pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
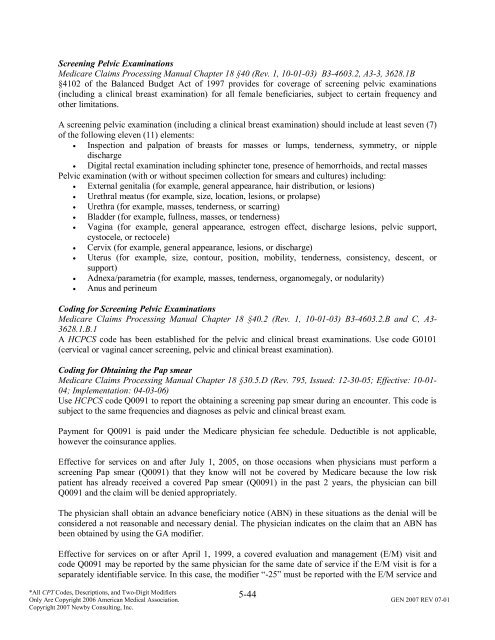
Screening Pelvic Examinations<br />
Medicare Claims Processing Manual Chapter 18 §40 (Rev. 1, 10-01-03) B3-4603.2, A3-3, 3628.1B<br />
§4102 <strong>of</strong> the Balanced Budget Act <strong>of</strong> 1997 provides for coverage <strong>of</strong> screening pelvic examinations<br />
(including a clinical breast examination) for all female beneficiaries, subject to certain frequency <strong>and</strong><br />
other limitations.<br />
A screening pelvic examination (including a clinical breast examination) should include at least seven (7)<br />
<strong>of</strong> the following eleven (11) elements:<br />
• Inspection <strong>and</strong> palpation <strong>of</strong> breasts for masses or lumps, tenderness, symmetry, or nipple<br />
discharge<br />
• Digital rectal examination including sphincter tone, presence <strong>of</strong> hemorrhoids, <strong>and</strong> rectal masses<br />
Pelvic examination (with or without specimen collection for smears <strong>and</strong> cultures) including:<br />
• External genitalia (for example, general appearance, hair distribution, or lesions)<br />
• Urethral meatus (for example, size, location, lesions, or prolapse)<br />
• Urethra (for example, masses, tenderness, or scarring)<br />
• Bladder (for example, fullness, masses, or tenderness)<br />
• Vagina (for example, general appearance, estrogen effect, discharge lesions, pelvic support,<br />
cystocele, or rectocele)<br />
• Cervix (for example, general appearance, lesions, or discharge)<br />
• Uterus (for example, size, contour, position, mobility, tenderness, consistency, descent, or<br />
support)<br />
• Adnexa/parametria (for example, masses, tenderness, organomegaly, or nodularity)<br />
• Anus <strong>and</strong> perineum<br />
Coding for Screening Pelvic Examinations<br />
Medicare Claims Processing Manual Chapter 18 §40.2 (Rev. 1, 10-01-03) B3-4603.2.B <strong>and</strong> C, A3-<br />
3628.1.B.1<br />
A HCPCS code has been established for the pelvic <strong>and</strong> clinical breast examinations. Use code G0101<br />
(cervical or vaginal cancer screening, pelvic <strong>and</strong> clinical breast examination).<br />
Coding for Obtaining the Pap smear<br />
Medicare Claims Processing Manual Chapter 18 §30.5.D (Rev. 795, Issued: 12-30-05; Effective: 10-01-<br />
04; Implementation: 04-03-06)<br />
Use HCPCS code Q0091 to report the obtaining a screening pap smear during an encounter. This code is<br />
subject to the same frequencies <strong>and</strong> diagnoses as pelvic <strong>and</strong> clinical breast exam.<br />
Payment for Q0091 is paid under the Medicare physician fee schedule. Deductible is not applicable,<br />
however the coinsurance applies.<br />
Effective for services on <strong>and</strong> after July 1, 2005, on those occasions when physicians must perform a<br />
screening Pap smear (Q0091) that they know will not be covered by Medicare because the low risk<br />
patient has already received a covered Pap smear (Q0091) in the past 2 years, the physician can bill<br />
Q0091 <strong>and</strong> the claim will be denied appropriately.<br />
The physician shall obtain an advance beneficiary notice (ABN) in these situations as the denial will be<br />
considered a not reasonable <strong>and</strong> necessary denial. The physician indicates on the claim that an ABN has<br />
been obtained by using the GA modifier.<br />
Effective for services on or after April 1, 1999, a covered evaluation <strong>and</strong> management (E/M) visit <strong>and</strong><br />
code Q0091 may be reported by the same physician for the same date <strong>of</strong> service if the E/M visit is for a<br />
separately identifiable service. In this case, the modifier “-25” must be reported with the E/M service <strong>and</strong><br />
5-44<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.