.<br />
CPT II code modifiers fall into two categories, exclusion modifiers <strong>and</strong> the 8P <strong>reporting</strong> modifier.<br />
1. Exclusion modifiers may be appended to a CPT II code to indicate that an action specified in the<br />
<strong>measure</strong> was not provided due to medical, patient, or system reason(s) documented in the medical<br />
record.<br />
These modifiers serve as denominator exclusions for the purpose <strong>of</strong> measuring performance.<br />
Some <strong>measure</strong>s do not provide for performance exclusions. Reasons for appending a performance<br />
<strong>measure</strong> exclusion modifier fall into one <strong>of</strong> three categories:<br />
• 1P exclusion modifier due to medical reasons<br />
Examples include: not indicated (absence <strong>of</strong> organ/limb, already received/performed);<br />
contraindicated (patient allergic history, potential adverse drug interaction)<br />
• 2P exclusion modifier due to patient reasons<br />
Examples include: patient declined; economic, social, or religious reasons<br />
• 3P exclusion modifier due to system reasons<br />
Examples include: resources to perform the services not available; insurance or<br />
coverage/payer-related limitations; other reasons attributable to health care delivery<br />
system<br />
2. Reporting modifier 8P is available for use only with CPT II codes to facilitate <strong>reporting</strong> an<br />
eligible case when an action described in a <strong>measure</strong> is not performed <strong>and</strong> the reason is not<br />
specified. Instructions for appending this modifier to CPT Category II codes are included in<br />
applicable <strong>measure</strong>s. Use <strong>of</strong> the 8P <strong>reporting</strong> modifier indicates that the patient is eligible for the<br />
<strong>measure</strong>; however, there is no indication in the record that the action described in the <strong>measure</strong><br />
was performed, nor was there any documented reason attributable to the exclusion modifiers.<br />
• 8P <strong>reporting</strong> modifier - action not performed, reason not otherwise specified<br />
The 8P modifier facilitates <strong>reporting</strong> an eligible case on a given <strong>measure</strong> when the<br />
clinical action does not apply to a specific encounter. Eligible pr<strong>of</strong>essionals can use the<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.<br />
5-1
8P modifier to receive credit for successful <strong>reporting</strong> but will not receive credit for<br />
performance.<br />
For example, a patient with diabetes may present to a clinician for reasons that do not involve<br />
glycemic control, hypertension, or cholesterol management. However, the claim for services for<br />
that encounter will contain ICD-9 <strong>and</strong> CPT codes that will draw the patient into the diabetes<br />
<strong>measure</strong>s’ denominator during analysis. The 8P modifier serves to include the patient in the<br />
numerator when <strong>reporting</strong> rates are calculated for PQRI.<br />
Reporting Frequency <strong>and</strong> Performance Timeframes<br />
Each <strong>measure</strong> includes a <strong>reporting</strong> frequency requirement for each denominator-eligible patient seen<br />
during the <strong>reporting</strong> period. The <strong>reporting</strong> frequency is described in the instructions:<br />
• Report one-time only<br />
• Report once for each procedure performed<br />
• Report once for each acute episode<br />
A <strong>measure</strong>’s performance timeframe is defined in the <strong>measure</strong>’s description <strong>and</strong> is distinct from the<br />
<strong>reporting</strong> frequency requirement. The performance timeframe, unique to each <strong>measure</strong>, delineates the<br />
timeframe in which the clinical action described in the numerator may be accomplished.<br />
Performance timeframes may be stated as “within 12 months,” or “most recent.” This means that:<br />
1. The clinical action in the numerator need be performed only once during a 12-month period for<br />
each patient seen during the <strong>reporting</strong> period<br />
2. The quality code need be reported only one time for each patient by each eligible pr<strong>of</strong>essional<br />
caring for the patient who has chosen to report that <strong>measure</strong> during the <strong>reporting</strong> period<br />
If the <strong>measure</strong> calls for a clinical test result, then the most recent test result only needs to be obtained,<br />
assessed, <strong>and</strong> reported one time per <strong>reporting</strong> period. A test does not need to have been performed within<br />
the <strong>reporting</strong> period, nor does it need to have been performed by the same eligible pr<strong>of</strong>essional.<br />
Performance timeframes may also be tied to a specific clinical event that requires <strong>reporting</strong> each time the<br />
event occurs within the <strong>reporting</strong> period. The following are examples <strong>of</strong> <strong>measure</strong>s reported each time the<br />
clinical action described by the <strong>measure</strong> numerator is taken:<br />
• Procedure-related <strong>measure</strong>s require <strong>reporting</strong> each time the procedure is performed <strong>and</strong> have<br />
distinct performance timeframes tied to them. The date <strong>of</strong> service is the date that is used to report<br />
the <strong>measure</strong>. Examples are perioperative care or imaging <strong>measure</strong>s.<br />
• Chronic care <strong>measure</strong>s, such as those that call for prescribing a medication, require the eligible<br />
pr<strong>of</strong>essional to verify whether the medication is current <strong>and</strong> being taken by the patient. A new<br />
prescription is not required to meet the <strong>measure</strong> requirement unless it is clinically indicated.<br />
• Acute care <strong>measure</strong>s are tied to specific episodes <strong>of</strong> acute care <strong>and</strong> require <strong>reporting</strong> each time an<br />
acute event occurs. Examples are <strong>measure</strong>s related to hospitalizations, fractures <strong>and</strong> osteoporosis<br />
management, or stroke <strong>measure</strong>s.<br />
Claims-Based Reporting Principles<br />
The following <strong>principles</strong> apply to the <strong>reporting</strong> <strong>of</strong> quality-data codes for PQRI <strong>measure</strong><br />
• The CPT Category II code, which supplies the numerator, must be reported on the same claim<br />
form as the payment codes, usually ICD-9 <strong>and</strong> CPT Category I codes, which supply the<br />
denominator.<br />
• Quality-data codes must be submitted with a line item charge <strong>of</strong> zero dollars ($0.00) at the time<br />
the associated covered service is performed.<br />
! The submitted charge field cannot be blank.<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.<br />
5-2
! The line item charge should be $0.00.<br />
! If a system does not allow a $0.00 line item charge, use a small amount such as $0.01<br />
! Entire claims with a zero charge will be rejected. (Total charge for the claim cannot be<br />
$0.00)<br />
! Quality data code line items will be denied for payment, but are then passed through the<br />
claims processing system for PQRI analysis.<br />
• Multiple eligible pr<strong>of</strong>essionals’ quality-data codes can be reported on the same claim.<br />
• Multiple CPT Category II codes for multiple <strong>measure</strong>s that are applicable to a patient visit can be<br />
reported on the same claim, as long as the corresponding denominator codes are also line items<br />
on that claim.<br />
• The individual NPI <strong>of</strong> the participating eligible pr<strong>of</strong>essional(s) must be properly used on the<br />
claim.<br />
Timeliness <strong>of</strong> Quality Data Submission<br />
Claims processed by the Carrier/MAC must reach the national Medicare claims system data warehouse<br />
(National Claims History file) by February 29, 2008 to be included in the analysis. Claims for services<br />
furnished toward the end <strong>of</strong> the <strong>reporting</strong> period should be filed promptly. Claims that are resubmitted<br />
only to add quality-data codes will not be included in the analysis.<br />
Successful Reporting<br />
The 2007 PQRI incentive payment is an all-or-nothing bonus (subject to cap) based on successful<br />
<strong>reporting</strong>.<br />
Eligible pr<strong>of</strong>essionals need not enroll or file an intent to participate for the PQRI. Eligible pr<strong>of</strong>essionals<br />
can participate by <strong>reporting</strong> the appropriate quality <strong>measure</strong> data on claims submitted to their Medicare<br />
claims processing contractor.<br />
In order to satisfactorily meet the requirements <strong>of</strong> the program <strong>and</strong> receive the bonus payment, certain<br />
<strong>reporting</strong> thresholds must be met. When four or more <strong>measure</strong>s are applicable to the services provided by<br />
an eligible pr<strong>of</strong>essional, the 80% threshold must be met on at least three <strong>of</strong> the <strong>measure</strong>s reported.<br />
Good news for those physicians practicing in a group practice, not all physicians in the group must<br />
participate in PQRI to be eligible for the bonus payment. Individual analysis will be done using the<br />
individual physician’s national provider identifier (NPI) to determine satisfactory <strong>reporting</strong> <strong>and</strong> the bonus<br />
payment calculation. Thus, physicians must bill with an NPI to participate in PQRI. The potential 1.5<br />
percent incentive payment will be paid in mid-2008 as a lump-sum bonus payment made to the practice at<br />
the Taxpayer Identification Number (TIN) level. According to the CMS website, the NPI is the only<br />
unique provider enumerator that can be used by the CMS PQRI analysis contractor to properly identify<br />
eligible physicians at the individual-physician level.<br />
The performing pr<strong>of</strong>essional’s NPI must be used for the quality-data codes <strong>and</strong> related services. For<br />
claims submitted via the ASC X12N 837 pr<strong>of</strong>essional health care claim transaction, the group practice<br />
NPI is placed in the provider billing segment, loop 2010AA, <strong>and</strong> the performing pr<strong>of</strong>essional’s NPI is<br />
placed in loop 2420A. For claims submitted via the CMS 1500 form, the performing pr<strong>of</strong>essional’s NPI is<br />
placed on the individual line item. Placing the performing eligible pr<strong>of</strong>essional’s NPI on the individual<br />
line item will allow the analysis <strong>of</strong> successful <strong>reporting</strong> <strong>and</strong> the bonus payment calculation to be<br />
performed at the individual level, though payment will be made at the TIN level.<br />
Bonus Payment<br />
Participating eligible pr<strong>of</strong>essionals who successfully report may earn a 1.5% bonus, subject to cap. The<br />
potential 1.5% bonus will be based on allowed charges for covered pr<strong>of</strong>essional services:<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.<br />
5-3
1. Furnished during the <strong>reporting</strong> period <strong>of</strong> July 1 through December 31, 2007,<br />
2. Received into the CMS National Claims History (NCH) file by February 29, 2008 (Joy’s<br />
comment: claim should be received by the Carrier no later than February 28, 2008), <strong>and</strong><br />
3. Paid under the Medicare Physician Fee Schedule (Joy’s comment: HCPCS “J” codes for drugs<br />
are not subject to the bonus).<br />
Because claims processing times may vary by time <strong>of</strong> the year <strong>and</strong> Medicare Carrier/Medicare<br />
Administrative Contractor (MAC), physicians should submit claims from the end <strong>of</strong> 2007 promptly, so<br />
that those claims will reach the NCH file by February 29, 2008. Bonuses will be paid as a lump sum in<br />
mid-2008. There is no beneficiary copayment or notice to the beneficiary regarding the bonus payments.<br />
A payment cap that would reduce the potential bonus below 1.5% <strong>of</strong> allowed charges may apply in<br />
situations where a physician reports relatively few instances <strong>of</strong> quality <strong>measure</strong> data. The physician’s cap<br />
will be calculated by multiplying: (1) the physician’s total instances <strong>of</strong> <strong>reporting</strong> quality data for all<br />
<strong>measure</strong>s (not limited only to <strong>measure</strong>s meeting the 80% threshold), by (2) a constant <strong>of</strong> 300%, <strong>and</strong> by (3)<br />
the national average per <strong>measure</strong> payment amount.<br />
The national average per <strong>measure</strong> payment amount is one value for all <strong>measure</strong>s <strong>and</strong> all participants that<br />
is calculated by dividing: (1) the total amount <strong>of</strong> allowed charges under the Physician Fee Schedule for all<br />
covered pr<strong>of</strong>essional services furnished during the <strong>reporting</strong> period on claims for which quality <strong>measure</strong>s<br />
were reported by all participants in the program by (2) the total number <strong>of</strong> instances for which data were<br />
reported by all participants in the program for all <strong>measure</strong>s during the <strong>reporting</strong> period. (Note that the<br />
national average per <strong>measure</strong> payment amount calculation only takes into account the charges on claims<br />
for which quality <strong>measure</strong>s were reported, whereas the individual bonus calculation takes into account<br />
charges for all services furnished during the <strong>reporting</strong> period.) While the purpose <strong>of</strong> the cap is clear, it is<br />
not possible to determine the impact <strong>of</strong> the cap until the national average per <strong>measure</strong> payment amount<br />
can be calculated after the end <strong>of</strong> the <strong>reporting</strong> period.<br />
CMS recommends that physicians report on every quality <strong>measure</strong> that is applicable to their patient<br />
populations to: (1) increase the likelihood that they will reach the 80% satisfactorily <strong>reporting</strong><br />
requirement for the requisite number <strong>of</strong> <strong>measure</strong>s <strong>and</strong> (2) increase the likelihood that they will not be<br />
affected by the bonus payment cap.<br />
2007 Physician Quality Reporting Initiative Measures - Not All Inclusive<br />
1) Hemoglobin A1c Poor Control in Type 1 or 2 Diabetes Mellitus - Percentage <strong>of</strong> patients aged 18-75<br />
years with diabetes (type 1 or type 2) who had most recent hemoglobin A1c greater than 9.0% - This <strong>measure</strong> is to<br />
be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period for patients seen during the <strong>reporting</strong> period. The performance<br />
period for this <strong>measure</strong> is 12 months. It is anticipated that clinicians who provide services for the primary<br />
management <strong>of</strong> diabetes mellitus will submit this <strong>measure</strong><br />
ICD-9: 250.00-250.93, 648.00-648.04 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit) (<strong>of</strong>fice/outpatient visit); 99341-99350 (home visit);<br />
99304-99310 (nursing facility); 99324-99337 (domiciliary); 97802-97804 <strong>and</strong> G0270-G0271 (nutrition therapy)<br />
_____<br />
_____<br />
_____<br />
_____<br />
Most recent hemoglobin A1c level > 9.0% (3046F)<br />
Most recent hemoglobin A1c level < 7.0% (3044F)<br />
Most recent hemoglobin A1c level 7.0% to 9.0% (3045F)<br />
Hemoglobin A1c not performed during last 12 months reason not specified (3046F-8P)<br />
2) Low Density Lipoprotein Control in Type 1 or 2 Diabetes Mellitus - Percentage <strong>of</strong> patients aged 18-75<br />
years with diabetes (type 1 or type 2) who had most recent LDL-C level in control (less than 100 mg/dl) - This<br />
<strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period for patients seen during the <strong>reporting</strong> period. The<br />
performance period for this <strong>measure</strong> is 12 months. It is anticipated that clinicians who provide services for the<br />
primary management <strong>of</strong> diabetes mellitus will submit this <strong>measure</strong>.<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.<br />
5-4
ICD-9: 250.00-250.93, 648.00-648.04 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit) (<strong>of</strong>fice/outpatient visit); 99341-99350 (home visit);<br />
99304-99310 (nursing facility); 99324-99337 (domiciliary); 97802-97804 <strong>and</strong> G0270-G0271 (nutrition therapy)<br />
_____<br />
_____<br />
_____<br />
_____<br />
Most recent LDL-C < 100 mg/dL (3048F)<br />
Most recent LDL-C 100-129 mg/dL (3049F)<br />
Most recent LDL-C ≥ 130 mg/dL (3050F)<br />
LDL-C level not performed during last 12 months reason not specified (3048F-8P)<br />
3) High Blood Pressure Control in Type 1 or 2 Diabetes Mellitus - Percentage <strong>of</strong> patients aged 18-75<br />
years with diabetes (type 1 or type 2) who had most recent blood pressure in control (less than 140/80 mm Hg) -<br />
This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period for patients seen during the <strong>reporting</strong> period.<br />
The performance period for this <strong>measure</strong> is 12 months. It is anticipated that clinicians who provide services for the<br />
primary management <strong>of</strong> diabetes mellitus will submit this <strong>measure</strong>.<br />
ICD-9: 250.00-250.93, 648.00-648.04 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit); 99341-99350 (home visit); 99304-99310 (nursing<br />
facility); 99324-99337 (domiciliary); 97802-97804 <strong>and</strong> G0270-G0271 (nutrition therapy)<br />
Systolic codes<br />
_____ Most recent systolic blood pressure < 130 mm Hg (3074F)<br />
_____ Most recent systolic blood pressure 130 to 139 mm Hg (3075F)<br />
_____ Most recent systolic blood pressure > 140 mm Hg (3077F)<br />
AND<br />
Diastolic codes<br />
_____ Most recent diastolic blood pressure < 80 mm Hg (3078F)<br />
_____ Most recent diastolic blood pressure 80-89 mm Hg (3079F)<br />
_____ Most recent diastolic blood pressure > 90 mm Hg (3080F)<br />
OR<br />
_____<br />
Blood pressure <strong>measure</strong>ment not performed, reason not specified (2000F-8P)<br />
4) Screening for Future Fall Risk - Percentage <strong>of</strong> patients aged 65 years <strong>and</strong> older who were screened for<br />
future fall risk (patients are considered at risk for future falls if they have had 2 or more falls in the past year or any<br />
fall with injury in the past year) at least once within 12 months - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once<br />
per <strong>reporting</strong> period for patients seen during the <strong>reporting</strong> period. This <strong>measure</strong> is appropriate for use in all nonacute<br />
settings (excludes emergency departments <strong>and</strong> acute care hospitals). It is anticipated that clinicians who<br />
provide primary care for the patient will submit this <strong>measure</strong>.<br />
ICD-9: None specified - CPT: 97001-97004 (PT eval); 99201-99215 (<strong>of</strong>fice/outpatient visit), 99304-99310 (nursing facility), 99324-99328<br />
(domiciliary), 99334-99337 (domiciliary), 99341-99350 (home visits), 99387 <strong>and</strong> 99397 (preventive), 99401-99404 (preventive counseling),<br />
Definition: A fall is defined as a sudden, unintentional change in position causing an individual to l<strong>and</strong> at a lower<br />
level, on an object, the floor, or the ground, other than as a consequence <strong>of</strong> sudden onset <strong>of</strong> paralysis, epileptic<br />
seizure, or overwhelming external force (Tinetti).<br />
_____<br />
_____<br />
_____<br />
_____<br />
Screening for future fall risk; documentation <strong>of</strong> 2 or more falls in the past year or any fall with injury in the<br />
past year (1100F)<br />
Screening for future fall risk; documentation <strong>of</strong> no falls in the past year or only 1 fall without injury in the<br />
past year (1101F)<br />
Screening for future fall risk not performed for medical reasons (1100F-1P)<br />
Screening for future fall risk not performed, reason not specified (1100F-8P)<br />
5) Heart Failure: Angiotensin-Converting Enzyme (ACE) Inhibitor or Angiotensin Receptor<br />
Blocker (ARB) Therapy for Left Ventricular Systolic Dysfunction (LVSD) - Percentage <strong>of</strong> patients aged<br />
18 years <strong>and</strong> older with a diagnosis <strong>of</strong> heart failure <strong>and</strong> left ventricular systolic dysfunction (LVSD) who were<br />
prescribed ACE inhibitor or ARB therapy - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period<br />
for all heart failure patients seen during the <strong>reporting</strong> period. The left ventricular systolic dysfunction may be<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.<br />
5-5
determined by quantitative or qualitative assessment. Examples <strong>of</strong> a quantitative or qualitative assessment may<br />
include an echocardiogram: 1) that provides a numerical value <strong>of</strong> left ventricular systolic dysfunction or 2) that uses<br />
descriptive terms such as moderately or severely depressed left ventricular dysfunction. It is anticipated that<br />
clinicians who provide primary management <strong>of</strong> patients with heart failure will submit this <strong>measure</strong>.<br />
ICD-9: 402.01, 402.11, 402.91; 404.01, 404.03, 404.11, 404.13, 404.91, 404.93; 428.0, 428.1, 428.20-428.23, 428.30-428.33, 428.40-428.43,<br />
428.9 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99238, 99239 (discharge), 99241-99245 (<strong>of</strong>fice/outpatient consult), 99304-99310<br />
(nursing facility), 99324-99337 (domiciliary), 99341-99350 (home visit)<br />
_____<br />
OR<br />
_____<br />
_____<br />
_____<br />
AND<br />
_____<br />
_____<br />
_____<br />
ACE inhibitor or ARB therapy prescribed <strong>and</strong> left ventricular ejection fraction (LVEF)
_____<br />
_____<br />
_____<br />
_____<br />
_____<br />
Beta-blocker therapy prescribed (4006F)<br />
Documentation <strong>of</strong> medical reason(s) for not prescribing beta-blocker therapy (4006F-1P)<br />
Documentation <strong>of</strong> patient reason(s) for not prescribing beta-blocker therapy (4006F-2P)<br />
Documentation <strong>of</strong> system reason(s) for not prescribing beta-blocker therapy (4006F-3P)<br />
Beta-blocker therapy not prescribed, reason not specified (4006F-8P)<br />
8) Heart Failure: Beta-blocker Therapy for Left Ventricular Systolic Dysfunction - Percentage <strong>of</strong><br />
patients aged 18 years <strong>and</strong> older with a diagnosis <strong>of</strong> heart failure who also have left ventricular systolic dysfunction<br />
(LVSD) <strong>and</strong> who were prescribed beta-blocker therapy - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once per<br />
<strong>reporting</strong> period for all heart failure patients seen during the <strong>reporting</strong> period. The left ventricular systolic<br />
dysfunction may be determined by quantitative or qualitative assessment. Examples <strong>of</strong> a quantitative or qualitative<br />
assessment may include an echocardiogram: 1) that provides a numerical value <strong>of</strong> left ventricular systolic<br />
dysfunction or 2) that uses descriptive terms such as moderately or severely depressed left ventricular dysfunction. It<br />
is anticipated that clinicians who provide primary management <strong>of</strong> patients with heart failure will submit this<br />
<strong>measure</strong>.<br />
ICD-9: 402.01, 402.11, 402.91; 404.01, 404.03, 404.11, 404.13, 404.91, 404.93; 428.0, 428.1, 428.20-428.23, 428.30-428.33, 428.40-428.43,<br />
428.9 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice/outpatient consult), 99341-99350 (home visit), 99304-99310<br />
(nursing facility), 99324-99337 (domiciliary)<br />
