pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
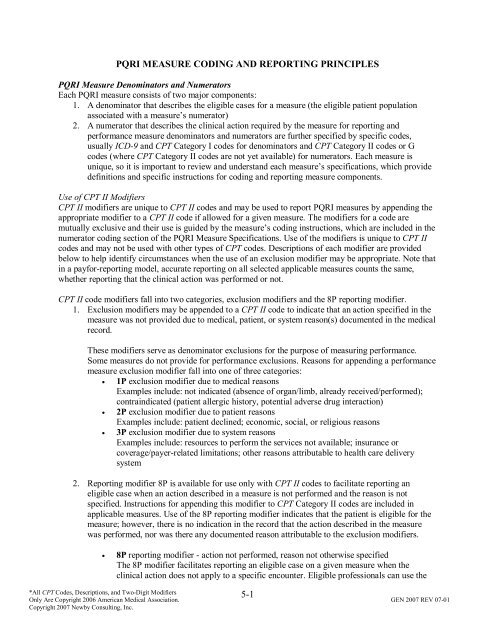
PQRI MEASURE CODING AND REPORTING PRINCIPLES<br />
PQRI Measure Denominators <strong>and</strong> Numerators<br />
Each PQRI <strong>measure</strong> consists <strong>of</strong> two major components:<br />
1. A denominator that describes the eligible cases for a <strong>measure</strong> (the eligible patient population<br />
associated with a <strong>measure</strong>’s numerator)<br />
2. A numerator that describes the clinical action required by the <strong>measure</strong> for <strong>reporting</strong> <strong>and</strong><br />
performance <strong>measure</strong> denominators <strong>and</strong> numerators are further specified by specific codes,<br />
usually ICD-9 <strong>and</strong> CPT Category I codes for denominators <strong>and</strong> CPT Category II codes or G<br />
codes (where CPT Category II codes are not yet available) for numerators. Each <strong>measure</strong> is<br />
unique, so it is important to review <strong>and</strong> underst<strong>and</strong> each <strong>measure</strong>’s specifications, which provide<br />
definitions <strong>and</strong> specific instructions for <strong>coding</strong> <strong>and</strong> <strong>reporting</strong> <strong>measure</strong> components.<br />
Use <strong>of</strong> CPT II Modifiers<br />
CPT II modifiers are unique to CPT II codes <strong>and</strong> may be used to report PQRI <strong>measure</strong>s by appending the<br />
appropriate modifier to a CPT II code if allowed for a given <strong>measure</strong>. The modifiers for a code are<br />
mutually exclusive <strong>and</strong> their use is guided by the <strong>measure</strong>’s <strong>coding</strong> instructions, which are included in the<br />
numerator <strong>coding</strong> section <strong>of</strong> the PQRI Measure Specifications. Use <strong>of</strong> the modifiers is unique to CPT II<br />
codes <strong>and</strong> may not be used with other types <strong>of</strong> CPT codes. Descriptions <strong>of</strong> each modifier are provided<br />
below to help identify circumstances when the use <strong>of</strong> an exclusion modifier may be appropriate. Note that<br />
in a payfor-<strong>reporting</strong> model, accurate <strong>reporting</strong> on all selected applicable <strong>measure</strong>s counts the same,<br />
whether <strong>reporting</strong> that the clinical action was performed or not.<br />
CPT II code modifiers fall into two categories, exclusion modifiers <strong>and</strong> the 8P <strong>reporting</strong> modifier.<br />
1. Exclusion modifiers may be appended to a CPT II code to indicate that an action specified in the<br />
<strong>measure</strong> was not provided due to medical, patient, or system reason(s) documented in the medical<br />
record.<br />
These modifiers serve as denominator exclusions for the purpose <strong>of</strong> measuring performance.<br />
Some <strong>measure</strong>s do not provide for performance exclusions. Reasons for appending a performance<br />
<strong>measure</strong> exclusion modifier fall into one <strong>of</strong> three categories:<br />
• 1P exclusion modifier due to medical reasons<br />
Examples include: not indicated (absence <strong>of</strong> organ/limb, already received/performed);<br />
contraindicated (patient allergic history, potential adverse drug interaction)<br />
• 2P exclusion modifier due to patient reasons<br />
Examples include: patient declined; economic, social, or religious reasons<br />
• 3P exclusion modifier due to system reasons<br />
Examples include: resources to perform the services not available; insurance or<br />
coverage/payer-related limitations; other reasons attributable to health care delivery<br />
system<br />
2. Reporting modifier 8P is available for use only with CPT II codes to facilitate <strong>reporting</strong> an<br />
eligible case when an action described in a <strong>measure</strong> is not performed <strong>and</strong> the reason is not<br />
specified. Instructions for appending this modifier to CPT Category II codes are included in<br />
applicable <strong>measure</strong>s. Use <strong>of</strong> the 8P <strong>reporting</strong> modifier indicates that the patient is eligible for the<br />
<strong>measure</strong>; however, there is no indication in the record that the action described in the <strong>measure</strong><br />
was performed, nor was there any documented reason attributable to the exclusion modifiers.<br />
• 8P <strong>reporting</strong> modifier - action not performed, reason not otherwise specified<br />
The 8P modifier facilitates <strong>reporting</strong> an eligible case on a given <strong>measure</strong> when the<br />
clinical action does not apply to a specific encounter. Eligible pr<strong>of</strong>essionals can use the<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.<br />
5-1
8P modifier to receive credit for successful <strong>reporting</strong> but will not receive credit for<br />
performance.<br />
For example, a patient with diabetes may present to a clinician for reasons that do not involve<br />
glycemic control, hypertension, or cholesterol management. However, the claim for services for<br />
that encounter will contain ICD-9 <strong>and</strong> CPT codes that will draw the patient into the diabetes<br />
<strong>measure</strong>s’ denominator during analysis. The 8P modifier serves to include the patient in the<br />
numerator when <strong>reporting</strong> rates are calculated for PQRI.<br />
Reporting Frequency <strong>and</strong> Performance Timeframes<br />
Each <strong>measure</strong> includes a <strong>reporting</strong> frequency requirement for each denominator-eligible patient seen<br />
during the <strong>reporting</strong> period. The <strong>reporting</strong> frequency is described in the instructions:<br />
• Report one-time only<br />
• Report once for each procedure performed<br />
• Report once for each acute episode<br />
A <strong>measure</strong>’s performance timeframe is defined in the <strong>measure</strong>’s description <strong>and</strong> is distinct from the<br />
<strong>reporting</strong> frequency requirement. The performance timeframe, unique to each <strong>measure</strong>, delineates the<br />
timeframe in which the clinical action described in the numerator may be accomplished.<br />
Performance timeframes may be stated as “within 12 months,” or “most recent.” This means that:<br />
1. The clinical action in the numerator need be performed only once during a 12-month period for<br />
each patient seen during the <strong>reporting</strong> period<br />
2. The quality code need be reported only one time for each patient by each eligible pr<strong>of</strong>essional<br />
caring for the patient who has chosen to report that <strong>measure</strong> during the <strong>reporting</strong> period<br />
If the <strong>measure</strong> calls for a clinical test result, then the most recent test result only needs to be obtained,<br />
assessed, <strong>and</strong> reported one time per <strong>reporting</strong> period. A test does not need to have been performed within<br />
the <strong>reporting</strong> period, nor does it need to have been performed by the same eligible pr<strong>of</strong>essional.<br />
Performance timeframes may also be tied to a specific clinical event that requires <strong>reporting</strong> each time the<br />
event occurs within the <strong>reporting</strong> period. The following are examples <strong>of</strong> <strong>measure</strong>s reported each time the<br />
clinical action described by the <strong>measure</strong> numerator is taken:<br />
• Procedure-related <strong>measure</strong>s require <strong>reporting</strong> each time the procedure is performed <strong>and</strong> have<br />
distinct performance timeframes tied to them. The date <strong>of</strong> service is the date that is used to report<br />
the <strong>measure</strong>. Examples are perioperative care or imaging <strong>measure</strong>s.<br />
• Chronic care <strong>measure</strong>s, such as those that call for prescribing a medication, require the eligible<br />
pr<strong>of</strong>essional to verify whether the medication is current <strong>and</strong> being taken by the patient. A new<br />
prescription is not required to meet the <strong>measure</strong> requirement unless it is clinically indicated.<br />
• Acute care <strong>measure</strong>s are tied to specific episodes <strong>of</strong> acute care <strong>and</strong> require <strong>reporting</strong> each time an<br />
acute event occurs. Examples are <strong>measure</strong>s related to hospitalizations, fractures <strong>and</strong> osteoporosis<br />
management, or stroke <strong>measure</strong>s.<br />
Claims-Based Reporting Principles<br />
The following <strong>principles</strong> apply to the <strong>reporting</strong> <strong>of</strong> quality-data codes for PQRI <strong>measure</strong><br />
• The CPT Category II code, which supplies the numerator, must be reported on the same claim<br />
form as the payment codes, usually ICD-9 <strong>and</strong> CPT Category I codes, which supply the<br />
denominator.<br />
• Quality-data codes must be submitted with a line item charge <strong>of</strong> zero dollars ($0.00) at the time<br />
the associated covered service is performed.<br />
! The submitted charge field cannot be blank.<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.<br />
5-2
! The line item charge should be $0.00.<br />
! If a system does not allow a $0.00 line item charge, use a small amount such as $0.01<br />
! Entire claims with a zero charge will be rejected. (Total charge for the claim cannot be<br />
$0.00)<br />
! Quality data code line items will be denied for payment, but are then passed through the<br />
claims processing system for PQRI analysis.<br />
• Multiple eligible pr<strong>of</strong>essionals’ quality-data codes can be reported on the same claim.<br />
• Multiple CPT Category II codes for multiple <strong>measure</strong>s that are applicable to a patient visit can be<br />
reported on the same claim, as long as the corresponding denominator codes are also line items<br />
on that claim.<br />
• The individual NPI <strong>of</strong> the participating eligible pr<strong>of</strong>essional(s) must be properly used on the<br />
claim.<br />
Timeliness <strong>of</strong> Quality Data Submission<br />
Claims processed by the Carrier/MAC must reach the national Medicare claims system data warehouse<br />
(National Claims History file) by February 29, 2008 to be included in the analysis. Claims for services<br />
furnished toward the end <strong>of</strong> the <strong>reporting</strong> period should be filed promptly. Claims that are resubmitted<br />
only to add quality-data codes will not be included in the analysis.<br />
Successful Reporting<br />
The 2007 PQRI incentive payment is an all-or-nothing bonus (subject to cap) based on successful<br />
<strong>reporting</strong>.<br />
Eligible pr<strong>of</strong>essionals need not enroll or file an intent to participate for the PQRI. Eligible pr<strong>of</strong>essionals<br />
can participate by <strong>reporting</strong> the appropriate quality <strong>measure</strong> data on claims submitted to their Medicare<br />
claims processing contractor.<br />
In order to satisfactorily meet the requirements <strong>of</strong> the program <strong>and</strong> receive the bonus payment, certain<br />
<strong>reporting</strong> thresholds must be met. When four or more <strong>measure</strong>s are applicable to the services provided by<br />
an eligible pr<strong>of</strong>essional, the 80% threshold must be met on at least three <strong>of</strong> the <strong>measure</strong>s reported.<br />
Good news for those physicians practicing in a group practice, not all physicians in the group must<br />
participate in PQRI to be eligible for the bonus payment. Individual analysis will be done using the<br />
individual physician’s national provider identifier (NPI) to determine satisfactory <strong>reporting</strong> <strong>and</strong> the bonus<br />
payment calculation. Thus, physicians must bill with an NPI to participate in PQRI. The potential 1.5<br />
percent incentive payment will be paid in mid-2008 as a lump-sum bonus payment made to the practice at<br />
the Taxpayer Identification Number (TIN) level. According to the CMS website, the NPI is the only<br />
unique provider enumerator that can be used by the CMS PQRI analysis contractor to properly identify<br />
eligible physicians at the individual-physician level.<br />
The performing pr<strong>of</strong>essional’s NPI must be used for the quality-data codes <strong>and</strong> related services. For<br />
claims submitted via the ASC X12N 837 pr<strong>of</strong>essional health care claim transaction, the group practice<br />
NPI is placed in the provider billing segment, loop 2010AA, <strong>and</strong> the performing pr<strong>of</strong>essional’s NPI is<br />
placed in loop 2420A. For claims submitted via the CMS 1500 form, the performing pr<strong>of</strong>essional’s NPI is<br />
placed on the individual line item. Placing the performing eligible pr<strong>of</strong>essional’s NPI on the individual<br />
line item will allow the analysis <strong>of</strong> successful <strong>reporting</strong> <strong>and</strong> the bonus payment calculation to be<br />
performed at the individual level, though payment will be made at the TIN level.<br />
Bonus Payment<br />
Participating eligible pr<strong>of</strong>essionals who successfully report may earn a 1.5% bonus, subject to cap. The<br />
potential 1.5% bonus will be based on allowed charges for covered pr<strong>of</strong>essional services:<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.<br />
5-3
1. Furnished during the <strong>reporting</strong> period <strong>of</strong> July 1 through December 31, 2007,<br />
2. Received into the CMS National Claims History (NCH) file by February 29, 2008 (Joy’s<br />
comment: claim should be received by the Carrier no later than February 28, 2008), <strong>and</strong><br />
3. Paid under the Medicare Physician Fee Schedule (Joy’s comment: HCPCS “J” codes for drugs<br />
are not subject to the bonus).<br />
Because claims processing times may vary by time <strong>of</strong> the year <strong>and</strong> Medicare Carrier/Medicare<br />
Administrative Contractor (MAC), physicians should submit claims from the end <strong>of</strong> 2007 promptly, so<br />
that those claims will reach the NCH file by February 29, 2008. Bonuses will be paid as a lump sum in<br />
mid-2008. There is no beneficiary copayment or notice to the beneficiary regarding the bonus payments.<br />
A payment cap that would reduce the potential bonus below 1.5% <strong>of</strong> allowed charges may apply in<br />
situations where a physician reports relatively few instances <strong>of</strong> quality <strong>measure</strong> data. The physician’s cap<br />
will be calculated by multiplying: (1) the physician’s total instances <strong>of</strong> <strong>reporting</strong> quality data for all<br />
<strong>measure</strong>s (not limited only to <strong>measure</strong>s meeting the 80% threshold), by (2) a constant <strong>of</strong> 300%, <strong>and</strong> by (3)<br />
the national average per <strong>measure</strong> payment amount.<br />
The national average per <strong>measure</strong> payment amount is one value for all <strong>measure</strong>s <strong>and</strong> all participants that<br />
is calculated by dividing: (1) the total amount <strong>of</strong> allowed charges under the Physician Fee Schedule for all<br />
covered pr<strong>of</strong>essional services furnished during the <strong>reporting</strong> period on claims for which quality <strong>measure</strong>s<br />
were reported by all participants in the program by (2) the total number <strong>of</strong> instances for which data were<br />
reported by all participants in the program for all <strong>measure</strong>s during the <strong>reporting</strong> period. (Note that the<br />
national average per <strong>measure</strong> payment amount calculation only takes into account the charges on claims<br />
for which quality <strong>measure</strong>s were reported, whereas the individual bonus calculation takes into account<br />
charges for all services furnished during the <strong>reporting</strong> period.) While the purpose <strong>of</strong> the cap is clear, it is<br />
not possible to determine the impact <strong>of</strong> the cap until the national average per <strong>measure</strong> payment amount<br />
can be calculated after the end <strong>of</strong> the <strong>reporting</strong> period.<br />
CMS recommends that physicians report on every quality <strong>measure</strong> that is applicable to their patient<br />
populations to: (1) increase the likelihood that they will reach the 80% satisfactorily <strong>reporting</strong><br />
requirement for the requisite number <strong>of</strong> <strong>measure</strong>s <strong>and</strong> (2) increase the likelihood that they will not be<br />
affected by the bonus payment cap.<br />
2007 Physician Quality Reporting Initiative Measures - Not All Inclusive<br />
1) Hemoglobin A1c Poor Control in Type 1 or 2 Diabetes Mellitus - Percentage <strong>of</strong> patients aged 18-75<br />
years with diabetes (type 1 or type 2) who had most recent hemoglobin A1c greater than 9.0% - This <strong>measure</strong> is to<br />
be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period for patients seen during the <strong>reporting</strong> period. The performance<br />
period for this <strong>measure</strong> is 12 months. It is anticipated that clinicians who provide services for the primary<br />
management <strong>of</strong> diabetes mellitus will submit this <strong>measure</strong><br />
ICD-9: 250.00-250.93, 648.00-648.04 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit) (<strong>of</strong>fice/outpatient visit); 99341-99350 (home visit);<br />
99304-99310 (nursing facility); 99324-99337 (domiciliary); 97802-97804 <strong>and</strong> G0270-G0271 (nutrition therapy)<br />
_____<br />
_____<br />
_____<br />
_____<br />
Most recent hemoglobin A1c level > 9.0% (3046F)<br />
Most recent hemoglobin A1c level < 7.0% (3044F)<br />
Most recent hemoglobin A1c level 7.0% to 9.0% (3045F)<br />
Hemoglobin A1c not performed during last 12 months reason not specified (3046F-8P)<br />
2) Low Density Lipoprotein Control in Type 1 or 2 Diabetes Mellitus - Percentage <strong>of</strong> patients aged 18-75<br />
years with diabetes (type 1 or type 2) who had most recent LDL-C level in control (less than 100 mg/dl) - This<br />
<strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period for patients seen during the <strong>reporting</strong> period. The<br />
performance period for this <strong>measure</strong> is 12 months. It is anticipated that clinicians who provide services for the<br />
primary management <strong>of</strong> diabetes mellitus will submit this <strong>measure</strong>.<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.<br />
5-4
ICD-9: 250.00-250.93, 648.00-648.04 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit) (<strong>of</strong>fice/outpatient visit); 99341-99350 (home visit);<br />
99304-99310 (nursing facility); 99324-99337 (domiciliary); 97802-97804 <strong>and</strong> G0270-G0271 (nutrition therapy)<br />
_____<br />
_____<br />
_____<br />
_____<br />
Most recent LDL-C < 100 mg/dL (3048F)<br />
Most recent LDL-C 100-129 mg/dL (3049F)<br />
Most recent LDL-C ≥ 130 mg/dL (3050F)<br />
LDL-C level not performed during last 12 months reason not specified (3048F-8P)<br />
3) High Blood Pressure Control in Type 1 or 2 Diabetes Mellitus - Percentage <strong>of</strong> patients aged 18-75<br />
years with diabetes (type 1 or type 2) who had most recent blood pressure in control (less than 140/80 mm Hg) -<br />
This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period for patients seen during the <strong>reporting</strong> period.<br />
The performance period for this <strong>measure</strong> is 12 months. It is anticipated that clinicians who provide services for the<br />
primary management <strong>of</strong> diabetes mellitus will submit this <strong>measure</strong>.<br />
ICD-9: 250.00-250.93, 648.00-648.04 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit); 99341-99350 (home visit); 99304-99310 (nursing<br />
facility); 99324-99337 (domiciliary); 97802-97804 <strong>and</strong> G0270-G0271 (nutrition therapy)<br />
Systolic codes<br />
_____ Most recent systolic blood pressure < 130 mm Hg (3074F)<br />
_____ Most recent systolic blood pressure 130 to 139 mm Hg (3075F)<br />
_____ Most recent systolic blood pressure > 140 mm Hg (3077F)<br />
AND<br />
Diastolic codes<br />
_____ Most recent diastolic blood pressure < 80 mm Hg (3078F)<br />
_____ Most recent diastolic blood pressure 80-89 mm Hg (3079F)<br />
_____ Most recent diastolic blood pressure > 90 mm Hg (3080F)<br />
OR<br />
_____<br />
Blood pressure <strong>measure</strong>ment not performed, reason not specified (2000F-8P)<br />
4) Screening for Future Fall Risk - Percentage <strong>of</strong> patients aged 65 years <strong>and</strong> older who were screened for<br />
future fall risk (patients are considered at risk for future falls if they have had 2 or more falls in the past year or any<br />
fall with injury in the past year) at least once within 12 months - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once<br />
per <strong>reporting</strong> period for patients seen during the <strong>reporting</strong> period. This <strong>measure</strong> is appropriate for use in all nonacute<br />
settings (excludes emergency departments <strong>and</strong> acute care hospitals). It is anticipated that clinicians who<br />
provide primary care for the patient will submit this <strong>measure</strong>.<br />
ICD-9: None specified - CPT: 97001-97004 (PT eval); 99201-99215 (<strong>of</strong>fice/outpatient visit), 99304-99310 (nursing facility), 99324-99328<br />
(domiciliary), 99334-99337 (domiciliary), 99341-99350 (home visits), 99387 <strong>and</strong> 99397 (preventive), 99401-99404 (preventive counseling),<br />
Definition: A fall is defined as a sudden, unintentional change in position causing an individual to l<strong>and</strong> at a lower<br />
level, on an object, the floor, or the ground, other than as a consequence <strong>of</strong> sudden onset <strong>of</strong> paralysis, epileptic<br />
seizure, or overwhelming external force (Tinetti).<br />
_____<br />
_____<br />
_____<br />
_____<br />
Screening for future fall risk; documentation <strong>of</strong> 2 or more falls in the past year or any fall with injury in the<br />
past year (1100F)<br />
Screening for future fall risk; documentation <strong>of</strong> no falls in the past year or only 1 fall without injury in the<br />
past year (1101F)<br />
Screening for future fall risk not performed for medical reasons (1100F-1P)<br />
Screening for future fall risk not performed, reason not specified (1100F-8P)<br />
5) Heart Failure: Angiotensin-Converting Enzyme (ACE) Inhibitor or Angiotensin Receptor<br />
Blocker (ARB) Therapy for Left Ventricular Systolic Dysfunction (LVSD) - Percentage <strong>of</strong> patients aged<br />
18 years <strong>and</strong> older with a diagnosis <strong>of</strong> heart failure <strong>and</strong> left ventricular systolic dysfunction (LVSD) who were<br />
prescribed ACE inhibitor or ARB therapy - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period<br />
for all heart failure patients seen during the <strong>reporting</strong> period. The left ventricular systolic dysfunction may be<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.<br />
5-5
determined by quantitative or qualitative assessment. Examples <strong>of</strong> a quantitative or qualitative assessment may<br />
include an echocardiogram: 1) that provides a numerical value <strong>of</strong> left ventricular systolic dysfunction or 2) that uses<br />
descriptive terms such as moderately or severely depressed left ventricular dysfunction. It is anticipated that<br />
clinicians who provide primary management <strong>of</strong> patients with heart failure will submit this <strong>measure</strong>.<br />
ICD-9: 402.01, 402.11, 402.91; 404.01, 404.03, 404.11, 404.13, 404.91, 404.93; 428.0, 428.1, 428.20-428.23, 428.30-428.33, 428.40-428.43,<br />
428.9 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99238, 99239 (discharge), 99241-99245 (<strong>of</strong>fice/outpatient consult), 99304-99310<br />
(nursing facility), 99324-99337 (domiciliary), 99341-99350 (home visit)<br />
_____<br />
OR<br />
_____<br />
_____<br />
_____<br />
AND<br />
