pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
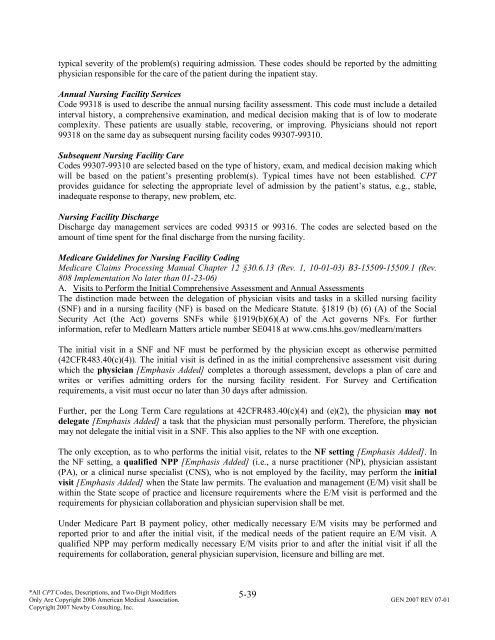
typical severity <strong>of</strong> the problem(s) requiring admission. These codes should be reported by the admitting<br />
physician responsible for the care <strong>of</strong> the patient during the inpatient stay.<br />
Annual Nursing Facility Services<br />
Code 99318 is used to describe the annual nursing facility assessment. This code must include a detailed<br />
interval history, a comprehensive examination, <strong>and</strong> medical decision making that is <strong>of</strong> low to moderate<br />
complexity. These patients are usually stable, recovering, or improving. Physicians should not report<br />
99318 on the same day as subsequent nursing facility codes 99307-99310.<br />
Subsequent Nursing Facility Care<br />
Codes 99307-99310 are selected based on the type <strong>of</strong> history, exam, <strong>and</strong> medical decision making which<br />
will be based on the patient’s presenting problem(s). Typical times have not been established. CPT<br />
provides guidance for selecting the appropriate level <strong>of</strong> admission by the patient’s status, e.g., stable,<br />
inadequate response to therapy, new problem, etc.<br />
Nursing Facility Discharge<br />
Discharge day management services are coded 99315 or 99316. The codes are selected based on the<br />
amount <strong>of</strong> time spent for the final discharge from the nursing facility.<br />
Medicare Guidelines for Nursing Facility Coding<br />
Medicare Claims Processing Manual Chapter 12 §30.6.13 (Rev. 1, 10-01-03) B3-15509-15509.1 (Rev.<br />
808 Implementation No later than 01-23-06)<br />
A. Visits to Perform the Initial Comprehensive Assessment <strong>and</strong> Annual Assessments<br />
The distinction made between the delegation <strong>of</strong> physician visits <strong>and</strong> tasks in a skilled nursing facility<br />
(SNF) <strong>and</strong> in a nursing facility (NF) is based on the Medicare Statute. §1819 (b) (6) (A) <strong>of</strong> the Social<br />
Security Act (the Act) governs SNFs while §1919(b)(6)(A) <strong>of</strong> the Act governs NFs. For further<br />
information, refer to Medlearn Matters article number SE0418 at www.cms.hhs.gov/medlearn/matters<br />
The initial visit in a SNF <strong>and</strong> NF must be performed by the physician except as otherwise permitted<br />
(42CFR483.40(c)(4)). The initial visit is defined in as the initial comprehensive assessment visit during<br />
which the physician [Emphasis Added] completes a thorough assessment, develops a plan <strong>of</strong> care <strong>and</strong><br />
writes or verifies admitting orders for the nursing facility resident. For Survey <strong>and</strong> Certification<br />
requirements, a visit must occur no later than 30 days after admission.<br />
Further, per the Long Term Care regulations at 42CFR483.40(c)(4) <strong>and</strong> (e)(2), the physician may not<br />
delegate [Emphasis Added] a task that the physician must personally perform. Therefore, the physician<br />
may not delegate the initial visit in a SNF. This also applies to the NF with one exception.<br />
The only exception, as to who performs the initial visit, relates to the NF setting [Emphasis Added]. In<br />
the NF setting, a qualified NPP [Emphasis Added] (i.e., a nurse practitioner (NP), physician assistant<br />
(PA), or a clinical nurse specialist (CNS), who is not employed by the facility, may perform the initial<br />
visit [Emphasis Added] when the State law permits. The evaluation <strong>and</strong> management (E/M) visit shall be<br />
within the State scope <strong>of</strong> practice <strong>and</strong> licensure requirements where the E/M visit is performed <strong>and</strong> the<br />
requirements for physician collaboration <strong>and</strong> physician supervision shall be met.<br />
Under Medicare Part B payment policy, other medically necessary E/M visits may be performed <strong>and</strong><br />
reported prior to <strong>and</strong> after the initial visit, if the medical needs <strong>of</strong> the patient require an E/M visit. A<br />
qualified NPP may perform medically necessary E/M visits prior to <strong>and</strong> after the initial visit if all the<br />
requirements for collaboration, general physician supervision, licensure <strong>and</strong> billing are met.<br />
5-39<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.