_____<br />
Beta blocker therapy prescribed <strong>and</strong> left ventricular ejection fraction (LVEF) < 40% or documentation <strong>of</strong><br />
moderately or severely depressed left ventricular systolic function (4006F <strong>and</strong> 3021F)<br />
OR<br />
_____<br />
_____<br />
_____<br />
Documentation <strong>of</strong> medical reason(s) for not prescribing beta-blocker therapy (4006F-1P)<br />
Documentation <strong>of</strong> patient reason(s) for not prescribing beta-blocker therapy (4006F-2P)<br />
Documentation <strong>of</strong> system reason(s) for not prescribing beta-blocker therapy (4006F-3P)<br />
AND<br />
_____<br />
_____<br />
_____<br />
Left ventricular ejection fraction (LVEF) < 40% or documentation <strong>of</strong> moderately or severely depressed left<br />
ventricular systolic function (3021F)<br />
Left ventricular ejection fraction (LVEF) ≥ 40% or documentation as normal or mildly depressed left<br />
ventricular systolic function (3022F)<br />
Left ventricular ejection fraction (LVEF) was not performed or documented, reason not otherwise specified<br />
(3021F-8P)<br />
OR<br />
_____<br />
Beta-blocker therapy was not prescribed, reason not otherwise specified <strong>and</strong> left ventricular ejection<br />
fraction (LVEF) < 40% or documentation <strong>of</strong> moderately or severely depressed left ventricular systolic<br />
function (4006F-8P <strong>and</strong> 3021F)<br />
9) Antidepressant Medication During Acute Phase for Patients with New Episode <strong>of</strong> Major<br />
Depression - Percentage <strong>of</strong> patients aged 18 years <strong>and</strong> older diagnosed with new episode <strong>of</strong> major depressive<br />
disorder (MDD) <strong>and</strong> documented as treated with antidepressant medication during the entire 84-day (12 week) acute<br />
treatment phase - This <strong>measure</strong> is to be reported for each occurrence <strong>of</strong> MDD during the <strong>reporting</strong> period. It is<br />
anticipated that clinicians who provide the primary management <strong>of</strong> patients with major depressive disorder (MDD)<br />
will submit this <strong>measure</strong>.<br />
ICD-9: 296.20-296.24, 296.30-296.34, 298.0, 300.4, 309.1, 311 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit); 90801, 90802, 90804-90809,<br />
90862 (psychiatry)<br />
Definition: A “new episode” is defined as a patient with major depression who has not been seen or treated for<br />
major depression by any practitioner in the prior 4 months. A new episode can either be a recurrence for a patient<br />
with prior major depression or a patient with a new onset <strong>of</strong> major depression.<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.<br />
5-7
Report G8126: 1) For all patients with a diagnosis <strong>of</strong> Major Depression, New Episode who were prescribed a full<br />
12 week course <strong>of</strong> antidepressant medication OR 2) At the completion <strong>of</strong> a 12 week course <strong>of</strong> antidepressant<br />
medication.<br />
_____<br />
_____<br />
_____<br />
Patient with new episode <strong>of</strong> MDD documented as being treated with antidepressant medication during the<br />
entire 12 week acute treatment phase (G8126)<br />
Patient with new episode <strong>of</strong> MDD not documented as being treated with antidepressant medication during<br />
the entire 12 week acute treatment phase (G8127)<br />
Clinician documented that patient with a new episode <strong>of</strong> MDD was not an eligible c<strong>and</strong>idate for<br />
antidepressant medication treatment or patient did not have a new episode <strong>of</strong> MDD (G8128)<br />
39) Screening or Therapy for Osteoporosis for Women Aged 65 Years <strong>and</strong> Older - Percentage <strong>of</strong><br />
female patients aged 65 years <strong>and</strong> older who have a central dual-energy X-ray absorptiometry (DXA) <strong>measure</strong>ment<br />
ordered or performed at least once since age 60 or pharmacologic therapy prescribed within 12 months - This<br />
<strong>measure</strong> is to be reported a minimum <strong>of</strong> once during the <strong>reporting</strong> period for patients seen during the <strong>reporting</strong><br />
period. Female patients aged 65 years <strong>and</strong> older should have a central DXA <strong>measure</strong>ment ordered or performed at<br />
least once since the time they turned 60 years or have pharmacologic therapy prescribed to prevent or treat<br />
osteoporosis. It is anticipated that clinicians who provide primary care or care for treatment <strong>of</strong> fracture or<br />
osteoporosis will submit this <strong>measure</strong>.<br />
ICD-9: No specific diagnosis codes <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99387 <strong>and</strong> 99397 (preventive), 99401-99404 (preventive<br />
counseling)<br />
Definition: Pharmacologic Therapy: U.S. Food <strong>and</strong> Drug Administration approved pharmacologic options for<br />
osteoporosis prevention <strong>and</strong>/or treatment <strong>of</strong> postmenopausal osteoporosis include, in alphabetical order:<br />
bisphosphonates (alendronate, ib<strong>and</strong>ronate, <strong>and</strong> risedronate), calcitonin, estrogens (estrogens <strong>and</strong>/or hormone<br />
therapy), parathyroid hormone [PTH (1-34), teriparatide], <strong>and</strong> selective estrogen receptor modules or SERMs<br />
(raloxifene).<br />
_____<br />
_____<br />
_____<br />
_____<br />
_____<br />
_____<br />
_____<br />
Central Dual-energy X-Ray Absorptiometry (DXA) ordered (3096F)<br />
Central Dual-energy X-Ray Absorptiometry (DXA) results documented (3095F)<br />
Pharmacologic therapy (other than minerals/vitamins) for osteoporosis prescribed (4005F)<br />
Documentation <strong>of</strong> medical reason(s) for not ordering or performing a central dual energy X-ray<br />
absorptiometry (DXA) <strong>measure</strong>ment or not prescribing pharmacologic therapy for osteoporosis (3096F-1P)<br />
Documentation <strong>of</strong> patient reason(s) for not ordering or performing central dual energy X-ray<br />
absorptiometry (DXA) <strong>measure</strong>ment or not prescribing pharmacologic therapy for osteoporosis (3096F-2P)<br />
Documentation <strong>of</strong> system reason(s) for not ordering or performing central dual energy X-ray<br />
absorptiometry (DXA) <strong>measure</strong>ment or not prescribing pharmacologic therapy for osteoporosis (3096F-3P)<br />
Central dual energy X-ray absorptiometry (DXA) <strong>measure</strong>ment was not ordered or performed <strong>and</strong> a<br />
pharmacologic therapy for osteoporosis was not prescribed reason not otherwise specified (3096F-8P)<br />
40) Osteoporosis: Management Following Fracture - Percentage <strong>of</strong> patients aged 50 years <strong>and</strong> older with<br />
fracture <strong>of</strong> the hip, spine, or distal radius who had a central dual-energy X-ray absorptiometry (DXA) <strong>measure</strong>ment<br />
ordered or performed or pharmacologic therapy prescribed - This <strong>measure</strong> is to be reported after each occurrence <strong>of</strong><br />
a fracture during the <strong>reporting</strong> period. Patients with a fracture <strong>of</strong> the hip, spine, or distal radius should have a central<br />
DXA <strong>measure</strong>ment ordered or performed or pharmacologic therapy prescribed. The management (DXA ordered or<br />
performed or pharmacologic therapy prescribed) should occur within three months <strong>of</strong> the initial visit with the<br />
<strong>reporting</strong> clinician following the fracture. Patients with documentation <strong>of</strong> prior central DXA <strong>measure</strong>ment or already<br />
receiving pharmacologic therapy would automatically meet the intent <strong>of</strong> this <strong>measure</strong>. It is anticipated that clinicians<br />
who manage the primary or ongoing care for osteoporosis or osteoporosis related fracture(s) will submit this<br />
<strong>measure</strong>.<br />
ICD-9: 733.12-733.14, 805.00-805.08, 805.10-805.18, 805.2, 805.4, 805.6, 805.8, 813.40-813.42, 813.44, 813.45, 813.50-813.52, 813.54,<br />
820.00-820.03, 820.09-820.11, 820.20-820.22, 820.13. 820.8, 820.9 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice<br />
consult)<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.<br />
5-8
Definition: Pharmacologic Therapy: U.S. Food <strong>and</strong> Drug Administration approved pharmacologic options for<br />
osteoporosis prevention <strong>and</strong>/or treatment <strong>of</strong> postmenopausal osteoporosis include, in alphabetical order:<br />
bisphosphonates (alendronate, ib<strong>and</strong>ronate, <strong>and</strong> risedronate), calcitonin, estrogens (estrogens <strong>and</strong>/or hormone<br />
therapy), parathyroid hormone [PTH (1-34), teriparatide], <strong>and</strong> selective estrogen receptor modules or SERMs<br />
(raloxifene).<br />
_____<br />
_____<br />
_____<br />
_____<br />
_____<br />
_____<br />
_____<br />
Central dual energy X-ray absorptiometry (DXA) ordered (3096F)<br />
Central dual energy X-ray absorptiometry (DXA) results documented (3095F)<br />
Pharmacologic therapy (other than minerals/vitamins) for osteoporosis prescribed (4005F)<br />
Documentation <strong>of</strong> medical reason(s) for not ordering or performing a central dual energy X-ray<br />
absorptiometry (DXA) <strong>measure</strong>ment or not prescribing pharmacologic therapy for osteoporosis (3096F-1P)<br />
Documentation <strong>of</strong> patient reason(s) for not ordering or performing a central dual energy X-ray<br />
absorptiometry (DXA) <strong>measure</strong>ment or not prescribing pharmacologic therapy for osteoporosis (3096F-2P)<br />
Documentation <strong>of</strong> system reason(s) for not ordering or performing a central dual energy X-ray<br />
absorptiometry (DXA) <strong>measure</strong>ment or not prescribing pharmacologic therapy for osteoporosis (3096F-3P)<br />
Central dual energy X-ray absorptiometry (DXA) <strong>measure</strong>ment was not ordered or performed <strong>and</strong> a<br />
pharmacologic therapy for osteoporosis was not prescribed reason not otherwise specified (3096F-8P)<br />
41) Osteoporosis: Pharmacologic Therapy - Percentage <strong>of</strong> patients aged 50 years <strong>and</strong> older with a diagnosis<br />
<strong>of</strong> osteoporosis who were prescribed pharmacologic therapy within 12 months - This <strong>measure</strong> is to be reported a<br />
minimum <strong>of</strong> once per <strong>reporting</strong> period for patients seen during the <strong>reporting</strong> period. Patients with a diagnosis <strong>of</strong><br />
osteoporosis should be prescribed pharmacologic therapy to treat osteoporosis. It is anticipated that clinicians who<br />
provide services for patients with the diagnosis <strong>of</strong> osteoporosis will submit this <strong>measure</strong>.<br />
ICD-9: 733.00-733.03, 733.09 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice/outpatient consult), 99386-99387 <strong>and</strong><br />
99396- 99397 (preventive), 99401-99404 (preventive counseling)<br />
Definition: Pharmacologic Therapy: U.S. Food <strong>and</strong> Drug Administration approved pharmacologic options for<br />
osteoporosis prevention <strong>and</strong>/or treatment <strong>of</strong> postmenopausal osteoporosis include, in alphabetical order:<br />
bisphosphonates (alendronate, ib<strong>and</strong>ronate, <strong>and</strong> risedronate), calcitonin, estrogens (estrogens <strong>and</strong>/or hormone<br />
therapy), parathyroid hormone [PTH (1-34), teriparatide], <strong>and</strong> selective estrogen receptor modules or SERMs<br />
(raloxifene).<br />
_____<br />
_____<br />
1P)<br />
_____<br />
_____<br />
_____<br />
Pharmacologic therapy (other than minerals/vitamins) for osteoporosis prescribed (4005F)<br />
Documentation <strong>of</strong> medical reason(s) for not prescribing pharmacologic therapy for osteoporosis (4005F-<br />
Documentation <strong>of</strong> patient reason(s) for not prescribing pharmacologic therapy for osteoporosis (4005F-2P)<br />
Documentation <strong>of</strong> system reason for not prescribing pharmacologic therapy for osteoporosis (4005F-3P)<br />
Pharmacologic therapy for osteoporosis was not prescribed reason not otherwise specified (4005F-8P)<br />
42) Osteoporosis: Counseling for Vitamin D, Calcium Intake, <strong>and</strong> Exercise - Percentage <strong>of</strong> patients,<br />
regardless <strong>of</strong> age, with a diagnosis <strong>of</strong> osteoporosis who are either receiving both calcium <strong>and</strong> vitamin D or have<br />
been counseled regarding both calcium <strong>and</strong> vitamin D intake, <strong>and</strong> exercise at least once within 12 months - This<br />
<strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period for patients seen during the <strong>reporting</strong> period.<br />
Patients with a diagnosis <strong>of</strong> osteoporosis should be receiving both calcium <strong>and</strong> vitamin D or had counseling<br />
regarding their use <strong>and</strong> counseled on exercise. It is anticipated that clinicians who provide services for patients with<br />
the diagnosis <strong>of</strong> osteoporosis will submit this <strong>measure</strong>.<br />
ICD-9: 733.00-733.03, 733.09 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice/outpatient consult), 99385-99387 <strong>and</strong><br />
99395-99397 (preventive), 99401-99404 (preventive counseling)<br />
_____<br />
_____<br />
_____<br />
Documentation <strong>of</strong> receipt <strong>of</strong> counseling on exercise AND either both calcium <strong>and</strong> vitamin D use or<br />
counseling regarding both calcium <strong>and</strong> vitamin D use (4019F)<br />
Documentation <strong>of</strong> medical reason(s) for patient not receiving both calcium <strong>and</strong> vitamin D or <strong>and</strong> not<br />
needing counseling regarding both calcium <strong>and</strong> vitamin D intake, <strong>and</strong> exercise (e.g., patient has dementia<br />
<strong>and</strong> is unable to receive counseling) (4019F-1P)<br />
Receipt <strong>of</strong> counseling on exercise AND either both calcium <strong>and</strong> vitamin D use or counseling regarding<br />
both calcium <strong>and</strong> vitamin D use was not documented reason not otherwise specified (4019F-8P)<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.<br />
5-9
46) Medication Reconciliation - Percentage <strong>of</strong> patients aged 65 years <strong>and</strong> older discharged from any inpatient<br />
facility (e.g., hospital, skilled nursing facility, or rehabilitation facility) <strong>and</strong> seen within 60 days following discharge<br />
in the <strong>of</strong>fice by the physician providing on-going care who had a reconciliation <strong>of</strong> the discharge medications with<br />
the current medication list in the medical record documented - This <strong>measure</strong> is to be reported at an <strong>of</strong>fice visit<br />
occurring within 60 days <strong>of</strong> each inpatient facility discharge during the <strong>reporting</strong> period. This <strong>measure</strong> is appropriate<br />
for use in the ambulatory setting only. It is anticipated that clinicians who provide primary on-going care will submit<br />
this <strong>measure</strong> when a patient is seen in the <strong>of</strong>fice within 60 days following discharge from any inpatient facility. If a<br />
patient has not been discharged within the 60-day timeframe from an inpatient facility, there are no <strong>reporting</strong><br />
requirements for this <strong>measure</strong>.<br />
ICD-9: No specific diagnosis code <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99387 <strong>and</strong> 99397 (preventive), 99401-99404 (preventive<br />
counseling)<br />
_____<br />
_____<br />
Patient discharged from an inpatient facility within the last 60 days <strong>and</strong> discharge medications reconciled<br />
with the current medication list in outpatient medical record (1110F <strong>and</strong> 1111F)<br />
Patient discharged from an inpatient facility within the last 60 days <strong>and</strong> discharge medication not<br />
reconciled with current medication list in the medical record, reason not specified (1110F <strong>and</strong> 1111F-8P)<br />
47) Advance Care Plan - Percentage <strong>of</strong> patients aged 65 years <strong>and</strong> older with documentation <strong>of</strong> a surrogate<br />
decision-maker or advance care plan in the medical record - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once per<br />
<strong>reporting</strong> period for patients seen during the <strong>reporting</strong> period. This <strong>measure</strong> is appropriate for use in all healthcare<br />
settings. It is anticipated that clinicians who provide primary care services for the patient will submit this <strong>measure</strong>.<br />
ICD-9: No specific diagnosis codes <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99218-99220 (observation services), 99221-99223 (initial<br />
inpatient), 99231-99233 (subsequent inpatient), 99234-99236 (admit <strong>and</strong> discharge on the same day), 99281-99285 (ED services), 99291<br />
(critical care), 99304-99310 (nursing facility), 99324-99337 (domiciliary/rest home), 99341-99350 (home visits), 99387 <strong>and</strong> 99397<br />
(preventive services), 99401-99404 (preventive counseling)<br />
_____<br />
_____<br />
_____<br />
Surrogate decision maker or advance care plan documented in the medical record (1080F)<br />
Surrogate decision maker or advance directive not documented for patient reasons (1080F-2P)<br />
Surrogate decision maker or advance directive not documented, reason not specified (1080F-8P)<br />
(Joy’s Comment: For successful <strong>reporting</strong> <strong>of</strong> this <strong>measure</strong>, primary care physicians will have to report on this<br />
<strong>measure</strong> at least one time for every Medicare patient.)<br />
48) Assessment <strong>of</strong> Presence or Absence <strong>of</strong> Urinary Incontinence in Women Aged 65 Years <strong>and</strong><br />
Older - Percentage <strong>of</strong> female patients aged 65 years <strong>and</strong> older who were assessed for the presence or absence <strong>of</strong><br />
urinary incontinence within 12 months - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period for<br />
patients seen during the <strong>reporting</strong> period. This <strong>measure</strong> is appropriate for use in the ambulatory setting only. It is<br />
anticipated that clinicians who provide primary care for the patient will submit this <strong>measure</strong>.<br />
ICD-9: No specific codes <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99387 <strong>and</strong> 99397 (preventive), 99401-99404 (preventive<br />
counseling)<br />
Definition: Urinary incontinence is defined as any involuntary leakage <strong>of</strong> urine.<br />
_____<br />
_____<br />
_____<br />
Presence or absence <strong>of</strong> urinary incontinence assessed (1090F)<br />
Presence or absence <strong>of</strong> urinary incontinence not assessed for medical reasons (1090F-1P)<br />
Presence or absence <strong>of</strong> urinary incontinence not assessed reason not specified (1090F-8P)<br />
49) Characterization <strong>of</strong> Urinary Incontinence in Women Aged 65 Years <strong>and</strong> Older - Percentage <strong>of</strong><br />
female patients aged 65 years <strong>and</strong> older with a diagnosis <strong>of</strong> urinary incontinence whose urinary incontinence was<br />
characterized at least once within 12 months - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong><br />
period for patients seen during the <strong>reporting</strong> period. This <strong>measure</strong> is appropriate for use in the ambulatory setting<br />
only. It is anticipated that clinicians who provide services for patients with the diagnosis <strong>of</strong> urinary incontinence will<br />
submit this <strong>measure</strong>.<br />
ICD-9: 307.6, 625.6, 788.30-788.39 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice/outpatient consult), 99387 <strong>and</strong> 99397<br />
(preventive), 99401-99404 (preventive counseling)<br />
5-10<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
Definition: Characterization includes, but is not limited to, (frequency, volume, timing, type <strong>of</strong> symptoms, how<br />
bothersome)<br />
_____<br />
_____<br />
Urinary incontinence characterized (1091F)<br />
Urinary incontinence not characterized reason not specified (1091F-8P)<br />
50) Plan <strong>of</strong> Care for Urinary Incontinence in Women Aged 65 Years <strong>and</strong> Older - Percentage <strong>of</strong> female<br />
patients aged 65 years <strong>and</strong> older with a diagnosis <strong>of</strong> urinary incontinence with a documented plan <strong>of</strong> care for urinary<br />
incontinence at least once within 12 months - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period<br />
for patients seen during the <strong>reporting</strong> period. This <strong>measure</strong> is appropriate for use in the ambulatory setting only. It is<br />
anticipated that clinicians who provide services for patients with the diagnosis <strong>of</strong> urinary incontinence will submit<br />
this <strong>measure</strong>.<br />
ICD-9: 307.6, 625.6, 788.30-788.39 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice/outpatient consult), 99387 <strong>and</strong> 99397<br />
(preventive), 99401-99404 (preventive counseling)<br />
Definition: Plan <strong>of</strong> care may include behavioral interventions (e.g., bladder training, pelvic floor muscle training,<br />
prompted voiding), referral to specialist, surgical treatment, reassess at follow-up visit, lifestyle interventions,<br />
addressing co-morbid factors, modification or discontinuation <strong>of</strong> medications contributing to urinary incontinence,<br />
or pharmacologic therapy.<br />
_____<br />
_____<br />
Urinary incontinence plan <strong>of</strong> care documented (0509F)<br />
Plan <strong>of</strong> care for urinary incontinence not documented reason not specified (0509F-8P)<br />
51) Chronic Obstructive Pulmonary Disease (COPD): Spirometry Evaluation - Percentage <strong>of</strong> patients<br />
aged 18 years <strong>and</strong> older with a diagnosis <strong>of</strong> COPD who had spirometry evaluation results documented - This<br />
<strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period using the most recent spirometry results in the<br />
patient record for patients seen during the <strong>reporting</strong> period. It is anticipated that clinicians who provide primary care<br />
services for the patient will submit this <strong>measure</strong>.<br />
ICD-9: 491.0, 491.1, 491.20-491.22, 491.8, 491.9, 492.0, 492.8, 496 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245<br />
(<strong>of</strong>fice/outpatient consult), 99385-99387, 99395-99397 (preventive), 99401-99404 (preventive counseling)<br />
Instructions: Look for most recent documentation <strong>of</strong> spirometry evaluation results in the medical record; do not<br />
limit the search to the <strong>reporting</strong> period.<br />
_____<br />
_____<br />
_____<br />
_____<br />
_____<br />
Spirometry results documented <strong>and</strong> reviewed (3023F)<br />
Spirometry results not documented medical reason(s) (3023F-1P)<br />
Spirometry results not documented for patient reasons (3023F-2P)<br />
Spirometry results not documented for system reasons (3023F-3P)<br />
Spirometry results not documented, reason not specified (3023F-8P)<br />
52) Chronic Obstructive Pulmonary Disease (COPD): Bronchodilator Therapy - Percentage <strong>of</strong> patients<br />
aged 18 years <strong>and</strong> older with a diagnosis <strong>of</strong> COPD <strong>and</strong> who have an FEV1/FVC less than 70% <strong>and</strong> have symptoms<br />
who were prescribed an inhaled bronchodilator - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong><br />
period for all COPD patients seen during the <strong>reporting</strong> period. It is anticipated that clinicians who provide primary<br />
care services for the patient will submit this <strong>measure</strong>.<br />