_____<br />
_____<br />
_____<br />
ACE inhibitor or ARB therapy prescribed <strong>and</strong> left ventricular ejection fraction (LVEF)
_____<br />
_____<br />
_____<br />
_____<br />
_____<br />
Beta-blocker therapy prescribed (4006F)<br />
Documentation <strong>of</strong> medical reason(s) for not prescribing beta-blocker therapy (4006F-1P)<br />
Documentation <strong>of</strong> patient reason(s) for not prescribing beta-blocker therapy (4006F-2P)<br />
Documentation <strong>of</strong> system reason(s) for not prescribing beta-blocker therapy (4006F-3P)<br />
Beta-blocker therapy not prescribed, reason not specified (4006F-8P)<br />
8) Heart Failure: Beta-blocker Therapy for Left Ventricular Systolic Dysfunction - Percentage <strong>of</strong><br />
patients aged 18 years <strong>and</strong> older with a diagnosis <strong>of</strong> heart failure who also have left ventricular systolic dysfunction<br />
(LVSD) <strong>and</strong> who were prescribed beta-blocker therapy - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once per<br />
<strong>reporting</strong> period for all heart failure patients seen during the <strong>reporting</strong> period. The left ventricular systolic<br />
dysfunction may be determined by quantitative or qualitative assessment. Examples <strong>of</strong> a quantitative or qualitative<br />
assessment may include an echocardiogram: 1) that provides a numerical value <strong>of</strong> left ventricular systolic<br />
dysfunction or 2) that uses descriptive terms such as moderately or severely depressed left ventricular dysfunction. It<br />
is anticipated that clinicians who provide primary management <strong>of</strong> patients with heart failure will submit this<br />
<strong>measure</strong>.<br />
ICD-9: 402.01, 402.11, 402.91; 404.01, 404.03, 404.11, 404.13, 404.91, 404.93; 428.0, 428.1, 428.20-428.23, 428.30-428.33, 428.40-428.43,<br />
428.9 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice/outpatient consult), 99341-99350 (home visit), 99304-99310<br />
(nursing facility), 99324-99337 (domiciliary)<br />
_____<br />
Beta blocker therapy prescribed <strong>and</strong> left ventricular ejection fraction (LVEF) < 40% or documentation <strong>of</strong><br />
moderately or severely depressed left ventricular systolic function (4006F <strong>and</strong> 3021F)<br />
OR<br />
_____<br />
_____<br />
_____<br />
Documentation <strong>of</strong> medical reason(s) for not prescribing beta-blocker therapy (4006F-1P)<br />
Documentation <strong>of</strong> patient reason(s) for not prescribing beta-blocker therapy (4006F-2P)<br />
Documentation <strong>of</strong> system reason(s) for not prescribing beta-blocker therapy (4006F-3P)<br />
AND<br />
_____<br />
_____<br />
_____<br />
Left ventricular ejection fraction (LVEF) < 40% or documentation <strong>of</strong> moderately or severely depressed left<br />
ventricular systolic function (3021F)<br />
Left ventricular ejection fraction (LVEF) ≥ 40% or documentation as normal or mildly depressed left<br />
ventricular systolic function (3022F)<br />
Left ventricular ejection fraction (LVEF) was not performed or documented, reason not otherwise specified<br />
(3021F-8P)<br />
OR<br />
_____<br />
Beta-blocker therapy was not prescribed, reason not otherwise specified <strong>and</strong> left ventricular ejection<br />
fraction (LVEF) < 40% or documentation <strong>of</strong> moderately or severely depressed left ventricular systolic<br />
function (4006F-8P <strong>and</strong> 3021F)<br />
9) Antidepressant Medication During Acute Phase for Patients with New Episode <strong>of</strong> Major<br />
Depression - Percentage <strong>of</strong> patients aged 18 years <strong>and</strong> older diagnosed with new episode <strong>of</strong> major depressive<br />
disorder (MDD) <strong>and</strong> documented as treated with antidepressant medication during the entire 84-day (12 week) acute<br />
treatment phase - This <strong>measure</strong> is to be reported for each occurrence <strong>of</strong> MDD during the <strong>reporting</strong> period. It is<br />
anticipated that clinicians who provide the primary management <strong>of</strong> patients with major depressive disorder (MDD)<br />
will submit this <strong>measure</strong>.<br />
ICD-9: 296.20-296.24, 296.30-296.34, 298.0, 300.4, 309.1, 311 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit); 90801, 90802, 90804-90809,<br />
90862 (psychiatry)<br />
Definition: A “new episode” is defined as a patient with major depression who has not been seen or treated for<br />
major depression by any practitioner in the prior 4 months. A new episode can either be a recurrence for a patient<br />
with prior major depression or a patient with a new onset <strong>of</strong> major depression.<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.<br />
5-7
Report G8126: 1) For all patients with a diagnosis <strong>of</strong> Major Depression, New Episode who were prescribed a full<br />
12 week course <strong>of</strong> antidepressant medication OR 2) At the completion <strong>of</strong> a 12 week course <strong>of</strong> antidepressant<br />
medication.<br />
_____<br />
_____<br />
_____<br />
Patient with new episode <strong>of</strong> MDD documented as being treated with antidepressant medication during the<br />
entire 12 week acute treatment phase (G8126)<br />
Patient with new episode <strong>of</strong> MDD not documented as being treated with antidepressant medication during<br />
the entire 12 week acute treatment phase (G8127)<br />
Clinician documented that patient with a new episode <strong>of</strong> MDD was not an eligible c<strong>and</strong>idate for<br />
antidepressant medication treatment or patient did not have a new episode <strong>of</strong> MDD (G8128)<br />
39) Screening or Therapy for Osteoporosis for Women Aged 65 Years <strong>and</strong> Older - Percentage <strong>of</strong><br />
female patients aged 65 years <strong>and</strong> older who have a central dual-energy X-ray absorptiometry (DXA) <strong>measure</strong>ment<br />
ordered or performed at least once since age 60 or pharmacologic therapy prescribed within 12 months - This<br />
<strong>measure</strong> is to be reported a minimum <strong>of</strong> once during the <strong>reporting</strong> period for patients seen during the <strong>reporting</strong><br />
period. Female patients aged 65 years <strong>and</strong> older should have a central DXA <strong>measure</strong>ment ordered or performed at<br />
least once since the time they turned 60 years or have pharmacologic therapy prescribed to prevent or treat<br />
osteoporosis. It is anticipated that clinicians who provide primary care or care for treatment <strong>of</strong> fracture or<br />
osteoporosis will submit this <strong>measure</strong>.<br />
ICD-9: No specific diagnosis codes <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99387 <strong>and</strong> 99397 (preventive), 99401-99404 (preventive<br />
counseling)<br />
Definition: Pharmacologic Therapy: U.S. Food <strong>and</strong> Drug Administration approved pharmacologic options for<br />
osteoporosis prevention <strong>and</strong>/or treatment <strong>of</strong> postmenopausal osteoporosis include, in alphabetical order:<br />
bisphosphonates (alendronate, ib<strong>and</strong>ronate, <strong>and</strong> risedronate), calcitonin, estrogens (estrogens <strong>and</strong>/or hormone<br />
therapy), parathyroid hormone [PTH (1-34), teriparatide], <strong>and</strong> selective estrogen receptor modules or SERMs<br />
(raloxifene).<br />
_____<br />
_____<br />
_____<br />
_____<br />
_____<br />
_____<br />
_____<br />
Central Dual-energy X-Ray Absorptiometry (DXA) ordered (3096F)<br />
Central Dual-energy X-Ray Absorptiometry (DXA) results documented (3095F)<br />
Pharmacologic therapy (other than minerals/vitamins) for osteoporosis prescribed (4005F)<br />
Documentation <strong>of</strong> medical reason(s) for not ordering or performing a central dual energy X-ray<br />
absorptiometry (DXA) <strong>measure</strong>ment or not prescribing pharmacologic therapy for osteoporosis (3096F-1P)<br />
Documentation <strong>of</strong> patient reason(s) for not ordering or performing central dual energy X-ray<br />
absorptiometry (DXA) <strong>measure</strong>ment or not prescribing pharmacologic therapy for osteoporosis (3096F-2P)<br />
Documentation <strong>of</strong> system reason(s) for not ordering or performing central dual energy X-ray<br />
absorptiometry (DXA) <strong>measure</strong>ment or not prescribing pharmacologic therapy for osteoporosis (3096F-3P)<br />
Central dual energy X-ray absorptiometry (DXA) <strong>measure</strong>ment was not ordered or performed <strong>and</strong> a<br />
pharmacologic therapy for osteoporosis was not prescribed reason not otherwise specified (3096F-8P)<br />
40) Osteoporosis: Management Following Fracture - Percentage <strong>of</strong> patients aged 50 years <strong>and</strong> older with<br />
fracture <strong>of</strong> the hip, spine, or distal radius who had a central dual-energy X-ray absorptiometry (DXA) <strong>measure</strong>ment<br />
ordered or performed or pharmacologic therapy prescribed - This <strong>measure</strong> is to be reported after each occurrence <strong>of</strong><br />
a fracture during the <strong>reporting</strong> period. Patients with a fracture <strong>of</strong> the hip, spine, or distal radius should have a central<br />
DXA <strong>measure</strong>ment ordered or performed or pharmacologic therapy prescribed. The management (DXA ordered or<br />
performed or pharmacologic therapy prescribed) should occur within three months <strong>of</strong> the initial visit with the<br />
<strong>reporting</strong> clinician following the fracture. Patients with documentation <strong>of</strong> prior central DXA <strong>measure</strong>ment or already<br />
receiving pharmacologic therapy would automatically meet the intent <strong>of</strong> this <strong>measure</strong>. It is anticipated that clinicians<br />
who manage the primary or ongoing care for osteoporosis or osteoporosis related fracture(s) will submit this<br />
<strong>measure</strong>.<br />
ICD-9: 733.12-733.14, 805.00-805.08, 805.10-805.18, 805.2, 805.4, 805.6, 805.8, 813.40-813.42, 813.44, 813.45, 813.50-813.52, 813.54,<br />
820.00-820.03, 820.09-820.11, 820.20-820.22, 820.13. 820.8, 820.9 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice<br />
consult)<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.<br />
5-8
Definition: Pharmacologic Therapy: U.S. Food <strong>and</strong> Drug Administration approved pharmacologic options for<br />
osteoporosis prevention <strong>and</strong>/or treatment <strong>of</strong> postmenopausal osteoporosis include, in alphabetical order:<br />
bisphosphonates (alendronate, ib<strong>and</strong>ronate, <strong>and</strong> risedronate), calcitonin, estrogens (estrogens <strong>and</strong>/or hormone<br />
therapy), parathyroid hormone [PTH (1-34), teriparatide], <strong>and</strong> selective estrogen receptor modules or SERMs<br />
(raloxifene).<br />
_____<br />
_____<br />
_____<br />
_____<br />
_____<br />
_____<br />
_____<br />
Central dual energy X-ray absorptiometry (DXA) ordered (3096F)<br />
Central dual energy X-ray absorptiometry (DXA) results documented (3095F)<br />
Pharmacologic therapy (other than minerals/vitamins) for osteoporosis prescribed (4005F)<br />
Documentation <strong>of</strong> medical reason(s) for not ordering or performing a central dual energy X-ray<br />
absorptiometry (DXA) <strong>measure</strong>ment or not prescribing pharmacologic therapy for osteoporosis (3096F-1P)<br />
Documentation <strong>of</strong> patient reason(s) for not ordering or performing a central dual energy X-ray<br />
absorptiometry (DXA) <strong>measure</strong>ment or not prescribing pharmacologic therapy for osteoporosis (3096F-2P)<br />
Documentation <strong>of</strong> system reason(s) for not ordering or performing a central dual energy X-ray<br />
absorptiometry (DXA) <strong>measure</strong>ment or not prescribing pharmacologic therapy for osteoporosis (3096F-3P)<br />
Central dual energy X-ray absorptiometry (DXA) <strong>measure</strong>ment was not ordered or performed <strong>and</strong> a<br />
pharmacologic therapy for osteoporosis was not prescribed reason not otherwise specified (3096F-8P)<br />
41) Osteoporosis: Pharmacologic Therapy - Percentage <strong>of</strong> patients aged 50 years <strong>and</strong> older with a diagnosis<br />
<strong>of</strong> osteoporosis who were prescribed pharmacologic therapy within 12 months - This <strong>measure</strong> is to be reported a<br />
minimum <strong>of</strong> once per <strong>reporting</strong> period for patients seen during the <strong>reporting</strong> period. Patients with a diagnosis <strong>of</strong><br />
osteoporosis should be prescribed pharmacologic therapy to treat osteoporosis. It is anticipated that clinicians who<br />
provide services for patients with the diagnosis <strong>of</strong> osteoporosis will submit this <strong>measure</strong>.<br />
ICD-9: 733.00-733.03, 733.09 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice/outpatient consult), 99386-99387 <strong>and</strong><br />
99396- 99397 (preventive), 99401-99404 (preventive counseling)<br />
Definition: Pharmacologic Therapy: U.S. Food <strong>and</strong> Drug Administration approved pharmacologic options for<br />
osteoporosis prevention <strong>and</strong>/or treatment <strong>of</strong> postmenopausal osteoporosis include, in alphabetical order:<br />
bisphosphonates (alendronate, ib<strong>and</strong>ronate, <strong>and</strong> risedronate), calcitonin, estrogens (estrogens <strong>and</strong>/or hormone<br />
therapy), parathyroid hormone [PTH (1-34), teriparatide], <strong>and</strong> selective estrogen receptor modules or SERMs<br />
(raloxifene).<br />
_____<br />
_____<br />
1P)<br />
_____<br />
_____<br />
_____<br />
Pharmacologic therapy (other than minerals/vitamins) for osteoporosis prescribed (4005F)<br />
Documentation <strong>of</strong> medical reason(s) for not prescribing pharmacologic therapy for osteoporosis (4005F-<br />
Documentation <strong>of</strong> patient reason(s) for not prescribing pharmacologic therapy for osteoporosis (4005F-2P)<br />
Documentation <strong>of</strong> system reason for not prescribing pharmacologic therapy for osteoporosis (4005F-3P)<br />
Pharmacologic therapy for osteoporosis was not prescribed reason not otherwise specified (4005F-8P)<br />
42) Osteoporosis: Counseling for Vitamin D, Calcium Intake, <strong>and</strong> Exercise - Percentage <strong>of</strong> patients,<br />
regardless <strong>of</strong> age, with a diagnosis <strong>of</strong> osteoporosis who are either receiving both calcium <strong>and</strong> vitamin D or have<br />
been counseled regarding both calcium <strong>and</strong> vitamin D intake, <strong>and</strong> exercise at least once within 12 months - This<br />
<strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period for patients seen during the <strong>reporting</strong> period.<br />
Patients with a diagnosis <strong>of</strong> osteoporosis should be receiving both calcium <strong>and</strong> vitamin D or had counseling<br />
regarding their use <strong>and</strong> counseled on exercise. It is anticipated that clinicians who provide services for patients with<br />
the diagnosis <strong>of</strong> osteoporosis will submit this <strong>measure</strong>.<br />
ICD-9: 733.00-733.03, 733.09 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice/outpatient consult), 99385-99387 <strong>and</strong><br />
99395-99397 (preventive), 99401-99404 (preventive counseling)<br />
_____<br />
_____<br />
_____<br />
Documentation <strong>of</strong> receipt <strong>of</strong> counseling on exercise AND either both calcium <strong>and</strong> vitamin D use or<br />
counseling regarding both calcium <strong>and</strong> vitamin D use (4019F)<br />
Documentation <strong>of</strong> medical reason(s) for patient not receiving both calcium <strong>and</strong> vitamin D or <strong>and</strong> not<br />
needing counseling regarding both calcium <strong>and</strong> vitamin D intake, <strong>and</strong> exercise (e.g., patient has dementia<br />
<strong>and</strong> is unable to receive counseling) (4019F-1P)<br />
Receipt <strong>of</strong> counseling on exercise AND either both calcium <strong>and</strong> vitamin D use or counseling regarding<br />
both calcium <strong>and</strong> vitamin D use was not documented reason not otherwise specified (4019F-8P)<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.<br />
5-9
46) Medication Reconciliation - Percentage <strong>of</strong> patients aged 65 years <strong>and</strong> older discharged from any inpatient<br />
facility (e.g., hospital, skilled nursing facility, or rehabilitation facility) <strong>and</strong> seen within 60 days following discharge<br />
in the <strong>of</strong>fice by the physician providing on-going care who had a reconciliation <strong>of</strong> the discharge medications with<br />
the current medication list in the medical record documented - This <strong>measure</strong> is to be reported at an <strong>of</strong>fice visit<br />
occurring within 60 days <strong>of</strong> each inpatient facility discharge during the <strong>reporting</strong> period. This <strong>measure</strong> is appropriate<br />
for use in the ambulatory setting only. It is anticipated that clinicians who provide primary on-going care will submit<br />
this <strong>measure</strong> when a patient is seen in the <strong>of</strong>fice within 60 days following discharge from any inpatient facility. If a<br />
patient has not been discharged within the 60-day timeframe from an inpatient facility, there are no <strong>reporting</strong><br />
requirements for this <strong>measure</strong>.<br />
ICD-9: No specific diagnosis code <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99387 <strong>and</strong> 99397 (preventive), 99401-99404 (preventive<br />
counseling)<br />
_____<br />
_____<br />
Patient discharged from an inpatient facility within the last 60 days <strong>and</strong> discharge medications reconciled<br />
with the current medication list in outpatient medical record (1110F <strong>and</strong> 1111F)<br />
Patient discharged from an inpatient facility within the last 60 days <strong>and</strong> discharge medication not<br />
reconciled with current medication list in the medical record, reason not specified (1110F <strong>and</strong> 1111F-8P)<br />
47) Advance Care Plan - Percentage <strong>of</strong> patients aged 65 years <strong>and</strong> older with documentation <strong>of</strong> a surrogate<br />
decision-maker or advance care plan in the medical record - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once per<br />
<strong>reporting</strong> period for patients seen during the <strong>reporting</strong> period. This <strong>measure</strong> is appropriate for use in all healthcare<br />
settings. It is anticipated that clinicians who provide primary care services for the patient will submit this <strong>measure</strong>.<br />
ICD-9: No specific diagnosis codes <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99218-99220 (observation services), 99221-99223 (initial<br />
inpatient), 99231-99233 (subsequent inpatient), 99234-99236 (admit <strong>and</strong> discharge on the same day), 99281-99285 (ED services), 99291<br />
(critical care), 99304-99310 (nursing facility), 99324-99337 (domiciliary/rest home), 99341-99350 (home visits), 99387 <strong>and</strong> 99397<br />
(preventive services), 99401-99404 (preventive counseling)<br />
_____<br />
_____<br />
_____<br />
Surrogate decision maker or advance care plan documented in the medical record (1080F)<br />
Surrogate decision maker or advance directive not documented for patient reasons (1080F-2P)<br />
Surrogate decision maker or advance directive not documented, reason not specified (1080F-8P)<br />
(Joy’s Comment: For successful <strong>reporting</strong> <strong>of</strong> this <strong>measure</strong>, primary care physicians will have to report on this<br />
<strong>measure</strong> at least one time for every Medicare patient.)<br />
48) Assessment <strong>of</strong> Presence or Absence <strong>of</strong> Urinary Incontinence in Women Aged 65 Years <strong>and</strong><br />
Older - Percentage <strong>of</strong> female patients aged 65 years <strong>and</strong> older who were assessed for the presence or absence <strong>of</strong><br />
urinary incontinence within 12 months - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period for<br />
patients seen during the <strong>reporting</strong> period. This <strong>measure</strong> is appropriate for use in the ambulatory setting only. It is<br />
anticipated that clinicians who provide primary care for the patient will submit this <strong>measure</strong>.<br />
ICD-9: No specific codes <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99387 <strong>and</strong> 99397 (preventive), 99401-99404 (preventive<br />
counseling)<br />
Definition: Urinary incontinence is defined as any involuntary leakage <strong>of</strong> urine.<br />
_____<br />
_____<br />
_____<br />
Presence or absence <strong>of</strong> urinary incontinence assessed (1090F)<br />
Presence or absence <strong>of</strong> urinary incontinence not assessed for medical reasons (1090F-1P)<br />
Presence or absence <strong>of</strong> urinary incontinence not assessed reason not specified (1090F-8P)<br />
49) Characterization <strong>of</strong> Urinary Incontinence in Women Aged 65 Years <strong>and</strong> Older - Percentage <strong>of</strong><br />
female patients aged 65 years <strong>and</strong> older with a diagnosis <strong>of</strong> urinary incontinence whose urinary incontinence was<br />
characterized at least once within 12 months - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong><br />
period for patients seen during the <strong>reporting</strong> period. This <strong>measure</strong> is appropriate for use in the ambulatory setting<br />
only. It is anticipated that clinicians who provide services for patients with the diagnosis <strong>of</strong> urinary incontinence will<br />
submit this <strong>measure</strong>.<br />
ICD-9: 307.6, 625.6, 788.30-788.39 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice/outpatient consult), 99387 <strong>and</strong> 99397<br />
(preventive), 99401-99404 (preventive counseling)<br />
5-10<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
Definition: Characterization includes, but is not limited to, (frequency, volume, timing, type <strong>of</strong> symptoms, how<br />
bothersome)<br />
_____<br />
_____<br />
Urinary incontinence characterized (1091F)<br />
Urinary incontinence not characterized reason not specified (1091F-8P)<br />
50) Plan <strong>of</strong> Care for Urinary Incontinence in Women Aged 65 Years <strong>and</strong> Older - Percentage <strong>of</strong> female<br />
patients aged 65 years <strong>and</strong> older with a diagnosis <strong>of</strong> urinary incontinence with a documented plan <strong>of</strong> care for urinary<br />
incontinence at least once within 12 months - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period<br />
for patients seen during the <strong>reporting</strong> period. This <strong>measure</strong> is appropriate for use in the ambulatory setting only. It is<br />
anticipated that clinicians who provide services for patients with the diagnosis <strong>of</strong> urinary incontinence will submit<br />
this <strong>measure</strong>.<br />
ICD-9: 307.6, 625.6, 788.30-788.39 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice/outpatient consult), 99387 <strong>and</strong> 99397<br />
(preventive), 99401-99404 (preventive counseling)<br />
Definition: Plan <strong>of</strong> care may include behavioral interventions (e.g., bladder training, pelvic floor muscle training,<br />
prompted voiding), referral to specialist, surgical treatment, reassess at follow-up visit, lifestyle interventions,<br />
addressing co-morbid factors, modification or discontinuation <strong>of</strong> medications contributing to urinary incontinence,<br />
or pharmacologic therapy.<br />
_____<br />
_____<br />
Urinary incontinence plan <strong>of</strong> care documented (0509F)<br />
Plan <strong>of</strong> care for urinary incontinence not documented reason not specified (0509F-8P)<br />
51) Chronic Obstructive Pulmonary Disease (COPD): Spirometry Evaluation - Percentage <strong>of</strong> patients<br />
aged 18 years <strong>and</strong> older with a diagnosis <strong>of</strong> COPD who had spirometry evaluation results documented - This<br />
<strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period using the most recent spirometry results in the<br />
patient record for patients seen during the <strong>reporting</strong> period. It is anticipated that clinicians who provide primary care<br />
services for the patient will submit this <strong>measure</strong>.<br />
ICD-9: 491.0, 491.1, 491.20-491.22, 491.8, 491.9, 492.0, 492.8, 496 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245<br />
(<strong>of</strong>fice/outpatient consult), 99385-99387, 99395-99397 (preventive), 99401-99404 (preventive counseling)<br />
Instructions: Look for most recent documentation <strong>of</strong> spirometry evaluation results in the medical record; do not<br />
limit the search to the <strong>reporting</strong> period.<br />
_____<br />
_____<br />
_____<br />
_____<br />
_____<br />
Spirometry results documented <strong>and</strong> reviewed (3023F)<br />
Spirometry results not documented medical reason(s) (3023F-1P)<br />
Spirometry results not documented for patient reasons (3023F-2P)<br />
Spirometry results not documented for system reasons (3023F-3P)<br />
Spirometry results not documented, reason not specified (3023F-8P)<br />
52) Chronic Obstructive Pulmonary Disease (COPD): Bronchodilator Therapy - Percentage <strong>of</strong> patients<br />
aged 18 years <strong>and</strong> older with a diagnosis <strong>of</strong> COPD <strong>and</strong> who have an FEV1/FVC less than 70% <strong>and</strong> have symptoms<br />
who were prescribed an inhaled bronchodilator - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong><br />
period for all COPD patients seen during the <strong>reporting</strong> period. It is anticipated that clinicians who provide primary<br />
care services for the patient will submit this <strong>measure</strong>.<br />
ICD-9: 491.0, 491.1, 491.20-491.22, 491.8, 491.9, 492.0, 492.8, 496 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245<br />
(<strong>of</strong>fice/outpatient consult), 99385-99387, 99395-99397 (preventive), 99401-99404 (preventive counseling)<br />
_____<br />
_____<br />
_____<br />
Inhaled bronchodilator prescribed <strong>and</strong> spirometry test results demonstrate FEV 1 /FVC < 70% with COPD<br />
symptoms (e.g., dyspnea, cough/sputum, wheezing) (4025F <strong>and</strong> 3025F)<br />
Documentation <strong>of</strong> medical reason(s) for not prescribing an inhaled bronchodilator <strong>and</strong> spirometry test<br />
results demonstrate FEV 1 /FVC < 70% with COPD symptoms (e.g., dyspnea, cough/sputum, wheezing)<br />
(4025F-1P <strong>and</strong> 3025F)<br />
Documentation <strong>of</strong> patient reason(s) for not prescribing an inhaled bronchodilator <strong>and</strong> spirometry test results<br />
demonstrate FEV 1 /FVC < 70% with COPD symptoms (e.g., dyspnea, cough/sputum, wheezing) (4025F-2P<br />
<strong>and</strong> 3025F)<br />
5-11<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
_____<br />
_____<br />
_____<br />
_____<br />
Documentation <strong>of</strong> system reason(s) for not prescribing an inhaled bronchodilator <strong>and</strong> spirometry test results<br />
demonstrate FEV 1 /FVC < 70% with COPD symptoms (e.g., dyspnea, cough/sputum, wheezing) (4025F-3P<br />
<strong>and</strong> 3025F)<br />
Spirometry results demonstrate FEV 1 /FVC ≥ 70% or patient does not have COPD symptoms (3027F)<br />
Spirometry test not performed or documented (3025F-8P)<br />
Inhaled bronchodilator not prescribed, reason not specified <strong>and</strong> spirometry test results demonstrate<br />
FEV 1 /FVC < 70% with COPD symptoms (e.g., dyspnea, cough/sputum, wheezing) (4025F-8P <strong>and</strong> 3025F)<br />
53) Asthma: Pharmacologic Therapy - Percentage <strong>of</strong> patients aged 5 to 40 years with a diagnosis <strong>of</strong> mild,<br />
moderate, or severe persistent asthma who were prescribed either the preferred long-term control medication<br />
(inhaled corticosteroid) or an acceptable alternative treatment - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once<br />
per <strong>reporting</strong> period for all asthma patients seen during the <strong>reporting</strong> period. It is anticipated that clinicians who<br />
provide primary care services for the patient will submit this <strong>measure</strong>.<br />
ICD-9: 493.00-493.02, 493.10-493.12, 493.20-493.22, 493.81, 493.82, 493.90, 493.92 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-<br />
99245 (<strong>of</strong>fice/outpatient consult), 99383-99386, 99393-99396 (preventive), 99401-99404 (preventive counseling)<br />
Definition: acceptable alternative treatment (leukotriene modifiers, cromolyn sodium, nedocromil sodium, or<br />
sustained-released methylxanthines)<br />
_____<br />
_____<br />
_____<br />
_____<br />
Persistent asthma (mild, moderate, or severe) <strong>and</strong> preferred long term control medication or acceptable<br />
alternative treatment prescribed (4015F <strong>and</strong> 1038F)<br />
Persistent asthma (mild, moderate, or severe) <strong>and</strong> preferred long-term control medication or acceptable<br />
alternative treatment not prescribed for patient reasons (4015F-2P <strong>and</strong> 1038F)<br />
Intermittent asthma (1039F)<br />
Persistent asthma (mild, moderate, or severe) <strong>and</strong> preferred long-term control medication or acceptable<br />
alternative treatment not prescribed, reason not specified (4015F-8P <strong>and</strong> 1038F)<br />
60) Gastroesophageal Reflux Disease (GERD): Assessment for Alarm Symptoms - Percentage <strong>of</strong><br />
patients aged 18 years <strong>and</strong> older with a diagnosis <strong>of</strong> GERD, seen for an initial evaluation, who were assessed for the<br />
presence or absence <strong>of</strong> the following alarm symptoms: involuntary weight loss, dysphagia, <strong>and</strong> GI bleeding - This<br />
<strong>measure</strong> is to be reported once for all GERD patients seen during the <strong>reporting</strong> period. Patients seen for an initial<br />
evaluation <strong>of</strong> GERD should have documentation in the medical record <strong>of</strong> the presence or absence <strong>of</strong> alarm<br />
symptoms. If the initial evaluation <strong>of</strong> GERD occurred prior to the <strong>reporting</strong> period, report the proper CPT Category<br />
II code with modifier indicated in the numerator <strong>coding</strong> indicating this is not the initial evaluation. It is anticipated<br />
that clinicians who provide care for patients with GERD will submit this <strong>measure</strong>.<br />
ICD-9: 530.81, 530.10-530.12, 530.19 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice/outpatient consult)<br />
Definition: Patients assessed for the presence or absence <strong>of</strong> the following alarm symptoms: involuntary weight loss,<br />
dysphagia, <strong>and</strong> GI bleeding<br />
_____<br />
_____<br />
_____<br />
_____<br />
_____<br />
Alarm symptoms assessed; none present (1070F)<br />
Alarm symptoms assessed; one or more present (1071F)<br />
Patient does not meet denominator inclusion because the initial evaluation <strong>of</strong> GERD occurred prior to the<br />
<strong>reporting</strong> period (1070F-8P)<br />
Alarm symptoms not assessed for medical reasons (1070F-1P)<br />
Alarm symptoms not assessed, reason not specified (1071F-8P)<br />
(Joy’s Comment: For successful <strong>reporting</strong> <strong>of</strong> this <strong>measure</strong>, physicians will have to report on this <strong>measure</strong> at least<br />
one time for every Medicare patient with GERD.)<br />
61) Gastroesophageal Reflux Disease (GERD): Upper Endoscopy for Patients with Alarm<br />
Symptoms - Percentage <strong>of</strong> patients aged 18 years <strong>and</strong> older with a diagnosis <strong>of</strong> GERD, seen for an initial<br />
evaluation, with at least one alarm symptom who were either referred for upper endoscopy or had an upper<br />
endoscopy performed - This <strong>measure</strong> is to be reported once for all GERD patients seen during the <strong>reporting</strong> period.<br />
Patients seen for an initial evaluation <strong>of</strong> GERD <strong>and</strong> at least one alarm symptom will be referred for upper endoscopy<br />
or have an upper endoscopy performed. If the initial evaluation <strong>of</strong> GERD occurred prior to the <strong>reporting</strong> period,<br />
5-12<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
eport the proper CPT II Category II code with modifier indicated in the numerator <strong>coding</strong> indicating this is not the<br />
initial evaluation. It is anticipated that clinicians who provide care for patients with GERD will submit this <strong>measure</strong>.<br />
ICD-9: 530.81, 530.10-530.12, 530.19 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice/outpatient consult)<br />
Definition: Alarm symptoms for GERD include involuntary weight loss, dysphagia, <strong>and</strong> GI bleeding.<br />
_____ Upper gastrointestinal endoscopy performed (3130F)<br />
_____ Documentation <strong>of</strong> referral for upper gastrointestinal endoscopy (3132F <strong>and</strong> 1071F)<br />
_____ Patient does not have alarm symptoms (1070F)<br />
_____ Initial evaluation <strong>of</strong> GERD occurred prior to the <strong>reporting</strong> period (1071F-8P)<br />
_____ Upper endoscopy not performed or patient not referred for upper endoscopy for medical reasons (e.g.,<br />
patient has already had the procedure) (3130F-1P <strong>and</strong> 1071F)<br />
_____ Upper endoscopy not performed or patient not referred for upper endoscopy for patient reasons (3130F-2P<br />
<strong>and</strong> 1071F)<br />
_____ Upper endoscopy not performed or patient not referred for upper endoscopy for system reasons (3130F-3P<br />
<strong>and</strong> 1071F)<br />
_____ Upper endoscopy not performed or patient not referred for upper endoscopy, reason not specified (3130F-<br />
8P <strong>and</strong> 1071F)<br />
(Joy’s Comment: For successful <strong>reporting</strong> <strong>of</strong> this <strong>measure</strong>, physicians will have to report on this <strong>measure</strong> <strong>and</strong><br />
<strong>measure</strong> #60 at least one time for every Medicare patient with GERD.)<br />
63) Gastroesophageal Reflux Disease (GERD): Barium Swallow- Inappropriate Use - Percentage <strong>of</strong><br />
patients aged 18 years <strong>and</strong> older with a diagnosis <strong>of</strong> GERD, seen for an initial evaluation, who did not have a<br />
Barium swallow test ordered - This <strong>measure</strong> is to be reported once for all GERD patients seen during the <strong>reporting</strong><br />
period. Patients being seen for an initial evaluation <strong>of</strong> GERD should not receive a barium swallow test. If the initial<br />
evaluation <strong>of</strong> GERD occurred prior to the <strong>reporting</strong> period, report the proper CPT Category II with modifier<br />
indicated in the numerator <strong>coding</strong> indicating this is not the initial evaluation. It is anticipated that clinicians who<br />
provide care for patients with GERD will submit this <strong>measure</strong>.<br />
ICD-9: 530.81, 530.10-530.12, 530.19 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-99245 (<strong>of</strong>fice/outpatient consult)<br />
Definitions: This is an overuse <strong>measure</strong>. For performance, the numerator will be calculated as the difference<br />
between patients in the denominator <strong>and</strong> patients for whom a CPT Category II code was reported for barium<br />
swallow test ordered. A higher score indicates appropriate treatment <strong>of</strong> patients with GERD (i.e., the proportion for<br />
whom a barium swallow test was not ordered).<br />
_____<br />
_____<br />
_____<br />
_____<br />
Barium swallow test ordered (3142F)<br />
Patient does not meet denominator inclusion because the initial evaluation <strong>of</strong> GERD occurred prior to the<br />
<strong>reporting</strong> period (3200F-8P)<br />
Barium swallow test ordered for medical reasons (3142F-1P)<br />
Barium swallow test not ordered (3200F)<br />
(Joy’s Comment: For successful <strong>reporting</strong> <strong>of</strong> this <strong>measure</strong>, physicians will have to report on this <strong>measure</strong> <strong>and</strong><br />
<strong>measure</strong> #60 at least one time for every Medicare patient with GERD.)<br />
64) Asthma Assessment - Percentage <strong>of</strong> patients aged 5 to 40 years with a diagnosis <strong>of</strong> asthma who were<br />
evaluated during at least one <strong>of</strong>fice visit within 12 months for the frequency (numeric) <strong>of</strong> daytime <strong>and</strong> nocturnal<br />
asthma symptoms - This <strong>measure</strong> is to be reported a minimum <strong>of</strong> once per <strong>reporting</strong> period for patients seen during<br />
the <strong>reporting</strong> period. It is anticipated that clinicians who provide primary care services for the patient with a<br />
diagnosis <strong>of</strong> asthma will submit this <strong>measure</strong>.<br />
ICD-9: 493.00-493.02, 493.10-493.12, 493.20-493.22, 493.81, 493.82, 493.90, 493.92 <strong>and</strong> CPT: 99201-99215 (<strong>of</strong>fice/outpatient visit), 99241-<br />
99245 (<strong>of</strong>fice/outpatient consult), 99383-99386, 99393-99396 (preventive), 99401-99404 (preventive counseling)<br />
Definitions: To be counted in calculations <strong>of</strong> this <strong>measure</strong>, symptom frequency must be numerically quantified.<br />
Measure may also be met by clinician documentation or patient completion <strong>of</strong> an asthma assessment<br />
5-13<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
tool/survey/questionnaire. Assessment tool may include the Quality Metric Asthma Control Test, National Asthma<br />
Education & Prevention Program (NAEPP) Asthma Symptoms <strong>and</strong> Peak Flow Diary.<br />
_____<br />
_____<br />
Asthma symptoms evaluated (includes physician documentation <strong>of</strong> numeric frequency <strong>of</strong> symptoms or<br />
patient completion <strong>of</strong> an asthma assessment tool/survey/questionnaire) (1005F)<br />
Asthma symptom frequency not evaluated, reason not specified (1005F-8P)<br />
PAYMENT FOR EVALUATION AND MANAGEMENT SERVICES<br />
PROVIDED DURING GLOBAL PERIOD OF SURGERY<br />
Medicare Claims Processing Manual Chapter 12 §30.6.6 (Rev. 954, Issued: 05-19-06, Effective: 06-01-<br />
06, Implementation: 08-20-06)<br />
CPT Modifier -24 - Unrelated Evaluation <strong>and</strong> Management Service by Same Physician during<br />
Postoperative Period<br />
Carriers pay for an evaluation <strong>and</strong> management service other than inpatient hospital care before discharge<br />
from the hospital following surgery (CPT codes 99221-99238) if it was provided during the postoperative<br />
period <strong>of</strong> a surgical procedure, furnished by the same physician who performed the procedure, billed with<br />
CPT modifier -24, <strong>and</strong> accompanied by documentation that supports that the service is not related to the<br />
postoperative care <strong>of</strong> the procedure. They do not pay for inpatient hospital care that is furnished during<br />
the hospital stay in which the surgery occurred unless the doctor is also treating another medical condition<br />
that is unrelated to the surgery. All care provided during the inpatient stay in which the surgery occurred<br />
is compensated through the global surgical payment.<br />
CPT Modifier -25 - Significant Evaluation <strong>and</strong> Management Service by Same Physician on Date <strong>of</strong><br />
Global Procedure<br />
Medicare requires that Current Procedural Terminology (CPT) modifier -25 should only be used on<br />
claims for evaluation <strong>and</strong> management (E/M) services, <strong>and</strong> only when these services are provided by the<br />
same physician (or same qualified nonphysician practitioner) to the same patient on the same day as<br />
another procedure or other service. Carriers pay for an E/M service provided on the day <strong>of</strong> a procedure<br />
with a global fee period if the physician indicates that the service is for a significant, separately<br />
identifiable E/M service that is above <strong>and</strong> beyond the usual pre- <strong>and</strong> post-operative work <strong>of</strong> the<br />
procedure. Different diagnoses are not required for <strong>reporting</strong> the E/M service on the same date as the<br />
procedure or other service. Modifier -25 is added to the E/M code on the claim.<br />
Both the medically necessary E/M service <strong>and</strong> the procedure must be appropriately <strong>and</strong> sufficiently<br />
documented by the physician or qualified nonphysician practitioner in the patient’s medical record to<br />
support the claim for these services, even though the documentation is not required to be submitted with<br />
the claim.<br />
CPT Modifier -57 - Decision for Surgery Made Within Global Surgical Period<br />
Carriers pay for an evaluation <strong>and</strong> management service on the day <strong>of</strong> or on the day before a procedure<br />
with a 90-day global surgical period if the physician uses CPT modifier -57 to indicate that the service<br />
resulted in the decision to perform the procedure. Carriers may not pay for an evaluation <strong>and</strong> management<br />
service billed with the CPT modifier -57 if it was provided on the day <strong>of</strong> or the day before a procedure<br />
with a 0 or 10-day global surgical period.<br />
Payment for Evaluation <strong>and</strong> Management Services Provided During Global Period <strong>of</strong> Surgery<br />
• The Centers for Medicare & Medicaid Services (CMS) has clarified the documentation<br />
requirements <strong>and</strong> policy requirements for the use <strong>of</strong> CPT modifier -25 used with E/M services.<br />
Please refer to the manual attachment to CR5025, The Medicare Claims Processing Manual,<br />
Chapter 12, §30.6.6, for revisions regarding the use <strong>of</strong> CPT modifier -25<br />
5-14<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
• Physicians <strong>and</strong> qualified nonphysician practitioners (NPP) should use CPT modifier -25 to<br />
designate a significant, separately identifiable E/M service provided by the same<br />
physician/qualified NPP to the same patient on the same day as another procedure or other<br />
service with a global fee period.<br />
• Common Procedural Terminology (CPT) modifier -25 identifies a significant, separately<br />
identifiable evaluation <strong>and</strong> management (E/M) service. It should be used when the E/M service is<br />
above <strong>and</strong> beyond the usual pre- <strong>and</strong> postoperative work <strong>of</strong> a procedure with a global fee period<br />
performed on the same day as the E/M service.<br />
• Different diagnoses are not required for <strong>reporting</strong> the E/M service on the same date as the<br />
procedure or other service with a global fee period. Modifier -25 is added to the E/M code on the<br />
claim.<br />
• Both the medically necessary E/M service <strong>and</strong> the procedure must be appropriately <strong>and</strong><br />
sufficiently documented by the physician or qualified NPP in the patient’s medical record to<br />
support the need for modifier -25 on the claim for these services, even though the documentation<br />
is not required to be submitted with the claim.<br />
• Your Carrier will not retract payment for claims already paid or retroactively pay claims<br />
processed prior to the implementation <strong>of</strong> CR5025. But, they will adjust claims brought to their<br />
attention.<br />
• Carriers will not pay for an E/M service reported with a procedure having a global fee period<br />
unless CPT modifier -25 is appended to the E/M service to designate it as a significant <strong>and</strong><br />
separately identifiable E/M service from the procedure.<br />
PREOPERATIVE SERVICES<br />
§1862(a)(1)(A) <strong>of</strong> the Social Security Act requires that in order to qualify for Medicare coverage, a<br />
service must be reasonable <strong>and</strong> necessary for the diagnosis <strong>and</strong> treatment <strong>of</strong> illness or injury, or to<br />
improve the functioning <strong>of</strong> a malformed body member. A preoperative service performed due to hospital<br />
or malpractice protocol cannot supercede this guideline for Medicare coverage purposes. Medicare will<br />
pay for preoperative evaluation <strong>and</strong> management services, <strong>and</strong> diagnostic tests if they are medically<br />
necessary <strong>and</strong> meet the documentation requirements <strong>of</strong> the service rendered.<br />
CMS Transmittal #1707 – May 31, 2001<br />
A. General--This manual instruction addresses payment for preoperative services that are not included in<br />
the global surgery payment.<br />
B. Non-global Preoperative Services -- Consist <strong>of</strong> evaluation <strong>and</strong> management (E/M) services<br />
(preoperative examinations) that are not included in the global surgical package <strong>and</strong> diagnostic tests<br />
performed for the purpose <strong>of</strong> evaluating a patient's risk <strong>of</strong> perioperative complications <strong>and</strong> optimizing<br />
perioperative care. Medicare will pay for all medically necessary preoperative.<br />
C. Non-global Preoperative Examinations -- E/M services performed that are not included in the global<br />
surgical package for evaluating a patient's risk <strong>of</strong> perioperative complications <strong>and</strong> to optimize<br />
perioperative care. Preoperative examinations may be billed by using an appropriate CPT code (e.g.,<br />
new patient, established patient, or consultation). Such non-global preoperative examinations are<br />
payable if they are medically necessary <strong>and</strong> meet the documentation <strong>and</strong> other requirements for the<br />
service billed.<br />
D. Preoperative Diagnostic Tests -- Tests performed to determine a patient's perioperative risk <strong>and</strong><br />
optimize perioperative care. Preoperative diagnostic tests are payable if they are medically necessary<br />
<strong>and</strong> meet any other applicable requirements.<br />
5-15<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
E. Statutory Basis for Payment<br />
1. §1862(a)(7) <strong>of</strong> the Social Security Act (the Act) excludes payment for "routine physical<br />
checkups." Both physical examinations <strong>and</strong> diagnostic tests that are performed in the absence <strong>of</strong><br />
signs or symptoms <strong>of</strong> illness or injury may be denied as a routine physical checkup under<br />
§1862(a)(7) <strong>of</strong> the Act. The regulatory provision that further explains this policy is contained in<br />
42 CFR Part 411.15(a)(1).<br />
2. §1862(a)(1)(A) <strong>of</strong> the Act states that no payment will be made for "items or services which are<br />
not reasonable <strong>and</strong> necessary for the diagnosis or treatment <strong>of</strong> illness or injury or to improve the<br />
functioning <strong>of</strong> a malformed body member." Both physical examinations <strong>and</strong> diagnostic tests<br />
performed in the absence <strong>of</strong> signs or symptoms can be denied as unnecessary under<br />
§1862(a)(1)(A) <strong>of</strong> the Act.<br />
3. Through previous program <strong>and</strong> decision memor<strong>and</strong>a, Medicare has established a clear hierarchy<br />
in the application <strong>of</strong> these two statutory provisions for use in denying payment for physical<br />
examinations <strong>and</strong> diagnostic tests. Claims are initially evaluated against the statutory<br />
requirements <strong>of</strong> §1862(a)(7) <strong>of</strong> the Act <strong>and</strong>, if not denied on that basis, they are evaluated against<br />
the statutory requirements <strong>of</strong> §1862 (a)(1)(A). If they meet the statutory requirements <strong>of</strong><br />
§1862(a)(1)(A) <strong>of</strong> the Act, they are paid. In general, §1862(a)(1)(A) <strong>of</strong> the Act is to be invoked<br />
only for denying payment for services that are otherwise covered, <strong>and</strong> are not otherwise excluded<br />
from payment, but which are not covered in a particular case because they are not deemed<br />
"medically reasonable <strong>and</strong> necessary" when performed in that specific situation.<br />
