pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
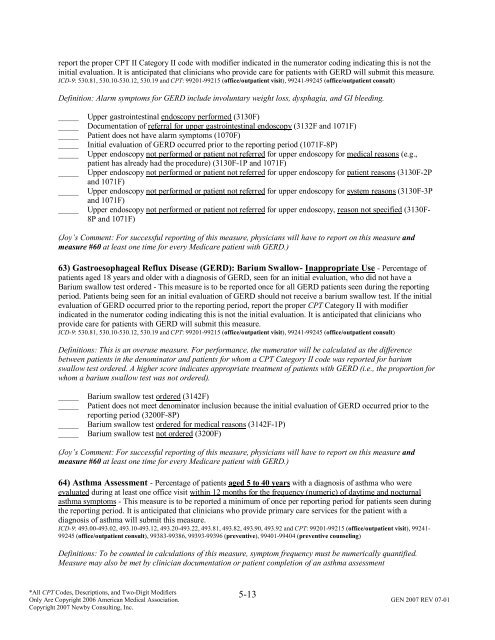
eport the proper CPT II Category II code with modifier indicated in the numerator <strong>coding</strong> indicating this is not the<br />
initial evaluation. It is anticipated that clinicians who provide care for patients with GERD will submit this <strong>measure</strong>.<br />
ICD-9: 530.81, 530.10-530.12, 530.19 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice/outpatient consult)<br />
Definition: Alarm symptoms for GERD include involuntary weight loss, dysphagia, <strong>and</strong> GI bleeding.<br />
_____ Upper gastrointestinal endoscopy performed (3130F)<br />
_____ Documentation <strong>of</strong> referral for upper gastrointestinal endoscopy (3132F <strong>and</strong> 1071F)<br />
_____ Patient does not have alarm symptoms (1070F)<br />
_____ Initial evaluation <strong>of</strong> GERD occurred prior to the <strong>reporting</strong> period (1071F-8P)<br />
_____ Upper endoscopy not performed or patient not referred for upper endoscopy for medical reasons (e.g.,<br />
patient has already had the procedure) (3130F-1P <strong>and</strong> 1071F)<br />
_____ Upper endoscopy not performed or patient not referred for upper endoscopy for patient reasons (3130F-2P<br />
<strong>and</strong> 1071F)<br />
_____ Upper endoscopy not performed or patient not referred for upper endoscopy for system reasons (3130F-3P<br />
<strong>and</strong> 1071F)<br />
_____ Upper endoscopy not performed or patient not referred for upper endoscopy, reason not specified (3130F-<br />
8P <strong>and</strong> 1071F)<br />
(Joy’s Comment: For successful <strong>reporting</strong> <strong>of</strong> this <strong>measure</strong>, physicians will have to report on this <strong>measure</strong> <strong>and</strong><br />
<strong>measure</strong> #60 at least one time for every Medicare patient with GERD.)<br />
63) Gastroesophageal Reflux Disease (GERD): Barium Swallow- Inappropriate Use - Percentage <strong>of</strong><br />
patients aged 18 years <strong>and</strong> older with a diagnosis <strong>of</strong> GERD, seen for an initial evaluation, who did not have a<br />
Barium swallow test ordered - This <strong>measure</strong> is to be reported once for all GERD patients seen during the <strong>reporting</strong><br />
period. Patients being seen for an initial evaluation <strong>of</strong> GERD should not receive a barium swallow test. If the initial<br />
evaluation <strong>of</strong> GERD occurred prior to the <strong>reporting</strong> period, report the proper CPT Category II with modifier<br />
indicated in the numerator <strong>coding</strong> indicating this is not the initial evaluation. It is anticipated that clinicians who<br />
provide care for patients with GERD will submit this <strong>measure</strong>.<br />
ICD-9: 530.81, 530.10-530.12, 530.19 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice/outpatient consult)<br />
Definitions: This is an overuse <strong>measure</strong>. For performance, the numerator will be calculated as the difference<br />
between patients in the denominator <strong>and</strong> patients for whom a CPT Category II code was reported for barium<br />
swallow test ordered. A higher score indicates appropriate treatment <strong>of</strong> patients with GERD (i.e., the proportion for<br />
whom a barium swallow test was not ordered).<br />
_____<br />
_____<br />
_____<br />
_____<br />
Barium swallow test ordered (3142F)<br />
Patient does not meet denominator inclusion because the initial evaluation <strong>of</strong> GERD occurred prior to the<br />
<strong>reporting</strong> period (3200F-8P)<br />
Barium swallow test ordered for medical reasons (3142F-1P)<br />
Barium swallow test not ordered (3200F)<br />
(Joy’s Comment: For successful <strong>reporting</strong> <strong>of</strong> this <strong>measure</strong>, physicians will have to report on this <strong>measure</strong> <strong>and</strong><br />
<strong>measure</strong> #60 at least one time for every Medicare patient with GERD.)<br />
64) Asthma Assessment - Percentage <strong>of</strong> patients aged 5 to 40 years with a diagnosis <strong>of</strong> asthma who were<br />
evaluated during at least one <strong>of</strong>fice visit within 12 months for the frequency (numeric) <strong>of</strong> daytime <strong>and</strong> nocturnal<br />
asthma symptoms - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period for patients seen during<br />
the <strong>reporting</strong> period. It is anticipated that clinicians who provide primary care services for the patient with a<br />
diagnosis <strong>of</strong> asthma will submit this <strong>measure</strong>.<br />
ICD-9: 493.00-493.02, 493.10-493.12, 493.20-493.22, 493.81, 493.82, 493.90, 493.92 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-<br />
99245 (<strong>of</strong>fice/outpatient consult), 99383-99386, 99393-99396 (preventive), 99401-99404 (preventive counseling)<br />
Definitions: To be counted in calculations <strong>of</strong> this <strong>measure</strong>, symptom frequency must be numerically quantified.<br />
Measure may also be met by clinician documentation or patient completion <strong>of</strong> an asthma assessment<br />
5-13<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.