ICD-9: 491.0, 491.1, 491.20-491.22, 491.8, 491.9, 492.0, 492.8, 496 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245<br />
(<strong>of</strong>fice/outpatient consult), 99385-99387, 99395-99397 (preventive), 99401-99404 (preventive counseling)<br />
_____<br />
_____<br />
_____<br />
Inhaled bronchodilator prescribed <strong>and</strong> spirometry test results demonstrate FEV 1 /FVC < 70% with COPD<br />
symptoms (e.g., dyspnea, cough/sputum, wheezing) (4025F <strong>and</strong> 3025F)<br />
Documentation <strong>of</strong> medical reason(s) for not prescribing an inhaled bronchodilator <strong>and</strong> spirometry test<br />
results demonstrate FEV 1 /FVC < 70% with COPD symptoms (e.g., dyspnea, cough/sputum, wheezing)<br />
(4025F-1P <strong>and</strong> 3025F)<br />
Documentation <strong>of</strong> patient reason(s) for not prescribing an inhaled bronchodilator <strong>and</strong> spirometry test results<br />
demonstrate FEV 1 /FVC < 70% with COPD symptoms (e.g., dyspnea, cough/sputum, wheezing) (4025F-2P<br />
<strong>and</strong> 3025F)<br />
5-11<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
_____<br />
_____<br />
_____<br />
_____<br />
Documentation <strong>of</strong> system reason(s) for not prescribing an inhaled bronchodilator <strong>and</strong> spirometry test results<br />
demonstrate FEV 1 /FVC < 70% with COPD symptoms (e.g., dyspnea, cough/sputum, wheezing) (4025F-3P<br />
<strong>and</strong> 3025F)<br />
Spirometry results demonstrate FEV 1 /FVC ≥ 70% or patient does not have COPD symptoms (3027F)<br />
Spirometry test not performed or documented (3025F-8P)<br />
Inhaled bronchodilator not prescribed, reason not specified <strong>and</strong> spirometry test results demonstrate<br />
FEV 1 /FVC < 70% with COPD symptoms (e.g., dyspnea, cough/sputum, wheezing) (4025F-8P <strong>and</strong> 3025F)<br />
53) Asthma: Pharmacologic Therapy - Percentage <strong>of</strong> patients aged 5 to 40 years with a diagnosis <strong>of</strong> mild,<br />
moderate, or severe persistent asthma who were prescribed either the preferred long-term control medication<br />
(inhaled corticosteroid) or an acceptable alternative treatment - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once<br />
per <strong>reporting</strong> period for all asthma patients seen during the <strong>reporting</strong> period. It is anticipated that clinicians who<br />
provide primary care services for the patient will submit this <strong>measure</strong>.<br />
ICD-9: 493.00-493.02, 493.10-493.12, 493.20-493.22, 493.81, 493.82, 493.90, 493.92 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-<br />
99245 (<strong>of</strong>fice/outpatient consult), 99383-99386, 99393-99396 (preventive), 99401-99404 (preventive counseling)<br />
Definition: acceptable alternative treatment (leukotriene modifiers, cromolyn sodium, nedocromil sodium, or<br />
sustained-released methylxanthines)<br />
_____<br />
_____<br />
_____<br />
_____<br />
Persistent asthma (mild, moderate, or severe) <strong>and</strong> preferred long term control medication or acceptable<br />
alternative treatment prescribed (4015F <strong>and</strong> 1038F)<br />
Persistent asthma (mild, moderate, or severe) <strong>and</strong> preferred long-term control medication or acceptable<br />
alternative treatment not prescribed for patient reasons (4015F-2P <strong>and</strong> 1038F)<br />
Intermittent asthma (1039F)<br />
Persistent asthma (mild, moderate, or severe) <strong>and</strong> preferred long-term control medication or acceptable<br />
alternative treatment not prescribed, reason not specified (4015F-8P <strong>and</strong> 1038F)<br />
60) Gastroesophageal Reflux Disease (GERD): Assessment for Alarm Symptoms - Percentage <strong>of</strong><br />
patients aged 18 years <strong>and</strong> older with a diagnosis <strong>of</strong> GERD, seen for an initial evaluation, who were assessed for the<br />
presence or absence <strong>of</strong> the following alarm symptoms: involuntary weight loss, dysphagia, <strong>and</strong> GI bleeding - This<br />
<strong>measure</strong> is to be reported once for all GERD patients seen during the <strong>reporting</strong> period. Patients seen for an initial<br />
evaluation <strong>of</strong> GERD should have documentation in the medical record <strong>of</strong> the presence or absence <strong>of</strong> alarm<br />
symptoms. If the initial evaluation <strong>of</strong> GERD occurred prior to the <strong>reporting</strong> period, report the proper CPT Category<br />
II code with modifier indicated in the numerator <strong>coding</strong> indicating this is not the initial evaluation. It is anticipated<br />
that clinicians who provide care for patients with GERD will submit this <strong>measure</strong>.<br />
ICD-9: 530.81, 530.10-530.12, 530.19 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice/outpatient consult)<br />
Definition: Patients assessed for the presence or absence <strong>of</strong> the following alarm symptoms: involuntary weight loss,<br />
dysphagia, <strong>and</strong> GI bleeding<br />
_____<br />
_____<br />
_____<br />
_____<br />
_____<br />
Alarm symptoms assessed; none present (1070F)<br />
Alarm symptoms assessed; one or more present (1071F)<br />
Patient does not meet denominator inclusion because the initial evaluation <strong>of</strong> GERD occurred prior to the<br />
<strong>reporting</strong> period (1070F-8P)<br />
Alarm symptoms not assessed for medical reasons (1070F-1P)<br />
Alarm symptoms not assessed, reason not specified (1071F-8P)<br />
(Joy’s Comment: For successful <strong>reporting</strong> <strong>of</strong> this <strong>measure</strong>, physicians will have to report on this <strong>measure</strong> at least<br />
one time for every Medicare patient with GERD.)<br />
61) Gastroesophageal Reflux Disease (GERD): Upper Endoscopy for Patients with Alarm<br />
Symptoms - Percentage <strong>of</strong> patients aged 18 years <strong>and</strong> older with a diagnosis <strong>of</strong> GERD, seen for an initial<br />
evaluation, with at least one alarm symptom who were either referred for upper endoscopy or had an upper<br />
endoscopy performed - This <strong>measure</strong> is to be reported once for all GERD patients seen during the <strong>reporting</strong> period.<br />
Patients seen for an initial evaluation <strong>of</strong> GERD <strong>and</strong> at least one alarm symptom will be referred for upper endoscopy<br />
or have an upper endoscopy performed. If the initial evaluation <strong>of</strong> GERD occurred prior to the <strong>reporting</strong> period,<br />
5-12<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
eport the proper CPT II Category II code with modifier indicated in the numerator <strong>coding</strong> indicating this is not the<br />
initial evaluation. It is anticipated that clinicians who provide care for patients with GERD will submit this <strong>measure</strong>.<br />
ICD-9: 530.81, 530.10-530.12, 530.19 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice/outpatient consult)<br />
Definition: Alarm symptoms for GERD include involuntary weight loss, dysphagia, <strong>and</strong> GI bleeding.<br />
_____ Upper gastrointestinal endoscopy performed (3130F)<br />
_____ Documentation <strong>of</strong> referral for upper gastrointestinal endoscopy (3132F <strong>and</strong> 1071F)<br />
_____ Patient does not have alarm symptoms (1070F)<br />
_____ Initial evaluation <strong>of</strong> GERD occurred prior to the <strong>reporting</strong> period (1071F-8P)<br />
_____ Upper endoscopy not performed or patient not referred for upper endoscopy for medical reasons (e.g.,<br />
patient has already had the procedure) (3130F-1P <strong>and</strong> 1071F)<br />
_____ Upper endoscopy not performed or patient not referred for upper endoscopy for patient reasons (3130F-2P<br />
<strong>and</strong> 1071F)<br />
_____ Upper endoscopy not performed or patient not referred for upper endoscopy for system reasons (3130F-3P<br />
<strong>and</strong> 1071F)<br />
_____ Upper endoscopy not performed or patient not referred for upper endoscopy, reason not specified (3130F-<br />
8P <strong>and</strong> 1071F)<br />
(Joy’s Comment: For successful <strong>reporting</strong> <strong>of</strong> this <strong>measure</strong>, physicians will have to report on this <strong>measure</strong> <strong>and</strong><br />
<strong>measure</strong> #60 at least one time for every Medicare patient with GERD.)<br />
63) Gastroesophageal Reflux Disease (GERD): Barium Swallow- Inappropriate Use - Percentage <strong>of</strong><br />
patients aged 18 years <strong>and</strong> older with a diagnosis <strong>of</strong> GERD, seen for an initial evaluation, who did not have a<br />
Barium swallow test ordered - This <strong>measure</strong> is to be reported once for all GERD patients seen during the <strong>reporting</strong><br />
period. Patients being seen for an initial evaluation <strong>of</strong> GERD should not receive a barium swallow test. If the initial<br />
evaluation <strong>of</strong> GERD occurred prior to the <strong>reporting</strong> period, report the proper CPT Category II with modifier<br />
indicated in the numerator <strong>coding</strong> indicating this is not the initial evaluation. It is anticipated that clinicians who<br />
provide care for patients with GERD will submit this <strong>measure</strong>.<br />
ICD-9: 530.81, 530.10-530.12, 530.19 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice/outpatient consult)<br />
Definitions: This is an overuse <strong>measure</strong>. For performance, the numerator will be calculated as the difference<br />
between patients in the denominator <strong>and</strong> patients for whom a CPT Category II code was reported for barium<br />
swallow test ordered. A higher score indicates appropriate treatment <strong>of</strong> patients with GERD (i.e., the proportion for<br />
whom a barium swallow test was not ordered).<br />
_____<br />
_____<br />
_____<br />
_____<br />
Barium swallow test ordered (3142F)<br />
Patient does not meet denominator inclusion because the initial evaluation <strong>of</strong> GERD occurred prior to the<br />
<strong>reporting</strong> period (3200F-8P)<br />
Barium swallow test ordered for medical reasons (3142F-1P)<br />
Barium swallow test not ordered (3200F)<br />
(Joy’s Comment: For successful <strong>reporting</strong> <strong>of</strong> this <strong>measure</strong>, physicians will have to report on this <strong>measure</strong> <strong>and</strong><br />
<strong>measure</strong> #60 at least one time for every Medicare patient with GERD.)<br />
64) Asthma Assessment - Percentage <strong>of</strong> patients aged 5 to 40 years with a diagnosis <strong>of</strong> asthma who were<br />
evaluated during at least one <strong>of</strong>fice visit within 12 months for the frequency (numeric) <strong>of</strong> daytime <strong>and</strong> nocturnal<br />
asthma symptoms - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period for patients seen during<br />
the <strong>reporting</strong> period. It is anticipated that clinicians who provide primary care services for the patient with a<br />
diagnosis <strong>of</strong> asthma will submit this <strong>measure</strong>.<br />
ICD-9: 493.00-493.02, 493.10-493.12, 493.20-493.22, 493.81, 493.82, 493.90, 493.92 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-<br />
99245 (<strong>of</strong>fice/outpatient consult), 99383-99386, 99393-99396 (preventive), 99401-99404 (preventive counseling)<br />
Definitions: To be counted in calculations <strong>of</strong> this <strong>measure</strong>, symptom frequency must be numerically quantified.<br />
Measure may also be met by clinician documentation or patient completion <strong>of</strong> an asthma assessment<br />
5-13<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
tool/survey/questionnaire. Assessment tool may include the Quality Metric Asthma Control Test, National Asthma<br />
Education & Prevention Program (NAEPP) Asthma Symptoms <strong>and</strong> Peak Flow Diary.<br />
_____<br />
_____<br />
Asthma symptoms evaluated (includes physician documentation <strong>of</strong> numeric frequency <strong>of</strong> symptoms or<br />
patient completion <strong>of</strong> an asthma assessment tool/survey/questionnaire) (1005F)<br />
Asthma symptom frequency not evaluated, reason not specified (1005F-8P)<br />
PAYMENT FOR EVALUATION AND MANAGEMENT SERVICES<br />
PROVIDED DURING GLOBAL PERIOD OF SURGERY<br />
Medicare Claims Processing Manual Chapter 12 §30.6.6 (Rev. 954, Issued: 05-19-06, Effective: 06-01-<br />
06, Implementation: 08-20-06)<br />
CPT Modifier -24 - Unrelated Evaluation <strong>and</strong> Management Service by Same Physician during<br />
Postoperative Period<br />
Carriers pay for an evaluation <strong>and</strong> management service other than inpatient hospital care before discharge<br />
from the hospital following surgery (CPT codes 99221-99238) if it was provided during the postoperative<br />
period <strong>of</strong> a surgical procedure, furnished by the same physician who performed the procedure, billed with<br />
CPT modifier -24, <strong>and</strong> accompanied by documentation that supports that the service is not related to the<br />
postoperative care <strong>of</strong> the procedure. They do not pay for inpatient hospital care that is furnished during<br />
the hospital stay in which the surgery occurred unless the doctor is also treating another medical condition<br />
that is unrelated to the surgery. All care provided during the inpatient stay in which the surgery occurred<br />
is compensated through the global surgical payment.<br />
CPT Modifier -25 - Significant Evaluation <strong>and</strong> Management Service by Same Physician on Date <strong>of</strong><br />
Global Procedure<br />
Medicare requires that Current Procedural Terminology (CPT) modifier -25 should only be used on<br />
claims for evaluation <strong>and</strong> management (E/M) services, <strong>and</strong> only when these services are provided by the<br />
same physician (or same qualified nonphysician practitioner) to the same patient on the same day as<br />
another procedure or other service. Carriers pay for an E/M service provided on the day <strong>of</strong> a procedure<br />
with a global fee period if the physician indicates that the service is for a significant, separately<br />
identifiable E/M service that is above <strong>and</strong> beyond the usual pre- <strong>and</strong> post-operative work <strong>of</strong> the<br />
procedure. Different diagnoses are not required for <strong>reporting</strong> the E/M service on the same date as the<br />
procedure or other service. Modifier -25 is added to the E/M code on the claim.<br />
Both the medically necessary E/M service <strong>and</strong> the procedure must be appropriately <strong>and</strong> sufficiently<br />
documented by the physician or qualified nonphysician practitioner in the patient’s medical record to<br />
support the claim for these services, even though the documentation is not required to be submitted with<br />
the claim.<br />
CPT Modifier -57 - Decision for Surgery Made Within Global Surgical Period<br />
Carriers pay for an evaluation <strong>and</strong> management service on the day <strong>of</strong> or on the day before a procedure<br />
with a 90-day global surgical period if the physician uses CPT modifier -57 to indicate that the service<br />
resulted in the decision to perform the procedure. Carriers may not pay for an evaluation <strong>and</strong> management<br />
service billed with the CPT modifier -57 if it was provided on the day <strong>of</strong> or the day before a procedure<br />
with a 0 or 10-day global surgical period.<br />
Payment for Evaluation <strong>and</strong> Management Services Provided During Global Period <strong>of</strong> Surgery<br />
• The Centers for Medicare & Medicaid Services (CMS) has clarified the documentation<br />
requirements <strong>and</strong> policy requirements for the use <strong>of</strong> CPT modifier -25 used with E/M services.<br />
Please refer to the manual attachment to CR5025, The Medicare Claims Processing Manual,<br />
Chapter 12, §30.6.6, for revisions regarding the use <strong>of</strong> CPT modifier -25<br />
5-14<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
• Physicians <strong>and</strong> qualified nonphysician practitioners (NPP) should use CPT modifier -25 to<br />
designate a significant, separately identifiable E/M service provided by the same<br />
physician/qualified NPP to the same patient on the same day as another procedure or other<br />
service with a global fee period.<br />
• Common Procedural Terminology (CPT) modifier -25 identifies a significant, separately<br />
identifiable evaluation <strong>and</strong> management (E/M) service. It should be used when the E/M service is<br />
above <strong>and</strong> beyond the usual pre- <strong>and</strong> postoperative work <strong>of</strong> a procedure with a global fee period<br />
performed on the same day as the E/M service.<br />
• Different diagnoses are not required for <strong>reporting</strong> the E/M service on the same date as the<br />
procedure or other service with a global fee period. Modifier -25 is added to the E/M code on the<br />
claim.<br />
• Both the medically necessary E/M service <strong>and</strong> the procedure must be appropriately <strong>and</strong><br />
sufficiently documented by the physician or qualified NPP in the patient’s medical record to<br />
support the need for modifier -25 on the claim for these services, even though the documentation<br />
is not required to be submitted with the claim.<br />
• Your Carrier will not retract payment for claims already paid or retroactively pay claims<br />
processed prior to the implementation <strong>of</strong> CR5025. But, they will adjust claims brought to their<br />
attention.<br />
• Carriers will not pay for an E/M service reported with a procedure having a global fee period<br />
unless CPT modifier -25 is appended to the E/M service to designate it as a significant <strong>and</strong><br />
separately identifiable E/M service from the procedure.<br />
PREOPERATIVE SERVICES<br />
§1862(a)(1)(A) <strong>of</strong> the Social Security Act requires that in order to qualify for Medicare coverage, a<br />
service must be reasonable <strong>and</strong> necessary for the diagnosis <strong>and</strong> treatment <strong>of</strong> illness or injury, or to<br />
improve the functioning <strong>of</strong> a malformed body member. A preoperative service performed due to hospital<br />
or malpractice protocol cannot supercede this guideline for Medicare coverage purposes. Medicare will<br />
pay for preoperative evaluation <strong>and</strong> management services, <strong>and</strong> diagnostic tests if they are medically<br />
necessary <strong>and</strong> meet the documentation requirements <strong>of</strong> the service rendered.<br />
CMS Transmittal #1707 – May 31, 2001<br />
A. General--This manual instruction addresses payment for preoperative services that are not included in<br />
the global surgery payment.<br />
B. Non-global Preoperative Services -- Consist <strong>of</strong> evaluation <strong>and</strong> management (E/M) services<br />
(preoperative examinations) that are not included in the global surgical package <strong>and</strong> diagnostic tests<br />
performed for the purpose <strong>of</strong> evaluating a patient's risk <strong>of</strong> perioperative complications <strong>and</strong> optimizing<br />
perioperative care. Medicare will pay for all medically necessary preoperative.<br />
C. Non-global Preoperative Examinations -- E/M services performed that are not included in the global<br />
surgical package for evaluating a patient's risk <strong>of</strong> perioperative complications <strong>and</strong> to optimize<br />
perioperative care. Preoperative examinations may be billed by using an appropriate CPT code (e.g.,<br />
new patient, established patient, or consultation). Such non-global preoperative examinations are<br />
payable if they are medically necessary <strong>and</strong> meet the documentation <strong>and</strong> other requirements for the<br />
service billed.<br />
D. Preoperative Diagnostic Tests -- Tests performed to determine a patient's perioperative risk <strong>and</strong><br />
optimize perioperative care. Preoperative diagnostic tests are payable if they are medically necessary<br />
<strong>and</strong> meet any other applicable requirements.<br />
5-15<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
E. Statutory Basis for Payment<br />
1. §1862(a)(7) <strong>of</strong> the Social Security Act (the Act) excludes payment for "routine physical<br />
checkups." Both physical examinations <strong>and</strong> diagnostic tests that are performed in the absence <strong>of</strong><br />
signs or symptoms <strong>of</strong> illness or injury may be denied as a routine physical checkup under<br />
§1862(a)(7) <strong>of</strong> the Act. The regulatory provision that further explains this policy is contained in<br />
42 CFR Part 411.15(a)(1).<br />
2. §1862(a)(1)(A) <strong>of</strong> the Act states that no payment will be made for "items or services which are<br />
not reasonable <strong>and</strong> necessary for the diagnosis or treatment <strong>of</strong> illness or injury or to improve the<br />
functioning <strong>of</strong> a malformed body member." Both physical examinations <strong>and</strong> diagnostic tests<br />
performed in the absence <strong>of</strong> signs or symptoms can be denied as unnecessary under<br />
§1862(a)(1)(A) <strong>of</strong> the Act.<br />
3. Through previous program <strong>and</strong> decision memor<strong>and</strong>a, Medicare has established a clear hierarchy<br />
in the application <strong>of</strong> these two statutory provisions for use in denying payment for physical<br />
examinations <strong>and</strong> diagnostic tests. Claims are initially evaluated against the statutory<br />
requirements <strong>of</strong> §1862(a)(7) <strong>of</strong> the Act <strong>and</strong>, if not denied on that basis, they are evaluated against<br />
the statutory requirements <strong>of</strong> §1862 (a)(1)(A). If they meet the statutory requirements <strong>of</strong><br />
§1862(a)(1)(A) <strong>of</strong> the Act, they are paid. In general, §1862(a)(1)(A) <strong>of</strong> the Act is to be invoked<br />
only for denying payment for services that are otherwise covered, <strong>and</strong> are not otherwise excluded<br />
from payment, but which are not covered in a particular case because they are not deemed<br />
"medically reasonable <strong>and</strong> necessary" when performed in that specific situation.<br />
F. Applicability <strong>of</strong> §1862(a)(7) <strong>of</strong> the Act to Preoperative Services<br />
1. Preoperative Examinations—For purposes <strong>of</strong> billing under the Physician Fee Schedule, medical<br />
preoperative examinations performed by, or at the request <strong>of</strong>, the attending surgeon do not fall<br />
within the statutory exclusion articulated in §1862(a)(7) <strong>of</strong> the Act. These examinations are<br />
payable if they are medically necessary (i.e., based on a determination <strong>of</strong> medical necessity under<br />
§1862(a)(1)(A) <strong>of</strong> the Act), <strong>and</strong> meet the documentation requirements <strong>of</strong> the service billed.<br />
Determination <strong>of</strong> the appropriate E/M code is based on the requirements <strong>of</strong> the specific type <strong>and</strong><br />
level <strong>of</strong> visit or consultation the physician submits on his claim (e.g., established patient, new<br />
patient, consultation).<br />
2. Preoperative Diagnostic Tests—When billing under the Physician Fee Schedule, preoperative<br />
diagnostic tests performed by, or at the request <strong>of</strong>, the physician performing preoperative<br />
examinations, do not fall within the statutory exclusion articulated in §1862)(a)(7) <strong>of</strong> the Act.<br />
These diagnostic tests are payable if they are medically necessary (i.e., they may be denied under<br />
§1862(a)(1)(A)).<br />
G. ICD-9 Coding Requirements for Preoperative Service - All claims for preoperative medical<br />
examination <strong>and</strong> preoperative diagnostic tests (i.e., preoperative medical evaluations) must be<br />