F. Applicability <strong>of</strong> §1862(a)(7) <strong>of</strong> the Act to Preoperative Services<br />
1. Preoperative Examinations—For purposes <strong>of</strong> billing under the Physician Fee Schedule, medical<br />
preoperative examinations performed by, or at the request <strong>of</strong>, the attending surgeon do not fall<br />
within the statutory exclusion articulated in §1862(a)(7) <strong>of</strong> the Act. These examinations are<br />
payable if they are medically necessary (i.e., based on a determination <strong>of</strong> medical necessity under<br />
§1862(a)(1)(A) <strong>of</strong> the Act), <strong>and</strong> meet the documentation requirements <strong>of</strong> the service billed.<br />
Determination <strong>of</strong> the appropriate E/M code is based on the requirements <strong>of</strong> the specific type <strong>and</strong><br />
level <strong>of</strong> visit or consultation the physician submits on his claim (e.g., established patient, new<br />
patient, consultation).<br />
2. Preoperative Diagnostic Tests—When billing under the Physician Fee Schedule, preoperative<br />
diagnostic tests performed by, or at the request <strong>of</strong>, the physician performing preoperative<br />
examinations, do not fall within the statutory exclusion articulated in §1862)(a)(7) <strong>of</strong> the Act.<br />
These diagnostic tests are payable if they are medically necessary (i.e., they may be denied under<br />
§1862(a)(1)(A)).<br />
G. ICD-9 Coding Requirements for Preoperative Service - All claims for preoperative medical<br />
examination <strong>and</strong> preoperative diagnostic tests (i.e., preoperative medical evaluations) must be<br />
accompanied by the appropriate ICD-9 code for preoperative examination (e.g., V72.81 through<br />
V72.84). Additional appropriate ICD-9 codes for the condition(s) that prompted surgery <strong>and</strong> for<br />
conditions that prompted the preoperative medical evaluation (if any), should also be documented on<br />
the claim. Other diagnoses <strong>and</strong> conditions affecting the patient may also be documented on the claim,<br />
if appropriate. The ICD-9 code appearing in the line item <strong>of</strong> a preoperative examination or diagnostic<br />
test must be the code for the appropriate preoperative examination (e.g., V72.81 through V72.84)<br />
H. Reasonable <strong>and</strong> Necessary Services -For the purposes <strong>of</strong> establishing preoperative services as<br />
reasonable <strong>and</strong> necessary, all claims are subject to applicable national coverage decisions. In the<br />
absence <strong>of</strong> a national coverage decision, reasonable <strong>and</strong> necessary services are determined by Carrier<br />
discretion. Establishing reasonable <strong>and</strong> necessary preoperative medical evaluations is facilitated when<br />
the ICD-9 code(s) for the condition(s) that prompted surgery, <strong>and</strong> for the conditions that prompted the<br />
5-16<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
preoperative medical evaluation (if any), are documented as additional diagnoses on the claim.<br />
[Medicare Carriers Manual, Part 3, Claims Process §15046 – CMS Paper Manual<br />
Physician Regulatory Issues Team (PRIT) Issue – History <strong>and</strong> Physicals by Podiatrists<br />
Issue<br />
Status<br />
Podiatrists have asked that Medicare allow them to perform H&Ps on hospital<br />
inpatients.<br />
CMS is considering a change to the Hospital Condition <strong>of</strong> Participation that<br />
would permit Podiatrists to perform this service.<br />
August 13, 2004 The Hospital Condition <strong>of</strong> Participation are now in the final approval process.<br />
One <strong>of</strong> 4 PRIT issues which will be resolved in the soon to be released Hospitals<br />
October 6, 2004 Conditions <strong>of</strong> Participation.<br />
The PRIT will announce on this website when the Hospital CoP is released.<br />
Dec 20, 2004 CMS published a proposed rule - Hospital CoP 3122-P - that addresses this<br />
issue.<br />
March 25, 2005 The clearance process is very involved for changes to the Conditions <strong>of</strong><br />
Participation. However, we are confident that the new CoP will be released late<br />
May 9, 2006<br />
in 2006 or very early in 2007.<br />
Date Issue Created 12/01/2003<br />
Physician Regulatory Issues Team (PRIT) Issue – History <strong>and</strong> Physicals for Outpatient Surgical<br />
Procedures<br />
Issue<br />
Hospitals have asked if it would be permissible to allow non-credentialed<br />
physicians to do the History <strong>and</strong> Physicals.<br />
Status<br />
Current interpretive guidelines require that a physician must be credentialed by a<br />
hospital in order to be able to do the history <strong>and</strong> physical which is required<br />
before a patient can have ambulatory surgery at that hospital. We will discuss<br />
this policy with CMS policy experts <strong>and</strong> appropriate specialty societies.<br />
We have discussed this issue with the American College <strong>of</strong> Surgeons <strong>and</strong> we<br />
July 15<br />
have a meeting about this issue with the American College <strong>of</strong> Physicians next<br />
week.<br />
Surgeons routinely provide focused H&Ps to their surgical patients as part <strong>of</strong> the<br />
September 29 preoperative services which are bundled into the payment for the surgery.<br />
Patients who have significant comorbid conditions may require a preoperative<br />
visit with an internist or subspecialist in which case that visit would be covered.<br />
It would be appropriate for the internist to perform a focused H&P <strong>and</strong> make<br />
recommendations concerning the management <strong>of</strong> the patient’s comorbid<br />
conditions during the preoperative period.<br />
Date Issue Created 12/01/2005<br />
LESION DESTRUCTION/EXCISION<br />
Coding the destruction or removal <strong>of</strong> skin lesions can be one <strong>of</strong> the most challenging <strong>coding</strong> processes<br />
faced by a biller. The anatomical site, number (<strong>and</strong> size, if necessary) <strong>of</strong> lesions involved, the type <strong>of</strong><br />
lesion (e.g., skin tag, benign or malignant), <strong>and</strong> method <strong>of</strong> removal must be identified to select the proper<br />
code(s).<br />
Paring or Cutting<br />
To report paring or cutting <strong>of</strong> benign hyperkeratotic lesions (e.g., corn or callus) see codes 11055-11057<br />
5-17<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
Note codes 11055-11057 are reported based on the number <strong>of</strong> lesions involved. Only one code would be<br />
used to describe the procedure based on the number <strong>of</strong> lesions pared or cut. For example, if the physician<br />
pared three (3) corns. The physician would report 11056. This code is to be used to report two to four<br />
lesions.<br />
Removal <strong>of</strong> Skin Tags<br />
Regardless <strong>of</strong> the method <strong>of</strong> removal (e.g., scissoring, sharp method, ligature strangulation,<br />
electrosurgical destruction, or combination <strong>of</strong> treatment modalities including chemical or<br />
electrocauterization <strong>of</strong> wound, with or without local anesthesia), codes 11200-11201 are used to report the<br />
service.<br />
Note these codes are based on the number <strong>of</strong> skin tags involved. Code 11201 is an add-on procedure that<br />
cannot be reported without 11200. Multiple surgical procedures rules do not apply to add-on codes. For<br />
example, 20 skin tags are removed.<br />
The service should be reported as:<br />
11200 1 unit<br />
11201 1 unit<br />
Shaving <strong>of</strong> Epidermal or Dermal Lesions<br />
According to CPT, Shaving is the sharp removal by transverse incision or horizontal slicing to remove<br />
epidermal <strong>and</strong> dermal lesions without a full-thickness dermal excision. This includes local anesthesia,<br />
chemical, or electrocauterization <strong>of</strong> the wound. The wound does not require suture closure.<br />
Physicians sometimes refer to this procedure as a shave biopsy. If the term shave biopsy is used, the coder<br />
needs to verify if the entire lesion was shaved (11300-11313) or if a piece <strong>of</strong> tissue was removed to be<br />
sent for pathology (11100 <strong>and</strong> 11101).<br />
The shaving codes (11300-11313) are defined by size <strong>and</strong> anatomical site. Each lesion removed by shave<br />
technique is coded separately. Multiple surgical procedure rules apply to these codes.<br />
Excision Benign Lesions<br />
Benign excision is defined as full-thickness (through the dermis) removal <strong>of</strong> lesions <strong>of</strong> the skin or<br />
subcutaneous tissue (e.g., cicatricial, fibrous, inflammatory, congenital, cystic lesions, etc.). Simple<br />
closure is included in the excision code; however, intermediate or complex closure may be reported<br />
separately for excised diameter greater than 0.5 cm. When both the excision <strong>and</strong> repair codes are reported,<br />
multiple surgical procedure rules apply.<br />
The excision <strong>of</strong> benign lesion codes (11400-11446) are defined by size (including margins) <strong>and</strong><br />
anatomical site. Each lesion excised is coded separately. Multiple surgical procedure rules apply to these<br />
codes.<br />
Excision <strong>of</strong> Malignant Lesions<br />
Malignant lesion excision is defined as full-thickness (through the dermis) removal <strong>of</strong> malignant lesions<br />
(pathology report available) <strong>of</strong> the skin or subcutaneous tissue. Closure by suture is required when using<br />
codes 11600-11646. Simple closure is included in the excision code; however, intermediate or complex<br />
closure may be reported separately. When both the excision <strong>and</strong> repair codes are reported, multiple<br />
surgical procedure rules apply.<br />
5-18<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
The excision <strong>of</strong> malignant lesion codes (11600-11646) are defined by size (including margins) <strong>and</strong><br />
anatomical site. Each lesion excised is coded separately. Multiple surgical procedure rules apply to these<br />
codes.<br />
Destruction<br />
According to CPT, Destruction means the ablation <strong>of</strong> benign, premalignant, or malignant tissues by any<br />
method, with or without curettement, including local anesthesia, <strong>and</strong> not usually requiring closure.<br />
Any method includes electrosurgery, cryosurgery, laser, <strong>and</strong> chemical treatment. Lesions include<br />
condylomata, papillomata, molluscum contagiosum, herpetic lesions, warts (i.e., common, plantar, flat),<br />
milia, or other benign, premalignant (e.g., actinic keratoses), or malignant lesions.<br />
Destruction Premalignant Lesions - Coding Change – Reporting Destruction <strong>of</strong> Benign or Premalignant<br />
Lesions<br />
Newby Note: Significant revisions in the descriptions for the following codes require<br />
adjustments <strong>of</strong> billing practices for the destruction <strong>of</strong> lesions. Be sure to update your<br />
superbill/charge ticket to reflect these changes.<br />
17000 Destruction (e.g., laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement),<br />
premalignant lesions [Emphasis Added] (e.g., actinic keratosis); first lesion<br />
17003 Destruction (e.g., laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement),<br />
premalignant lesions [Emphasis Added] (e.g., actinic keratosis); second through 14 lesions each<br />
(List separately in addition to code for first lesion)<br />
17004 Destruction (e.g., laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement),<br />
premalignant lesions [Emphasis Added] (e.g., actinic keratosis); 15 or more lesions<br />
Please note code 17004 is not an add-on code. If 15 or more lesions are destroyed on the same patient on<br />
the same day, only code 17004 is reported (codes 17000 <strong>and</strong> 17003 are bundled).<br />
Destruction Benign Lesions including Flat Wart, Molluscum Contagiosum, or Milia<br />
Codes 17110-17111 should be used to report the destruction <strong>of</strong> benign lesions, flat warts, molluscum<br />
contagiosum, or milia.<br />
17110 Destruction (e.g., laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement),<br />
benign lesions [Emphasis Added] other than skin tags or cutaneous vascular lesions; up to 14<br />
lesions<br />
17111 Destruction (e.g., laser surgery, electrosurgery, cryosurgery, chemosurgery, surgical curettement),<br />
benign lesions [Emphasis Added] other than skin tags or cutaneous vascular lesions; 15 or more<br />
lesions<br />
Destructions Malignant Lesions<br />
Codes 17260-17286 are used to report the destruction <strong>of</strong> malignant lesions (pathology report available).<br />
Note codes 17260-17286 are defined by size <strong>and</strong> anatomical site. Each lesion is coded separately.<br />
Multiple surgical procedure rules apply to these codes.<br />
ACTINIC KERATOSIS<br />
Medicare National Coverage Determinations Manual – Chapter 1, Part 4 - §250.4 - (Rev. 1, 10-01-03)<br />
CIM 35-101<br />
Actinic keratoses (AKs), also known as solar keratoses, are common, sun-induced skin lesions that are<br />
confined to the epidermis <strong>and</strong> have the potential to become a skin cancer.<br />
5-19<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
Various options exist for treating AKs. Clinicians should select an appropriate treatment based on the<br />
patient’s medical history, the lesion’s characteristics, <strong>and</strong> on the patient’s preference for a specific<br />
treatment. Commonly performed treatments for AKs include cryosurgery with liquid nitrogen, topical<br />
drug therapy, <strong>and</strong> curettage. Less commonly performed treatments for AK include dermabrasion,<br />
excision, chemical peels, laser therapy, <strong>and</strong> photodynamic therapy (PDT). An alternative approach to<br />
treating AKs is to observe the lesions over time <strong>and</strong> remove them only if they exhibit specific clinical<br />
features suggesting possible transformation to invasive squamous cell carcinoma (SCC).<br />
Medicare covers the destruction <strong>of</strong> actinic keratoses without restrictions based on lesion or patient<br />
characteristics.<br />
WOUND REPAIR (CLOSURE) - CPT/HCPCS Codes 12001-13300 <strong>and</strong> G0168<br />
These series <strong>of</strong> codes are used to describe laceration repair <strong>and</strong>, in limited situations, closure from a<br />
procedure. Wound closure includes repair by sutures, staples, or tissue adhesives (e.g., 2-cyanoacrylate),<br />
either singly or in combination with each other, or in combination with adhesive strips. Wound closure<br />
utilizing adhesive strips as the sole repair material should be coded using the appropriate E/M code. For<br />
Medicare claims when a wound is closed solely with tissue adhesive, physicians are instructed to use code<br />
G0168, wound closure utilizing tissue adhesive only. Repair (closure) <strong>of</strong> most surgical wounds is<br />
included in the allowance for the primary surgical procedure. However, for certain procedures, wound<br />
closure may be separately billed.<br />
Undermining the wound margins to permit closure is usually not separately billable using the<br />
intermediate or complex wound repair codes.<br />
When the wound repair codes 12001-13300 are used for closure <strong>of</strong> traumatic wounds, the CPT <strong>coding</strong><br />
guidelines should be followed.<br />
Codes 20100-20103 are used to report exploration <strong>and</strong> repair <strong>of</strong> trauma wounds requiring Enlargement,<br />
extension <strong>of</strong> dissection (to determine penetration), debridement, removal <strong>of</strong> foreign body(s), ligation or<br />
coagulation <strong>of</strong> minor subcutaneous <strong>and</strong>/or muscular blood vessel(s) <strong>of</strong> the subcutaneous tissue, muscle<br />
fascia, <strong>and</strong>/or muscle, not requiring thoracotomy or laparoscopy.<br />
Bundling Of Repair Codes Into Excision Of Benign Lesion Codes<br />
Payment for the excision <strong>of</strong> benign or malignant lesions <strong>of</strong> skin includes payment for simple repairs.<br />
Separate payment for simple repairs (CPT codes 12001-12018) will not be made when reported with the<br />
CPT codes for the excision <strong>of</strong> benign lesions (11400-11446) or the excision <strong>of</strong> malignant lesions<br />
(11600-11646).<br />
Medicare Bundling<br />
For Medicare claims, payment for the excision <strong>of</strong> benign lesions with an excised diameter <strong>of</strong> 0.5 cm or<br />
less (CPT 11400, 11420, <strong>and</strong> 11440) includes payment for simple, intermediate, or complex repairs. In<br />
other words, separate payment for simple, intermediate, or complex repairs (CPT 12001-12018) will not<br />
be made when reported with CPT codes 11400, 11420, <strong>and</strong> 11440.<br />
Carriers use existing definitions for simple, intermediate, <strong>and</strong> complex repairs listed in the American<br />
Medical Association's Physicians’ Current Procedural Terminology (CPT). For Medicare claims, payment<br />
for the excision <strong>of</strong> a benign lesion with an excised diameter greater than 0.5 cm or the excision <strong>of</strong> a<br />
malignant lesion <strong>of</strong> any size does not include payment for intermediate or complex repairs. Separate<br />
payment for medically necessary intermediate repairs (CPT codes 12031-12057) or medically necessary<br />
5-20<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
complex repairs (CPT codes 13100-13152) may be made when reported with CPT codes 11401-11406,<br />
11421-11426, 11441-11446, <strong>and</strong> 11600-11646.<br />
REMOVAL OF CERUMEN<br />
In collaboration with the American <strong>Academy</strong> <strong>of</strong> Otolaryngology-Head <strong>and</strong> Neck Surgery (AAO-HNS),<br />
the American Medical Association (AMA) included the following information in the July 2005 issue <strong>of</strong><br />
CPT Assistant. The intent <strong>of</strong> presenting the material is to provide some typical <strong>coding</strong> scenarios with<br />
regard to the appropriate use <strong>and</strong> application <strong>of</strong> CPT codes related to earwax removal e.g., 69210.<br />
These three scenarios represent frequent patient encounters related to the need for earwax removal:<br />
1. The patient presents to the <strong>of</strong>fice for the removal <strong>of</strong> “earwax” by the nurse via<br />
irrigation.<br />
2. The patient presents to the <strong>of</strong>fice for the removal <strong>of</strong> “earwax” by the primary care<br />
physician via irrigation or lavage.<br />
3. The patient presents to the <strong>of</strong>fice for “earwax” removal as the presenting complaint.<br />
This is described as impacted cerumen because it completely covers the eardrum <strong>and</strong><br />
the patient has hearing loss. The impacted cerumen is removed by the primary care<br />
physician or otolaryngologist with magnification provided by an otoscope or<br />
operating microscope <strong>and</strong> instruments such as wax curettes, forceps, <strong>and</strong> suction.<br />
The AMA states, “A major element in determining whether code 69210 should be<br />
reported is underst<strong>and</strong>ing the definition <strong>of</strong> impacted cerumen.” According to the AAO-<br />
HNS,<br />
If any one or more <strong>of</strong> the following are present, cerumen should be considered<br />
“impacted” clinically:<br />
• Visual considerations: Cerumen impairs exam <strong>of</strong> clinically significant portions <strong>of</strong><br />
the external auditory canal, tympanic membrane, or middle ear conditions.<br />
• Qualitative considerations: Extremely hard, dry, irritative cerumen causing<br />
symptoms such as pain, itching, hearing loss, etc<br />
• Inflammatory considerations: associated with foul odor, infection, or dermatitis<br />
• Quantitative considerations: Obstructive, copious cerumen that cannot be<br />
removed without magnification <strong>and</strong> multiple instruments requiring physician<br />
skills.”<br />
The article also includes:<br />
Removing wax that is not impacted does not warrant the <strong>reporting</strong> <strong>of</strong> CPT code<br />
69210. Rather, that work would appropriately be captured by an evaluation <strong>and</strong><br />
management (E/M) code regardless <strong>of</strong> how it is removed.<br />
If, however, the wax is truly impacted, then its removal should be reported with<br />
69210 if performed by a physician using at a minimum an otoscope <strong>and</strong><br />
instruments such as wax curettes, or in the case <strong>of</strong> many otolaryngologists, with<br />
an operating microscope <strong>and</strong> suction plus specific ear instruments (e.g., cup<br />
forceps, right angles).<br />
Accompanying documentation should indicate the time, effort, <strong>and</strong> equipment<br />
required to provide the service.<br />
5-21<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
Add-on code 69990, microsurgical techniques, requiring use <strong>of</strong> operating<br />
microscope (List separately in addition to code for primary procedure), should<br />
not be reported if the operating microscope is used for cerumen removal. In this<br />
latter instance, however, code 92504 binocular microscopy (separate diagnostic<br />
procedure), may be reported.<br />
Therefore, based on this information, Scenarios 1 <strong>and</strong> 2 above would not be<br />
reported with code 69210. These scenarios would be captured by the appropriate<br />
E/M code.<br />
Scenario 3, however, should be reported with code 69210 because both criteria<br />
were met; the patient had cerumen impaction <strong>and</strong> the removal required physician<br />
work using at least an otoscope <strong>and</strong> instrumentation rather than simple lavage.<br />
BURNS, LOCAL TREATMENT<br />
The following codes are used to report local treatment <strong>of</strong> burned surface only.<br />
CPT<br />
CODE<br />
STATUS OF<br />
PROBLEMS<br />
16000 Initial treatment, first degree burn, when not more than local treatment is required<br />
16020 Dressings <strong>and</strong>/or debridement <strong>of</strong> partial-thickness burns, initial or subsequent; small (less<br />
than 5% total body surface area)<br />
16025<br />
16030<br />
Dressings <strong>and</strong>/or debridement <strong>of</strong> partial-thickness burns, initial or subsequent; medium<br />
(e.g., whole face or whole extremity, or 5% to 10% total body surface area)<br />
Dressings <strong>and</strong>/or debridement <strong>of</strong> partial-thickness burns, initial or subsequent; large (e.g.,<br />
more than one extremity, or greater than 10% total body surface area<br />
SPRAINED FINGER(S)<br />
The following information was presented during the 2003 CPT Coding Symposium, November 14, 2002.<br />
Question: What is the correct code for buddy taping fingers, taping one finger to another for<br />
immobilizing a sprained finger<br />
Answer: Taping one finger to another for immobilizing a sprained finger is not reported<br />
separately, as it is considered a part <strong>of</strong> an Evaluation <strong>and</strong> Management (E/M) code.<br />
FRACTURE CARE<br />
If a physician treats a fracture <strong>and</strong> is responsible for the total fracture care, the appropriate fracture code<br />
would be reported based on the treatment provided.<br />
The fracture/dislocation treatment codes are generally reported by the physician responsible for the initial<br />
casting/strapping/splinting <strong>and</strong> follow-up care until the fracture/dislocation is healed. This is considered<br />
surgical treatment.<br />
When the physician provides a non-surgical treatment <strong>of</strong> the fracture/dislocation without the application<br />
<strong>of</strong> a brace, splint, or cast or without any follow-up care, the physician should only report the appropriate<br />
E/M codes based on the type <strong>of</strong> history, exam, <strong>and</strong> medical decision making required by the patient.<br />
5-22<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
HEMORRHOIDECTOMY BY SIMPLE LIGATURE<br />
Billing Excessive Units <strong>of</strong> Service for CPT 46221<br />
Recent data analysis <strong>and</strong> Medical Review findings for CPT 46221 (Hemorrhoidectomy, by simple<br />
