pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
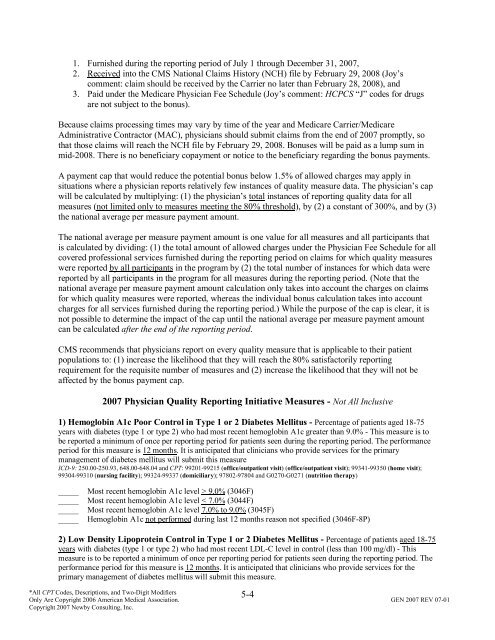
1. Furnished during the <strong>reporting</strong> period <strong>of</strong> July 1 through December 31, 2007,<br />
2. Received into the CMS National Claims History (NCH) file by February 29, 2008 (Joy’s<br />
comment: claim should be received by the Carrier no later than February 28, 2008), <strong>and</strong><br />
3. Paid under the Medicare Physician Fee Schedule (Joy’s comment: HCPCS “J” codes for drugs<br />
are not subject to the bonus).<br />
Because claims processing times may vary by time <strong>of</strong> the year <strong>and</strong> Medicare Carrier/Medicare<br />
Administrative Contractor (MAC), physicians should submit claims from the end <strong>of</strong> 2007 promptly, so<br />
that those claims will reach the NCH file by February 29, 2008. Bonuses will be paid as a lump sum in<br />
mid-2008. There is no beneficiary copayment or notice to the beneficiary regarding the bonus payments.<br />
A payment cap that would reduce the potential bonus below 1.5% <strong>of</strong> allowed charges may apply in<br />
situations where a physician reports relatively few instances <strong>of</strong> quality <strong>measure</strong> data. The physician’s cap<br />
will be calculated by multiplying: (1) the physician’s total instances <strong>of</strong> <strong>reporting</strong> quality data for all<br />
<strong>measure</strong>s (not limited only to <strong>measure</strong>s meeting the 80% threshold), by (2) a constant <strong>of</strong> 300%, <strong>and</strong> by (3)<br />
the national average per <strong>measure</strong> payment amount.<br />
The national average per <strong>measure</strong> payment amount is one value for all <strong>measure</strong>s <strong>and</strong> all participants that<br />
is calculated by dividing: (1) the total amount <strong>of</strong> allowed charges under the Physician Fee Schedule for all<br />
covered pr<strong>of</strong>essional services furnished during the <strong>reporting</strong> period on claims for which quality <strong>measure</strong>s<br />
were reported by all participants in the program by (2) the total number <strong>of</strong> instances for which data were<br />
reported by all participants in the program for all <strong>measure</strong>s during the <strong>reporting</strong> period. (Note that the<br />
national average per <strong>measure</strong> payment amount calculation only takes into account the charges on claims<br />
for which quality <strong>measure</strong>s were reported, whereas the individual bonus calculation takes into account<br />
charges for all services furnished during the <strong>reporting</strong> period.) While the purpose <strong>of</strong> the cap is clear, it is<br />
not possible to determine the impact <strong>of</strong> the cap until the national average per <strong>measure</strong> payment amount<br />
can be calculated after the end <strong>of</strong> the <strong>reporting</strong> period.<br />
CMS recommends that physicians report on every quality <strong>measure</strong> that is applicable to their patient<br />
populations to: (1) increase the likelihood that they will reach the 80% satisfactorily <strong>reporting</strong><br />
requirement for the requisite number <strong>of</strong> <strong>measure</strong>s <strong>and</strong> (2) increase the likelihood that they will not be<br />
affected by the bonus payment cap.<br />
2007 Physician Quality Reporting Initiative Measures - Not All Inclusive<br />
1) Hemoglobin A1c Poor Control in Type 1 or 2 Diabetes Mellitus - Percentage <strong>of</strong> patients aged 18-75<br />
years with diabetes (type 1 or type 2) who had most recent hemoglobin A1c greater than 9.0% - This <strong>measure</strong> is to<br />
be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period for patients seen during the <strong>reporting</strong> period. The performance<br />
period for this <strong>measure</strong> is 12 months. It is anticipated that clinicians who provide services for the primary<br />
management <strong>of</strong> diabetes mellitus will submit this <strong>measure</strong><br />
ICD-9: 250.00-250.93, 648.00-648.04 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit) (<strong>of</strong>fice/outpatient visit); 99341-99350 (home visit);<br />
99304-99310 (nursing facility); 99324-99337 (domiciliary); 97802-97804 <strong>and</strong> G0270-G0271 (nutrition therapy)<br />
_____<br />
_____<br />
_____<br />
_____<br />
Most recent hemoglobin A1c level > 9.0% (3046F)<br />
Most recent hemoglobin A1c level < 7.0% (3044F)<br />
Most recent hemoglobin A1c level 7.0% to 9.0% (3045F)<br />
Hemoglobin A1c not performed during last 12 months reason not specified (3046F-8P)<br />
2) Low Density Lipoprotein Control in Type 1 or 2 Diabetes Mellitus - Percentage <strong>of</strong> patients aged 18-75<br />
years with diabetes (type 1 or type 2) who had most recent LDL-C level in control (less than 100 mg/dl) - This<br />
<strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period for patients seen during the <strong>reporting</strong> period. The<br />
performance period for this <strong>measure</strong> is 12 months. It is anticipated that clinicians who provide services for the<br />
primary management <strong>of</strong> diabetes mellitus will submit this <strong>measure</strong>.<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.<br />
5-4