accompanied by the appropriate ICD-9 code for preoperative examination (e.g., V72.81 through<br />
V72.84). Additional appropriate ICD-9 codes for the condition(s) that prompted surgery <strong>and</strong> for<br />
conditions that prompted the preoperative medical evaluation (if any), should also be documented on<br />
the claim. Other diagnoses <strong>and</strong> conditions affecting the patient may also be documented on the claim,<br />
if appropriate. The ICD-9 code appearing in the line item <strong>of</strong> a preoperative examination or diagnostic<br />
test must be the code for the appropriate preoperative examination (e.g., V72.81 through V72.84)<br />
H. Reasonable <strong>and</strong> Necessary Services -For the purposes <strong>of</strong> establishing preoperative services as<br />
reasonable <strong>and</strong> necessary, all claims are subject to applicable national coverage decisions. In the<br />
absence <strong>of</strong> a national coverage decision, reasonable <strong>and</strong> necessary services are determined by Carrier<br />
discretion. Establishing reasonable <strong>and</strong> necessary preoperative medical evaluations is facilitated when<br />
the ICD-9 code(s) for the condition(s) that prompted surgery, <strong>and</strong> for the conditions that prompted the<br />
5-16<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
preoperative medical evaluation (if any), are documented as additional diagnoses on the claim.<br />
[Medicare Carriers Manual, Part 3, Claims Process §15046 – CMS Paper Manual<br />
Physician Regulatory Issues Team (PRIT) Issue – History <strong>and</strong> Physicals by Podiatrists<br />
Issue<br />
Status<br />
Podiatrists have asked that Medicare allow them to perform H&Ps on hospital<br />
inpatients.<br />
CMS is considering a change to the Hospital Condition <strong>of</strong> Participation that<br />
would permit Podiatrists to perform this service.<br />
August 13, 2004 The Hospital Condition <strong>of</strong> Participation are now in the final approval process.<br />
One <strong>of</strong> 4 PRIT issues which will be resolved in the soon to be released Hospitals<br />
October 6, 2004 Conditions <strong>of</strong> Participation.<br />
The PRIT will announce on this website when the Hospital CoP is released.<br />
Dec 20, 2004 CMS published a proposed rule - Hospital CoP 3122-P - that addresses this<br />
issue.<br />
March 25, 2005 The clearance process is very involved for changes to the Conditions <strong>of</strong><br />
Participation. However, we are confident that the new CoP will be released late<br />
May 9, 2006<br />
in 2006 or very early in 2007.<br />
Date Issue Created 12/01/2003<br />
Physician Regulatory Issues Team (PRIT) Issue – History <strong>and</strong> Physicals for Outpatient Surgical<br />
Procedures<br />
Issue<br />
Hospitals have asked if it would be permissible to allow non-credentialed<br />
physicians to do the History <strong>and</strong> Physicals.<br />
Status<br />
Current interpretive guidelines require that a physician must be credentialed by a<br />
hospital in order to be able to do the history <strong>and</strong> physical which is required<br />
before a patient can have ambulatory surgery at that hospital. We will discuss<br />
this policy with CMS policy experts <strong>and</strong> appropriate specialty societies.<br />
We have discussed this issue with the American College <strong>of</strong> Surgeons <strong>and</strong> we<br />
July 15<br />
have a meeting about this issue with the American College <strong>of</strong> Physicians next<br />
week.<br />
Surgeons routinely provide focused H&Ps to their surgical patients as part <strong>of</strong> the<br />
September 29 preoperative services which are bundled into the payment for the surgery.<br />
Patients who have significant comorbid conditions may require a preoperative<br />
visit with an internist or subspecialist in which case that visit would be covered.<br />
It would be appropriate for the internist to perform a focused H&P <strong>and</strong> make<br />
recommendations concerning the management <strong>of</strong> the patient’s comorbid<br />
conditions during the preoperative period.<br />
Date Issue Created 12/01/2005<br />
LESION DESTRUCTION/EXCISION<br />
Coding the destruction or removal <strong>of</strong> skin lesions can be one <strong>of</strong> the most challenging <strong>coding</strong> processes<br />
faced by a biller. The anatomical site, number (<strong>and</strong> size, if necessary) <strong>of</strong> lesions involved, the type <strong>of</strong><br />
lesion (e.g., skin tag, benign or malignant), <strong>and</strong> method <strong>of</strong> removal must be identified to select the proper<br />
code(s).<br />
Paring or Cutting<br />
To report paring or cutting <strong>of</strong> benign hyperkeratotic lesions (e.g., corn or callus) see codes 11055-11057<br />
5-17<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
Note codes 11055-11057 are reported based on the number <strong>of</strong> lesions involved. Only one code would be<br />
used to describe the procedure based on the number <strong>of</strong> lesions pared or cut. For example, if the physician<br />
pared three (3) corns. The physician would report 11056. This code is to be used to report two to four<br />
lesions.<br />
Removal <strong>of</strong> Skin Tags<br />
Regardless <strong>of</strong> the method <strong>of</strong> removal (e.g., scissoring, sharp method, ligature strangulation,<br />
electrosurgical destruction, or combination <strong>of</strong> treatment modalities including chemical or<br />
electrocauterization <strong>of</strong> wound, with or without local anesthesia), codes 11200-11201 are used to report the<br />
service.<br />
Note these codes are based on the number <strong>of</strong> skin tags involved. Code 11201 is an add-on procedure that<br />
cannot be reported without 11200. Multiple surgical procedures rules do not apply to add-on codes. For<br />
example, 20 skin tags are removed.<br />
The service should be reported as:<br />
11200 1 unit<br />
11201 1 unit<br />
Shaving <strong>of</strong> Epidermal or Dermal Lesions<br />
According to CPT, Shaving is the sharp removal by transverse incision or horizontal slicing to remove<br />
epidermal <strong>and</strong> dermal lesions without a full-thickness dermal excision. This includes local anesthesia,<br />
chemical, or electrocauterization <strong>of</strong> the wound. The wound does not require suture closure.<br />
Physicians sometimes refer to this procedure as a shave biopsy. If the term shave biopsy is used, the coder<br />
needs to verify if the entire lesion was shaved (11300-11313) or if a piece <strong>of</strong> tissue was removed to be<br />
sent for pathology (11100 <strong>and</strong> 11101).<br />
The shaving codes (11300-11313) are defined by size <strong>and</strong> anatomical site. Each lesion removed by shave<br />
technique is coded separately. Multiple surgical procedure rules apply to these codes.<br />
Excision Benign Lesions<br />
Benign excision is defined as full-thickness (through the dermis) removal <strong>of</strong> lesions <strong>of</strong> the skin or<br />
subcutaneous tissue (e.g., cicatricial, fibrous, inflammatory, congenital, cystic lesions, etc.). Simple<br />
closure is included in the excision code; however, intermediate or complex closure may be reported<br />
separately for excised diameter greater than 0.5 cm. When both the excision <strong>and</strong> repair codes are reported,<br />
multiple surgical procedure rules apply.<br />
The excision <strong>of</strong> benign lesion codes (11400-11446) are defined by size (including margins) <strong>and</strong><br />
anatomical site. Each lesion excised is coded separately. Multiple surgical procedure rules apply to these<br />
codes.<br />
Excision <strong>of</strong> Malignant Lesions<br />
Malignant lesion excision is defined as full-thickness (through the dermis) removal <strong>of</strong> malignant lesions<br />
(pathology report available) <strong>of</strong> the skin or subcutaneous tissue. Closure by suture is required when using<br />
codes 11600-11646. Simple closure is included in the excision code; however, intermediate or complex<br />
closure may be reported separately. When both the excision <strong>and</strong> repair codes are reported, multiple<br />
surgical procedure rules apply.<br />
5-18<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
The excision <strong>of</strong> malignant lesion codes (11600-11646) are defined by size (including margins) <strong>and</strong><br />
anatomical site. Each lesion excised is coded separately. Multiple surgical procedure rules apply to these<br />
codes.<br />
Destruction<br />
According to CPT, Destruction means the ablation <strong>of</strong> benign, premalignant, or malignant tissues by any<br />
method, with or without curettement, including local anesthesia, <strong>and</strong> not usually requiring closure.<br />
Any method includes electrosurgery, cryosurgery, laser, <strong>and</strong> chemical treatment. Lesions include<br />
condylomata, papillomata, molluscum contagiosum, herpetic lesions, warts (i.e., common, plantar, flat),<br />
milia, or other benign, premalignant (e.g., actinic keratoses), or malignant lesions.<br />
Destruction Premalignant Lesions - Coding Change – Reporting Destruction <strong>of</strong> Benign or Premalignant<br />
Lesions<br />
Newby Note: Significant revisions in the descriptions for the following codes require<br />
adjustments <strong>of</strong> billing practices for the destruction <strong>of</strong> lesions. Be sure to update your<br />
superbill/charge ticket to reflect these changes.<br />
17000 Destruction (e.g., laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement),<br />
premalignant lesions [Emphasis Added] (e.g., actinic keratosis); first lesion<br />
17003 Destruction (e.g., laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement),<br />
premalignant lesions [Emphasis Added] (e.g., actinic keratosis); second through 14 lesions each<br />
(List separately in addition to code for first lesion)<br />
17004 Destruction (e.g., laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement),<br />
premalignant lesions [Emphasis Added] (e.g., actinic keratosis); 15 or more lesions<br />
Please note code 17004 is not an add-on code. If 15 or more lesions are destroyed on the same patient on<br />
the same day, only code 17004 is reported (codes 17000 <strong>and</strong> 17003 are bundled).<br />
Destruction Benign Lesions including Flat Wart, Molluscum Contagiosum, or Milia<br />
Codes 17110-17111 should be used to report the destruction <strong>of</strong> benign lesions, flat warts, molluscum<br />
contagiosum, or milia.<br />
17110 Destruction (e.g., laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement),<br />
benign lesions [Emphasis Added] other than skin tags or cutaneous vascular lesions; up to 14<br />
lesions<br />
17111 Destruction (e.g., laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement),<br />
benign lesions [Emphasis Added] other than skin tags or cutaneous vascular lesions; 15 or more<br />
lesions<br />
Destructions Malignant Lesions<br />
Codes 17260-17286 are used to report the destruction <strong>of</strong> malignant lesions (pathology report available).<br />
Note codes 17260-17286 are defined by size <strong>and</strong> anatomical site. Each lesion is coded separately.<br />
Multiple surgical procedure rules apply to these codes.<br />
ACTINIC KERATOSIS<br />
Medicare National Coverage Determinations Manual – Chapter 1, Part 4 - §250.4 - (Rev. 1, 10-01-03)<br />
CIM 35-101<br />
Actinic keratoses (AKs), also known as solar keratoses, are common, sun-induced skin lesions that are<br />
confined to the epidermis <strong>and</strong> have the potential to become a skin cancer.<br />
5-19<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
Various options exist for treating AKs. Clinicians should select an appropriate treatment based on the<br />
patient’s medical history, the lesion’s characteristics, <strong>and</strong> on the patient’s preference for a specific<br />
treatment. Commonly performed treatments for AKs include cryosurgery with liquid nitrogen, topical<br />
drug therapy, <strong>and</strong> curettage. Less commonly performed treatments for AK include dermabrasion,<br />
excision, chemical peels, laser therapy, <strong>and</strong> photodynamic therapy (PDT). An alternative approach to<br />
treating AKs is to observe the lesions over time <strong>and</strong> remove them only if they exhibit specific clinical<br />
features suggesting possible transformation to invasive squamous cell carcinoma (SCC).<br />
Medicare covers the destruction <strong>of</strong> actinic keratoses without restrictions based on lesion or patient<br />
characteristics.<br />
WOUND REPAIR (CLOSURE) - CPT/HCPCS Codes 12001-13300 <strong>and</strong> G0168<br />
These series <strong>of</strong> codes are used to describe laceration repair <strong>and</strong>, in limited situations, closure from a<br />
procedure. Wound closure includes repair by sutures, staples, or tissue adhesives (e.g., 2-cyanoacrylate),<br />
either singly or in combination with each other, or in combination with adhesive strips. Wound closure<br />
utilizing adhesive strips as the sole repair material should be coded using the appropriate E/M code. For<br />
Medicare claims when a wound is closed solely with tissue adhesive, physicians are instructed to use code<br />
G0168, wound closure utilizing tissue adhesive only. Repair (closure) <strong>of</strong> most surgical wounds is<br />
included in the allowance for the primary surgical procedure. However, for certain procedures, wound<br />
closure may be separately billed.<br />
Undermining the wound margins to permit closure is usually not separately billable using the<br />
intermediate or complex wound repair codes.<br />
When the wound repair codes 12001-13300 are used for closure <strong>of</strong> traumatic wounds, the CPT <strong>coding</strong><br />
guidelines should be followed.<br />
Codes 20100-20103 are used to report exploration <strong>and</strong> repair <strong>of</strong> trauma wounds requiring Enlargement,<br />
extension <strong>of</strong> dissection (to determine penetration), debridement, removal <strong>of</strong> foreign body(s), ligation or<br />
coagulation <strong>of</strong> minor subcutaneous <strong>and</strong>/or muscular blood vessel(s) <strong>of</strong> the subcutaneous tissue, muscle<br />
fascia, <strong>and</strong>/or muscle, not requiring thoracotomy or laparoscopy.<br />
Bundling Of Repair Codes Into Excision Of Benign Lesion Codes<br />
Payment for the excision <strong>of</strong> benign or malignant lesions <strong>of</strong> skin includes payment for simple repairs.<br />
Separate payment for simple repairs (CPT codes 12001-12018) will not be made when reported with the<br />
CPT codes for the excision <strong>of</strong> benign lesions (11400-11446) or the excision <strong>of</strong> malignant lesions<br />
(11600-11646).<br />
Medicare Bundling<br />
For Medicare claims, payment for the excision <strong>of</strong> benign lesions with an excised diameter <strong>of</strong> 0.5 cm or<br />
less (CPT 11400, 11420, <strong>and</strong> 11440) includes payment for simple, intermediate, or complex repairs. In<br />
other words, separate payment for simple, intermediate, or complex repairs (CPT 12001-12018) will not<br />
be made when reported with CPT codes 11400, 11420, <strong>and</strong> 11440.<br />
Carriers use existing definitions for simple, intermediate, <strong>and</strong> complex repairs listed in the American<br />
Medical Association's Physicians’ Current Procedural Terminology (CPT). For Medicare claims, payment<br />
for the excision <strong>of</strong> a benign lesion with an excised diameter greater than 0.5 cm or the excision <strong>of</strong> a<br />
malignant lesion <strong>of</strong> any size does not include payment for intermediate or complex repairs. Separate<br />
payment for medically necessary intermediate repairs (CPT codes 12031-12057) or medically necessary<br />
5-20<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
complex repairs (CPT codes 13100-13152) may be made when reported with CPT codes 11401-11406,<br />
11421-11426, 11441-11446, <strong>and</strong> 11600-11646.<br />
REMOVAL OF CERUMEN<br />
In collaboration with the American <strong>Academy</strong> <strong>of</strong> Otolaryngology-Head <strong>and</strong> Neck Surgery (AAO-HNS),<br />
the American Medical Association (AMA) included the following information in the July 2005 issue <strong>of</strong><br />
CPT Assistant. The intent <strong>of</strong> presenting the material is to provide some typical <strong>coding</strong> scenarios with<br />
regard to the appropriate use <strong>and</strong> application <strong>of</strong> CPT codes related to earwax removal e.g., 69210.<br />
These three scenarios represent frequent patient encounters related to the need for earwax removal:<br />
1. The patient presents to the <strong>of</strong>fice for the removal <strong>of</strong> “earwax” by the nurse via<br />
irrigation.<br />
2. The patient presents to the <strong>of</strong>fice for the removal <strong>of</strong> “earwax” by the primary care<br />
physician via irrigation or lavage.<br />
3. The patient presents to the <strong>of</strong>fice for “earwax” removal as the presenting complaint.<br />
This is described as impacted cerumen because it completely covers the eardrum <strong>and</strong><br />
the patient has hearing loss. The impacted cerumen is removed by the primary care<br />
physician or otolaryngologist with magnification provided by an otoscope or<br />
operating microscope <strong>and</strong> instruments such as wax curettes, forceps, <strong>and</strong> suction.<br />
The AMA states, “A major element in determining whether code 69210 should be<br />
reported is underst<strong>and</strong>ing the definition <strong>of</strong> impacted cerumen.” According to the AAO-<br />
HNS,<br />
If any one or more <strong>of</strong> the following are present, cerumen should be considered<br />
“impacted” clinically:<br />
• Visual considerations: Cerumen impairs exam <strong>of</strong> clinically significant portions <strong>of</strong><br />
the external auditory canal, tympanic membrane, or middle ear conditions.<br />
• Qualitative considerations: Extremely hard, dry, irritative cerumen causing<br />
symptoms such as pain, itching, hearing loss, etc<br />
• Inflammatory considerations: associated with foul odor, infection, or dermatitis<br />
• Quantitative considerations: Obstructive, copious cerumen that cannot be<br />
removed without magnification <strong>and</strong> multiple instruments requiring physician<br />
skills.”<br />
The article also includes:<br />
Removing wax that is not impacted does not warrant the <strong>reporting</strong> <strong>of</strong> CPT code<br />
69210. Rather, that work would appropriately be captured by an evaluation <strong>and</strong><br />
management (E/M) code regardless <strong>of</strong> how it is removed.<br />
If, however, the wax is truly impacted, then its removal should be reported with<br />
69210 if performed by a physician using at a minimum an otoscope <strong>and</strong><br />
instruments such as wax curettes, or in the case <strong>of</strong> many otolaryngologists, with<br />
an operating microscope <strong>and</strong> suction plus specific ear instruments (e.g., cup<br />
forceps, right angles).<br />
Accompanying documentation should indicate the time, effort, <strong>and</strong> equipment<br />
required to provide the service.<br />
5-21<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
Add-on code 69990, microsurgical techniques, requiring use <strong>of</strong> operating<br />
microscope (List separately in addition to code for primary procedure), should<br />
not be reported if the operating microscope is used for cerumen removal. In this<br />
latter instance, however, code 92504 binocular microscopy (separate diagnostic<br />
procedure), may be reported.<br />
Therefore, based on this information, Scenarios 1 <strong>and</strong> 2 above would not be<br />
reported with code 69210. These scenarios would be captured by the appropriate<br />
E/M code.<br />
Scenario 3, however, should be reported with code 69210 because both criteria<br />
were met; the patient had cerumen impaction <strong>and</strong> the removal required physician<br />
work using at least an otoscope <strong>and</strong> instrumentation rather than simple lavage.<br />
BURNS, LOCAL TREATMENT<br />
The following codes are used to report local treatment <strong>of</strong> burned surface only.<br />
CPT<br />
CODE<br />
STATUS OF<br />
PROBLEMS<br />
16000 Initial treatment, first degree burn, when not more than local treatment is required<br />
16020 Dressings <strong>and</strong>/or debridement <strong>of</strong> partial-thickness burns, initial or subsequent; small (less<br />
than 5% total body surface area)<br />
16025<br />
16030<br />
Dressings <strong>and</strong>/or debridement <strong>of</strong> partial-thickness burns, initial or subsequent; medium<br />
(e.g., whole face or whole extremity, or 5% to 10% total body surface area)<br />
Dressings <strong>and</strong>/or debridement <strong>of</strong> partial-thickness burns, initial or subsequent; large (e.g.,<br />
more than one extremity, or greater than 10% total body surface area<br />
SPRAINED FINGER(S)<br />
The following information was presented during the 2003 CPT Coding Symposium, November 14, 2002.<br />
Question: What is the correct code for buddy taping fingers, taping one finger to another for<br />
immobilizing a sprained finger<br />
Answer: Taping one finger to another for immobilizing a sprained finger is not reported<br />
separately, as it is considered a part <strong>of</strong> an Evaluation <strong>and</strong> Management (E/M) code.<br />
FRACTURE CARE<br />
If a physician treats a fracture <strong>and</strong> is responsible for the total fracture care, the appropriate fracture code<br />
would be reported based on the treatment provided.<br />
The fracture/dislocation treatment codes are generally reported by the physician responsible for the initial<br />
casting/strapping/splinting <strong>and</strong> follow-up care until the fracture/dislocation is healed. This is considered<br />
surgical treatment.<br />
When the physician provides a non-surgical treatment <strong>of</strong> the fracture/dislocation without the application<br />
<strong>of</strong> a brace, splint, or cast or without any follow-up care, the physician should only report the appropriate<br />
E/M codes based on the type <strong>of</strong> history, exam, <strong>and</strong> medical decision making required by the patient.<br />
5-22<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
HEMORRHOIDECTOMY BY SIMPLE LIGATURE<br />
Billing Excessive Units <strong>of</strong> Service for CPT 46221<br />
Recent data analysis <strong>and</strong> Medical Review findings for CPT 46221 (Hemorrhoidectomy, by simple<br />
ligature (e.g., rubber b<strong>and</strong>)) indicated a high error rate in the utilization <strong>of</strong> this code. Reviews revealed<br />
providers were billing CPT 46221 more than once per session for the same beneficiary.<br />
When billing CPT 46221, only one unit <strong>of</strong> service is reported regardless <strong>of</strong> the number <strong>of</strong> hemorrhoids<br />
ligated during the session. The October 1997 CPT Assistant article states "Each session <strong>of</strong> rubber b<strong>and</strong><br />
ligation, regardless <strong>of</strong> the number <strong>of</strong> hemorrhoids, is coded once."<br />
Please review your billing <strong>of</strong> CPT 46221 to determine any potential overpayments made to your practice.<br />
If you identify any overpayments, it is your responsibility to perform a voluntary refund to the Medicare<br />
Program.<br />
URETHRAL CATHETERIZATION<br />
Code 5170 describes catheterization <strong>of</strong> a patient for residual urine.<br />
Code 51702 describes insertion <strong>of</strong> Foley catheter for patients with chronic problems, such as<br />
neurogenic bladder <strong>and</strong> insertion <strong>of</strong> catheters in patients in acute retention in the hospital setting.<br />