ligature (e.g., rubber b<strong>and</strong>)) indicated a high error rate in the utilization <strong>of</strong> this code. Reviews revealed<br />
providers were billing CPT 46221 more than once per session for the same beneficiary.<br />
When billing CPT 46221, only one unit <strong>of</strong> service is reported regardless <strong>of</strong> the number <strong>of</strong> hemorrhoids<br />
ligated during the session. The October 1997 CPT Assistant article states "Each session <strong>of</strong> rubber b<strong>and</strong><br />
ligation, regardless <strong>of</strong> the number <strong>of</strong> hemorrhoids, is coded once."<br />
Please review your billing <strong>of</strong> CPT 46221 to determine any potential overpayments made to your practice.<br />
If you identify any overpayments, it is your responsibility to perform a voluntary refund to the Medicare<br />
Program.<br />
URETHRAL CATHETERIZATION<br />
Code 5170 describes catheterization <strong>of</strong> a patient for residual urine.<br />
Code 51702 describes insertion <strong>of</strong> Foley catheter for patients with chronic problems, such as<br />
neurogenic bladder <strong>and</strong> insertion <strong>of</strong> catheters in patients in acute retention in the hospital setting.<br />
Code 51703 describes a complicated insertion (e.g., altered anatomy, fractured catheter/balloon).<br />
Newby Note: Physicians should continue to use HCPCS code P9612, catheterization for<br />
collection <strong>of</strong> specimen, single patient, all places <strong>of</strong> service, when the patient is catheterized<br />
for a sterile urine specimen.<br />
GROUP PRACTICE DEFINED<br />
Medicare General Information, Eligibility, <strong>and</strong> Entitlement Chapter 5 §90.4 (Rev. 1, 09-11-02)<br />
A group practice is a group <strong>of</strong> two or more physicians <strong>and</strong> non-physician practitioners legally organized<br />
in a partnership, pr<strong>of</strong>essional corporation, foundation, not-for-pr<strong>of</strong>it corporation, faculty practice plan, or<br />
similar association:<br />
• In which each physician who is a member <strong>of</strong> the group provides substantially the full range <strong>of</strong><br />
services which the physician routinely provides (including medical care, consultation, diagnosis,<br />
or treatment) through the joint use <strong>of</strong> shared <strong>of</strong>fice space, facilities, equipment, <strong>and</strong> personnel<br />
• For which substantially all <strong>of</strong> the services <strong>of</strong> the physicians who are members <strong>of</strong> the group are<br />
provided through the group <strong>and</strong> are billed in the name <strong>of</strong> the group <strong>and</strong> amounts so received are<br />
treated as receipts <strong>of</strong> the group<br />
• In which the overhead expenses <strong>of</strong> <strong>and</strong> the income from the practice are distributed in accordance<br />
with methods previously determined by members <strong>of</strong> the group<br />
• Which meets such other st<strong>and</strong>ards as the Secretary may impose by regulation to implement<br />
§1877(h)(4) <strong>of</strong> the Social Security Act. The group practice definition also applies to health care<br />
practitioners.<br />
Physicians in Group Practice<br />
Medicare Claims Processing Manual Chapter 12 §30.6.5 (Rev. 1, 10-01-03)<br />
Physicians in the same group practice who are in the same specialty must bill <strong>and</strong> be paid as though they<br />
were a single physician. If more than one evaluation <strong>and</strong> management (face-to-face) service is provided<br />
on the same day to the same patient by the same physician or more than one physician in the same<br />
specialty in the same group, only one evaluation <strong>and</strong> management service may be reported unless the<br />
evaluation <strong>and</strong> management services are for unrelated problems. Instead <strong>of</strong> billing separately, the<br />
5-23<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
physicians should select a level <strong>of</strong> service representative <strong>of</strong> the combined visits <strong>and</strong> submit the<br />
appropriate code for that level.<br />
Physicians in the same group practice but who are in different specialties may bill <strong>and</strong> be paid without<br />
regard to their membership in the same group.<br />
EVALUATION AND MANAGEMENT (E/M) SERVICES FURNISHED INCIDENT TO<br />
PHYSICIAN’S SERVICE BY NONPHYSICIAN PRACTITIONERS<br />
Medicare Claims Processing Manual Chapter 12 §30.6.4 (Rev. 1, 10-01-03)<br />
When evaluation <strong>and</strong> management services are furnished incident to a physician’s service by a<br />
nonphysician practitioner, the physician may bill the CPT code that describes the evaluation <strong>and</strong><br />
management service furnished.<br />
When evaluation <strong>and</strong> management services are furnished incident to a physician’s service by a<br />
nonphysician employee <strong>of</strong> the physician, not as part <strong>of</strong> a physician service, the physician bills code 99211<br />
for the service.<br />
A physician is not precluded from billing under the “incident to” provision for services provided by<br />
employees whose services cannot be paid for directly under the Medicare Program. Employees <strong>of</strong> the<br />
physician may provide services incident to the physician’s service, but the physician alone is permitted to<br />
bill Medicare.<br />
Services provided by employees as “incident to” are covered when they meet all the requirements for<br />
incident to <strong>and</strong> are medically necessary for the individual needs <strong>of</strong> the patient.<br />
Split/Shared E/M Service<br />
Office/Clinic Setting<br />
In the <strong>of</strong>fice/clinic setting when the physician performs the E/M service the service must be reported<br />
using the physician’s UPIN/PIN. When an E/M service is a shared/split encounter between a physician<br />
<strong>and</strong> a non-physician practitioner (NP, PA, CNS, or CNM), the service is considered to have been<br />
performed “incident to” if the requirements for “incident to” are met <strong>and</strong> the patient is an established<br />
patient. If “incident to” requirements are not met for the shared/split E/M service, the service must be<br />
billed under the NPP’s UPIN/PIN, <strong>and</strong> payment will be made at the appropriate physician fee schedule<br />
payment.<br />
Hospital Inpatient/Outpatient/Emergency Department Setting<br />
When a hospital inpatient/hospital outpatient or emergency department E/M is shared between a<br />
physician <strong>and</strong> an NPP from the same group practice <strong>and</strong> the physician provides any face-to-face portion<br />
<strong>of</strong> the E/M encounter with the patient, the service may be billed under either the physician's or the NPP's<br />
UPIN/PIN number. However, if there was no face-to-face encounter between the patient <strong>and</strong> the<br />
physician (e.g., even if the physician participated in the service by reviewing the patient’s medical<br />
record), then the service may only be billed under the NPP's UPIN/PIN. Payment will be made at the<br />
appropriate physician fee schedule rate based on the UPIN/PIN entered on the claim.<br />
Examples <strong>of</strong> Shared Visits<br />
• If the NPP sees a hospital inpatient in the morning <strong>and</strong> the physician follows with a later face-t<strong>of</strong>ace<br />
visit with the patient on the same day, the physician or the NPP may report the service.<br />
• In an <strong>of</strong>fice setting the NPP performs a portion <strong>of</strong> an E/M encounter <strong>and</strong> the physician completes<br />
the E/M service. If the "incident to" requirements are met, the physician reports the service. If the<br />
“incident to” requirements are not met, the service must be reported using the NPP’s UPIN/PIN.<br />
5-24<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
Medicare “Incident to Clarification”<br />
Medicare Benefit Policy Manual - Chapter 15 – §60.1 - (Rev. 1, 10-01-03) - B3-2050.1<br />
Incident to a physician’s pr<strong>of</strong>essional services means that the services or supplies are furnished as an<br />
integral, although incidental, part <strong>of</strong> the physician’s personal pr<strong>of</strong>essional services in the course <strong>of</strong><br />
diagnosis or treatment <strong>of</strong> an injury or illness.<br />
Where a physician supervises auxiliary personnel to assist him/her in rendering services to patients <strong>and</strong><br />
includes the charges for their services in his/her own bills, the services <strong>of</strong> such personnel are considered<br />
incident to the physician’s service if there is a physician’s service rendered to which the services <strong>of</strong> such<br />
personnel are an incidental part <strong>and</strong> there is direct supervision by the physician.<br />
This does not mean, however, that to be considered incident to, each occasion <strong>of</strong> service by auxiliary<br />
personnel (or the furnishing <strong>of</strong> a supply) need also always be the occasion <strong>of</strong> the actual rendition <strong>of</strong> a<br />
personal pr<strong>of</strong>essional service by the physician. Such a service or supply could be considered to be<br />
incident to when furnished during a course <strong>of</strong> treatment where the physician performs an initial service<br />
[Emphasis added] <strong>and</strong> subsequent services <strong>of</strong> a frequency which reflect his/her active participation in <strong>and</strong><br />
management <strong>of</strong> the course <strong>of</strong> treatment. (However, the direct supervision requirement must still be met<br />
with respect to every nonphysician service.)<br />
Direct supervision in the <strong>of</strong>fice setting does not mean that the physician must be present in the same room<br />
with his or her aide. However, the physician must be present in the <strong>of</strong>fice suite <strong>and</strong> immediately available<br />
to provide assistance <strong>and</strong> direction throughout the time the aide is performing services.<br />
If auxiliary personnel perform services outside the <strong>of</strong>fice setting, e.g., in a patient’s home or in an<br />
institution (other than hospital or SNF), their services are covered incident to a physician’s service only if<br />
there is direct supervision by the physician. For example, if a nurse accompanied the physician on house<br />
calls <strong>and</strong> administered an injection, the nurse’s services are covered. If the same nurse made the calls<br />
alone <strong>and</strong> administered the injection, the services are not covered (even when billed by the physician)<br />
since the physician is not providing direct supervision. Services provided by auxiliary personnel in an<br />
institution (e.g., nursing, or convalescent home) present a special problem in determining whether direct<br />
physician supervision exists. The availability <strong>of</strong> the physician by telephone <strong>and</strong> the presence <strong>of</strong> the<br />
physician somewhere in the institution does not constitute direct supervision. For hospital patients <strong>and</strong> for<br />
SNF patients who are in a Medicare covered stay, there is no Medicare Part B coverage <strong>of</strong> the services <strong>of</strong><br />
physician-employed auxiliary personnel as services incident to physicians’ services under §1861(s)(2)(A)<br />
<strong>of</strong> the Act. Such services can be covered only under the hospital or SNF benefit <strong>and</strong> payment for such<br />
services can be made to only the hospital or SNF by a Medicare Intermediary.<br />
Services Of Nonphysician Personnel Furnished Incident To Physician’s Services<br />
Medicare Benefit Policy Manual - Chapter 15 – §60.2 - (Rev. 1, 10-01-03) - B3-2050.2<br />
In addition to coverage being available for the services <strong>of</strong> such auxiliary personnel as nurses, technicians,<br />
<strong>and</strong> therapists when furnished incident to the pr<strong>of</strong>essional services <strong>of</strong> a physician (as discussed in §60.1),<br />
a physician may also have the services <strong>of</strong> certain nonphysician practitioners covered as services incident<br />
to a physician’s pr<strong>of</strong>essional services. These nonphysician practitioners, who are being licensed by the<br />
States under various programs to assist or act in the place <strong>of</strong> the physician, include, for example, certified<br />
nurse midwives, clinical psychologists, clinical social workers, physician assistants, nurse practitioners,<br />
<strong>and</strong> clinical nurse specialists.<br />
Services performed by these nonphysician practitioners incident to a physician’s pr<strong>of</strong>essional services<br />
include not only services ordinarily rendered by a physician’s <strong>of</strong>fice staff person (e.g., medical services<br />
such as taking blood pressures <strong>and</strong> temperatures, giving injections, <strong>and</strong> changing dressings) but also<br />
5-25<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
services ordinarily performed by the physician such as minor surgery, setting casts or simple fractures,<br />
reading x-rays, <strong>and</strong> other activities that involve evaluation or treatment <strong>of</strong> a patient’s condition.<br />
Nonetheless, in order for services <strong>of</strong> a nonphysician practitioner to be covered as incident to the services<br />
<strong>of</strong> a physician, the services must meet all <strong>of</strong> the requirements for coverage specified in §§60 through 60.1.<br />
For example, the services must be an integral, although incidental, part <strong>of</strong> the physician’s personal<br />
pr<strong>of</strong>essional services, <strong>and</strong> they must be performed under the physician’s direct supervision.<br />
A nonphysician practitioner such as a physician assistant or a nurse practitioner may be licensed under<br />
State law to perform a specific medical procedure <strong>and</strong> may be able to perform the procedure without<br />
physician supervision <strong>and</strong> have the service separately covered <strong>and</strong> paid for by Medicare as a physician<br />
assistant’s or nurse practitioner’s service. However, in order to have that same service covered as incident<br />
to the services <strong>of</strong> a physician, it must be performed under the direct supervision <strong>of</strong> the physician as an<br />
integral part <strong>of</strong> the physician’s personal in-<strong>of</strong>fice service.<br />
As explained in §60.1, this does not mean that each occasion <strong>of</strong> an incidental service performed by a<br />
nonphysician practitioner must always be the occasion <strong>of</strong> a service actually rendered by the physician. It<br />
does mean that there must have been a direct, personal, pr<strong>of</strong>essional service furnished by the physician to<br />
initiate the course <strong>of</strong> treatment <strong>of</strong> which the service being performed by the nonphysician practitioner is<br />
an incidental part, <strong>and</strong> there must be subsequent services by the physician <strong>of</strong> a frequency that reflects the<br />
physician’s continuing active participation in <strong>and</strong> management <strong>of</strong> the course <strong>of</strong> treatment. In addition, the<br />
physician must be physically present in the same <strong>of</strong>fice suite <strong>and</strong> be immediately available to render<br />
assistance if that becomes necessary.<br />
Incident-To Services on Form CMS-1500<br />
Medicare Claims Processing Manual – Chapter 26 - §10.4 - Items 14-33 - Provider <strong>of</strong> Service or<br />
Supplier Information = (Rev. 1215, Issued: 03-30-07, Effective: 04-01-07, Implementation: 04-30-07)<br />
Item 17 When a service is incident to the service <strong>of</strong> a physician or non-physician practitioner, the<br />
name <strong>of</strong> the physician or non-physician practitioner who performs the initial service <strong>and</strong><br />
orders the non-physician service must appear in item 17;<br />
Item 17a Enter the ID qualifier 1G, followed by the CMS assigned UPIN <strong>of</strong> the referring/ordering<br />
physician listed in item 17. Under Medicare’s NPI contingency plan, the UPIN may be<br />
reported on the Form CMS-1500 <strong>and</strong> MUST be reported if an NPI is not available.<br />
Item 17b<br />
Item 24J<br />
Enter the NPI <strong>of</strong> the referring/ordering physician listed in item 17 as soon as it is available.<br />
During Medicare’s NPI contingency plan, enter the rendering provider’s PIN in the shaded<br />
portion. In the case <strong>of</strong> a service provided incident to the service <strong>of</strong> a physician or nonphysician<br />
practitioner, when the person who ordered the service is not supervising, enter the<br />
PIN <strong>of</strong> the supervisor in the shaded portion.<br />
Enter the rendering provider’s NPI number in the lower portion. In the case <strong>of</strong> a service<br />
provided incident to the service <strong>of</strong> a physician or non-physician practitioner, when the person<br />
who ordered the service is not supervising, enter the NPI <strong>of</strong> the supervisor in the lower<br />
portion.<br />
OFFICE/OUTPATIENT VISITS – CPT CODES 99201-99215<br />
A. Definition <strong>of</strong> New Patient for Selection <strong>of</strong> E/M Visit Code<br />
Interpret the phrase “new patient” to mean a patient who has not received any pr<strong>of</strong>essional services, i.e.,<br />
E/M service or other face-to-face service (e.g., surgical procedure) from the physician or physician group<br />
practice (same physician specialty) within the previous 3 years. For example, if a pr<strong>of</strong>essional component<br />
<strong>of</strong> a previous procedure is billed in a 3 year time period, e.g., a lab interpretation is billed <strong>and</strong> no E/M<br />
5-26<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
service or other face-to-face service with the patient is performed, then this patient remains a new patient<br />
for the initial visit. An interpretation <strong>of</strong> a diagnostic test, reading an x-ray or EKG etc., in the absence <strong>of</strong><br />
an E/M service or other face-to-face service with the patient does not affect the designation <strong>of</strong> a new<br />
patient.<br />
Newby Note: If more than one evaluation <strong>and</strong> management (face-to-face) service is<br />
provided on the same day to the same patient by the same physician or more than one<br />
physician in the same specialty in the same group, only one evaluation <strong>and</strong> management<br />
service may be reported unless the evaluation <strong>and</strong> management services are for unrelated<br />
problems. Instead <strong>of</strong> billing separately, the physician should select a level <strong>of</strong> service<br />
representative <strong>of</strong> the combined visits <strong>and</strong> submit the appropriate code for that level.<br />
Physicians in the same group practice but who are in different specialties may bill <strong>and</strong> be<br />
paid without regard to their membership in the same group.<br />
There is no difference if the group physicians are located in the same or different<br />
buildings. Therefore, even though a physician may be located on another campus, if a<br />
patient previously cared for by the same specialty physician in the same group within the<br />
previous three years is seen by a group physician <strong>of</strong> the same specialty at a setting apart<br />
from where his/her care is generally rendered <strong>and</strong> where his/her medical records may be<br />
located, for billing purposes, that patient remains an established patient for that same<br />
group, same specialty physician. It is the group’s responsibility to coordinate record<br />
keeping when different locations are involved.<br />
Changing Group Practices<br />
Dr. Smith leaves his/her practice in <strong>Indiana</strong>polis to join a new practice in Carmel. If Dr.<br />
Smith, or another physician <strong>of</strong> the same specialty in the Carmel practice, has not provided<br />
any pr<strong>of</strong>essional services to that patient within the past three years, then Dr. Smith would<br />
consider the patient a new patient. If Dr. Smith has rendered pr<strong>of</strong>essional services to the<br />
patient in either the <strong>Indiana</strong>polis or Carmel practice within the past three years, the<br />
patient is considered established to Dr. Smith. If Dr. Smith saw the patient in <strong>Indiana</strong>polis,<br />
but one <strong>of</strong> the Carmel physicians sees the patient, the patient would be considered new.<br />
B. Office/Outpatient E/M Visits Provided on Same Day for Unrelated Problems<br />
As for all other E/M services except where specifically noted, Carriers may not pay two E/M <strong>of</strong>fice visits<br />
billed by a physician (or physician <strong>of</strong> the same specialty from the same group practice) for the same<br />
beneficiary on the same day unless the physician documents that the visits were for unrelated problems in<br />
the <strong>of</strong>fice or outpatient setting which could not be provided during the same encounter (e.g., <strong>of</strong>fice visit<br />
for blood pressure medication evaluation, followed five hours later by a visit for evaluation <strong>of</strong> leg pain<br />
following an accident).<br />
C. Office/Outpatient or Emergency Department E/M Visit on Day <strong>of</strong> Admission to Nursing Facility<br />
Carriers may not pay a physician for an emergency department visit or an <strong>of</strong>fice visit <strong>and</strong> a<br />
comprehensive nursing facility assessment on the same day. Bundle E/M visits on the same date provided<br />
in sites other than the nursing facility into the initial nursing facility care code when performed on the<br />
same date as the nursing facility admission by the same physician.<br />
D. Drug Administration Services <strong>and</strong> E/M Visits Billed on Same Day <strong>of</strong> Service<br />
Carriers must advise physicians that CPT code 99211 cannot be paid if it is billed with a drug<br />
administration service such as a chemotherapy or nonchemotherapy drug infusion code (effective January<br />
1, 2004). This drug administration policy was exp<strong>and</strong>ed in the Physician Fee Schedule Final Rule,<br />
November 15, 2004, to also include a therapeutic or diagnostic injection code (effective January 1, 2005).<br />
Therefore, when a medically necessary, significant <strong>and</strong> separately identifiable E/M service (which meets<br />
a higher complexity level than CPT code 99211) is performed, in addition to one <strong>of</strong> these drug<br />
5-27<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
administration services, the appropriate E/M CPT code should be reported with modifier -25.<br />
Documentation should support the level <strong>of</strong> E/M service billed. For an E/M service provided on the same<br />
day, a different diagnosis is not required.<br />
99211 Most Abused Code<br />
Nationwide, 99211 is one <strong>of</strong> the most abused codes for usage. Code 99211 describes a service provided<br />
for minimal problems that may not require the presence <strong>of</strong> a physician, but does require the presence <strong>of</strong> a<br />
patient. As stated previously, this code cannot be billed if only an injection is given, without documented<br />
pertinent questioning or instructions. It cannot be billed for:<br />
• telephone calls,<br />
• venipunctures,<br />
• prescription renewals to a pharmacy,<br />
• telephone calls for a patient to reschedule an appointment, <strong>and</strong><br />
• telephone calls with the results <strong>of</strong> laboratory testing.<br />
Billing 99211 is not allowed for every patient who enters the <strong>of</strong>fice for a minimal service <strong>and</strong> receives an<br />
unnecessary pulse, temperature, or blood pressure recording.<br />
Prothrombin Time <strong>and</strong> Evaluation <strong>of</strong> Patient Anti-Coagulation Status - CPT Code 99211<br />
The following was developed from consultation among Medicare Part B Contractor Medical Directors<br />
