pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
pqri measure coding and reporting principles - Indiana Academy of ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
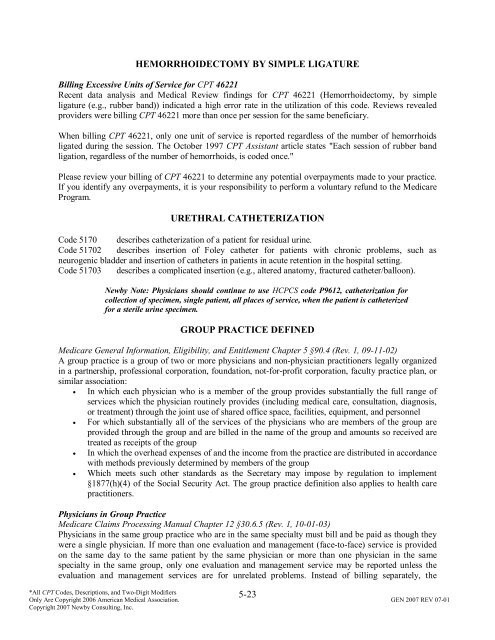
HEMORRHOIDECTOMY BY SIMPLE LIGATURE<br />
Billing Excessive Units <strong>of</strong> Service for CPT 46221<br />
Recent data analysis <strong>and</strong> Medical Review findings for CPT 46221 (Hemorrhoidectomy, by simple<br />
ligature (e.g., rubber b<strong>and</strong>)) indicated a high error rate in the utilization <strong>of</strong> this code. Reviews revealed<br />
providers were billing CPT 46221 more than once per session for the same beneficiary.<br />
When billing CPT 46221, only one unit <strong>of</strong> service is reported regardless <strong>of</strong> the number <strong>of</strong> hemorrhoids<br />
ligated during the session. The October 1997 CPT Assistant article states "Each session <strong>of</strong> rubber b<strong>and</strong><br />
ligation, regardless <strong>of</strong> the number <strong>of</strong> hemorrhoids, is coded once."<br />
Please review your billing <strong>of</strong> CPT 46221 to determine any potential overpayments made to your practice.<br />
If you identify any overpayments, it is your responsibility to perform a voluntary refund to the Medicare<br />
Program.<br />
URETHRAL CATHETERIZATION<br />
Code 5170 describes catheterization <strong>of</strong> a patient for residual urine.<br />
Code 51702 describes insertion <strong>of</strong> Foley catheter for patients with chronic problems, such as<br />
neurogenic bladder <strong>and</strong> insertion <strong>of</strong> catheters in patients in acute retention in the hospital setting.<br />
Code 51703 describes a complicated insertion (e.g., altered anatomy, fractured catheter/balloon).<br />
Newby Note: Physicians should continue to use HCPCS code P9612, catheterization for<br />
collection <strong>of</strong> specimen, single patient, all places <strong>of</strong> service, when the patient is catheterized<br />
for a sterile urine specimen.<br />
GROUP PRACTICE DEFINED<br />
Medicare General Information, Eligibility, <strong>and</strong> Entitlement Chapter 5 §90.4 (Rev. 1, 09-11-02)<br />
A group practice is a group <strong>of</strong> two or more physicians <strong>and</strong> non-physician practitioners legally organized<br />
in a partnership, pr<strong>of</strong>essional corporation, foundation, not-for-pr<strong>of</strong>it corporation, faculty practice plan, or<br />
similar association:<br />
• In which each physician who is a member <strong>of</strong> the group provides substantially the full range <strong>of</strong><br />
services which the physician routinely provides (including medical care, consultation, diagnosis,<br />
or treatment) through the joint use <strong>of</strong> shared <strong>of</strong>fice space, facilities, equipment, <strong>and</strong> personnel<br />
• For which substantially all <strong>of</strong> the services <strong>of</strong> the physicians who are members <strong>of</strong> the group are<br />
provided through the group <strong>and</strong> are billed in the name <strong>of</strong> the group <strong>and</strong> amounts so received are<br />
treated as receipts <strong>of</strong> the group<br />
• In which the overhead expenses <strong>of</strong> <strong>and</strong> the income from the practice are distributed in accordance<br />
with methods previously determined by members <strong>of</strong> the group<br />
• Which meets such other st<strong>and</strong>ards as the Secretary may impose by regulation to implement<br />
§1877(h)(4) <strong>of</strong> the Social Security Act. The group practice definition also applies to health care<br />
practitioners.<br />
Physicians in Group Practice<br />
Medicare Claims Processing Manual Chapter 12 §30.6.5 (Rev. 1, 10-01-03)<br />
Physicians in the same group practice who are in the same specialty must bill <strong>and</strong> be paid as though they<br />
were a single physician. If more than one evaluation <strong>and</strong> management (face-to-face) service is provided<br />
on the same day to the same patient by the same physician or more than one physician in the same<br />
specialty in the same group, only one evaluation <strong>and</strong> management service may be reported unless the<br />
evaluation <strong>and</strong> management services are for unrelated problems. Instead <strong>of</strong> billing separately, the<br />
5-23<br />
*All CPT Codes, Descriptions, <strong>and</strong> Two-Digit Modifiers<br />
Only Are Copyright 2006 American Medical Association. GEN 2007 REV 07-01<br />
Copyright 2007 Newby Consulting, Inc.