Code 51703 describes a complicated insertion (e.g., altered anatomy, fractured catheter/balloon).<br />
Newby Note: Physicians should continue to use HCPCS code P9612, catheterization for<br />
collection <strong>of</strong> specimen, single patient, all places <strong>of</strong> service, when the patient is catheterized<br />
for a sterile urine specimen.<br />
GROUP PRACTICE DEFINED<br />
Medicare General Information, Eligibility, <strong>and</strong> Entitlement Chapter 5 §90.4 (Rev. 1, 09-11-02)<br />
A group practice is a group <strong>of</strong> two or more physicians <strong>and</strong> non-physician practitioners legally organized<br />
in a partnership, pr<strong>of</strong>essional corporation, foundation, not-for-pr<strong>of</strong>it corporation, faculty practice plan, or<br />
similar association:<br />
• In which each physician who is a member <strong>of</strong> the group provides substantially the full range <strong>of</strong><br />
services which the physician routinely provides (including medical care, consultation, diagnosis,<br />
or treatment) through the joint use <strong>of</strong> shared <strong>of</strong>fice space, facilities, equipment, <strong>and</strong> personnel<br />
• For which substantially all <strong>of</strong> the services <strong>of</strong> the physicians who are members <strong>of</strong> the group are<br />
provided through the group <strong>and</strong> are billed in the name <strong>of</strong> the group <strong>and</strong> amounts so received are<br />
treated as receipts <strong>of</strong> the group<br />
• In which the overhead expenses <strong>of</strong> <strong>and</strong> the income from the practice are distributed in accordance<br />
with methods previously determined by members <strong>of</strong> the group<br />
• Which meets such other st<strong>and</strong>ards as the Secretary may impose by regulation to implement<br />
§1877(h)(4) <strong>of</strong> the Social Security Act. The group practice definition also applies to health care<br />
practitioners.<br />
Physicians in Group Practice<br />
Medicare Claims Processing Manual Chapter 12 §30.6.5 (Rev. 1, 10-01-03)<br />
Physicians in the same group practice who are in the same specialty must bill <strong>and</strong> be paid as though they<br />
were a single physician. If more than one evaluation <strong>and</strong> management (face-to-face) service is provided<br />
on the same day to the same patient by the same physician or more than one physician in the same<br />
specialty in the same group, only one evaluation <strong>and</strong> management service may be reported unless the<br />
evaluation <strong>and</strong> management services are for unrelated problems. Instead <strong>of</strong> billing separately, the<br />
5-23<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
physicians should select a level <strong>of</strong> service representative <strong>of</strong> the combined visits <strong>and</strong> submit the<br />
appropriate code for that level.<br />
Physicians in the same group practice but who are in different specialties may bill <strong>and</strong> be paid without<br />
regard to their membership in the same group.<br />
EVALUATION AND MANAGEMENT (E/M) SERVICES FURNISHED INCIDENT TO<br />
PHYSICIAN’S SERVICE BY NONPHYSICIAN PRACTITIONERS<br />
Medicare Claims Processing Manual Chapter 12 §30.6.4 (Rev. 1, 10-01-03)<br />
When evaluation <strong>and</strong> management services are furnished incident to a physician’s service by a<br />
nonphysician practitioner, the physician may bill the CPT code that describes the evaluation <strong>and</strong><br />
management service furnished.<br />
When evaluation <strong>and</strong> management services are furnished incident to a physician’s service by a<br />
nonphysician employee <strong>of</strong> the physician, not as part <strong>of</strong> a physician service, the physician bills code 99211<br />
for the service.<br />
A physician is not precluded from billing under the “incident to” provision for services provided by<br />
employees whose services cannot be paid for directly under the Medicare Program. Employees <strong>of</strong> the<br />
physician may provide services incident to the physician’s service, but the physician alone is permitted to<br />
bill Medicare.<br />
Services provided by employees as “incident to” are covered when they meet all the requirements for<br />
incident to <strong>and</strong> are medically necessary for the individual needs <strong>of</strong> the patient.<br />
Split/Shared E/M Service<br />
Office/Clinic Setting<br />
In the <strong>of</strong>fice/clinic setting when the physician performs the E/M service the service must be reported<br />
using the physician’s UPIN/PIN. When an E/M service is a shared/split encounter between a physician<br />
<strong>and</strong> a non-physician practitioner (NP, PA, CNS, or CNM), the service is considered to have been<br />
performed “incident to” if the requirements for “incident to” are met <strong>and</strong> the patient is an established<br />
patient. If “incident to” requirements are not met for the shared/split E/M service, the service must be<br />
billed under the NPP’s UPIN/PIN, <strong>and</strong> payment will be made at the appropriate physician fee schedule<br />
payment.<br />
Hospital Inpatient/Outpatient/Emergency Department Setting<br />
When a hospital inpatient/hospital outpatient or emergency department E/M is shared between a<br />
physician <strong>and</strong> an NPP from the same group practice <strong>and</strong> the physician provides any face-to-face portion<br />
<strong>of</strong> the E/M encounter with the patient, the service may be billed under either the physician's or the NPP's<br />
UPIN/PIN number. However, if there was no face-to-face encounter between the patient <strong>and</strong> the<br />
physician (e.g., even if the physician participated in the service by reviewing the patient’s medical<br />
record), then the service may only be billed under the NPP's UPIN/PIN. Payment will be made at the<br />
appropriate physician fee schedule rate based on the UPIN/PIN entered on the claim.<br />
Examples <strong>of</strong> Shared Visits<br />
• If the NPP sees a hospital inpatient in the morning <strong>and</strong> the physician follows with a later face-t<strong>of</strong>ace<br />
visit with the patient on the same day, the physician or the NPP may report the service.<br />
• In an <strong>of</strong>fice setting the NPP performs a portion <strong>of</strong> an E/M encounter <strong>and</strong> the physician completes<br />
the E/M service. If the "incident to" requirements are met, the physician reports the service. If the<br />
“incident to” requirements are not met, the service must be reported using the NPP’s UPIN/PIN.<br />
5-24<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
Medicare “Incident to Clarification”<br />
Medicare Benefit Policy Manual - Chapter 15 – §60.1 - (Rev. 1, 10-01-03) - B3-2050.1<br />
Incident to a physician’s pr<strong>of</strong>essional services means that the services or supplies are furnished as an<br />
integral, although incidental, part <strong>of</strong> the physician’s personal pr<strong>of</strong>essional services in the course <strong>of</strong><br />
diagnosis or treatment <strong>of</strong> an injury or illness.<br />
Where a physician supervises auxiliary personnel to assist him/her in rendering services to patients <strong>and</strong><br />
includes the charges for their services in his/her own bills, the services <strong>of</strong> such personnel are considered<br />
incident to the physician’s service if there is a physician’s service rendered to which the services <strong>of</strong> such<br />
personnel are an incidental part <strong>and</strong> there is direct supervision by the physician.<br />
This does not mean, however, that to be considered incident to, each occasion <strong>of</strong> service by auxiliary<br />
personnel (or the furnishing <strong>of</strong> a supply) need also always be the occasion <strong>of</strong> the actual rendition <strong>of</strong> a<br />
personal pr<strong>of</strong>essional service by the physician. Such a service or supply could be considered to be<br />
incident to when furnished during a course <strong>of</strong> treatment where the physician performs an initial service<br />
[Emphasis added] <strong>and</strong> subsequent services <strong>of</strong> a frequency which reflect his/her active participation in <strong>and</strong><br />
management <strong>of</strong> the course <strong>of</strong> treatment. (However, the direct supervision requirement must still be met<br />
with respect to every nonphysician service.)<br />
Direct supervision in the <strong>of</strong>fice setting does not mean that the physician must be present in the same room<br />
with his or her aide. However, the physician must be present in the <strong>of</strong>fice suite <strong>and</strong> immediately available<br />
to provide assistance <strong>and</strong> direction throughout the time the aide is performing services.<br />
If auxiliary personnel perform services outside the <strong>of</strong>fice setting, e.g., in a patient’s home or in an<br />
institution (other than hospital or SNF), their services are covered incident to a physician’s service only if<br />
there is direct supervision by the physician. For example, if a nurse accompanied the physician on house<br />
calls <strong>and</strong> administered an injection, the nurse’s services are covered. If the same nurse made the calls<br />
alone <strong>and</strong> administered the injection, the services are not covered (even when billed by the physician)<br />
since the physician is not providing direct supervision. Services provided by auxiliary personnel in an<br />
institution (e.g., nursing, or convalescent home) present a special problem in determining whether direct<br />
physician supervision exists. The availability <strong>of</strong> the physician by telephone <strong>and</strong> the presence <strong>of</strong> the<br />
physician somewhere in the institution does not constitute direct supervision. For hospital patients <strong>and</strong> for<br />
SNF patients who are in a Medicare covered stay, there is no Medicare Part B coverage <strong>of</strong> the services <strong>of</strong><br />
physician-employed auxiliary personnel as services incident to physicians’ services under §1861(s)(2)(A)<br />
<strong>of</strong> the Act. Such services can be covered only under the hospital or SNF benefit <strong>and</strong> payment for such<br />
services can be made to only the hospital or SNF by a Medicare Intermediary.<br />
Services Of Nonphysician Personnel Furnished Incident To Physician’s Services<br />
Medicare Benefit Policy Manual - Chapter 15 – §60.2 - (Rev. 1, 10-01-03) - B3-2050.2<br />
In addition to coverage being available for the services <strong>of</strong> such auxiliary personnel as nurses, technicians,<br />
<strong>and</strong> therapists when furnished incident to the pr<strong>of</strong>essional services <strong>of</strong> a physician (as discussed in §60.1),<br />
a physician may also have the services <strong>of</strong> certain nonphysician practitioners covered as services incident<br />
to a physician’s pr<strong>of</strong>essional services. These nonphysician practitioners, who are being licensed by the<br />
States under various programs to assist or act in the place <strong>of</strong> the physician, include, for example, certified<br />
nurse midwives, clinical psychologists, clinical social workers, physician assistants, nurse practitioners,<br />
<strong>and</strong> clinical nurse specialists.<br />
Services performed by these nonphysician practitioners incident to a physician’s pr<strong>of</strong>essional services<br />
include not only services ordinarily rendered by a physician’s <strong>of</strong>fice staff person (e.g., medical services<br />
such as taking blood pressures <strong>and</strong> temperatures, giving injections, <strong>and</strong> changing dressings) but also<br />
5-25<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
services ordinarily performed by the physician such as minor surgery, setting casts or simple fractures,<br />
reading x-rays, <strong>and</strong> other activities that involve evaluation or treatment <strong>of</strong> a patient’s condition.<br />
Nonetheless, in order for services <strong>of</strong> a nonphysician practitioner to be covered as incident to the services<br />
<strong>of</strong> a physician, the services must meet all <strong>of</strong> the requirements for coverage specified in §§60 through 60.1.<br />
For example, the services must be an integral, although incidental, part <strong>of</strong> the physician’s personal<br />
pr<strong>of</strong>essional services, <strong>and</strong> they must be performed under the physician’s direct supervision.<br />
A nonphysician practitioner such as a physician assistant or a nurse practitioner may be licensed under<br />
State law to perform a specific medical procedure <strong>and</strong> may be able to perform the procedure without<br />
physician supervision <strong>and</strong> have the service separately covered <strong>and</strong> paid for by Medicare as a physician<br />
assistant’s or nurse practitioner’s service. However, in order to have that same service covered as incident<br />
to the services <strong>of</strong> a physician, it must be performed under the direct supervision <strong>of</strong> the physician as an<br />
integral part <strong>of</strong> the physician’s personal in-<strong>of</strong>fice service.<br />
As explained in §60.1, this does not mean that each occasion <strong>of</strong> an incidental service performed by a<br />
nonphysician practitioner must always be the occasion <strong>of</strong> a service actually rendered by the physician. It<br />
does mean that there must have been a direct, personal, pr<strong>of</strong>essional service furnished by the physician to<br />
initiate the course <strong>of</strong> treatment <strong>of</strong> which the service being performed by the nonphysician practitioner is<br />
an incidental part, <strong>and</strong> there must be subsequent services by the physician <strong>of</strong> a frequency that reflects the<br />
physician’s continuing active participation in <strong>and</strong> management <strong>of</strong> the course <strong>of</strong> treatment. In addition, the<br />
physician must be physically present in the same <strong>of</strong>fice suite <strong>and</strong> be immediately available to render<br />
assistance if that becomes necessary.<br />
Incident-To Services on Form CMS-1500<br />
Medicare Claims Processing Manual – Chapter 26 - §10.4 - Items 14-33 - Provider <strong>of</strong> Service or<br />
Supplier Information = (Rev. 1215, Issued: 03-30-07, Effective: 04-01-07, Implementation: 04-30-07)<br />
Item 17 When a service is incident to the service <strong>of</strong> a physician or non-physician practitioner, the<br />
name <strong>of</strong> the physician or non-physician practitioner who performs the initial service <strong>and</strong><br />
orders the non-physician service must appear in item 17;<br />
Item 17a Enter the ID qualifier 1G, followed by the CMS assigned UPIN <strong>of</strong> the referring/ordering<br />
physician listed in item 17. Under Medicare’s NPI contingency plan, the UPIN may be<br />
reported on the Form CMS-1500 <strong>and</strong> MUST be reported if an NPI is not available.<br />
Item 17b<br />
Item 24J<br />
Enter the NPI <strong>of</strong> the referring/ordering physician listed in item 17 as soon as it is available.<br />
During Medicare’s NPI contingency plan, enter the rendering provider’s PIN in the shaded<br />
portion. In the case <strong>of</strong> a service provided incident to the service <strong>of</strong> a physician or nonphysician<br />
practitioner, when the person who ordered the service is not supervising, enter the<br />
PIN <strong>of</strong> the supervisor in the shaded portion.<br />
Enter the rendering provider’s NPI number in the lower portion. In the case <strong>of</strong> a service<br />
provided incident to the service <strong>of</strong> a physician or non-physician practitioner, when the person<br />
who ordered the service is not supervising, enter the NPI <strong>of</strong> the supervisor in the lower<br />
portion.<br />
OFFICE/OUTPATIENT VISITS – CPT CODES 99201-99215<br />
A. Definition <strong>of</strong> New Patient for Selection <strong>of</strong> E/M Visit Code<br />
Interpret the phrase “new patient” to mean a patient who has not received any pr<strong>of</strong>essional services, i.e.,<br />
E/M service or other face-to-face service (e.g., surgical procedure) from the physician or physician group<br />
practice (same physician specialty) within the previous 3 years. For example, if a pr<strong>of</strong>essional component<br />
<strong>of</strong> a previous procedure is billed in a 3 year time period, e.g., a lab interpretation is billed <strong>and</strong> no E/M<br />
5-26<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
service or other face-to-face service with the patient is performed, then this patient remains a new patient<br />
for the initial visit. An interpretation <strong>of</strong> a diagnostic test, reading an x-ray or EKG etc., in the absence <strong>of</strong><br />
an E/M service or other face-to-face service with the patient does not affect the designation <strong>of</strong> a new<br />
patient.<br />
Newby Note: If more than one evaluation <strong>and</strong> management (face-to-face) service is<br />
provided on the same day to the same patient by the same physician or more than one<br />
physician in the same specialty in the same group, only one evaluation <strong>and</strong> management<br />
service may be reported unless the evaluation <strong>and</strong> management services are for unrelated<br />
problems. Instead <strong>of</strong> billing separately, the physician should select a level <strong>of</strong> service<br />
representative <strong>of</strong> the combined visits <strong>and</strong> submit the appropriate code for that level.<br />
Physicians in the same group practice but who are in different specialties may bill <strong>and</strong> be<br />
paid without regard to their membership in the same group.<br />
There is no difference if the group physicians are located in the same or different<br />
buildings. Therefore, even though a physician may be located on another campus, if a<br />
patient previously cared for by the same specialty physician in the same group within the<br />
previous three years is seen by a group physician <strong>of</strong> the same specialty at a setting apart<br />
from where his/her care is generally rendered <strong>and</strong> where his/her medical records may be<br />
located, for billing purposes, that patient remains an established patient for that same<br />
group, same specialty physician. It is the group’s responsibility to coordinate record<br />
keeping when different locations are involved.<br />
Changing Group Practices<br />
Dr. Smith leaves his/her practice in <strong>Indiana</strong>polis to join a new practice in Carmel. If Dr.<br />
Smith, or another physician <strong>of</strong> the same specialty in the Carmel practice, has not provided<br />
any pr<strong>of</strong>essional services to that patient within the past three years, then Dr. Smith would<br />
consider the patient a new patient. If Dr. Smith has rendered pr<strong>of</strong>essional services to the<br />
patient in either the <strong>Indiana</strong>polis or Carmel practice within the past three years, the<br />
patient is considered established to Dr. Smith. If Dr. Smith saw the patient in <strong>Indiana</strong>polis,<br />
but one <strong>of</strong> the Carmel physicians sees the patient, the patient would be considered new.<br />
B. Office/Outpatient E/M Visits Provided on Same Day for Unrelated Problems<br />
As for all other E/M services except where specifically noted, Carriers may not pay two E/M <strong>of</strong>fice visits<br />
billed by a physician (or physician <strong>of</strong> the same specialty from the same group practice) for the same<br />
beneficiary on the same day unless the physician documents that the visits were for unrelated problems in<br />
the <strong>of</strong>fice or outpatient setting which could not be provided during the same encounter (e.g., <strong>of</strong>fice visit<br />
for blood pressure medication evaluation, followed five hours later by a visit for evaluation <strong>of</strong> leg pain<br />
following an accident).<br />
C. Office/Outpatient or Emergency Department E/M Visit on Day <strong>of</strong> Admission to Nursing Facility<br />
Carriers may not pay a physician for an emergency department visit or an <strong>of</strong>fice visit <strong>and</strong> a<br />
comprehensive nursing facility assessment on the same day. Bundle E/M visits on the same date provided<br />
in sites other than the nursing facility into the initial nursing facility care code when performed on the<br />
same date as the nursing facility admission by the same physician.<br />
D. Drug Administration Services <strong>and</strong> E/M Visits Billed on Same Day <strong>of</strong> Service<br />
Carriers must advise physicians that CPT code 99211 cannot be paid if it is billed with a drug<br />
administration service such as a chemotherapy or nonchemotherapy drug infusion code (effective January<br />
1, 2004). This drug administration policy was exp<strong>and</strong>ed in the Physician Fee Schedule Final Rule,<br />
November 15, 2004, to also include a therapeutic or diagnostic injection code (effective January 1, 2005).<br />
Therefore, when a medically necessary, significant <strong>and</strong> separately identifiable E/M service (which meets<br />
a higher complexity level than CPT code 99211) is performed, in addition to one <strong>of</strong> these drug<br />
5-27<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
administration services, the appropriate E/M CPT code should be reported with modifier -25.<br />
Documentation should support the level <strong>of</strong> E/M service billed. For an E/M service provided on the same<br />
day, a different diagnosis is not required.<br />
99211 Most Abused Code<br />
Nationwide, 99211 is one <strong>of</strong> the most abused codes for usage. Code 99211 describes a service provided<br />
for minimal problems that may not require the presence <strong>of</strong> a physician, but does require the presence <strong>of</strong> a<br />
patient. As stated previously, this code cannot be billed if only an injection is given, without documented<br />
pertinent questioning or instructions. It cannot be billed for:<br />
• telephone calls,<br />
• venipunctures,<br />
• prescription renewals to a pharmacy,<br />
• telephone calls for a patient to reschedule an appointment, <strong>and</strong><br />
• telephone calls with the results <strong>of</strong> laboratory testing.<br />
Billing 99211 is not allowed for every patient who enters the <strong>of</strong>fice for a minimal service <strong>and</strong> receives an<br />
unnecessary pulse, temperature, or blood pressure recording.<br />
Prothrombin Time <strong>and</strong> Evaluation <strong>of</strong> Patient Anti-Coagulation Status - CPT Code 99211<br />
The following was developed from consultation among Medicare Part B Contractor Medical Directors<br />
<strong>and</strong> review <strong>of</strong> the CMS Frequently Asked Questions Web site. The CPT code description for 99211<br />
follows:<br />
Office or other outpatient visit for the evaluation <strong>and</strong> management <strong>of</strong> an established patient that<br />
may not require the presence <strong>of</strong> a physician. Usually, the presenting problem(s) are minimal.<br />
Typically, five minutes are spent performing or supervising these services.<br />
When a face-to-face medication management is provided by qualified <strong>of</strong>fice staff on the same date <strong>of</strong> the<br />
laboratory test, the physician may bill CPT code 99211 if the services are medically necessary <strong>and</strong><br />
constitute a distinct, separately identifiable evaluation <strong>and</strong> management (E/M) service that is consistent<br />