<strong>and</strong> review <strong>of</strong> the CMS Frequently Asked Questions Web site. The CPT code description for 99211<br />
follows:<br />
Office or other outpatient visit for the evaluation <strong>and</strong> management <strong>of</strong> an established patient that<br />
may not require the presence <strong>of</strong> a physician. Usually, the presenting problem(s) are minimal.<br />
Typically, five minutes are spent performing or supervising these services.<br />
When a face-to-face medication management is provided by qualified <strong>of</strong>fice staff on the same date <strong>of</strong> the<br />
laboratory test, the physician may bill CPT code 99211 if the services are medically necessary <strong>and</strong><br />
constitute a distinct, separately identifiable evaluation <strong>and</strong> management (E/M) service that is consistent<br />
with the criteria for a low-level <strong>of</strong>fice visit. The following describes adequate documentation for CPT<br />
code 99211 when billed for an evaluation <strong>of</strong> a chronically anti-coagulated patient for whom a<br />
prothrombin time has been drawn <strong>and</strong> determined.<br />
Reason for the visit - A physician visit is not routinely necessary in order to draw blood for prothrombin<br />
time or other laboratory tests. Therefore, the documentation for 99211 or any other E/M code in this<br />
circumstance must demonstrate a need for clinical evaluation <strong>and</strong> management. In this case, services that<br />
would serve to demonstrate that evaluation <strong>and</strong> management were performed include evaluation <strong>of</strong><br />
significant new symptoms (such as excessive bruising or hemorrhage). Alternatively, for patients who<br />
have no new clinical concerns, demonstrating how the relevant laboratory information obtained was used<br />
to modify therapy will document that a separately payable E/M service has been performed.<br />
• Current medications listed (with notation <strong>of</strong> level <strong>of</strong> compliance)<br />
• Indication <strong>of</strong> physician’s evaluation <strong>of</strong> the information about signs/symptoms <strong>and</strong> laboratory test<br />
result <strong>and</strong> his or her management recommendation<br />
• Identity <strong>and</strong> credentials <strong>of</strong> provider(s) as listed in text above<br />
If the patient does not have any new symptoms or requires a change in the dosage <strong>of</strong> his/her medication,<br />
the physician cannot report 99211.<br />
5-28<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
HOSPITAL OBSERVATION SERVICES – CPT CODES 99217-99220<br />
Medicare Claims Processing Manual Chapter 12 §30.6.8 (Codes 99217 99220) (Rev. 1, 10-01-03) B3-<br />
15504<br />
A. Who May Bill Initial Observation Care<br />
Carriers pay for initial observation care billed by only the physician who admitted the patient to hospital<br />
observation <strong>and</strong> was responsible for the patient during his/her stay in observation. A physician who does<br />
not have inpatient admitting privileges but who is authorized to admit a patient to observation status may<br />
bill these codes.<br />
For a physician to bill the initial observation care codes, there must be a medical observation record for<br />
the patient which contains dated <strong>and</strong> timed physician’s admitting orders regarding the care the patient is<br />
to receive while in observation, nursing notes, <strong>and</strong> progress notes prepared by the physician while the<br />
patient was in observation status. This record must be in addition to any record prepared as a result <strong>of</strong> an<br />
emergency department or outpatient clinic encounter.<br />
Payment for an initial observation care code is for all the care rendered by the admitting physician on the<br />
date the patient was admitted to observation. All other physicians who see the patient while he or she is in<br />
observation must bill the <strong>of</strong>fice <strong>and</strong> other outpatient service codes or outpatient consultation codes as<br />
appropriate when they provide services to the patient.<br />
For example, if an internist admits a patient to observation <strong>and</strong> asks an allergist for a consultation on the<br />
patient’s condition, only the internist may bill the initial observation care code. The allergist must bill<br />
using the outpatient consultation code that best represents the services he or she provided. The allergist<br />
cannot bill an inpatient consultation since the patient was not a hospital inpatient.<br />
B. Physician Billing for Observation Care Following Admission to Observation<br />
If the patient is discharged on the same date as admission to observation, Carriers pay only the initial<br />
observation care code because that code represents a full day <strong>of</strong> care.<br />
If the patient remains in observation after the first date following the admission to observation, it is<br />
expected that the patient would be discharged on that second calendar date. The physician bills CPT code<br />
99217 for observation care discharge services provided on the second date.<br />
In the rare circumstance when a patient is held in observation status for more than two calendar dates, the<br />
physician must bill subsequent services furnished before the date <strong>of</strong> discharge using the outpatient/<strong>of</strong>fice<br />
visit codes. The physician may not use the subsequent hospital care codes since the patient is not an<br />
inpatient <strong>of</strong> the hospital.<br />
C. Admission to Inpatient Status from Observation<br />
If the same physician who admitted a patient to observation status also admits the patient to inpatient<br />
status from observation before the end <strong>of</strong> the date on which the patient was admitted to observation, pay<br />
only an initial hospital visit for the evaluation <strong>and</strong> management services provided on that date. Medicare<br />
payment for the initial hospital visit includes all services provided to the patient on the date <strong>of</strong> admission<br />
by that physician, regardless <strong>of</strong> the site <strong>of</strong> service. The physician may not bill an initial observation care<br />
code for services on the date that he or she admits the patient to inpatient status. If the patient is admitted<br />
to inpatient status from observation subsequent to the date <strong>of</strong> admission to observation, the physician<br />
must bill an initial hospital visit for the services provided on that date. The physician may not bill the<br />
hospital observation discharge management code (code 99217) or an outpatient/<strong>of</strong>fice visit for the care<br />
provided in observation on the date <strong>of</strong> admission to inpatient status.<br />
5-29<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
OBSERVATION OR INPATIENT CARE SERVICES – INCLUDING ADMISSION AND<br />
DISCHARGE SERVICES - CPT CODES 99234-99236<br />
This series <strong>of</strong> codes is used to report observation or inpatient hospital care services provided to patients<br />
admitted <strong>and</strong> discharged on the same date <strong>of</strong> service. In order to use these codes for a Medicare patient,<br />
the patient must have been an inpatient or an observation care patient for a minimum <strong>of</strong> eight (8) hours on<br />
the same calendar date.<br />
When observation status or initial inpatient hospital care is initiated in the course <strong>of</strong> an encounter in<br />
another site <strong>of</strong> service (e.g., hospital emergency department, physician’s <strong>of</strong>fice, nursing facility) all<br />
evaluation <strong>and</strong> management services provided by the supervising physician in conjunction with initiating<br />
observation status are considered part <strong>of</strong> the initial observation care or initial inpatient hospital care when<br />
performed on the same date. The level <strong>of</strong> service should include the services related to the admission<br />
provided in the other sites-<strong>of</strong>-service as well as in the observation setting when provided by the same<br />
physician.<br />
Newby Note: To use codes 99234-99236, the physician must clearly indicate in the<br />
patient’s medical record the number <strong>of</strong> hours the patient was in observation or inpatient<br />
status.<br />
For patients admitted to observation or inpatient care for less than eight (8) hours or discharged on a<br />
different date, see codes 99218-99220 <strong>and</strong> 99217, or 99221-99223 <strong>and</strong> 99238-99239.<br />
INPATIENT HOSPITAL VISITS – CPT CODES 99221-99239<br />
Medicare Claims Processing Manual Chapter 12 §30.6.9 General (Codes 99221-99239) (Rev. 1, 10-01-<br />
03) B3-15505-15505.2<br />
A. Hospital Visit <strong>and</strong> Critical Care on Same Day<br />
If critical care is required upon the patient’s presentation to the emergency department, only critical care<br />
codes 99291-99292 may be reported. Emergency department codes will not be paid for the same day. If<br />
there is a hospital or <strong>of</strong>fice/outpatient evaluation <strong>and</strong> management service furnished early in the day <strong>and</strong><br />
at that time the patient does not require critical care, but the patient requires critical care later in the day,<br />
both critical care <strong>and</strong> the evaluation <strong>and</strong> management service may be paid.<br />
Physicians must submit supporting documentation when critical care is billed on the same day as other<br />
evaluation <strong>and</strong> management services.<br />
B. Two Hospital Visits Same Day<br />
Carriers pay a physician for only one hospital visit per day for the same patient, whether the problems<br />
seen during the encounters are related or not. The inpatient hospital visit descriptors contain the phrase<br />
per day which means that the code <strong>and</strong> the payment established for the code represent all services<br />
provided on that date. The physician should select a code that reflects all services provided during the<br />
date <strong>of</strong> the service.<br />
C. Hospital Visits Same Day But by Different Physicians<br />
In a hospital inpatient situation involving one physician covering for another, if physician A sees the<br />
patient in the morning <strong>and</strong> physician B, who is covering for A, sees the same patient in the evening,<br />
Carriers do not pay physician B for the second visit. The hospital visit descriptors include the phrase per<br />
day meaning care for the day.<br />
5-30<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
If the physicians are each responsible for a different aspect <strong>of</strong> the patient’s care, pay both visits if the<br />
physicians are in different specialties <strong>and</strong> the visits are billed with different diagnoses. There are<br />
circumstances where concurrent care may be billed by physicians <strong>of</strong> the same specialty.<br />
D. Visits to Patients in Swing Beds<br />
If the inpatient care is being billed by the hospital as inpatient hospital care, the hospital care codes apply.<br />
If the inpatient care is being billed by the hospital as nursing facility care, then the nursing facility codes<br />
apply.<br />
Payment for Initial Hospital Care Services<br />
Medicare Claims Processing Manual Chapter 12 §30.6.9.1 (Codes 99221-99223) (Rev. 1, 10-01-03)<br />
A. Initial Hospital Care from Emergency Room<br />
Carriers pay for an initial hospital care service or an initial inpatient consultation if a physician sees<br />
his/her patient in the emergency room <strong>and</strong> decides to admit the person to the hospital. They do not pay for<br />
both E/M services. Also, they do not pay for an emergency department visit by the same physician on the<br />
same date <strong>of</strong> service. When the patient is admitted to the hospital via another site <strong>of</strong> service (e.g., hospital<br />
emergency department, physician’s <strong>of</strong>fice, nursing facility), all services provided by the physician in<br />
conjunction with that admission are considered part <strong>of</strong> the initial hospital care when performed on the<br />
same date as the admission.<br />
B. Initial Hospital Care on Day Following Visit<br />
Carriers pay both visits if a patient is seen in the <strong>of</strong>fice on one date <strong>and</strong> admitted to the hospital on the<br />
next date, even if fewer than 24 hours has elapsed between the visit <strong>and</strong> the admission.<br />
C. Initial Hospital Care <strong>and</strong> Discharge on Same Day<br />
Carriers pay only the initial hospital care code when a patient is admitted as an inpatient <strong>and</strong> discharged<br />
on the same day. They do not pay the hospital discharge management code on the date <strong>of</strong> admission.<br />
Newby Note: If the patient is admitted <strong>and</strong> discharged on the same date <strong>of</strong> service <strong>and</strong> the<br />
patient has been an inpatient for eight (8) or more hours, the physician may use code<br />
99234-99236.<br />
D. Physician Services Involving Transfer From One Hospital to Another; Transfer Within Facility to<br />
Prospective Payment System (PPS) Exempt Unit <strong>of</strong> Hospital; Transfer From One Facility to Another<br />
Separate Entity Under Same Ownership <strong>and</strong>/or Part <strong>of</strong> Same Complex; or Transfer From One<br />
Department to Another Within Single Facility<br />
Physicians may bill both the hospital discharge management code <strong>and</strong> an initial hospital care code when<br />
the discharge <strong>and</strong> admission do not occur on the same day if the transfer is between:<br />
• Different hospitals;<br />
• Different facilities under common ownership which do not have merged records; or<br />
• Between the acute care hospital <strong>and</strong> a PPS exempt unit within the same hospital when there are<br />
no merged records.<br />
In all other transfer circumstances, the physician should bill only the appropriate level <strong>of</strong> subsequent<br />
hospital care for the date <strong>of</strong> transfer.<br />
E. Initial Hospital Care Service History <strong>and</strong> Physical That Is Less Than Comprehensive<br />
When a physician performs a visit or consultation that meets the definition <strong>of</strong> a Level 5 <strong>of</strong>fice visit or<br />
consultation several days prior to an admission <strong>and</strong> on the day <strong>of</strong> admission performs less than a<br />
comprehensive history <strong>and</strong> physical, he or she should report the <strong>of</strong>fice visit or consultation that reflects<br />
5-31<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
the services furnished <strong>and</strong> also report the lowest level initial hospital care code (i.e., code 99221) for the<br />
initial hospital admission. Carriers pay the <strong>of</strong>fice visit as billed <strong>and</strong> the Level 1 initial hospital care code.<br />
F. Initial Hospital Care Visits by Two Different M.D.s or D.O.s When They Are Involved in Same<br />
Admission<br />
Physicians use the initial hospital care codes (codes 99221-99223) to report the first hospital inpatient<br />
encounter with the patient when he or she is the admitting physician.<br />
Carriers consider only one M.D. or D.O. to be the admitting physician <strong>and</strong> permit only the admitting<br />
physician to use the initial hospital care codes. Physicians that participate in the care <strong>of</strong> a patient but are<br />
not the admitting physician <strong>of</strong> record should bill the inpatient evaluation <strong>and</strong> management services codes<br />
that describe their participation in the patient’s care (i.e., subsequent hospital visit or inpatient<br />
consultation).<br />
G. Initial Hospital Care <strong>and</strong> Nursing Facility Visit on Same Day<br />
Carriers pay only the initial hospital care code if the patient is admitted to a hospital following a nursing<br />
facility visit on the same date by the same physician. Payment for the initial hospital care service includes<br />
all work performed by the physician in all sites <strong>of</strong> service on that date.<br />
Subsequent Hospital Visit <strong>and</strong> Hospital Discharge Management<br />
Medicare Claims Processing Manual Chapter 12 §30.6.9.2 (Codes 99231-99239) (Rev. 1, 10-01-03)<br />
A. Subsequent Hospital Visit <strong>and</strong> Discharge Management on Same Day<br />
Carriers only pay the hospital discharge management code on the day <strong>of</strong> discharge (unless it is also the<br />
day <strong>of</strong> admission, in which case, the admission service <strong>and</strong> not the discharge management service is<br />
billed). Carriers do not pay both a subsequent hospital visit in addition to hospital discharge day<br />
management service on the same day by the same physician.<br />
B. Hospital Discharge Management (CPT Codes 99238 <strong>and</strong> 99239) <strong>and</strong> Nursing Facility Admission<br />
Code When Patient Is Discharged From Hospital <strong>and</strong> Admitted to Nursing Facility on Same Day<br />
Carriers pay the hospital discharge code (codes 99238 or 99239) in addition to a nursing facility<br />
admission code when they are billed by the same physician with the same date <strong>of</strong> service.<br />
Face-to-Face Visit Required for Discharge Services<br />
All E/M services except where specifically stated (e.g., care plan oversight which is a monthly summary)<br />
require a face-to-face interaction between the physician <strong>and</strong> the patient. The discharge service is a face-t<strong>of</strong>ace<br />
E/M service.<br />
Carriers monitoring for the time period April 2004 through March 2005, the date <strong>of</strong> service (DOS) <strong>of</strong><br />
seven (7) to fifteen (15) percent <strong>of</strong> the discharge service codes (99238, 99239, 99315, <strong>and</strong> 99316)<br />
submitted were the same as the date <strong>of</strong> death <strong>of</strong> the patient.<br />
CMS provided the following information regarding the use <strong>of</strong> time-based codes:<br />
The discharge day management service by definition does not have the elements <strong>of</strong> history,<br />
physical examination, <strong>and</strong> medical decision-making, as many <strong>of</strong> the other E/M codes have. The<br />
provider uses this final visit as appropriate, for a final examination, discussion <strong>of</strong> problems,<br />
instructions, <strong>and</strong> follow-up. A provider may choose to bill a subsequent hospital visit service code<br />
instead <strong>of</strong> a discharge service code. The provider is not required to bill a discharge day<br />
management service.<br />
The discharge day management service is a time-based service. In order to support services that<br />
require greater than 30 minutes (codes 99239 <strong>and</strong> 99316) the total time spent must be<br />
5-32<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
documented. If the time is not documented, payment is allowed for the lower level services<br />
(99238 <strong>and</strong> 99315).<br />
A discharge day management service can be split/shared between the nonphysician practitioner<br />
(NPP) <strong>and</strong> physician. When the service is shared between a physician <strong>and</strong> an NPP from the same<br />
group practice <strong>and</strong> the physician provides any face-to-face portion <strong>of</strong> the E/M encounter with the<br />
patient, the service may be billed under either the physician’s or the NPP’s UPIN/PIN number.<br />
However, if there was no face-to-face encounter between the patient <strong>and</strong> the physician (e.g., even<br />
if the physician participated in the service by reviewing the patient’s medical record), the service<br />
must be billed under the NPP’s rendering provider number (PIN).<br />
Medicare will pay for pronouncement <strong>of</strong> death as long as the provider actually does the<br />
pronouncement face-to-face with the deceased patient (not over the telephone). There must be<br />
documentation supporting a face-to-face encounter when billing a discharge service on the date <strong>of</strong><br />
death. If the provider does not see the patient prior to the time <strong>of</strong> death or make the<br />
pronouncement <strong>of</strong> death face-to-face, no E/M service may be billed for that date <strong>of</strong> service.<br />
Medicare Certified Swing Bed Hospital Services<br />
MLN Matters Number: SE0606<br />
Under the Social Security Act (§1883(a)(1), [42 U.S.C. 1395tt]), any hospital that has an agreement under<br />
§1866 may enter into an agreement with CMS in which its inpatient hospital facilities may be used for<br />
furnishing types <strong>of</strong> service that, if furnished in a Skilled Nursing Facility (SNF), would constitute<br />
extended care services (subject to §1883(b)). Such a hospital is known as a swing bed hospital.<br />
Services Covered in a Medicare Certified Swing Bed<br />
Under the Social Security Act, Section 1883(a)(1), payment for swing bed services will be made only for<br />
services for which payment would be made as post-hospital extended care services if those services had<br />
been furnished by an SNF<br />
CONSULTATIONS – CPT CODES 99241-99255<br />
Medicare Claims Processing Manual – Chapter 12 §30.6.10 (Codes 99241 99275) (Rev. 1, 10-01-03) B3-<br />
15506 (Rev. 782, Issued 12-16-05 Effective 01-01-06 Implementation 01-17-06)<br />
A. Consultation Services versus Other Evaluation <strong>and</strong> Management (E/M) Visits<br />
Carriers pay for a reasonable <strong>and</strong> medically necessary consultation service when all <strong>of</strong> the following<br />
criteria for the use <strong>of</strong> a consultation code are met:<br />
• Specifically, a consultation service is distinguished from other evaluation <strong>and</strong> management (E/M)<br />
visits because it is provided by a physician or qualified nonphysician practitioner (NPP) whose<br />
opinion or advice regarding evaluation <strong>and</strong>/or management <strong>of</strong> a specific problem is requested by<br />
another physician or other appropriate source. The qualified NPP may perform consultation<br />
services within the scope <strong>of</strong> practice <strong>and</strong> licensure requirements for NPPs in the State in which<br />
he/she practices. Applicable collaboration <strong>and</strong> general supervision rules apply as well as billing<br />
rules;<br />
• A request for a consultation from an appropriate source <strong>and</strong> the need for consultation (i.e., the<br />
reason for a consultation service) shall be documented by the consultant in the patient’s medical<br />
record <strong>and</strong> included in the requesting physician or qualified NPP’s plan <strong>of</strong> care in the patient’s<br />
medical record; <strong>and</strong><br />
• After the consultation is provided, the consultant shall prepare a written report <strong>of</strong> his/her findings<br />
<strong>and</strong> recommendations, which shall be provided to the referring physician.<br />
5-33<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
The intent <strong>of</strong> a consultation service is that a physician or qualified NPP or other appropriate source is<br />
asking another physician or qualified NPP for advice, opinion, a recommendation, suggestion, direction,<br />
or counsel, etc. in evaluating or treating a patient because that individual has expertise in a specific<br />
medical area beyond the requesting pr<strong>of</strong>essional’s knowledge. Consultations may be billed based on time<br />
if the counseling/coordination <strong>of</strong> care constitutes more than 50 percent <strong>of</strong> the face-to-face encounter<br />
between the physician or qualified NPP <strong>and</strong> the patient. The preceding requirements (request, evaluation<br />
(or counseling/coordination) <strong>and</strong> written report) shall also be met when the consultation is based on time<br />
for counseling/coordination.<br />
A consultation shall not be performed as a split/shared E/M visit.<br />
B. Consultation Followed by Treatment<br />
A physician or qualified NPP consultant may initiate diagnostic services <strong>and</strong> treatment at the initial<br />