with the criteria for a low-level <strong>of</strong>fice visit. The following describes adequate documentation for CPT<br />
code 99211 when billed for an evaluation <strong>of</strong> a chronically anti-coagulated patient for whom a<br />
prothrombin time has been drawn <strong>and</strong> determined.<br />
Reason for the visit - A physician visit is not routinely necessary in order to draw blood for prothrombin<br />
time or other laboratory tests. Therefore, the documentation for 99211 or any other E/M code in this<br />
circumstance must demonstrate a need for clinical evaluation <strong>and</strong> management. In this case, services that<br />
would serve to demonstrate that evaluation <strong>and</strong> management were performed include evaluation <strong>of</strong><br />
significant new symptoms (such as excessive bruising or hemorrhage). Alternatively, for patients who<br />
have no new clinical concerns, demonstrating how the relevant laboratory information obtained was used<br />
to modify therapy will document that a separately payable E/M service has been performed.<br />
• Current medications listed (with notation <strong>of</strong> level <strong>of</strong> compliance)<br />
• Indication <strong>of</strong> physician’s evaluation <strong>of</strong> the information about signs/symptoms <strong>and</strong> laboratory test<br />
result <strong>and</strong> his or her management recommendation<br />
• Identity <strong>and</strong> credentials <strong>of</strong> provider(s) as listed in text above<br />
If the patient does not have any new symptoms or requires a change in the dosage <strong>of</strong> his/her medication,<br />
the physician cannot report 99211.<br />
5-28<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
HOSPITAL OBSERVATION SERVICES – CPT CODES 99217-99220<br />
Medicare Claims Processing Manual Chapter 12 §30.6.8 (Codes 99217 99220) (Rev. 1, 10-01-03) B3-<br />
15504<br />
A. Who May Bill Initial Observation Care<br />
Carriers pay for initial observation care billed by only the physician who admitted the patient to hospital<br />
observation <strong>and</strong> was responsible for the patient during his/her stay in observation. A physician who does<br />
not have inpatient admitting privileges but who is authorized to admit a patient to observation status may<br />
bill these codes.<br />
For a physician to bill the initial observation care codes, there must be a medical observation record for<br />
the patient which contains dated <strong>and</strong> timed physician’s admitting orders regarding the care the patient is<br />
to receive while in observation, nursing notes, <strong>and</strong> progress notes prepared by the physician while the<br />
patient was in observation status. This record must be in addition to any record prepared as a result <strong>of</strong> an<br />
emergency department or outpatient clinic encounter.<br />
Payment for an initial observation care code is for all the care rendered by the admitting physician on the<br />
date the patient was admitted to observation. All other physicians who see the patient while he or she is in<br />
observation must bill the <strong>of</strong>fice <strong>and</strong> other outpatient service codes or outpatient consultation codes as<br />
appropriate when they provide services to the patient.<br />
For example, if an internist admits a patient to observation <strong>and</strong> asks an allergist for a consultation on the<br />
patient’s condition, only the internist may bill the initial observation care code. The allergist must bill<br />
using the outpatient consultation code that best represents the services he or she provided. The allergist<br />
cannot bill an inpatient consultation since the patient was not a hospital inpatient.<br />
B. Physician Billing for Observation Care Following Admission to Observation<br />
If the patient is discharged on the same date as admission to observation, Carriers pay only the initial<br />
observation care code because that code represents a full day <strong>of</strong> care.<br />
If the patient remains in observation after the first date following the admission to observation, it is<br />
expected that the patient would be discharged on that second calendar date. The physician bills CPT code<br />
99217 for observation care discharge services provided on the second date.<br />
In the rare circumstance when a patient is held in observation status for more than two calendar dates, the<br />
physician must bill subsequent services furnished before the date <strong>of</strong> discharge using the outpatient/<strong>of</strong>fice<br />
visit codes. The physician may not use the subsequent hospital care codes since the patient is not an<br />
inpatient <strong>of</strong> the hospital.<br />
C. Admission to Inpatient Status from Observation<br />
If the same physician who admitted a patient to observation status also admits the patient to inpatient<br />
status from observation before the end <strong>of</strong> the date on which the patient was admitted to observation, pay<br />
only an initial hospital visit for the evaluation <strong>and</strong> management services provided on that date. Medicare<br />
payment for the initial hospital visit includes all services provided to the patient on the date <strong>of</strong> admission<br />
by that physician, regardless <strong>of</strong> the site <strong>of</strong> service. The physician may not bill an initial observation care<br />
code for services on the date that he or she admits the patient to inpatient status. If the patient is admitted<br />
to inpatient status from observation subsequent to the date <strong>of</strong> admission to observation, the physician<br />
must bill an initial hospital visit for the services provided on that date. The physician may not bill the<br />
hospital observation discharge management code (code 99217) or an outpatient/<strong>of</strong>fice visit for the care<br />
provided in observation on the date <strong>of</strong> admission to inpatient status.<br />
5-29<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
OBSERVATION OR INPATIENT CARE SERVICES – INCLUDING ADMISSION AND<br />
DISCHARGE SERVICES - CPT CODES 99234-99236<br />
This series <strong>of</strong> codes is used to report observation or inpatient hospital care services provided to patients<br />
admitted <strong>and</strong> discharged on the same date <strong>of</strong> service. In order to use these codes for a Medicare patient,<br />
the patient must have been an inpatient or an observation care patient for a minimum <strong>of</strong> eight (8) hours on<br />
the same calendar date.<br />
When observation status or initial inpatient hospital care is initiated in the course <strong>of</strong> an encounter in<br />
another site <strong>of</strong> service (e.g., hospital emergency department, physician’s <strong>of</strong>fice, nursing facility) all<br />
evaluation <strong>and</strong> management services provided by the supervising physician in conjunction with initiating<br />
observation status are considered part <strong>of</strong> the initial observation care or initial inpatient hospital care when<br />
performed on the same date. The level <strong>of</strong> service should include the services related to the admission<br />
provided in the other sites-<strong>of</strong>-service as well as in the observation setting when provided by the same<br />
physician.<br />
Newby Note: To use codes 99234-99236, the physician must clearly indicate in the<br />
patient’s medical record the number <strong>of</strong> hours the patient was in observation or inpatient<br />
status.<br />
For patients admitted to observation or inpatient care for less than eight (8) hours or discharged on a<br />
different date, see codes 99218-99220 <strong>and</strong> 99217, or 99221-99223 <strong>and</strong> 99238-99239.<br />
INPATIENT HOSPITAL VISITS – CPT CODES 99221-99239<br />
Medicare Claims Processing Manual Chapter 12 §30.6.9 General (Codes 99221-99239) (Rev. 1, 10-01-<br />
03) B3-15505-15505.2<br />
A. Hospital Visit <strong>and</strong> Critical Care on Same Day<br />
If critical care is required upon the patient’s presentation to the emergency department, only critical care<br />
codes 99291-99292 may be reported. Emergency department codes will not be paid for the same day. If<br />
there is a hospital or <strong>of</strong>fice/outpatient evaluation <strong>and</strong> management service furnished early in the day <strong>and</strong><br />
at that time the patient does not require critical care, but the patient requires critical care later in the day,<br />
both critical care <strong>and</strong> the evaluation <strong>and</strong> management service may be paid.<br />
Physicians must submit supporting documentation when critical care is billed on the same day as other<br />
evaluation <strong>and</strong> management services.<br />
B. Two Hospital Visits Same Day<br />
Carriers pay a physician for only one hospital visit per day for the same patient, whether the problems<br />
seen during the encounters are related or not. The inpatient hospital visit descriptors contain the phrase<br />
per day which means that the code <strong>and</strong> the payment established for the code represent all services<br />
provided on that date. The physician should select a code that reflects all services provided during the<br />
date <strong>of</strong> the service.<br />
C. Hospital Visits Same Day But by Different Physicians<br />
In a hospital inpatient situation involving one physician covering for another, if physician A sees the<br />
patient in the morning <strong>and</strong> physician B, who is covering for A, sees the same patient in the evening,<br />
Carriers do not pay physician B for the second visit. The hospital visit descriptors include the phrase per<br />
day meaning care for the day.<br />
5-30<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
If the physicians are each responsible for a different aspect <strong>of</strong> the patient’s care, pay both visits if the<br />
physicians are in different specialties <strong>and</strong> the visits are billed with different diagnoses. There are<br />
circumstances where concurrent care may be billed by physicians <strong>of</strong> the same specialty.<br />
D. Visits to Patients in Swing Beds<br />
If the inpatient care is being billed by the hospital as inpatient hospital care, the hospital care codes apply.<br />
If the inpatient care is being billed by the hospital as nursing facility care, then the nursing facility codes<br />
apply.<br />
Payment for Initial Hospital Care Services<br />
Medicare Claims Processing Manual Chapter 12 §30.6.9.1 (Codes 99221-99223) (Rev. 1, 10-01-03)<br />
A. Initial Hospital Care from Emergency Room<br />
Carriers pay for an initial hospital care service or an initial inpatient consultation if a physician sees<br />
his/her patient in the emergency room <strong>and</strong> decides to admit the person to the hospital. They do not pay for<br />
both E/M services. Also, they do not pay for an emergency department visit by the same physician on the<br />
same date <strong>of</strong> service. When the patient is admitted to the hospital via another site <strong>of</strong> service (e.g., hospital<br />
emergency department, physician’s <strong>of</strong>fice, nursing facility), all services provided by the physician in<br />
conjunction with that admission are considered part <strong>of</strong> the initial hospital care when performed on the<br />
same date as the admission.<br />
B. Initial Hospital Care on Day Following Visit<br />
Carriers pay both visits if a patient is seen in the <strong>of</strong>fice on one date <strong>and</strong> admitted to the hospital on the<br />
next date, even if fewer than 24 hours has elapsed between the visit <strong>and</strong> the admission.<br />
C. Initial Hospital Care <strong>and</strong> Discharge on Same Day<br />
Carriers pay only the initial hospital care code when a patient is admitted as an inpatient <strong>and</strong> discharged<br />
on the same day. They do not pay the hospital discharge management code on the date <strong>of</strong> admission.<br />
Newby Note: If the patient is admitted <strong>and</strong> discharged on the same date <strong>of</strong> service <strong>and</strong> the<br />
patient has been an inpatient for eight (8) or more hours, the physician may use code<br />
99234-99236.<br />
D. Physician Services Involving Transfer From One Hospital to Another; Transfer Within Facility to<br />
Prospective Payment System (PPS) Exempt Unit <strong>of</strong> Hospital; Transfer From One Facility to Another<br />
Separate Entity Under Same Ownership <strong>and</strong>/or Part <strong>of</strong> Same Complex; or Transfer From One<br />
Department to Another Within Single Facility<br />
Physicians may bill both the hospital discharge management code <strong>and</strong> an initial hospital care code when<br />
the discharge <strong>and</strong> admission do not occur on the same day if the transfer is between:<br />
• Different hospitals;<br />
• Different facilities under common ownership which do not have merged records; or<br />
• Between the acute care hospital <strong>and</strong> a PPS exempt unit within the same hospital when there are<br />
no merged records.<br />
In all other transfer circumstances, the physician should bill only the appropriate level <strong>of</strong> subsequent<br />
hospital care for the date <strong>of</strong> transfer.<br />
E. Initial Hospital Care Service History <strong>and</strong> Physical That Is Less Than Comprehensive<br />
When a physician performs a visit or consultation that meets the definition <strong>of</strong> a Level 5 <strong>of</strong>fice visit or<br />
consultation several days prior to an admission <strong>and</strong> on the day <strong>of</strong> admission performs less than a<br />
comprehensive history <strong>and</strong> physical, he or she should report the <strong>of</strong>fice visit or consultation that reflects<br />
5-31<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
the services furnished <strong>and</strong> also report the lowest level initial hospital care code (i.e., code 99221) for the<br />
initial hospital admission. Carriers pay the <strong>of</strong>fice visit as billed <strong>and</strong> the Level 1 initial hospital care code.<br />
F. Initial Hospital Care Visits by Two Different M.D.s or D.O.s When They Are Involved in Same<br />
Admission<br />
Physicians use the initial hospital care codes (codes 99221-99223) to report the first hospital inpatient<br />
encounter with the patient when he or she is the admitting physician.<br />
Carriers consider only one M.D. or D.O. to be the admitting physician <strong>and</strong> permit only the admitting<br />
physician to use the initial hospital care codes. Physicians that participate in the care <strong>of</strong> a patient but are<br />
not the admitting physician <strong>of</strong> record should bill the inpatient evaluation <strong>and</strong> management services codes<br />
that describe their participation in the patient’s care (i.e., subsequent hospital visit or inpatient<br />
consultation).<br />
G. Initial Hospital Care <strong>and</strong> Nursing Facility Visit on Same Day<br />
Carriers pay only the initial hospital care code if the patient is admitted to a hospital following a nursing<br />
facility visit on the same date by the same physician. Payment for the initial hospital care service includes<br />
all work performed by the physician in all sites <strong>of</strong> service on that date.<br />
Subsequent Hospital Visit <strong>and</strong> Hospital Discharge Management<br />
Medicare Claims Processing Manual Chapter 12 §30.6.9.2 (Codes 99231-99239) (Rev. 1, 10-01-03)<br />
A. Subsequent Hospital Visit <strong>and</strong> Discharge Management on Same Day<br />
Carriers only pay the hospital discharge management code on the day <strong>of</strong> discharge (unless it is also the<br />
day <strong>of</strong> admission, in which case, the admission service <strong>and</strong> not the discharge management service is<br />
billed). Carriers do not pay both a subsequent hospital visit in addition to hospital discharge day<br />
management service on the same day by the same physician.<br />
B. Hospital Discharge Management (CPT Codes 99238 <strong>and</strong> 99239) <strong>and</strong> Nursing Facility Admission<br />
Code When Patient Is Discharged From Hospital <strong>and</strong> Admitted to Nursing Facility on Same Day<br />
Carriers pay the hospital discharge code (codes 99238 or 99239) in addition to a nursing facility<br />
admission code when they are billed by the same physician with the same date <strong>of</strong> service.<br />
Face-to-Face Visit Required for Discharge Services<br />
All E/M services except where specifically stated (e.g., care plan oversight which is a monthly summary)<br />
require a face-to-face interaction between the physician <strong>and</strong> the patient. The discharge service is a face-t<strong>of</strong>ace<br />
E/M service.<br />
Carriers monitoring for the time period April 2004 through March 2005, the date <strong>of</strong> service (DOS) <strong>of</strong><br />
seven (7) to fifteen (15) percent <strong>of</strong> the discharge service codes (99238, 99239, 99315, <strong>and</strong> 99316)<br />
submitted were the same as the date <strong>of</strong> death <strong>of</strong> the patient.<br />
CMS provided the following information regarding the use <strong>of</strong> time-based codes:<br />
The discharge day management service by definition does not have the elements <strong>of</strong> history,<br />
physical examination, <strong>and</strong> medical decision-making, as many <strong>of</strong> the other E/M codes have. The<br />
provider uses this final visit as appropriate, for a final examination, discussion <strong>of</strong> problems,<br />
instructions, <strong>and</strong> follow-up. A provider may choose to bill a subsequent hospital visit service code<br />
instead <strong>of</strong> a discharge service code. The provider is not required to bill a discharge day<br />
management service.<br />
The discharge day management service is a time-based service. In order to support services that<br />
require greater than 30 minutes (codes 99239 <strong>and</strong> 99316) the total time spent must be<br />
5-32<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
documented. If the time is not documented, payment is allowed for the lower level services<br />
(99238 <strong>and</strong> 99315).<br />
A discharge day management service can be split/shared between the nonphysician practitioner<br />
(NPP) <strong>and</strong> physician. When the service is shared between a physician <strong>and</strong> an NPP from the same<br />
group practice <strong>and</strong> the physician provides any face-to-face portion <strong>of</strong> the E/M encounter with the<br />
patient, the service may be billed under either the physician’s or the NPP’s UPIN/PIN number.<br />
However, if there was no face-to-face encounter between the patient <strong>and</strong> the physician (e.g., even<br />
if the physician participated in the service by reviewing the patient’s medical record), the service<br />
must be billed under the NPP’s rendering provider number (PIN).<br />
Medicare will pay for pronouncement <strong>of</strong> death as long as the provider actually does the<br />
pronouncement face-to-face with the deceased patient (not over the telephone). There must be<br />
documentation supporting a face-to-face encounter when billing a discharge service on the date <strong>of</strong><br />
death. If the provider does not see the patient prior to the time <strong>of</strong> death or make the<br />
pronouncement <strong>of</strong> death face-to-face, no E/M service may be billed for that date <strong>of</strong> service.<br />
Medicare Certified Swing Bed Hospital Services<br />
MLN Matters Number: SE0606<br />
Under the Social Security Act (§1883(a)(1), [42 U.S.C. 1395tt]), any hospital that has an agreement under<br />
§1866 may enter into an agreement with CMS in which its inpatient hospital facilities may be used for<br />
furnishing types <strong>of</strong> service that, if furnished in a Skilled Nursing Facility (SNF), would constitute<br />
extended care services (subject to §1883(b)). Such a hospital is known as a swing bed hospital.<br />
Services Covered in a Medicare Certified Swing Bed<br />
Under the Social Security Act, Section 1883(a)(1), payment for swing bed services will be made only for<br />
services for which payment would be made as post-hospital extended care services if those services had<br />
been furnished by an SNF<br />
CONSULTATIONS – CPT CODES 99241-99255<br />
Medicare Claims Processing Manual – Chapter 12 §30.6.10 (Codes 99241 99275) (Rev. 1, 10-01-03) B3-<br />
15506 (Rev. 782, Issued 12-16-05 Effective 01-01-06 Implementation 01-17-06)<br />
A. Consultation Services versus Other Evaluation <strong>and</strong> Management (E/M) Visits<br />
Carriers pay for a reasonable <strong>and</strong> medically necessary consultation service when all <strong>of</strong> the following<br />
criteria for the use <strong>of</strong> a consultation code are met:<br />
• Specifically, a consultation service is distinguished from other evaluation <strong>and</strong> management (E/M)<br />
visits because it is provided by a physician or qualified nonphysician practitioner (NPP) whose<br />
opinion or advice regarding evaluation <strong>and</strong>/or management <strong>of</strong> a specific problem is requested by<br />
another physician or other appropriate source. The qualified NPP may perform consultation<br />
services within the scope <strong>of</strong> practice <strong>and</strong> licensure requirements for NPPs in the State in which<br />
he/she practices. Applicable collaboration <strong>and</strong> general supervision rules apply as well as billing<br />
rules;<br />
• A request for a consultation from an appropriate source <strong>and</strong> the need for consultation (i.e., the<br />
reason for a consultation service) shall be documented by the consultant in the patient’s medical<br />
record <strong>and</strong> included in the requesting physician or qualified NPP’s plan <strong>of</strong> care in the patient’s<br />
medical record; <strong>and</strong><br />
• After the consultation is provided, the consultant shall prepare a written report <strong>of</strong> his/her findings<br />
<strong>and</strong> recommendations, which shall be provided to the referring physician.<br />
5-33<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
The intent <strong>of</strong> a consultation service is that a physician or qualified NPP or other appropriate source is<br />
asking another physician or qualified NPP for advice, opinion, a recommendation, suggestion, direction,<br />
or counsel, etc. in evaluating or treating a patient because that individual has expertise in a specific<br />
medical area beyond the requesting pr<strong>of</strong>essional’s knowledge. Consultations may be billed based on time<br />
if the counseling/coordination <strong>of</strong> care constitutes more than 50 percent <strong>of</strong> the face-to-face encounter<br />
between the physician or qualified NPP <strong>and</strong> the patient. The preceding requirements (request, evaluation<br />
(or counseling/coordination) <strong>and</strong> written report) shall also be met when the consultation is based on time<br />
for counseling/coordination.<br />
A consultation shall not be performed as a split/shared E/M visit.<br />
B. Consultation Followed by Treatment<br />
A physician or qualified NPP consultant may initiate diagnostic services <strong>and</strong> treatment at the initial<br />
consultation service or subsequent visit. Ongoing management, following the initial consultation service<br />
by the consultant physician, shall not be reported with consultation service codes. These services shall be<br />
reported as subsequent visits for the appropriate place <strong>of</strong> service <strong>and</strong> level <strong>of</strong> service. Payment for a<br />
consultation service shall be made regardless <strong>of</strong> treatment initiation unless a transfer <strong>of</strong> care occurs.<br />
Transfer <strong>of</strong> Care<br />
A transfer <strong>of</strong> care occurs when a physician or qualified NPP requests that another physician or qualified<br />
NPP take over the responsibility for managing the patients’ complete care for the condition <strong>and</strong> does not<br />
expect to continue treating or caring for the patient for that condition.<br />
When this transfer is arranged, the requesting physician or qualified NPP is not asking for an opinion or<br />
advice to personally treat this patient <strong>and</strong> is not expecting to continue treating the patient for the<br />
condition. The receiving physician or qualified NPP shall document this transfer <strong>of</strong> the patient’s care, to<br />
his/her service, in the patient’s medical record or plan <strong>of</strong> care.<br />
In a transfer <strong>of</strong> care, the receiving physician or qualified NPP would report the appropriate new or<br />
established patient visit code according to the place <strong>of</strong> service <strong>and</strong> level <strong>of</strong> service performed <strong>and</strong> shall<br />
not report a consultation service.<br />
C. Initial <strong>and</strong> Follow-Up Consultation Services<br />
Initial Consultation Service<br />
In the hospital setting, the consulting physician or qualified NPP shall use the appropriate Initial Inpatient<br />
Consultation codes (99251 – 99255) for the initial consultation service. In the nursing facility setting, the<br />
consulting physician or qualified NPP shall use the appropriate Initial Inpatient Consultation codes<br />
(99251 – 99255) for the initial consultation service. The Initial Inpatient Consultation may be reported<br />
only once per consultant per patient per facility admission.<br />
In the <strong>of</strong>fice or other outpatient setting, the consulting physician, or qualified NPP shall use the<br />
appropriate Office or Other Outpatient Consultation (new or established patient) codes (99241 – 99245)<br />
for the initial consultation service.<br />
If an additional request for an opinion or advice, regarding the same or a new problem with the same<br />
patient, is received from the same or another physician or qualified NPP <strong>and</strong> documented in the medical<br />
record, the Office or Other Outpatient Consultation (new or established patient) codes (99241 – 99245)<br />
may be used again. However, if the consultant continues to care for the patient for the original condition<br />
following his/her initial consultation, repeat consultation services shall not be reported by this physician<br />
or qualified NPP during his/her ongoing management <strong>of</strong> this condition.<br />
5-34<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
Follow-Up Consultation Service<br />
Effective January 1, 2006, the follow-up inpatient consultation codes (99261 – 99263) are deleted.<br />
In the hospital setting, following the initial consultation service, the Subsequent Hospital Care codes<br />
(99231 – 99233) shall be reported for additional follow-up visits.<br />
In the nursing facility setting, following the initial consultation service, the Subsequent Nursing Facility<br />
(NF) Care codes (new CPT codes 99307 – 99310) shall be reported for additional follow-up visits.<br />
Effective January 1, 2006, CPT codes 99311 – 99313 are deleted <strong>and</strong> not valid for Subsequent NF visits.<br />
In the <strong>of</strong>fice or other outpatient setting, following the initial consultation service, the Office or Other<br />
Outpatient Established Patient codes (99212 – 99215) shall be reported for additional follow-up visits.<br />
The CPT code 99211 shall not be reported as a consultation service. The CPT code 99211 is not included<br />
by Medicare for a consultation service since this service typically does not require the presence <strong>of</strong> a<br />
physician or qualified NPP <strong>and</strong> would not meet the consultation service criteria.<br />
D. Second Opinion E/M Service Requests<br />
Effective January 1, 2006, the Confirmatory Consultation codes (99271 – 99275) are deleted.<br />
A second opinion E/M service is a request by the patient <strong>and</strong>/or family or m<strong>and</strong>ated (e.g., by a third-party<br />
payer) <strong>and</strong> is not requested by a physician or qualified NPP. A consultation service requested by a<br />
physician, qualified NPP or other appropriate source that meets the requirements stated in Section A shall<br />
be reported using the initial consultation service codes as discussed in Section C. A written report is not<br />
required by Medicare to be sent to a physician when an evaluation for a second opinion has been<br />
requested by the patient <strong>and</strong>/or family.<br />
A second opinion, for Medicare purposes, is generally performed as a request for a second or third<br />
opinion <strong>of</strong> a previously recommended medical treatment or surgical procedure. A second opinion E/M<br />
service initiated by a patient <strong>and</strong>/or family is not reported using the consultation codes.<br />
In both the inpatient hospital setting <strong>and</strong> the NF setting, a request for a second opinion would be made<br />
through the attending physician or physician <strong>of</strong> record. If an initial consultation is requested <strong>of</strong> another<br />
physician or qualified NPP by the attending physician <strong>and</strong> meets the requirements for a consultation<br />
service (as identified in Section A) then the appropriate Initial Inpatient Consultation code shall be<br />
reported by the consultant. If the service does not meet the consultation requirements, then the E/M<br />
service shall be reported using the Subsequent Hospital Care codes (99231 – 99233) in the inpatient<br />
hospital setting <strong>and</strong> the Subsequent NF Care codes (99307 – 99310) in the NF setting.<br />
A second opinion E/M service performed in the <strong>of</strong>fice or other outpatient setting shall be reported using<br />
the Office or Other Outpatient new patient codes (99201 – 99205) for a new patient <strong>and</strong> established<br />
patient codes (99212 – 99215) for an established patient, as appropriate. The 3 year rule regarding “new<br />
patient” status applies. Any medically necessary follow-up visits shall be reported using the appropriate<br />
subsequent visit/established patient E/M visit codes.<br />
The CPT modifier -32 (M<strong>and</strong>ated Services) is not recognized as a payment modifier in Medicare. A<br />
second opinion evaluation service to satisfy a requirement for a third party payer is not a covered service<br />
in Medicare.<br />
E. Consultations Requested by Members <strong>of</strong> Same Group<br />
Carriers pay for a consultation if one physician or qualified NPP in a group practice requests a<br />
consultation from another physician in the same group practice when the consulting physician or qualified<br />
5-35<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
NPP has expertise in a specific medical area beyond the requesting pr<strong>of</strong>essional’s knowledge. A<br />
consultation service shall not be reported on every patient as a routine practice between physicians <strong>and</strong><br />
qualified NPPs within a group practice setting.<br />
F. Documentation for Consultation Services<br />
Consultation Request<br />
• A written request for a consultation from an appropriate source <strong>and</strong> the need for a consultation<br />
must be documented in the patient’s medical record. The initial request may be a verbal<br />
interaction between the requesting physician <strong>and</strong> the consulting physician; however, the verbal<br />
conversation shall be documented in the patient’s medical record, indicating a request for a<br />
consultation service was made by the requesting physician or qualified NPP.<br />
• The reason for the consultation service shall be documented by the consultant (physician or<br />
qualified NPP) in the patient’s medical record <strong>and</strong> included in the requesting physician or<br />
qualified NPP’s plan <strong>of</strong> care. The consultation service request may be written on a physician<br />
order form by the requestor in a shared medical record.<br />
Consultation Report<br />
• A written report shall be furnished to the requesting physician or qualified NPP.<br />
In an emergency department or an inpatient or outpatient setting in which the medical record is shared<br />
between the referring physician or qualified NPP <strong>and</strong> the consultant, the request may be documented as<br />
part <strong>of</strong> a plan written in the requesting physician or qualified NPP’s progress note, an order in the medical<br />
record, or a specific written request for the consultation. In these settings, the report may consist <strong>of</strong> an<br />
appropriate entry in the common medical record.<br />
In an <strong>of</strong>fice setting, the documentation requirement may be met by a specific written request for the<br />
consultation from the requesting physician or qualified NPP or if the consultant’s records show a specific<br />
reference to the request. In this setting, the consultation report is a separate document communicated to<br />
the requesting physician or qualified NPP.<br />
In a large group practice, e.g., an academic department or a large multi-specialty group, in which there is<br />
<strong>of</strong>ten a shared medical record, it is acceptable to include the consultant’s report in the medical record<br />
documentation <strong>and</strong> not require a separate letter from the consulting physician or qualified NPP to the<br />
requesting physician or qualified NPP. The written request <strong>and</strong> the consultation evaluation, findings <strong>and</strong><br />
recommendations shall be available in the consultation report.<br />
G. Consultation for Preoperative Clearance<br />
Preoperative consultations are payable for new or established patients performed by any physician or<br />
qualified NPP at the request <strong>of</strong> a surgeon, as long as all <strong>of</strong> the requirements for performing <strong>and</strong> <strong>reporting</strong><br />
the consultation codes are met <strong>and</strong> the service is medically necessary <strong>and</strong> not routine screening.<br />
H. Postoperative Care by Physician Who Did Preoperative Clearance Consultation<br />
If subsequent to the completion <strong>of</strong> a preoperative consultation in the <strong>of</strong>fice or hospital, the consultant<br />
assumes responsibility for the management <strong>of</strong> a portion or all <strong>of</strong> the patient’s condition(s) during the<br />
postoperative period, the consultation codes should not be used postoperatively. In the hospital setting,<br />
the physician or qualified NPP who has performed a preoperative consultation <strong>and</strong> assumes responsibility<br />
for the management <strong>of</strong> a portion or all <strong>of</strong> the patient’s condition(s) during the postoperative period should<br />
use the appropriate subsequent hospital care codes to bill for the concurrent care he or she is providing. In<br />
the <strong>of</strong>fice setting, the appropriate established patient visit codes should be used during the postoperative<br />
period.<br />
5-36<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
A physician (primary care or specialist) or qualified NPP who performs a postoperative evaluation <strong>of</strong> a<br />
new or established patient at the request <strong>of</strong> the surgeon may bill the appropriate consultation code for<br />
evaluation <strong>and</strong> management services furnished during the postoperative period following surgery when all<br />
<strong>of</strong> the criteria for the use <strong>of</strong> the consultation codes are met <strong>and</strong> that same physician has not already<br />
performed a preoperative consultation.<br />
I. Surgeon’s Request That Another Physician Participate In Postoperative Care<br />
If the surgeon asks a physician or qualified NPP who had been treating the patient preoperatively or who<br />
had not seen the patient for a preoperative consultation to take responsibility for the management <strong>of</strong> an<br />
aspect <strong>of</strong> the patient’s condition during the postoperative period, the physician or qualified NPP may not<br />
bill a consultation because the surgeon is not asking the physician or qualified NPP’s opinion or advice<br />
for the surgeon’s use in treating the patient. The physician or qualified NPP’s services would constitute<br />
concurrent care <strong>and</strong> should be billed using the appropriate subsequent hospital care codes in the hospital<br />
inpatient setting, subsequent NF care codes in the SNF/NF setting or the appropriate <strong>of</strong>fice or other<br />
outpatient visit codes in the <strong>of</strong>fice or outpatient settings.<br />
Physicians Regulatory Issues Team (PRIT) – Definition <strong>of</strong> a Consultation<br />
Issue<br />
The <strong>Indiana</strong> State Medical Association <strong>and</strong> others feel confused by the<br />
definition <strong>of</strong> Transfer <strong>of</strong> Care found in Transmittal 788.<br />
Status<br />
The PRIT is facilitating dialog between CMS staff, providers, <strong>and</strong><br />
carrier staff to clarify this definition.<br />
July 10<br />
August 28<br />
October 23, 2006<br />
January 11, 2007<br />
The PRIT has been contacted by the Infectious Disease Society <strong>of</strong><br />
America, the American College <strong>of</strong> Physicians, the American Medical<br />
Association <strong>and</strong> several other specialty societies about clarifying the<br />
definition <strong>of</strong> a consult in transmittal 788. We are working with them to<br />
address the issue.<br />
This issue was discussed at the August 28 2006 meeting <strong>of</strong> the<br />
Practicing Physician's Advisory Council.<br />
A letter signed by 51 medical associations <strong>and</strong> societies was sent to the<br />
CMS administration requesting clarification on this issue.<br />
There are instances <strong>of</strong> a “shared care” scenario which do meet the<br />
intent <strong>of</strong> a consultation. For example, a primary care physician consults<br />
with a specialist for a specific problem. The specialist evaluates the<br />
patient <strong>and</strong> continues to manage that aspect <strong>of</strong> the patient's care while<br />
the primary care physician continues to manage the overall patient care<br />
guided by the information from the specialist.<br />
Date Issue Created 06/15/2006<br />
EMERGENCY DEPARTMENT VISITS – CPT CODES 99281-99285<br />
Medicare Claims Processing Manual Chapter 12 §30.6.11 (Codes 99281-99288) (Rev. 1, 10-01-03) B3-<br />
15507<br />
A. Use <strong>of</strong> Emergency Department Codes by Physicians Not Assigned to Emergency Department<br />
Any physician seeing a patient registered in the emergency department may use emergency department<br />
visit codes (for services matching the code description). It is not required that the physician be assigned to<br />
the emergency department.<br />
5-37<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
B. Use <strong>of</strong> Emergency Department Codes in Office<br />
Emergency department <strong>coding</strong> is not appropriate if the site <strong>of</strong> service is an <strong>of</strong>fice or outpatient setting or<br />
any sight <strong>of</strong> service other than an emergency department. The emergency department codes should only<br />
be used if the patient is seen in the emergency department <strong>and</strong> the services described by the HCPCS code<br />
definition are provided. The emergency department is defined as an organized hospital-based facility for<br />
the provision <strong>of</strong> unscheduled or episodic services to patients who present for immediate medical attention.<br />
C. Use <strong>of</strong> Emergency Department Codes to Bill Nonemergency Services<br />
Services in the emergency department may not be emergencies. However, the codes (99281-99288) are<br />
payable if the described services are provided.<br />
However, if the physician asks the patient to meet him or her in the emergency department as an<br />
alternative to the physician’s <strong>of</strong>fice <strong>and</strong> the patient is not registered as a patient in the emergency<br />
department, the physician should bill the appropriate <strong>of</strong>fice/outpatient visit codes. Normally a lower level<br />
<strong>of</strong> emergency department code would be reported for a nonemergency condition.<br />
D. Emergency Department or Office/Outpatient Visits on Same Day as Nursing Facility Admission<br />
Emergency department visit provided on the same day as a comprehensive nursing facility assessment are<br />
not paid. Payment for evaluation <strong>and</strong> management services on the same date provided in sites other than<br />
the nursing facility are included in the payment for initial nursing facility care when performed on the<br />
same date as the nursing facility admission.<br />
E. Physician Billing for Emergency Department Services Provided to Patient by Both Patient’s Personal<br />
Physician <strong>and</strong> Emergency Department Physician<br />
If a physician advises his/her own patient to go to an emergency department (ED) <strong>of</strong> a hospital for care<br />
<strong>and</strong> the physician subsequently is asked by the ED physician to come to the hospital to evaluate the<br />
patient <strong>and</strong> to advise the ED physician as to whether the patient should be admitted to the hospital or be<br />
sent home, the physicians should bill as follows:<br />
• If the patient is admitted to the hospital by the patient’s personal physician, then the patient’s<br />
regular physician should bill only the appropriate level <strong>of</strong> the initial hospital care (codes 99221-<br />
99223) because all evaluation <strong>and</strong> management services provided by that physician in<br />
conjunction with that admission are considered part <strong>of</strong> the initial hospital care when performed on<br />
the same date as the admission. The ED physician who saw the patient in the emergency<br />
department should bill the appropriate level <strong>of</strong> the ED codes.<br />
• If the ED physician, based on the advice <strong>of</strong> the patient’s personal physician who came to the<br />
emergency department to see the patient, sends the patient home, then the ED physician should<br />
bill the appropriate level <strong>of</strong> emergency department service. The patient’s personal physician<br />
should also bill the level <strong>of</strong> emergency department code that describes the service he or she<br />
provided in the emergency department. The patient’s personal physician would not bill a<br />
consultation because he or she is not providing information to the emergency department<br />
physician for his or her use in treating the patient. If the patient’s personal physician does not<br />
come to the hospital to see the patient, but only advises the emergency department physician by<br />
telephone, then the patient’s personal physician may not bill.<br />
NURSING FACILITY VISITS – CPT CODES 99304-99316<br />
Initial Nursing Facility Care<br />
Codes 99304-99306 are selected based on the type <strong>of</strong> history, exam, <strong>and</strong> medical decision making based<br />
which will be based on the patient’s problem(s) requiring admission to the facility. Typical times have not<br />
been established. CPT provides guidance for selecting the appropriate level <strong>of</strong> admission by giving the<br />
5-38<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
typical severity <strong>of</strong> the problem(s) requiring admission. These codes should be reported by the admitting<br />
physician responsible for the care <strong>of</strong> the patient during the inpatient stay.<br />
Annual Nursing Facility Services<br />
Code 99318 is used to describe the annual nursing facility assessment. This code must include a detailed<br />
interval history, a comprehensive examination, <strong>and</strong> medical decision making that is <strong>of</strong> low to moderate<br />
complexity. These patients are usually stable, recovering, or improving. Physicians should not report<br />
99318 on the same day as subsequent nursing facility codes 99307-99310.<br />
Subsequent Nursing Facility Care<br />
Codes 99307-99310 are selected based on the type <strong>of</strong> history, exam, <strong>and</strong> medical decision making which<br />
will be based on the patient’s presenting problem(s). Typical times have not been established. CPT<br />
provides guidance for selecting the appropriate level <strong>of</strong> admission by the patient’s status, e.g., stable,<br />
inadequate response to therapy, new problem, etc.<br />
Nursing Facility Discharge<br />
Discharge day management services are coded 99315 or 99316. The codes are selected based on the<br />
amount <strong>of</strong> time spent for the final discharge from the nursing facility.<br />
Medicare Guidelines for Nursing Facility Coding<br />
Medicare Claims Processing Manual Chapter 12 §30.6.13 (Rev. 1, 10-01-03) B3-15509-15509.1 (Rev.<br />
808 Implementation No later than 01-23-06)<br />
A. Visits to Perform the Initial Comprehensive Assessment <strong>and</strong> Annual Assessments<br />
The distinction made between the delegation <strong>of</strong> physician visits <strong>and</strong> tasks in a skilled nursing facility<br />
(SNF) <strong>and</strong> in a nursing facility (NF) is based on the Medicare Statute. §1819 (b) (6) (A) <strong>of</strong> the Social<br />
Security Act (the Act) governs SNFs while §1919(b)(6)(A) <strong>of</strong> the Act governs NFs. For further<br />
information, refer to Medlearn Matters article number SE0418 at www.cms.hhs.gov/medlearn/matters<br />
The initial visit in a SNF <strong>and</strong> NF must be performed by the physician except as otherwise permitted<br />
(42CFR483.40(c)(4)). The initial visit is defined in as the initial comprehensive assessment visit during<br />
which the physician [Emphasis Added] completes a thorough assessment, develops a plan <strong>of</strong> care <strong>and</strong><br />
writes or verifies admitting orders for the nursing facility resident. For Survey <strong>and</strong> Certification<br />
requirements, a visit must occur no later than 30 days after admission.<br />
Further, per the Long Term Care regulations at 42CFR483.40(c)(4) <strong>and</strong> (e)(2), the physician may not<br />
delegate [Emphasis Added] a task that the physician must personally perform. Therefore, the physician<br />
may not delegate the initial visit in a SNF. This also applies to the NF with one exception.<br />
The only exception, as to who performs the initial visit, relates to the NF setting [Emphasis Added]. In<br />
the NF setting, a qualified NPP [Emphasis Added] (i.e., a nurse practitioner (NP), physician assistant<br />
(PA), or a clinical nurse specialist (CNS), who is not employed by the facility, may perform the initial<br />
visit [Emphasis Added] when the State law permits. The evaluation <strong>and</strong> management (E/M) visit shall be<br />
within the State scope <strong>of</strong> practice <strong>and</strong> licensure requirements where the E/M visit is performed <strong>and</strong> the<br />
requirements for physician collaboration <strong>and</strong> physician supervision shall be met.<br />
Under Medicare Part B payment policy, other medically necessary E/M visits may be performed <strong>and</strong><br />
reported prior to <strong>and</strong> after the initial visit, if the medical needs <strong>of</strong> the patient require an E/M visit. A<br />
qualified NPP may perform medically necessary E/M visits prior to <strong>and</strong> after the initial visit if all the<br />
requirements for collaboration, general physician supervision, licensure <strong>and</strong> billing are met.<br />
5-39<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
The CPT Nursing Facility Services codes shall be used with place <strong>of</strong> service (POS) 31 (SNF) if the<br />
patient is in a Part A SNF stay. They shall be used with POS 32 (nursing facility) if the patient does not<br />