consultation service or subsequent visit. Ongoing management, following the initial consultation service<br />
by the consultant physician, shall not be reported with consultation service codes. These services shall be<br />
reported as subsequent visits for the appropriate place <strong>of</strong> service <strong>and</strong> level <strong>of</strong> service. Payment for a<br />
consultation service shall be made regardless <strong>of</strong> treatment initiation unless a transfer <strong>of</strong> care occurs.<br />
Transfer <strong>of</strong> Care<br />
A transfer <strong>of</strong> care occurs when a physician or qualified NPP requests that another physician or qualified<br />
NPP take over the responsibility for managing the patients’ complete care for the condition <strong>and</strong> does not<br />
expect to continue treating or caring for the patient for that condition.<br />
When this transfer is arranged, the requesting physician or qualified NPP is not asking for an opinion or<br />
advice to personally treat this patient <strong>and</strong> is not expecting to continue treating the patient for the<br />
condition. The receiving physician or qualified NPP shall document this transfer <strong>of</strong> the patient’s care, to<br />
his/her service, in the patient’s medical record or plan <strong>of</strong> care.<br />
In a transfer <strong>of</strong> care, the receiving physician or qualified NPP would report the appropriate new or<br />
established patient visit code according to the place <strong>of</strong> service <strong>and</strong> level <strong>of</strong> service performed <strong>and</strong> shall<br />
not report a consultation service.<br />
C. Initial <strong>and</strong> Follow-Up Consultation Services<br />
Initial Consultation Service<br />
In the hospital setting, the consulting physician or qualified NPP shall use the appropriate Initial Inpatient<br />
Consultation codes (99251 – 99255) for the initial consultation service. In the nursing facility setting, the<br />
consulting physician or qualified NPP shall use the appropriate Initial Inpatient Consultation codes<br />
(99251 – 99255) for the initial consultation service. The Initial Inpatient Consultation may be reported<br />
only once per consultant per patient per facility admission.<br />
In the <strong>of</strong>fice or other outpatient setting, the consulting physician, or qualified NPP shall use the<br />
appropriate Office or Other Outpatient Consultation (new or established patient) codes (99241 – 99245)<br />
for the initial consultation service.<br />
If an additional request for an opinion or advice, regarding the same or a new problem with the same<br />
patient, is received from the same or another physician or qualified NPP <strong>and</strong> documented in the medical<br />
record, the Office or Other Outpatient Consultation (new or established patient) codes (99241 – 99245)<br />
may be used again. However, if the consultant continues to care for the patient for the original condition<br />
following his/her initial consultation, repeat consultation services shall not be reported by this physician<br />
or qualified NPP during his/her ongoing management <strong>of</strong> this condition.<br />
5-34<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
Follow-Up Consultation Service<br />
Effective January 1, 2006, the follow-up inpatient consultation codes (99261 – 99263) are deleted.<br />
In the hospital setting, following the initial consultation service, the Subsequent Hospital Care codes<br />
(99231 – 99233) shall be reported for additional follow-up visits.<br />
In the nursing facility setting, following the initial consultation service, the Subsequent Nursing Facility<br />
(NF) Care codes (new CPT codes 99307 – 99310) shall be reported for additional follow-up visits.<br />
Effective January 1, 2006, CPT codes 99311 – 99313 are deleted <strong>and</strong> not valid for Subsequent NF visits.<br />
In the <strong>of</strong>fice or other outpatient setting, following the initial consultation service, the Office or Other<br />
Outpatient Established Patient codes (99212 – 99215) shall be reported for additional follow-up visits.<br />
The CPT code 99211 shall not be reported as a consultation service. The CPT code 99211 is not included<br />
by Medicare for a consultation service since this service typically does not require the presence <strong>of</strong> a<br />
physician or qualified NPP <strong>and</strong> would not meet the consultation service criteria.<br />
D. Second Opinion E/M Service Requests<br />
Effective January 1, 2006, the Confirmatory Consultation codes (99271 – 99275) are deleted.<br />
A second opinion E/M service is a request by the patient <strong>and</strong>/or family or m<strong>and</strong>ated (e.g., by a third-party<br />
payer) <strong>and</strong> is not requested by a physician or qualified NPP. A consultation service requested by a<br />
physician, qualified NPP or other appropriate source that meets the requirements stated in Section A shall<br />
be reported using the initial consultation service codes as discussed in Section C. A written report is not<br />
required by Medicare to be sent to a physician when an evaluation for a second opinion has been<br />
requested by the patient <strong>and</strong>/or family.<br />
A second opinion, for Medicare purposes, is generally performed as a request for a second or third<br />
opinion <strong>of</strong> a previously recommended medical treatment or surgical procedure. A second opinion E/M<br />
service initiated by a patient <strong>and</strong>/or family is not reported using the consultation codes.<br />
In both the inpatient hospital setting <strong>and</strong> the NF setting, a request for a second opinion would be made<br />
through the attending physician or physician <strong>of</strong> record. If an initial consultation is requested <strong>of</strong> another<br />
physician or qualified NPP by the attending physician <strong>and</strong> meets the requirements for a consultation<br />
service (as identified in Section A) then the appropriate Initial Inpatient Consultation code shall be<br />
reported by the consultant. If the service does not meet the consultation requirements, then the E/M<br />
service shall be reported using the Subsequent Hospital Care codes (99231 – 99233) in the inpatient<br />
hospital setting <strong>and</strong> the Subsequent NF Care codes (99307 – 99310) in the NF setting.<br />
A second opinion E/M service performed in the <strong>of</strong>fice or other outpatient setting shall be reported using<br />
the Office or Other Outpatient new patient codes (99201 – 99205) for a new patient <strong>and</strong> established<br />
patient codes (99212 – 99215) for an established patient, as appropriate. The 3 year rule regarding “new<br />
patient” status applies. Any medically necessary follow-up visits shall be reported using the appropriate<br />
subsequent visit/established patient E/M visit codes.<br />
The CPT modifier -32 (M<strong>and</strong>ated Services) is not recognized as a payment modifier in Medicare. A<br />
second opinion evaluation service to satisfy a requirement for a third party payer is not a covered service<br />
in Medicare.<br />
E. Consultations Requested by Members <strong>of</strong> Same Group<br />
Carriers pay for a consultation if one physician or qualified NPP in a group practice requests a<br />
consultation from another physician in the same group practice when the consulting physician or qualified<br />
5-35<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
NPP has expertise in a specific medical area beyond the requesting pr<strong>of</strong>essional’s knowledge. A<br />
consultation service shall not be reported on every patient as a routine practice between physicians <strong>and</strong><br />
qualified NPPs within a group practice setting.<br />
F. Documentation for Consultation Services<br />
Consultation Request<br />
• A written request for a consultation from an appropriate source <strong>and</strong> the need for a consultation<br />
must be documented in the patient’s medical record. The initial request may be a verbal<br />
interaction between the requesting physician <strong>and</strong> the consulting physician; however, the verbal<br />
conversation shall be documented in the patient’s medical record, indicating a request for a<br />
consultation service was made by the requesting physician or qualified NPP.<br />
• The reason for the consultation service shall be documented by the consultant (physician or<br />
qualified NPP) in the patient’s medical record <strong>and</strong> included in the requesting physician or<br />
qualified NPP’s plan <strong>of</strong> care. The consultation service request may be written on a physician<br />
order form by the requestor in a shared medical record.<br />
Consultation Report<br />
• A written report shall be furnished to the requesting physician or qualified NPP.<br />
In an emergency department or an inpatient or outpatient setting in which the medical record is shared<br />
between the referring physician or qualified NPP <strong>and</strong> the consultant, the request may be documented as<br />
part <strong>of</strong> a plan written in the requesting physician or qualified NPP’s progress note, an order in the medical<br />
record, or a specific written request for the consultation. In these settings, the report may consist <strong>of</strong> an<br />
appropriate entry in the common medical record.<br />
In an <strong>of</strong>fice setting, the documentation requirement may be met by a specific written request for the<br />
consultation from the requesting physician or qualified NPP or if the consultant’s records show a specific<br />
reference to the request. In this setting, the consultation report is a separate document communicated to<br />
the requesting physician or qualified NPP.<br />
In a large group practice, e.g., an academic department or a large multi-specialty group, in which there is<br />
<strong>of</strong>ten a shared medical record, it is acceptable to include the consultant’s report in the medical record<br />
documentation <strong>and</strong> not require a separate letter from the consulting physician or qualified NPP to the<br />
requesting physician or qualified NPP. The written request <strong>and</strong> the consultation evaluation, findings <strong>and</strong><br />
recommendations shall be available in the consultation report.<br />
G. Consultation for Preoperative Clearance<br />
Preoperative consultations are payable for new or established patients performed by any physician or<br />
qualified NPP at the request <strong>of</strong> a surgeon, as long as all <strong>of</strong> the requirements for performing <strong>and</strong> <strong>reporting</strong><br />
the consultation codes are met <strong>and</strong> the service is medically necessary <strong>and</strong> not routine screening.<br />
H. Postoperative Care by Physician Who Did Preoperative Clearance Consultation<br />
If subsequent to the completion <strong>of</strong> a preoperative consultation in the <strong>of</strong>fice or hospital, the consultant<br />
assumes responsibility for the management <strong>of</strong> a portion or all <strong>of</strong> the patient’s condition(s) during the<br />
postoperative period, the consultation codes should not be used postoperatively. In the hospital setting,<br />
the physician or qualified NPP who has performed a preoperative consultation <strong>and</strong> assumes responsibility<br />
for the management <strong>of</strong> a portion or all <strong>of</strong> the patient’s condition(s) during the postoperative period should<br />
use the appropriate subsequent hospital care codes to bill for the concurrent care he or she is providing. In<br />
the <strong>of</strong>fice setting, the appropriate established patient visit codes should be used during the postoperative<br />
period.<br />
5-36<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
A physician (primary care or specialist) or qualified NPP who performs a postoperative evaluation <strong>of</strong> a<br />
new or established patient at the request <strong>of</strong> the surgeon may bill the appropriate consultation code for<br />
evaluation <strong>and</strong> management services furnished during the postoperative period following surgery when all<br />
<strong>of</strong> the criteria for the use <strong>of</strong> the consultation codes are met <strong>and</strong> that same physician has not already<br />
performed a preoperative consultation.<br />
I. Surgeon’s Request That Another Physician Participate In Postoperative Care<br />
If the surgeon asks a physician or qualified NPP who had been treating the patient preoperatively or who<br />
had not seen the patient for a preoperative consultation to take responsibility for the management <strong>of</strong> an<br />
aspect <strong>of</strong> the patient’s condition during the postoperative period, the physician or qualified NPP may not<br />
bill a consultation because the surgeon is not asking the physician or qualified NPP’s opinion or advice<br />
for the surgeon’s use in treating the patient. The physician or qualified NPP’s services would constitute<br />
concurrent care <strong>and</strong> should be billed using the appropriate subsequent hospital care codes in the hospital<br />
inpatient setting, subsequent NF care codes in the SNF/NF setting or the appropriate <strong>of</strong>fice or other<br />
outpatient visit codes in the <strong>of</strong>fice or outpatient settings.<br />
Physicians Regulatory Issues Team (PRIT) – Definition <strong>of</strong> a Consultation<br />
Issue<br />
The <strong>Indiana</strong> State Medical Association <strong>and</strong> others feel confused by the<br />
definition <strong>of</strong> Transfer <strong>of</strong> Care found in Transmittal 788.<br />
Status<br />
The PRIT is facilitating dialog between CMS staff, providers, <strong>and</strong><br />
carrier staff to clarify this definition.<br />
July 10<br />
August 28<br />
October 23, 2006<br />
January 11, 2007<br />
The PRIT has been contacted by the Infectious Disease Society <strong>of</strong><br />
America, the American College <strong>of</strong> Physicians, the American Medical<br />
Association <strong>and</strong> several other specialty societies about clarifying the<br />
definition <strong>of</strong> a consult in transmittal 788. We are working with them to<br />
address the issue.<br />
This issue was discussed at the August 28 2006 meeting <strong>of</strong> the<br />
Practicing Physician's Advisory Council.<br />
A letter signed by 51 medical associations <strong>and</strong> societies was sent to the<br />
CMS administration requesting clarification on this issue.<br />
There are instances <strong>of</strong> a “shared care” scenario which do meet the<br />
intent <strong>of</strong> a consultation. For example, a primary care physician consults<br />
with a specialist for a specific problem. The specialist evaluates the<br />
patient <strong>and</strong> continues to manage that aspect <strong>of</strong> the patient's care while<br />
the primary care physician continues to manage the overall patient care<br />
guided by the information from the specialist.<br />
Date Issue Created 06/15/2006<br />
EMERGENCY DEPARTMENT VISITS – CPT CODES 99281-99285<br />
Medicare Claims Processing Manual Chapter 12 §30.6.11 (Codes 99281-99288) (Rev. 1, 10-01-03) B3-<br />
15507<br />
A. Use <strong>of</strong> Emergency Department Codes by Physicians Not Assigned to Emergency Department<br />
Any physician seeing a patient registered in the emergency department may use emergency department<br />
visit codes (for services matching the code description). It is not required that the physician be assigned to<br />
the emergency department.<br />
5-37<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
B. Use <strong>of</strong> Emergency Department Codes in Office<br />
Emergency department <strong>coding</strong> is not appropriate if the site <strong>of</strong> service is an <strong>of</strong>fice or outpatient setting or<br />
any sight <strong>of</strong> service other than an emergency department. The emergency department codes should only<br />
be used if the patient is seen in the emergency department <strong>and</strong> the services described by the HCPCS code<br />
definition are provided. The emergency department is defined as an organized hospital-based facility for<br />
the provision <strong>of</strong> unscheduled or episodic services to patients who present for immediate medical attention.<br />
C. Use <strong>of</strong> Emergency Department Codes to Bill Nonemergency Services<br />
Services in the emergency department may not be emergencies. However, the codes (99281-99288) are<br />
payable if the described services are provided.<br />
However, if the physician asks the patient to meet him or her in the emergency department as an<br />
alternative to the physician’s <strong>of</strong>fice <strong>and</strong> the patient is not registered as a patient in the emergency<br />
department, the physician should bill the appropriate <strong>of</strong>fice/outpatient visit codes. Normally a lower level<br />
<strong>of</strong> emergency department code would be reported for a nonemergency condition.<br />
D. Emergency Department or Office/Outpatient Visits on Same Day as Nursing Facility Admission<br />
Emergency department visit provided on the same day as a comprehensive nursing facility assessment are<br />
not paid. Payment for evaluation <strong>and</strong> management services on the same date provided in sites other than<br />
the nursing facility are included in the payment for initial nursing facility care when performed on the<br />
same date as the nursing facility admission.<br />
E. Physician Billing for Emergency Department Services Provided to Patient by Both Patient’s Personal<br />
Physician <strong>and</strong> Emergency Department Physician<br />
If a physician advises his/her own patient to go to an emergency department (ED) <strong>of</strong> a hospital for care<br />
<strong>and</strong> the physician subsequently is asked by the ED physician to come to the hospital to evaluate the<br />
patient <strong>and</strong> to advise the ED physician as to whether the patient should be admitted to the hospital or be<br />
sent home, the physicians should bill as follows:<br />
• If the patient is admitted to the hospital by the patient’s personal physician, then the patient’s<br />
regular physician should bill only the appropriate level <strong>of</strong> the initial hospital care (codes 99221-<br />
99223) because all evaluation <strong>and</strong> management services provided by that physician in<br />
conjunction with that admission are considered part <strong>of</strong> the initial hospital care when performed on<br />
the same date as the admission. The ED physician who saw the patient in the emergency<br />
department should bill the appropriate level <strong>of</strong> the ED codes.<br />
• If the ED physician, based on the advice <strong>of</strong> the patient’s personal physician who came to the<br />
emergency department to see the patient, sends the patient home, then the ED physician should<br />
bill the appropriate level <strong>of</strong> emergency department service. The patient’s personal physician<br />
should also bill the level <strong>of</strong> emergency department code that describes the service he or she<br />
provided in the emergency department. The patient’s personal physician would not bill a<br />
consultation because he or she is not providing information to the emergency department<br />
physician for his or her use in treating the patient. If the patient’s personal physician does not<br />
come to the hospital to see the patient, but only advises the emergency department physician by<br />
telephone, then the patient’s personal physician may not bill.<br />
NURSING FACILITY VISITS – CPT CODES 99304-99316<br />
Initial Nursing Facility Care<br />
Codes 99304-99306 are selected based on the type <strong>of</strong> history, exam, <strong>and</strong> medical decision making based<br />
which will be based on the patient’s problem(s) requiring admission to the facility. Typical times have not<br />
been established. CPT provides guidance for selecting the appropriate level <strong>of</strong> admission by giving the<br />
5-38<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
typical severity <strong>of</strong> the problem(s) requiring admission. These codes should be reported by the admitting<br />
physician responsible for the care <strong>of</strong> the patient during the inpatient stay.<br />
Annual Nursing Facility Services<br />
Code 99318 is used to describe the annual nursing facility assessment. This code must include a detailed<br />
interval history, a comprehensive examination, <strong>and</strong> medical decision making that is <strong>of</strong> low to moderate<br />
complexity. These patients are usually stable, recovering, or improving. Physicians should not report<br />
99318 on the same day as subsequent nursing facility codes 99307-99310.<br />
Subsequent Nursing Facility Care<br />
Codes 99307-99310 are selected based on the type <strong>of</strong> history, exam, <strong>and</strong> medical decision making which<br />
will be based on the patient’s presenting problem(s). Typical times have not been established. CPT<br />
provides guidance for selecting the appropriate level <strong>of</strong> admission by the patient’s status, e.g., stable,<br />
inadequate response to therapy, new problem, etc.<br />
Nursing Facility Discharge<br />
Discharge day management services are coded 99315 or 99316. The codes are selected based on the<br />
amount <strong>of</strong> time spent for the final discharge from the nursing facility.<br />
Medicare Guidelines for Nursing Facility Coding<br />
Medicare Claims Processing Manual Chapter 12 §30.6.13 (Rev. 1, 10-01-03) B3-15509-15509.1 (Rev.<br />
808 Implementation No later than 01-23-06)<br />
A. Visits to Perform the Initial Comprehensive Assessment <strong>and</strong> Annual Assessments<br />
The distinction made between the delegation <strong>of</strong> physician visits <strong>and</strong> tasks in a skilled nursing facility<br />
(SNF) <strong>and</strong> in a nursing facility (NF) is based on the Medicare Statute. §1819 (b) (6) (A) <strong>of</strong> the Social<br />
Security Act (the Act) governs SNFs while §1919(b)(6)(A) <strong>of</strong> the Act governs NFs. For further<br />
information, refer to Medlearn Matters article number SE0418 at www.cms.hhs.gov/medlearn/matters<br />
The initial visit in a SNF <strong>and</strong> NF must be performed by the physician except as otherwise permitted<br />
(42CFR483.40(c)(4)). The initial visit is defined in as the initial comprehensive assessment visit during<br />
which the physician [Emphasis Added] completes a thorough assessment, develops a plan <strong>of</strong> care <strong>and</strong><br />
writes or verifies admitting orders for the nursing facility resident. For Survey <strong>and</strong> Certification<br />
requirements, a visit must occur no later than 30 days after admission.<br />
Further, per the Long Term Care regulations at 42CFR483.40(c)(4) <strong>and</strong> (e)(2), the physician may not<br />
delegate [Emphasis Added] a task that the physician must personally perform. Therefore, the physician<br />
may not delegate the initial visit in a SNF. This also applies to the NF with one exception.<br />
The only exception, as to who performs the initial visit, relates to the NF setting [Emphasis Added]. In<br />
the NF setting, a qualified NPP [Emphasis Added] (i.e., a nurse practitioner (NP), physician assistant<br />
(PA), or a clinical nurse specialist (CNS), who is not employed by the facility, may perform the initial<br />
visit [Emphasis Added] when the State law permits. The evaluation <strong>and</strong> management (E/M) visit shall be<br />
within the State scope <strong>of</strong> practice <strong>and</strong> licensure requirements where the E/M visit is performed <strong>and</strong> the<br />
requirements for physician collaboration <strong>and</strong> physician supervision shall be met.<br />
Under Medicare Part B payment policy, other medically necessary E/M visits may be performed <strong>and</strong><br />
reported prior to <strong>and</strong> after the initial visit, if the medical needs <strong>of</strong> the patient require an E/M visit. A<br />
qualified NPP may perform medically necessary E/M visits prior to <strong>and</strong> after the initial visit if all the<br />
requirements for collaboration, general physician supervision, licensure <strong>and</strong> billing are met.<br />