have Part A SNF benefits or if the patient is in a NF or in a non-covered SNF stay (e.g., there was no<br />
preceding 3-day hospital stay). The CPT Nursing Facility code definition also includes POS 54<br />
(Intermediate Care Facility/Mentally Retarded) <strong>and</strong> POS 56 (Psychiatric Residential Treatment Center).<br />
Initial Nursing Facility Care, per day, (99304–99306) are used to report the initial visit. Only a physician<br />
may report these codes for an initial visit performed in a SNF or NF (with the exception <strong>of</strong> the qualified<br />
NPP in the NF setting who is not employed by the facility <strong>and</strong> when State law permits, as explained<br />
above).<br />
A readmission to a SNF or NF shall have the same payment policy requirements as an initial admission in<br />
both the SNF <strong>and</strong> NF settings.<br />
A physician who is employed by the SNF/NF may perform the E/M visits <strong>and</strong> bill independently to<br />
Medicare Part B for payment. An NPP who is employed by the SNF or NF may perform <strong>and</strong> bill<br />
Medicare Part B directly for those services where it is permitted as discussed above. The employer <strong>of</strong> the<br />
PA shall always report the visits performed by the PA. A physician, NP or CNS has the option to bill<br />
Medicare directly or to reassign payment for his/her pr<strong>of</strong>essional service to the facility.<br />
As with all E/M visits for Medicare Part B payment policy, the E/M documentation guidelines apply.<br />
B. Visits to Comply With Federal Regulations (42 CFR 483.40 (c) (1)) in the SNF <strong>and</strong> NF<br />
Payment is made under the physician fee schedule by Medicare Part B for federally m<strong>and</strong>ated visits.<br />
Following the initial visit by the physician, payment shall be made for federally m<strong>and</strong>ated visits that<br />
monitor <strong>and</strong> evaluate residents at least once every 30 days for the first 90 days after admission <strong>and</strong> at least<br />
once every 60 days thereafter.<br />
Subsequent Nursing Facility Care, per day, codes 99307–99310 are used to report federally m<strong>and</strong>ated<br />
physician E/M visits <strong>and</strong> medically necessary E/M visits.<br />
Carriers shall not pay for more than one E/M visit performed by the physician or qualified NPP for the<br />
same patient on the same date <strong>of</strong> service. The Nursing Facility Services codes represent a “per day”<br />
service.<br />
The federally m<strong>and</strong>ated E/M visit may serve also as a medically necessary E/M visit if the situation arises<br />
(i.e., the patient has health problems that need attention on the day the scheduled m<strong>and</strong>ated physician E/M<br />
visit occurs). The physician/qualified NPP shall bill only one E/M visit.<br />
Other Nursing Facility Service (99318), is used to report an annual nursing facility assessment visit on the<br />
required schedule <strong>of</strong> visits on an annual basis. For Medicare Part B payment policy, an annual nursing<br />
facility assessment visit code may substitute as meeting one <strong>of</strong> the federally m<strong>and</strong>ated physician visits if<br />
the code requirements for CPT code 99318 are fully met <strong>and</strong> in lieu <strong>of</strong> <strong>reporting</strong> a Subsequent Nursing<br />
Facility Care, per day, service (codes 99307–99310). It shall not be performed in addition to the required<br />
number <strong>of</strong> federally m<strong>and</strong>ated physician visits. Qualified NPPs, whether employed or not by the SNF,<br />
may perform alternating federally m<strong>and</strong>ated physician visits, at the option <strong>of</strong> the physician, after the<br />
initial visit by the physician in a SNF.<br />
Qualified NPPs in the NF setting, who are not employed by the NF, may perform federally m<strong>and</strong>ated<br />
physician visits, at the option <strong>of</strong> the State, after the initial visit by the physician.<br />
5-40<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
Medicare Part B payment policy does not pay for additional E/M visits that may be required by State law<br />
for a facility admission or for other additional visits to satisfy facility or other administrative purposes.<br />
E/M visits, prior to <strong>and</strong> after the initial physician visit, that are reasonable <strong>and</strong> medically necessary to<br />
meet the medical needs <strong>of</strong> the individual patient (unrelated to any State requirement or administrative<br />
purpose) are payable under Medicare Part B.<br />
C. Visits by Qualified Nonphysician Practitioners<br />
All E/M visits shall be within the State scope <strong>of</strong> practice <strong>and</strong> licensure requirements where the visit is<br />
performed <strong>and</strong> all the requirements for physician collaboration <strong>and</strong> physician supervision shall be met<br />
when performed <strong>and</strong> reported by qualified NPPs. General physician supervision <strong>and</strong> employer billing<br />
requirements shall be met for PA services in addition to the PA meeting the State scope <strong>of</strong> practice <strong>and</strong><br />
licensure requirements where the E/M visit is performed.<br />
Medically Necessary Visits<br />
Qualified NPPs may perform medically necessary E/M visits prior to <strong>and</strong> after the physician’s initial visit<br />
in both the SNF <strong>and</strong> NF. Medically necessary E/M visits for the diagnosis or treatment <strong>of</strong> an illness or<br />
injury or to improve the functioning <strong>of</strong> a malformed body member are payable under the physician fee<br />
schedule under Medicare Part B. CPT codes, Subsequent Nursing Facility Care, per day (99307-99310),<br />
shall be reported for these E/M visits even if the visits are provided prior to the initial visit by the<br />
physician.<br />
SNF Setting--Place <strong>of</strong> Service Code 31<br />
Following the initial visit by the physician, the physician may delegate alternate federally m<strong>and</strong>ated<br />
physician visits to a qualified NPP who meets collaboration <strong>and</strong> physician supervision requirements <strong>and</strong><br />
is licensed as such by the State <strong>and</strong> performing within the scope <strong>of</strong> practice in that State.<br />
NF Setting--Place <strong>of</strong> Service Code 32<br />
Per the regulations at 42CFR483.40(f), a qualified NPP, who meets the collaboration <strong>and</strong> physician<br />
supervision requirements, the State scope <strong>of</strong> practice <strong>and</strong> licensure requirements, <strong>and</strong> who is not<br />
employed by the NF, may at the option <strong>of</strong> the State, perform the initial visit in a NF, <strong>and</strong> may perform<br />
any other federally m<strong>and</strong>ated physician visit in a NF in addition to performing other medically necessary<br />
E/M visits.<br />
Questions pertaining to writing orders or certification <strong>and</strong> recertification issues in the SNF <strong>and</strong> NF<br />
settings shall be addressed to the appropriate State Survey <strong>and</strong> Certification Agency departments for<br />
clarification.<br />
D. Medically Complex Care<br />
Payment is made for E/M visits to patients in a SNF who are receiving services for medically complex<br />
care upon discharge from an acute care facility when the visits are reasonable <strong>and</strong> medically necessary<br />
<strong>and</strong> documented in the medical record. Physicians <strong>and</strong> qualified NPPs shall report E/M visits using the<br />
Subsequent Nursing Facility Care, per day (codes 99307-99310) for these E/M visits even if the visits are<br />
provided prior to the initial visit by the physician.<br />
E. Incident to Services<br />
Where a physician establishes an <strong>of</strong>fice in a SNF/NF, the “incident to” services <strong>and</strong> requirements are<br />
confined to this discrete part <strong>of</strong> the facility designated as his/her <strong>of</strong>fice. “Incident to” E/M visits, provided<br />
in a facility setting, are not payable under the Physician Fee Schedule for Medicare Part B. Thus, visits<br />
performed outside the designated “<strong>of</strong>fice” area in the SNF/NF would be subject to the coverage <strong>and</strong><br />
payment rules applicable to SNF/NF setting <strong>and</strong> shall not be reported using the CPT codes for <strong>of</strong>fice or<br />
other outpatient visits or use place <strong>of</strong> service code 11.<br />
5-41<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
F. Not Pertinent to this H<strong>and</strong>out<br />
G. Not Pertinent to this H<strong>and</strong>out<br />
H. Split/Shared E/M Visit<br />
A split/shared E/M visit cannot [Emphasis Added] be reported in the SNF/NF setting. A split/shared E/M<br />
visit is defined by Medicare Part B payment policy as a medically necessary encounter with a patient<br />
where the physician <strong>and</strong> a qualified NPP each personally perform a substantive portion <strong>of</strong> an E/M visit<br />
face-to-face with the same patient on the same date <strong>of</strong> service. A substantive portion <strong>of</strong> an E/M visit<br />
involves all or some portion <strong>of</strong> the history, exam, or medical decision making key components <strong>of</strong> an E/M<br />
service. The physician <strong>and</strong> the qualified NPP must be in the same group practice or be employed by the<br />
same employer. The split/shared E/M visit applies only to selected E/M visits <strong>and</strong> settings (i.e., hospital<br />
inpatient, hospital outpatient, hospital observation, emergency department, hospital discharge, <strong>of</strong>fice <strong>and</strong><br />
non facility clinic visits, <strong>and</strong> prolonged visits associated with these E/M visit codes). The split/shared E/M<br />
policy does not apply to consultation services, critical care services, or procedures.<br />
I. SNF/NF Discharge Day Management Service<br />
Medicare Part B payment policy requires a face-to-face visit with the patient provided by the physician or<br />
the qualified NPP to meet the SNF/NF discharge day management service as defined by the CPT code.<br />
The E/M discharge day management visit shall be reported for the date <strong>of</strong> the actual visit by the physician<br />
or qualified NPP even if the patient is discharged from the facility on a different calendar date. The CPT<br />
codes 99315 – 99316 shall be reported for this visit. The Discharge Day Management Service may be<br />
reported using CPT code 99315 or 99316, depending on the code requirement, for a patient who has<br />
expired, but only if the physician or qualified NPP personally performed the death pronouncement.<br />
99315 30 minutes or less<br />
99316 greater than 30 minutes<br />
DOMICILIARY CARE – CPT CODES 99324-99337<br />
There are five levels <strong>of</strong> care for the evaluation <strong>and</strong> management <strong>of</strong> new patients. Codes 99324-99328<br />
include the type <strong>of</strong> history, exam, <strong>and</strong> medical decision making as well as the typical time spent<br />
performing the service. Thus, these codes can be selected by time with more than 50 percent <strong>of</strong> the time is<br />
spent in counseling or coordination <strong>of</strong> care.<br />
Codes 99334-99337 provide four levels <strong>of</strong> care for the evaluation <strong>and</strong> management <strong>of</strong> established<br />
patients. These codes can be based on the content <strong>of</strong> the service provided (history, exam, <strong>and</strong> medical<br />
decision making) or by time when more than 50 percent <strong>of</strong> the time is spent in counseling or coordination<br />
<strong>of</strong> care.<br />
Place <strong>of</strong> service “13” - Assisted Living Facility – Definition: Congregate residential facility with selfcontained<br />
living units providing assessment <strong>of</strong> each resident's needs <strong>and</strong> on-site support 24 hours a day, 7<br />
days a week, with the capacity to deliver or arrange for services including some health care <strong>and</strong> other<br />
services.<br />
5-42<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
HOME SERVICES – CPT CODES 99341-99350<br />
Medicare Claims Processing Manual Chapter 12 §30.6.14.1 (Codes 99341-99350) (Rev. 1, 10-01-03) B3-<br />
15515, B3-15066<br />
A. Requirement for Physician Presence<br />
Home services codes 99341-99350 are paid when they are billed to report evaluation <strong>and</strong> management<br />
services provided in a private residence. A home visit cannot be billed by a physician unless the physician<br />
was actually present in the beneficiary’s home.<br />
B. Homebound Status<br />
Under the home health benefit, the beneficiary must be confined to the home for services to be covered.<br />
For home services provided by a physician using these codes, the beneficiary does not need to be<br />
confined to the home. The medical record must document the medical necessity <strong>of</strong> the home visit made<br />
in lieu <strong>of</strong> an <strong>of</strong>fice or outpatient visit. [Emphasis Added]<br />
SCREENING PAP SMEARS AND SCREENING PELVIC EXAMINATION<br />
(INCLUDING CLINICAL BREAST EXAM)<br />
Medicare Benefit Policy Manual Chapter 15 §280.4 (Rev. 1, 10-01-03) A3-3628.1, B3-4603.1<br />
Effective, July 1, 2001, the Consolidated Appropriations Act <strong>of</strong> 2001 (P.L. 106-554) modifies §1861(nn)<br />
to provide Medicare coverage for biennial screening Pap smears or more frequent coverage for women:<br />
1. At high-risk for cervical or vaginal cancer<br />
2. Of childbearing age who have had a Pap smear during any <strong>of</strong> the preceding three years indicating<br />
the presence <strong>of</strong> cervical or vaginal cancer or other abnormality<br />
Cervical Cancer High-Risk Factors<br />
1. Early onset <strong>of</strong> sexual activity (under 16 years <strong>of</strong> age)<br />
2. Multiple sexual partners (five (5) or more in a lifetime)<br />
3. History <strong>of</strong> a sexually transmitted disease (including HIV infection)<br />
4. Fewer than three negative or any Pap smears within the previous seven years<br />
Vaginal Cancer High Risk Factors<br />
1. DES (diethylstilbestrol) - exposed daughters <strong>of</strong> women who took DES during pregnancy<br />
The term “woman <strong>of</strong> childbearing age” means a woman who is premenopausal, <strong>and</strong> has been determined<br />
by a physician, or qualified practitioner, to be <strong>of</strong> childbearing age, based on her medical history or other<br />
findings. Payment is not made for a screening Pap smear for women at high-risk or who qualify for<br />
coverage under the childbearing provision more frequently than once every 11 months after the month<br />
that the last screening Pap smear covered by Medicare was performed.<br />
For Claims with Dates <strong>of</strong> Service on or After July 1, 2001<br />
When the beneficiary does not qualify for a more frequently performed screening Pap smear as noted in<br />
items 1 <strong>and</strong> 2 above, contractors pay for the screening Pap smear only after at least 23 months have<br />
passed following the month during which the beneficiary received her last covered screening Pap smear.<br />
All other coverage <strong>and</strong> payment requirements remain the same.<br />
5-43<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
Screening Pelvic Examinations<br />
Medicare Claims Processing Manual Chapter 18 §40 (Rev. 1, 10-01-03) B3-4603.2, A3-3, 3628.1B<br />
§4102 <strong>of</strong> the Balanced Budget Act <strong>of</strong> 1997 provides for coverage <strong>of</strong> screening pelvic examinations<br />
(including a clinical breast examination) for all female beneficiaries, subject to certain frequency <strong>and</strong><br />
other limitations.<br />
A screening pelvic examination (including a clinical breast examination) should include at least seven (7)<br />
<strong>of</strong> the following eleven (11) elements:<br />
• Inspection <strong>and</strong> palpation <strong>of</strong> breasts for masses or lumps, tenderness, symmetry, or nipple<br />
discharge<br />
• Digital rectal examination including sphincter tone, presence <strong>of</strong> hemorrhoids, <strong>and</strong> rectal masses<br />
Pelvic examination (with or without specimen collection for smears <strong>and</strong> cultures) including:<br />
• External genitalia (for example, general appearance, hair distribution, or lesions)<br />
• Urethral meatus (for example, size, location, lesions, or prolapse)<br />
• Urethra (for example, masses, tenderness, or scarring)<br />
• Bladder (for example, fullness, masses, or tenderness)<br />
• Vagina (for example, general appearance, estrogen effect, discharge lesions, pelvic support,<br />
cystocele, or rectocele)<br />
• Cervix (for example, general appearance, lesions, or discharge)<br />
• Uterus (for example, size, contour, position, mobility, tenderness, consistency, descent, or<br />
support)<br />
• Adnexa/parametria (for example, masses, tenderness, organomegaly, or nodularity)<br />
• Anus <strong>and</strong> perineum<br />
Coding for Screening Pelvic Examinations<br />
Medicare Claims Processing Manual Chapter 18 §40.2 (Rev. 1, 10-01-03) B3-4603.2.B <strong>and</strong> C, A3-<br />
3628.1.B.1<br />
A HCPCS code has been established for the pelvic <strong>and</strong> clinical breast examinations. Use code G0101<br />
(cervical or vaginal cancer screening, pelvic <strong>and</strong> clinical breast examination).<br />
Coding for Obtaining the Pap smear<br />
Medicare Claims Processing Manual Chapter 18 §30.5.D (Rev. 795, Issued: 12-30-05; Effective: 10-01-<br />
04; Implementation: 04-03-06)<br />
Use HCPCS code Q0091 to report the obtaining a screening pap smear during an encounter. This code is<br />
subject to the same frequencies <strong>and</strong> diagnoses as pelvic <strong>and</strong> clinical breast exam.<br />
Payment for Q0091 is paid under the Medicare physician fee schedule. Deductible is not applicable,<br />
however the coinsurance applies.<br />
Effective for services on <strong>and</strong> after July 1, 2005, on those occasions when physicians must perform a<br />
screening Pap smear (Q0091) that they know will not be covered by Medicare because the low risk<br />
patient has already received a covered Pap smear (Q0091) in the past 2 years, the physician can bill<br />
Q0091 <strong>and</strong> the claim will be denied appropriately.<br />
The physician shall obtain an advance beneficiary notice (ABN) in these situations as the denial will be<br />
considered a not reasonable <strong>and</strong> necessary denial. The physician indicates on the claim that an ABN has<br />
been obtained by using the GA modifier.<br />
Effective for services on or after April 1, 1999, a covered evaluation <strong>and</strong> management (E/M) visit <strong>and</strong><br />
code Q0091 may be reported by the same physician for the same date <strong>of</strong> service if the E/M visit is for a<br />
separately identifiable service. In this case, the modifier “-25” must be reported with the E/M service <strong>and</strong><br />
5-44<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
the medical records must clearly document the E/M reported. Both procedure codes should be shown as<br />
separate line items on the claim. These services can also be performed separately on separate <strong>of</strong>fice visits.<br />
Repeat Obtaining Screening Pap Smear Due To Inadequate Specimen<br />
Related Change Request (CR) #: 3659 Medlearn Matters Number: MM3659 Related CR Transmittal #:<br />
440 Implementation Date: July 5, 2005<br />
When a Pap smear specimen is not sufficient for the laboratory to interpret the results <strong>and</strong> another<br />
specimen is needed report Q0091 <strong>and</strong> append the -76 modifier to indicate it is a repeat specimen. The<br />
Carrier will pay for the collection <strong>of</strong> the specimen. Physicians should not report the screening pelvic<br />
examination again as the entire service is not medically necessary. It is also inappropriate to report an<br />
E/M code unless the patient has another problem needing a medically necessary evaluation on the same<br />
date <strong>of</strong> service.<br />
CMS Incident To Clarification<br />
CMS Region V clarified that screening pelvic examination with clinical breast exam (G0101) <strong>and</strong><br />
obtaining screening Pap smear (Q0091) cannot be billed “incident to” the physician’s services. The<br />
physician or nonphysician practitioner who PERFORMS the service(s) must report these screening<br />
services. This clarification applies to all screening services.<br />
Covered Diagnoses For Reporting Screening Pelvic Examination Or The Obtaining Of A Screening<br />
Pap Smear<br />
Medicare Claims Processing Manual Chapter 18 §30.6 (Rev. 1, 10-01-03) AB-03-054 (CR 2637) (Rev.<br />
440, Issued: 01-21-05, Effective: 07-01-05, Implementation: 07-05-05)<br />
Applicable Diagnoses for Billing a Carrier<br />
There are a number <strong>of</strong> appropriate diagnosis codes that can be used in billing for screening Pap smear<br />
services that the provider can list on the claim to give a true picture <strong>of</strong> the patient’s condition. To be<br />
covered one <strong>of</strong> the following diagnoses must be listed in Item 21 <strong>of</strong> Form CMS-1500 or the electronic<br />
equivalent.<br />
Below are the current diagnoses that should be used when billing for screening Pap smear services.<br />
Effective, July 1, 2005, V72.31 is being added to the CWF edit as an additional low risk diagnosis. The<br />
following chart lists the diagnosis codes that CWF must recognize for low risk or high-risk patients for<br />
screening Pap smear services.<br />
Low Risk Definitions<br />
Diagnosis Codes<br />
V76.2 Special screening for malignant neoplasms, cervix<br />
V76.47 Special screening for malignant neoplasm, vagina<br />
V76.49 Special screening for malignant neoplasm, other sites<br />
NOTE: providers use this diagnosis for women without a cervix.<br />
V72.31 Routine gynecological examination<br />
NOTE: This diagnosis should only be used when the provider<br />
performs a full gynecological examination.<br />
High Risk Diagnosis Code<br />
V15.89 Other<br />
If one <strong>of</strong> these diagnoses is not present or if the frequency requirements are not met, the CWF will reject<br />
the claim as “not medically necessary.”<br />
5-45<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
RISK ASSESSMENT FORM<br />
A screening pelvic examination (including a clinical breast examination) <strong>and</strong>/or screening pap smear is a<br />
covered Medicare service once every two years, unless a patient is considered high-risk for cervical or<br />
vaginal cancer. Listed below are the criteria considered to be high-risk. If you meet any <strong>of</strong> the following,<br />
<strong>and</strong> wish to share this information with us, the screening pelvic <strong>and</strong>/or screening pap may be paid<br />
annually.<br />
_____ Childbearing age <strong>and</strong> have had an examination indicating the presence <strong>of</strong> cervical or<br />
vaginal cancer or other abnormality during any <strong>of</strong> the preceding three years<br />
_____ Early onset <strong>of</strong> sexual activity (under 16 years <strong>of</strong> age)<br />
_____ Multiple sexual partners (five or more in a lifetime)<br />
_____ History <strong>of</strong> sexually transmitted disease (including the human immunodeficiency virus<br />
[HIV])<br />
_____ Any <strong>of</strong> the last three pap smears were positive<br />
_____ No pap smear within the past seven years<br />
_____ Prenatal exposure to diethylstilbestrol<br />
OR<br />
_____ None <strong>of</strong> the above (payment may be made by Medicare once every two years)<br />
__________________________________________<br />
Signature<br />
________________________<br />
Date<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. IAFP Annual Meeting 2007<br />
Copyright 2007 Newby Consulting, Inc.<br />
46