5-39<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
The CPT Nursing Facility Services codes shall be used with place <strong>of</strong> service (POS) 31 (SNF) if the<br />
patient is in a Part A SNF stay. They shall be used with POS 32 (nursing facility) if the patient does not<br />
have Part A SNF benefits or if the patient is in a NF or in a non-covered SNF stay (e.g., there was no<br />
preceding 3-day hospital stay). The CPT Nursing Facility code definition also includes POS 54<br />
(Intermediate Care Facility/Mentally Retarded) <strong>and</strong> POS 56 (Psychiatric Residential Treatment Center).<br />
Initial Nursing Facility Care, per day, (99304–99306) are used to report the initial visit. Only a physician<br />
may report these codes for an initial visit performed in a SNF or NF (with the exception <strong>of</strong> the qualified<br />
NPP in the NF setting who is not employed by the facility <strong>and</strong> when State law permits, as explained<br />
above).<br />
A readmission to a SNF or NF shall have the same payment policy requirements as an initial admission in<br />
both the SNF <strong>and</strong> NF settings.<br />
A physician who is employed by the SNF/NF may perform the E/M visits <strong>and</strong> bill independently to<br />
Medicare Part B for payment. An NPP who is employed by the SNF or NF may perform <strong>and</strong> bill<br />
Medicare Part B directly for those services where it is permitted as discussed above. The employer <strong>of</strong> the<br />
PA shall always report the visits performed by the PA. A physician, NP or CNS has the option to bill<br />
Medicare directly or to reassign payment for his/her pr<strong>of</strong>essional service to the facility.<br />
As with all E/M visits for Medicare Part B payment policy, the E/M documentation guidelines apply.<br />
B. Visits to Comply With Federal Regulations (42 CFR 483.40 (c) (1)) in the SNF <strong>and</strong> NF<br />
Payment is made under the physician fee schedule by Medicare Part B for federally m<strong>and</strong>ated visits.<br />
Following the initial visit by the physician, payment shall be made for federally m<strong>and</strong>ated visits that<br />
monitor <strong>and</strong> evaluate residents at least once every 30 days for the first 90 days after admission <strong>and</strong> at least<br />
once every 60 days thereafter.<br />
Subsequent Nursing Facility Care, per day, codes 99307–99310 are used to report federally m<strong>and</strong>ated<br />
physician E/M visits <strong>and</strong> medically necessary E/M visits.<br />
Carriers shall not pay for more than one E/M visit performed by the physician or qualified NPP for the<br />
same patient on the same date <strong>of</strong> service. The Nursing Facility Services codes represent a “per day”<br />
service.<br />
The federally m<strong>and</strong>ated E/M visit may serve also as a medically necessary E/M visit if the situation arises<br />
(i.e., the patient has health problems that need attention on the day the scheduled m<strong>and</strong>ated physician E/M<br />
visit occurs). The physician/qualified NPP shall bill only one E/M visit.<br />
Other Nursing Facility Service (99318), is used to report an annual nursing facility assessment visit on the<br />
required schedule <strong>of</strong> visits on an annual basis. For Medicare Part B payment policy, an annual nursing<br />
facility assessment visit code may substitute as meeting one <strong>of</strong> the federally m<strong>and</strong>ated physician visits if<br />
the code requirements for CPT code 99318 are fully met <strong>and</strong> in lieu <strong>of</strong> <strong>reporting</strong> a Subsequent Nursing<br />
Facility Care, per day, service (codes 99307–99310). It shall not be performed in addition to the required<br />
number <strong>of</strong> federally m<strong>and</strong>ated physician visits. Qualified NPPs, whether employed or not by the SNF,<br />
may perform alternating federally m<strong>and</strong>ated physician visits, at the option <strong>of</strong> the physician, after the<br />
initial visit by the physician in a SNF.<br />
Qualified NPPs in the NF setting, who are not employed by the NF, may perform federally m<strong>and</strong>ated<br />
physician visits, at the option <strong>of</strong> the State, after the initial visit by the physician.<br />
5-40<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
Medicare Part B payment policy does not pay for additional E/M visits that may be required by State law<br />
for a facility admission or for other additional visits to satisfy facility or other administrative purposes.<br />
E/M visits, prior to <strong>and</strong> after the initial physician visit, that are reasonable <strong>and</strong> medically necessary to<br />
meet the medical needs <strong>of</strong> the individual patient (unrelated to any State requirement or administrative<br />
purpose) are payable under Medicare Part B.<br />
C. Visits by Qualified Nonphysician Practitioners<br />
All E/M visits shall be within the State scope <strong>of</strong> practice <strong>and</strong> licensure requirements where the visit is<br />
performed <strong>and</strong> all the requirements for physician collaboration <strong>and</strong> physician supervision shall be met<br />
when performed <strong>and</strong> reported by qualified NPPs. General physician supervision <strong>and</strong> employer billing<br />
requirements shall be met for PA services in addition to the PA meeting the State scope <strong>of</strong> practice <strong>and</strong><br />
licensure requirements where the E/M visit is performed.<br />
Medically Necessary Visits<br />
Qualified NPPs may perform medically necessary E/M visits prior to <strong>and</strong> after the physician’s initial visit<br />
in both the SNF <strong>and</strong> NF. Medically necessary E/M visits for the diagnosis or treatment <strong>of</strong> an illness or<br />
injury or to improve the functioning <strong>of</strong> a malformed body member are payable under the physician fee<br />
schedule under Medicare Part B. CPT codes, Subsequent Nursing Facility Care, per day (99307-99310),<br />
shall be reported for these E/M visits even if the visits are provided prior to the initial visit by the<br />
physician.<br />
SNF Setting--Place <strong>of</strong> Service Code 31<br />
Following the initial visit by the physician, the physician may delegate alternate federally m<strong>and</strong>ated<br />
physician visits to a qualified NPP who meets collaboration <strong>and</strong> physician supervision requirements <strong>and</strong><br />
is licensed as such by the State <strong>and</strong> performing within the scope <strong>of</strong> practice in that State.<br />
NF Setting--Place <strong>of</strong> Service Code 32<br />
Per the regulations at 42CFR483.40(f), a qualified NPP, who meets the collaboration <strong>and</strong> physician<br />
supervision requirements, the State scope <strong>of</strong> practice <strong>and</strong> licensure requirements, <strong>and</strong> who is not<br />
employed by the NF, may at the option <strong>of</strong> the State, perform the initial visit in a NF, <strong>and</strong> may perform<br />
any other federally m<strong>and</strong>ated physician visit in a NF in addition to performing other medically necessary<br />
E/M visits.<br />
Questions pertaining to writing orders or certification <strong>and</strong> recertification issues in the SNF <strong>and</strong> NF<br />
settings shall be addressed to the appropriate State Survey <strong>and</strong> Certification Agency departments for<br />
clarification.<br />
D. Medically Complex Care<br />
Payment is made for E/M visits to patients in a SNF who are receiving services for medically complex<br />
care upon discharge from an acute care facility when the visits are reasonable <strong>and</strong> medically necessary<br />
<strong>and</strong> documented in the medical record. Physicians <strong>and</strong> qualified NPPs shall report E/M visits using the<br />
Subsequent Nursing Facility Care, per day (codes 99307-99310) for these E/M visits even if the visits are<br />
provided prior to the initial visit by the physician.<br />
E. Incident to Services<br />
Where a physician establishes an <strong>of</strong>fice in a SNF/NF, the “incident to” services <strong>and</strong> requirements are<br />
confined to this discrete part <strong>of</strong> the facility designated as his/her <strong>of</strong>fice. “Incident to” E/M visits, provided<br />
in a facility setting, are not payable under the Physician Fee Schedule for Medicare Part B. Thus, visits<br />
performed outside the designated “<strong>of</strong>fice” area in the SNF/NF would be subject to the coverage <strong>and</strong><br />
payment rules applicable to SNF/NF setting <strong>and</strong> shall not be reported using the CPT codes for <strong>of</strong>fice or<br />
other outpatient visits or use place <strong>of</strong> service code 11.<br />
5-41<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
F. Not Pertinent to this H<strong>and</strong>out<br />
G. Not Pertinent to this H<strong>and</strong>out<br />
H. Split/Shared E/M Visit<br />
A split/shared E/M visit cannot [Emphasis Added] be reported in the SNF/NF setting. A split/shared E/M<br />
visit is defined by Medicare Part B payment policy as a medically necessary encounter with a patient<br />
where the physician <strong>and</strong> a qualified NPP each personally perform a substantive portion <strong>of</strong> an E/M visit<br />
face-to-face with the same patient on the same date <strong>of</strong> service. A substantive portion <strong>of</strong> an E/M visit<br />
involves all or some portion <strong>of</strong> the history, exam, or medical decision making key components <strong>of</strong> an E/M<br />
service. The physician <strong>and</strong> the qualified NPP must be in the same group practice or be employed by the<br />
same employer. The split/shared E/M visit applies only to selected E/M visits <strong>and</strong> settings (i.e., hospital<br />
inpatient, hospital outpatient, hospital observation, emergency department, hospital discharge, <strong>of</strong>fice <strong>and</strong><br />
non facility clinic visits, <strong>and</strong> prolonged visits associated with these E/M visit codes). The split/shared E/M<br />
policy does not apply to consultation services, critical care services, or procedures.<br />
I. SNF/NF Discharge Day Management Service<br />
Medicare Part B payment policy requires a face-to-face visit with the patient provided by the physician or<br />
the qualified NPP to meet the SNF/NF discharge day management service as defined by the CPT code.<br />
The E/M discharge day management visit shall be reported for the date <strong>of</strong> the actual visit by the physician<br />
or qualified NPP even if the patient is discharged from the facility on a different calendar date. The CPT<br />
codes 99315 – 99316 shall be reported for this visit. The Discharge Day Management Service may be<br />
reported using CPT code 99315 or 99316, depending on the code requirement, for a patient who has<br />
expired, but only if the physician or qualified NPP personally performed the death pronouncement.<br />
99315 30 minutes or less<br />
99316 greater than 30 minutes<br />
DOMICILIARY CARE – CPT CODES 99324-99337<br />
There are five levels <strong>of</strong> care for the evaluation <strong>and</strong> management <strong>of</strong> new patients. Codes 99324-99328<br />
include the type <strong>of</strong> history, exam, <strong>and</strong> medical decision making as well as the typical time spent<br />
performing the service. Thus, these codes can be selected by time with more than 50 percent <strong>of</strong> the time is<br />
spent in counseling or coordination <strong>of</strong> care.<br />
Codes 99334-99337 provide four levels <strong>of</strong> care for the evaluation <strong>and</strong> management <strong>of</strong> established<br />
patients. These codes can be based on the content <strong>of</strong> the service provided (history, exam, <strong>and</strong> medical<br />
decision making) or by time when more than 50 percent <strong>of</strong> the time is spent in counseling or coordination<br />
<strong>of</strong> care.<br />
Place <strong>of</strong> service “13” - Assisted Living Facility – Definition: Congregate residential facility with selfcontained<br />
living units providing assessment <strong>of</strong> each resident's needs <strong>and</strong> on-site support 24 hours a day, 7<br />
days a week, with the capacity to deliver or arrange for services including some health care <strong>and</strong> other<br />
services.<br />
5-42<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
HOME SERVICES – CPT CODES 99341-99350<br />
Medicare Claims Processing Manual Chapter 12 §30.6.14.1 (Codes 99341-99350) (Rev. 1, 10-01-03) B3-<br />
15515, B3-15066<br />
A. Requirement for Physician Presence<br />
Home services codes 99341-99350 are paid when they are billed to report evaluation <strong>and</strong> management<br />
services provided in a private residence. A home visit cannot be billed by a physician unless the physician<br />
was actually present in the beneficiary’s home.<br />
B. Homebound Status<br />
Under the home health benefit, the beneficiary must be confined to the home for services to be covered.<br />
For home services provided by a physician using these codes, the beneficiary does not need to be<br />
confined to the home. The medical record must document the medical necessity <strong>of</strong> the home visit made<br />
in lieu <strong>of</strong> an <strong>of</strong>fice or outpatient visit. [Emphasis Added]<br />
SCREENING PAP SMEARS AND SCREENING PELVIC EXAMINATION<br />
(INCLUDING CLINICAL BREAST EXAM)<br />
Medicare Benefit Policy Manual Chapter 15 §280.4 (Rev. 1, 10-01-03) A3-3628.1, B3-4603.1<br />
Effective, July 1, 2001, the Consolidated Appropriations Act <strong>of</strong> 2001 (P.L. 106-554) modifies §1861(nn)<br />
to provide Medicare coverage for biennial screening Pap smears or more frequent coverage for women:<br />
1. At high-risk for cervical or vaginal cancer<br />
2. Of childbearing age who have had a Pap smear during any <strong>of</strong> the preceding three years indicating<br />
the presence <strong>of</strong> cervical or vaginal cancer or other abnormality<br />
Cervical Cancer High-Risk Factors<br />
1. Early onset <strong>of</strong> sexual activity (under 16 years <strong>of</strong> age)<br />
2. Multiple sexual partners (five (5) or more in a lifetime)<br />
3. History <strong>of</strong> a sexually transmitted disease (including HIV infection)<br />
4. Fewer than three negative or any Pap smears within the previous seven years<br />
Vaginal Cancer High Risk Factors<br />
1. DES (diethylstilbestrol) - exposed daughters <strong>of</strong> women who took DES during pregnancy<br />
The term “woman <strong>of</strong> childbearing age” means a woman who is premenopausal, <strong>and</strong> has been determined<br />
by a physician, or qualified practitioner, to be <strong>of</strong> childbearing age, based on her medical history or other<br />
findings. Payment is not made for a screening Pap smear for women at high-risk or who qualify for<br />
coverage under the childbearing provision more frequently than once every 11 months after the month<br />
that the last screening Pap smear covered by Medicare was performed.<br />
For Claims with Dates <strong>of</strong> Service on or After July 1, 2001<br />
When the beneficiary does not qualify for a more frequently performed screening Pap smear as noted in<br />
items 1 <strong>and</strong> 2 above, contractors pay for the screening Pap smear only after at least 23 months have<br />
passed following the month during which the beneficiary received her last covered screening Pap smear.<br />
All other coverage <strong>and</strong> payment requirements remain the same.<br />
5-43<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
Screening Pelvic Examinations<br />
Medicare Claims Processing Manual Chapter 18 §40 (Rev. 1, 10-01-03) B3-4603.2, A3-3, 3628.1B<br />
§4102 <strong>of</strong> the Balanced Budget Act <strong>of</strong> 1997 provides for coverage <strong>of</strong> screening pelvic examinations<br />
(including a clinical breast examination) for all female beneficiaries, subject to certain frequency <strong>and</strong><br />
other limitations.<br />
A screening pelvic examination (including a clinical breast examination) should include at least seven (7)<br />
<strong>of</strong> the following eleven (11) elements:<br />
• Inspection <strong>and</strong> palpation <strong>of</strong> breasts for masses or lumps, tenderness, symmetry, or nipple<br />
discharge<br />
• Digital rectal examination including sphincter tone, presence <strong>of</strong> hemorrhoids, <strong>and</strong> rectal masses<br />
Pelvic examination (with or without specimen collection for smears <strong>and</strong> cultures) including:<br />
• External genitalia (for example, general appearance, hair distribution, or lesions)<br />
• Urethral meatus (for example, size, location, lesions, or prolapse)<br />
• Urethra (for example, masses, tenderness, or scarring)<br />
• Bladder (for example, fullness, masses, or tenderness)<br />
• Vagina (for example, general appearance, estrogen effect, discharge lesions, pelvic support,<br />
cystocele, or rectocele)<br />
• Cervix (for example, general appearance, lesions, or discharge)<br />
• Uterus (for example, size, contour, position, mobility, tenderness, consistency, descent, or<br />
support)<br />
• Adnexa/parametria (for example, masses, tenderness, organomegaly, or nodularity)<br />
• Anus <strong>and</strong> perineum<br />
Coding for Screening Pelvic Examinations<br />
Medicare Claims Processing Manual Chapter 18 §40.2 (Rev. 1, 10-01-03) B3-4603.2.B <strong>and</strong> C, A3-<br />
3628.1.B.1<br />
A HCPCS code has been established for the pelvic <strong>and</strong> clinical breast examinations. Use code G0101<br />
(cervical or vaginal cancer screening, pelvic <strong>and</strong> clinical breast examination).<br />
Coding for Obtaining the Pap smear<br />
Medicare Claims Processing Manual Chapter 18 §30.5.D (Rev. 795, Issued: 12-30-05; Effective: 10-01-<br />
04; Implementation: 04-03-06)<br />
Use HCPCS code Q0091 to report the obtaining a screening pap smear during an encounter. This code is<br />
subject to the same frequencies <strong>and</strong> diagnoses as pelvic <strong>and</strong> clinical breast exam.<br />
Payment for Q0091 is paid under the Medicare physician fee schedule. Deductible is not applicable,<br />
however the coinsurance applies.<br />
Effective for services on <strong>and</strong> after July 1, 2005, on those occasions when physicians must perform a<br />
screening Pap smear (Q0091) that they know will not be covered by Medicare because the low risk<br />
patient has already received a covered Pap smear (Q0091) in the past 2 years, the physician can bill<br />
Q0091 <strong>and</strong> the claim will be denied appropriately.<br />
The physician shall obtain an advance beneficiary notice (ABN) in these situations as the denial will be<br />
considered a not reasonable <strong>and</strong> necessary denial. The physician indicates on the claim that an ABN has<br />
been obtained by using the GA modifier.<br />
Effective for services on or after April 1, 1999, a covered evaluation <strong>and</strong> management (E/M) visit <strong>and</strong><br />
code Q0091 may be reported by the same physician for the same date <strong>of</strong> service if the E/M visit is for a<br />
separately identifiable service. In this case, the modifier “-25” must be reported with the E/M service <strong>and</strong><br />
5-44<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
the medical records must clearly document the E/M reported. Both procedure codes should be shown as<br />
separate line items on the claim. These services can also be performed separately on separate <strong>of</strong>fice visits.<br />
Repeat Obtaining Screening Pap Smear Due To Inadequate Specimen<br />
Related Change Request (CR) #: 3659 Medlearn Matters Number: MM3659 Related CR Transmittal #:<br />
440 Implementation Date: July 5, 2005<br />
When a Pap smear specimen is not sufficient for the laboratory to interpret the results <strong>and</strong> another<br />
specimen is needed report Q0091 <strong>and</strong> append the -76 modifier to indicate it is a repeat specimen. The<br />
Carrier will pay for the collection <strong>of</strong> the specimen. Physicians should not report the screening pelvic<br />
examination again as the entire service is not medically necessary. It is also inappropriate to report an<br />
E/M code unless the patient has another problem needing a medically necessary evaluation on the same<br />
date <strong>of</strong> service.<br />
CMS Incident To Clarification<br />
CMS Region V clarified that screening pelvic examination with clinical breast exam (G0101) <strong>and</strong><br />
obtaining screening Pap smear (Q0091) cannot be billed “incident to” the physician’s services. The<br />
physician or nonphysician practitioner who PERFORMS the service(s) must report these screening<br />
services. This clarification applies to all screening services.<br />
Covered Diagnoses For Reporting Screening Pelvic Examination Or The Obtaining Of A Screening<br />
Pap Smear<br />
Medicare Claims Processing Manual Chapter 18 §30.6 (Rev. 1, 10-01-03) AB-03-054 (CR 2637) (Rev.<br />
440, Issued: 01-21-05, Effective: 07-01-05, Implementation: 07-05-05)<br />
Applicable Diagnoses for Billing a Carrier<br />
There are a number <strong>of</strong> appropriate diagnosis codes that can be used in billing for screening Pap smear<br />
services that the provider can list on the claim to give a true picture <strong>of</strong> the patient’s condition. To be<br />
covered one <strong>of</strong> the following diagnoses must be listed in Item 21 <strong>of</strong> Form CMS-1500 or the electronic<br />
equivalent.<br />
Below are the current diagnoses that should be used when billing for screening Pap smear services.<br />
Effective, July 1, 2005, V72.31 is being added to the CWF edit as an additional low risk diagnosis. The<br />
following chart lists the diagnosis codes that CWF must recognize for low risk or high-risk patients for<br />
screening Pap smear services.<br />
Low Risk Definitions<br />
Diagnosis Codes<br />
V76.2 Special screening for malignant neoplasms, cervix<br />
V76.47 Special screening for malignant neoplasm, vagina<br />
V76.49 Special screening for malignant neoplasm, other sites<br />
NOTE: providers use this diagnosis for women without a cervix.<br />
V72.31 Routine gynecological examination<br />
NOTE: This diagnosis should only be used when the provider<br />
performs a full gynecological examination.<br />
High Risk Diagnosis Code<br />
V15.89 Other<br />
If one <strong>of</strong> these diagnoses is not present or if the frequency requirements are not met, the CWF will reject<br />
the claim as “not medically necessary.”<br />
5-45<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.
RISK ASSESSMENT FORM<br />
A screening pelvic examination (including a clinical breast examination) <strong>and</strong>/or screening pap smear is a<br />
covered Medicare service once every two years, unless a patient is considered high-risk for cervical or<br />
vaginal cancer. Listed below are the criteria considered to be high-risk. If you meet any <strong>of</strong> the following,<br />
<strong>and</strong> wish to share this information with us, the screening pelvic <strong>and</strong>/or screening pap may be paid<br />
annually.<br />
_____ Childbearing age <strong>and</strong> have had an examination indicating the presence <strong>of</strong> cervical or<br />
vaginal cancer or other abnormality during any <strong>of</strong> the preceding three years<br />
_____ Early onset <strong>of</strong> sexual activity (under 16 years <strong>of</strong> age)<br />
_____ Multiple sexual partners (five or more in a lifetime)<br />
_____ History <strong>of</strong> sexually transmitted disease (including the human immunodeficiency virus<br />
[HIV])<br />
_____ Any <strong>of</strong> the last three pap smears were positive<br />
_____ No pap smear within the past seven years<br />
_____ Prenatal exposure to diethylstilbestrol<br />
OR<br />
_____ None <strong>of</strong> the above (payment may be made by Medicare once every two years)<br />
__________________________________________<br />
Signature<br />
________________________<br />
Date<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. IAFP Annual Meeting 2007<br />
Copyright 2007 Newby Consulting, Inc.<br />
46